Abstract
Both the development and exacerbation of allergic disease are complex processes involving many factors, both genetic and environmentally driven. Air pollution has long been recognized as a health hazard, contributing to the increased incidence and worsening of a variety of diseases, including allergic conditions. While identifying specific air pollutants to be a cause of such conditions can be difficult, a large body of data has provided significant evidence for the harmful effects of these substances. Both indoor and outdoor pollutants have been shown to have adverse health effects on allergic disease. Among the pollutants which have been linked to the presence and exacerbation of allergic disease are tobacco smoke, diesel exhaust, nitrogen dioxide, ozone, particulate matter, and sulfur oxides. Exposure to each of these characteristic substances has been extensively studied to determine their effects on asthma, allergic rhinitis, allergic conjunctivitis, and other atopic conditions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pollution
- Tobacco smoke
- Diesel exhaust
- Nitrogen dioxide
- Ozone
- Particulate matter
- Sulfur oxide
- Asthma
- Allergic rhinitis
- Allergic conjunctivitis
- Atopy
- Allergy
Introduction
The development and exacerbation of allergic disease are a multifaceted process involving an interplay between genetic and environmental factors. Airborne pollutants are nearly ubiquitous environmental hazards that have long been recognized as contributors to poor health outcomes in many disease processes. Recently, airborne pollutants have been implicated in the manifestations of allergic disease, especially those affecting the airways, such as asthma. The role of pollution in allergic disease is complex, and its effects vary based on a number of factors including the type of pollution and the attributes of the individual exposed to the pollution.
Characteristics of Pollutants
Indoor Versus Outdoor Pollution
Pollution is generally categorized as being either indoor or outdoor pollution, although there is overlap between the two types. Most people spend the majority of their time indoors whether they are at home, school, or work; therefore, exposure to indoor pollutants is a significant problem. Common sources of indoor air pollutants are tobacco smoke, appliances (i.e., gas stoves, fireplaces), and building and renovating materials such as paint. Environmental tobacco smoke, also known as secondhand smoke, is the most prevalent of all the indoor pollutants and has been shown to increase the risk of a number of disorders including asthma. Fortunately, some of these sources are being diminished such as through bans on indoor smoking. Nonetheless, the levels of many indoor pollutants may be up to 2–5 times higher than those found outdoors, and indoor levels can even reach 1000 times higher than outdoor levels immediately after certain activities, such as paint stripping. Exposures to indoor pollutants may also be prolonged due to the more energy-efficient, airtight building designs being used today that do not allow air to circulate as efficiently between the indoor and outdoor environments. Although these building designs bring benefits such as a reduction in heating and cooling expenditures, they also do not allow pollutants generated indoors to escape to the outdoor environment.
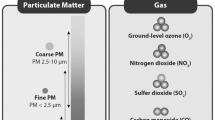
Outdoor air pollution has been the subject of intense research because of its public health implications and the potential health benefits that can be achieved on a national scale if exposure to these pollutants is reduced. To this end, the Environmental Protection Agency of the United States has set the National Ambient Air Quality Standards (NAAQS) which identify and set the national standards for acceptable levels of major outdoor pollutants that are considered to be harmful to health. Four of the six pollutants identified in the NAAQS are known contributors to the exacerbation of asthma or allergic disease (Table 28.1). The NAAQS is periodically reviewed by the Environmental Protection Agency, and changes to these standards are designed to increase protection of public health and welfare.
It is important to note that pollution is frequently a complex mixture of various pollutants; therefore, its effects are significantly more complex than those of a single pollutant listed by the NAAQS. For example, diesel exhaust contains numerous pollutants, including particulate matter, nitrogen dioxide, and carbon monoxide, that may act in concert to initiate or worsen disease.
Actions of Pollution
In general, pollution can interact with allergic disease in three ways: by contributing to the development of disease, the exacerbation of established disease, or both (Fig. 28.1). A single pollutant may act alone in all of these processes, as seen with tobacco smoke which contributes to both the development of asthma in exposed children and the exacerbation of asthma in individuals who already have the disease. On the other hand, pollutants may act in concert to initiate and exacerbate disease. For example, a child may develop asthma secondary to exposure to tobacco smoke and then develop an asthma exacerbation upon exposure to high levels of ozone.
The actions of pollutants are multifactorial. They can act in a nonspecific manner to worsen allergic disease, such as acting as simple irritants to worsen allergic rhinitis symptoms (see Chap. 6), or they can act in a more specific manner by contributing to allergic inflammation through the production of reactive oxygen species (ROS). This oxidative stress sets off a cascade of events marked by the production of pro-inflammatory products, which leads to the induction of Th2 responses and the downregulation of Th1 responses (see Chap. 1), both of which can promote the expression of allergic disease.
Characteristics of Individuals
The deleterious health effects of pollution are not only dependent on the specific features of the pollutant but also the features of the exposed population. Emerging research has shown an association between the genetic makeup of particular individuals and a predisposition to the development of allergic disease from pollution. Since airway inflammation and the response to oxidative stress are known to be genetically regulated, the variability of genes encoded to handle oxidative pathways is thought to contribute to the varying degrees of adverse health effects. In addition to genetic factors, the age of the exposed individual is one of the most important factors contributing to the effect of pollutants on an individual. The time period beginning in fetal life and extending throughout childhood is a period of marked vulnerability because this is when the respiratory tract and immune system are undergoing development and maturation. Furthermore, children usually have higher exposures to outdoor pollutants because they spend a larger portion of their time outdoors compared to adults. Children also have higher minute ventilation than adults leading to increased exposure to inhaled pollutants.
Respiratory Tract Development
The respiratory tract is only partially developed at birth and undergoes rapid changes postnatally. Development of the paranasal sinuses has only begun at birth with the presence of rudimentary ethmoid sinuses and early pneumatization of the maxillary sinuses. Complete development and pneumatization of all the sinuses do not occur until adolescence. Likewise, the lungs undergo significant changes after birth. Although the lungs are functional at birth, they are structurally immature with only a fraction of the alveoli present that will be present in adulthood. During the first 4 years of life, significant septation of the lung parenchyma occurs with the number of alveoli increasing by greater than tenfold. Pulmonary development continues to progress throughout adolescence with complete development being attained only in early adulthood. Due to the immaturity of the respiratory tract in utero and during childhood, exposure to pollution during this time period has the ability to alter normal pulmonary development, potentially leading to adverse consequences for an individual’s entire life. These adverse effects are not theoretical but are well-described events that will be discussed later in this chapter.
Immune System Development
Similar to the respiratory tract, the pediatric immune system is immature at birth and undergoes significant changes in the first few years of life. The healthy adult immune system maintains a fine balance between Th1 immune responses, which are important in cell-mediated immunity, and Th2 immune responses, which are important in humoral immunity and the development of allergic diseases. Infants naturally have a Th2-polarized immune system which later matures into an immune system which produces balanced Th1 and Th2 responses. Furthermore, atopic children maintain a Th2-polarized immune system for a longer period of time compared to nonatopic children indicating the central role of Th phenotype in allergic disease. Because the immune system continues to mature throughout early childhood, this is a time period during which children may be at heightened risk for the inappropriate skewing of immune responses toward the allergic, Th2 phenotype.
Specific Pollutants
In the following sections we will be reviewing the evidence implicating the role of various pollutants in the development of allergic disease and asthma. Tobacco smoke and diesel exhaust, two pollutants with complex mixtures of various compounds, will be discussed first, followed by the discussion of the four key pollutants affecting allergic disease identified in the NAAQS.
Tobacco Smoke
Exposure to tobacco smoke can occur through an active or passive process. Active exposure is through smoking a cigarette or other tobacco products. Passive exposure occurs by inhaling sidestream smoke (smoke released from the burning end of the cigarette) or inhaling smoke exhaled by the active smoker. This is referred to as secondhand smoke or environmental tobacco smoke (ETS).
ETS consists of a complex combination of hundreds of chemicals and pollutants. Exposure to ETS has been linked to numerous health problems affecting every age group starting from in utero development through adulthood. These health problems include intrauterine growth retardation, low birth weight, sudden infant death syndrome, asthma, otitis media, pneumonia, chronic obstructive pulmonary disease, cardiovascular disease, and cancer. Both the conducting airways and lung parenchyma can be adversely affected during development by the effects of tobacco smoke. In sudden infant death syndrome patients, inner airway wall thickening is more severe in patients with smoking mothers, compared to nonsmoking mothers, suggesting airway remodeling due to in utero and early postnatal exposure. In regard to allergic disease, ETS has been shown to both cause and exacerbate allergic diseases and asthma.
Disease Development
Current evidence supports a causal relationship between in utero exposure to tobacco smoke and disruptions of fetal airway development. While gathering randomized data on smoking during pregnancy is difficult due to ethical concerns, the majority of studies demonstrate in utero tobacco smoke negatively influences respiratory function. In utero tobacco smoke exposure has been shown to be an independent risk factor in the development of asthma, wheeze, and impaired lung function. One meta-analysis demonstrated an increased risk of asthma at 6 years old, in children exposed to antenatal tobacco smoke. In addition to its harmful in utero effects, data also favors an association between ETS and asthma development. Variability exists in clearly defining asthma end points for study among researchers, and this has contributed to some inconsistencies among studies. The vast majority of research, however, supports the link between ETS exposure and an increased risk of asthma. Postnatal tobacco smoke exposure has been shown to increase risk of asthma development among children ages 6–18 years old. ETS exposure also increases both total and allergen-specific serum IgE levels, potentially contributing to the development of other allergic diseases. It is estimated that up to 26,000 cases of childhood asthma in the United States are secondary to exposure to ETS.
Disease Exacerbation
ETS exposure has long been linked to worsening of asthma symptoms and increased emergency department visits. A large body of research has evaluated the respiratory effects of involuntary ETS exposure; however distinguishing between acute and chronic ETS exposure can be difficult and has only been undertaken in adult subjects, using controlled chamber studies. For this reason, observational studies performed are considered to represent chronic ETS exposure.
Previously, studies favored a causal relationship between ETS exposure and asthma exacerbation. More recently, studies suggest the two are strongly associated, but ETS may not be a causal factor in isolation. For example, studies involving preschool-aged children failed to show a causal relationship between ETS and worsening asthma. Similarly, in older children and adults, ETS exposure has not consistently been demonstrated to worsen asthma symptoms. Conversely, in a study of minority groups affected by asthma, in utero tobacco smoke exposure led to a higher incidence of persistent asthma in Mexican, Puerto Rican, and black patients, as well as poor asthma control in Latino and black patients. Recently published cross-sectional studies and one prospective study were able to demonstrate a worsening of asthma control and more frequent exacerbations in children exposed to ETS. Taken as a whole, these studies suggest that ETS exposure is associated with poor asthma control and asthma exacerbations in susceptible individuals, and these susceptibilities may be related to other environmental exposures or genetic factors. The lack of consistent concrete causal evidence despite the presence of the clear association that has been shown between ETS and asthma exacerbations is likely further compounded by inconsistent reporting of ETS by patients or their caregivers. A clear discrepancy has been shown between patient reporting of ETS exposure, in the form of parental surveys, and measurements of salivary cotinine levels, a nicotine metabolite.
ETS can also exacerbate allergic rhinitis and allergic conjunctivitis. ETS can act as an ocular irritant. In fact, ocular irritation is one of the most commonly reported effects of ETS by nonsmokers. The effects of ETS on the eye may be secondary to its ability to disrupt the thin, protective film of tear on the cornea. This is supported by experiments that document instability of the tear film after exposure to ETS and an increase in blinking and lacrimation (tearing), both of which act to reestablish the protective film of tear on the cornea. Although few studies have looked at ETS as the primary variable contributing to allergic conjunctivitis, symptoms of eye irritation and itching or tearing of the eyes have clearly been demonstrated in multiple studies on ETS-exposed patients.
Rhinitis symptoms also develop in many individuals upon exposure to ETS. ETS exposure can lead to the development of rhinorrhea and nasal congestion, and these symptoms coincide with objectively measured end points such as nasal airway resistance. Additionally, ETS promotes the production of allergen-specific IgE antibodies in nasal lavage, a hallmark of allergic rhinitis. Although these symptoms can occur in any individual upon exposure to ETS, they tend to be found predominately in atopic individuals.
Although different disorders of the respiratory tract have traditionally been thought of as isolated diseases, it is clear that disease activity in one part of the respiratory tract can adversely affect other parts. In other words, the respiratory tract may be envisioned as a unified system instead of as a combination of different components (i.e., nose, sinuses, lungs, etc.). For example, an episode of acute sinusitis, a disorder of the upper respiratory tract, can contribute to the development of an asthma exacerbation, a disorder of the lower respiratory tract. This concept of a unified respiratory system also extends to the effects of ETS, in that the effects of ETS that do not immediately affect the nasal cavity or lungs may still lead to exacerbations of allergic rhinitis or asthma. For example, evidence suggests the incidence of otitis media, adenoid hypertrophy, tonsillitis, and bronchitis is higher in children exposed to ETS in the home compared to those that are not. Secondary to the effects of the unified respiratory system, these disorders may contribute to the exacerbations of allergic rhinitis and asthma.
Diesel Exhaust
The burning of fuel by motor vehicles is one of the largest sources of airborne pollutants, and diesel exhaust accounts for a large portion of this pollution. Diesel exhaust consists of diesel exhaust particles (DEP) and gaseous combustion products. DEP are carbon particles of 0.1 μm or less to which numerous chemicals produced in the combustion process or already present in the atmosphere can attach. While each DEP particle is less than 0.1 μm, particles tend to combine to form aggregates with diameters of less than 0.25 μm. Gaseous combustion products include nitrogen dioxide, carbon monoxide, and hydrocarbons that are precursors to ozone production.
Like ETS, diesel exhaust has been linked to numerous adverse health outcomes including cardiovascular disease, leukemia, lymphoma, lung cancer, and wheezing. In regard to allergic disease, diesel exhaust is associated with the development and exacerbation of asthma, the promotion of sensitization to new allergens, and the enhancement of the allergic response to antigen.
Disease Development
There is significant epidemiologic and clinical research data indicating that exposure to diesel exhaust leads to the development of allergic disease. Accurate measurement of diesel exhaust exposure is difficult; therefore, studies have used proximity to automobile traffic and similar measures as a proxy for the measurement of diesel exhaust exposure. Infants exposed to traffic-related pollutants have 2.5 times the prevalence of wheezing compared to a nonexposed population. Of note, it is the proximity to traffic and the type of traffic (stop-and-go bus and truck traffic) that are the most significant risk factors for the development of disease, not the volume of traffic. Likewise, older children with exposure to traffic-related pollution have a prevalence of asthma twice as high as that compared to an unexposed population. As with asthma, exposure to DEP has been linked to the development of allergic disease. This has been clearly demonstrated in murine models in previous studies and more recently in humans where increased rates of allergic sensitization are found in individuals exposed to higher amounts of traffic-related pollutants.
From a mechanistic standpoint, there are numerous studies investigating the methods by which diesel exhaust induces the development of allergic disease. When atopic individuals are given an intranasal challenge of a new allergen plus DEP, they produce IgE specific to the allergen and upregulate Th2 cytokine production. On the other hand, atopic individuals challenged with a new allergen alone do not produce allergen-specific IgE, and there is no change in Th2 cytokine production. It has also been demonstrated that challenging individuals with DEP plus ragweed induces B lymphocytes producing ragweed-specific immunoglobulin to switch from the production of IgM to the production of IgE. This switch did not occur with challenge with ragweed alone. Therefore, diesel exhaust promotes the development of new allergic disease by inducing the immune system to produce Th2-polarized responses to new allergens and inducing the production of allergen-specific IgE.
Disease Exacerbation
In addition to being associated with the development of disease, exposure to traffic-related pollution is also associated with exacerbations of asthma. High levels of DEP exposure in children with allergic asthma result in more frequent symptoms over a 12-month period. The role of diesel exhaust in the exacerbation of asthma is described in detail in the sections below discussing the individual pollutants which are products of combustion (i.e., particulate matter, nitrogen dioxide, ozone). In general, increased exposure to traffic-related pollution increases the risk of asthma exacerbations for both children and adults.
Multiple mechanisms by which diesel exhaust exacerbates allergic disease have been elucidated. In individuals sensitized to an allergen, challenge with that particular allergen plus DEP leads to the augmented production of IgE and Th2 cytokines and downregulation of Th1 cytokines. This shift in immunoglobulin and cytokine production is a potent promoter of allergic inflammation. Furthermore, DEP augments mast cell degranulation leading to increased amounts of mast cell mediators being released from activated mast cells. DEP also alters the secretion pattern of various cytokines leading to alterations of cellular infiltration of tissues, such as the respiratory epithelium. This may promote allergic inflammation, leading to disease exacerbation.
Nitrogen Dioxide
Nitrogen dioxide (NO2) is a precursor to smog and ozone. It is both an important outdoor and indoor pollutant. Most NO2 is produced by the burning of fossil fuels by automobiles, but other important outdoor sources include fossil fuel combustion by power plants and other industrial sources. Natural gas-burning stoves are a major indoor source of NO2.
Although earlier studies evaluating the role of NO2 in allergic disease have been conflicting, more recent data suggests that NO2 does significantly influence the occurrence of asthma on elementary school-aged children. Exposure to NO2 in the air significantly influences the development of childhood asthma and symptoms of wheezing. In addition to asthma development, NO2 plays a role in the exacerbation of established disease. Indoor exposure from appliances using natural gas has been associated with an increased incidence of coughing and wheezing, and outdoor exposure has been linked to asthma exacerbations and diminished pulmonary development. NO2 has also been shown to augment the allergic response to allergen when subjects are pretreated with NO2. In addition to these direct effects, NO2 also reacts with sunlight and hydrocarbons in the atmosphere to produce ozone, another important pollutant, discussed below.
Ozone
Ozone (O3), which is naturally found in the upper parts of the atmosphere, has the beneficial effect of protecting the Earth’s surface from ultraviolet radiation produced by the sun. On the other hand, O3 is toxic when it is present in the lowest layer of the Earth’s atmosphere, known as the troposphere. As described above, ground-level O3 is produced primarily by the interaction of sunlight with by-products of fossil fuel combustion, namely, NO2 and hydrocarbons. O3 is a well-studied pollutant and has been associated with numerous adverse health outcomes including both the development and exacerbation of asthma.
Disease Development
In general, the evidence is lacking to sufficiently characterize O3 as a causative agent in the development of asthma. Studies have shown variable results with regard to O3 exposure and asthma prevalence in children. In a cohort of nearly 2500 asthma-free kindergarten and first-grade children with 3 years follow-up to evaluate the relationship between new-onset asthma and traffic-related pollution near homes and schools, there was no evidence to support that regional O3 exposure leads to the development of asthma. On the contrary, a well-conducted study investigated the role of O3 and other air pollutants on the incidence of asthma in children in southern California. Over 3500 children without asthma were followed prospectively for up to 5 years to determine if O3 exposure had an effect on the prevalence of asthma. The investigators discovered that children who spent a large amount of their time playing outdoor sports in areas with high O3 levels had greater than three times the risk of developing asthma than children who did not play outdoor sports. Outdoor sports activity had no effect on the development of asthma in areas with low O3 levels suggesting increased exposure to O3 may contribute to increased risk of asthma. Given the lack of consistent evidence directly pointing toward O3 as a risk factor for asthma development, O3 is not considered to be one of the pollutants strongly associated with increased asthma prevalence.
Disease Exacerbation
Despite the inconsistent evidence for disease development, the exacerbation of asthma secondary to exposure to O3 is well documented in numerous studies. Chronic exposure to ambient O3 is associated with a significantly increased risk of asthma hospitalizations. In addition to the deleterious effects of chronic exposure, short-term exposure to O3 has also proved harmful. Hospital admissions for respiratory symptoms and emergency department visits for asthma exacerbations increase during periods of exposure to elevated O3 levels. The use of asthma medications has also been reported to increase by nearly two times during periods of elevated O3 levels compared to periods of time with low levels. An interesting event highlighting the effect of O3 on asthma exacerbations in children occurred during the 1996 Summer Olympics in Atlanta, Georgia. During the Olympics, the city instituted citywide alternative traffic measures including expanded public transportation services and closure of the downtown area to private automobiles in an effort to decrease traffic congestion. These efforts led to a 28 % decrease in O3 levels associated with a greater than 40 % decrease in emergency department visits and hospitalizations secondary to asthma exacerbations. This study not only highlights the adverse effects of high levels of O3 but also demonstrates that reasonable changes in public policy can have a large positive impact on public health.
Of note, there may be up to a 2-day interval between O3 exposure and an increase in asthma exacerbations indicating that the effects of O3 on the respiratory system are more complex than just an irritant or bronchoconstrictive effect. This has been borne out in a number of studies involving challenges with O3. O3 exposure does lead to a rapid decrease in pulmonary function, but it also leads to pulmonary neutrophilic inflammation lasting for up to 1 day after exposure. In addition, studies have supported the notion that O3 contributes to increased innate immune activation in asthmatics. This mix of bronchoconstriction plus tissue inflammation describes mechanisms by which O3 exposure can lead to both early and delayed respiratory symptoms.
Particulate Matter
Particulate matter (PM) consists of tiny solid particles or liquid droplets that are suspended in the air and are, therefore, respirable. PM is classified into categories based on size by the US Environmental Protection Agency: <0.1 μm (ultrafine), 0.1–2.5 μm (fine), and 2.5–10 μm (coarse). PM >10 μm in diameter is not of significant concern in older children and adults because it is filtered out by the upper respiratory tract during nasal breathing. These particles may pose a problem for younger children because they are frequent mouth breathers, and the particles can therefore deposit in the lower respiratory tract. PM <0.1 μm (ultrafine) is found in relatively low levels in the environment because these particles tend to agglomerate quickly after production, yielding PM of larger sizes. When agglomeration does not occur, however, ultrafine PM can be inhaled deep into the small airways and alveoli of the lungs directly. This deposition causes penetration through the alveolar epithelial-endothelial layer, with the potential for hematogenous spread and adverse effect on a variety of organs. For example, a recently published study found that increased concentration of ultrafine particulate matter was associated with autonomic heart dysfunction in prediabetic and diabetic patients. On the other hand, PM <10 μm and <2.5 μm are considered significant pollutants because they are of a size that can easily penetrate the upper respiratory tract and deposit in the lungs, particularly PM <2.5 μm. Furthermore, PM <2.5 μm can remain airborne for many days, allowing it to be carried for many miles from its source of production.
PM is a major product of fossil fuel combustion and can be derived from a variety of traffic-related and industrial sources. PM is not a homogeneous pollutant, but rather is a combination of numerous constituents including metal ions, hydrocarbons, sulfates, nitrates, crustal materials (i.e., soil and ash), and biological contaminants. Furthermore, the composition of PM varies on a national scale due to its production from various sources in different locations. Due to this heterogeneous composition, it is difficult to identify the specific components that lead to adverse health outcomes. The Prevention and Incidence of Asthma and Mite Allergy (PIAMA) birth cohort study, however, tried to identify the importance of the different PM constituents using questionnaires, as well as lung function and allergic sensitization measurements in pediatric patients. The results indicated that certain PM constituents, particularly iron, copper, and zinc, increased the risk of allergy and asthma in school-aged children.
Disease Development
Epidemiologic studies have shown a correlation between increased levels of traffic-related air pollution and the incidence and prevalence of allergic disease. One study performed annual questionnaire reports on 3863 children during the first 8 years of life and estimated individual exposures to various pollutants, including particulate matter (PM) <2.5 μm. PM <2.5 μm levels were associated with an increased incidence and prevalence of asthma, as well as an increase in asthma symptoms. Increasing exposure to PM <10 μm has also been shown to be associated with an increased risk of developing allergic rhinitis. While further investigation is required to clearly define the role of PM in the development of allergic disease, it appears PM may be a risk factor for the development of a variety of allergic conditions.
Disease Exacerbation
Exposure to high levels of PM is associated with adverse outcomes in asthma. There is evidence that both short-term and long-term exposure to fine and ultrafine particulate matter can have detrimental effects on asthma symptomatology. There is an association between particulate matter exposure, as measured by air quality data, and increased asthma symptoms in children and adults. Elevated ambient PM levels have been associated with an increased number of hospitalizations secondary to asthma exacerbations in studies conducted in a number of countries. Elevated PM levels also lead to worsening asthma control as evidenced by increased nighttime symptoms, increased variability in peak expiratory flow rates, and lower forced expiratory volumes in 1 s. These effects may be more prominent in more severe asthmatics, defined as those requiring inhaled corticosteroids. PM exposure also leads to an increased need for asthma medication use and to increased hospitalizations secondary to respiratory infections.
Sulfur Oxides
Sulfur dioxide (SO2) is the primary sulfur oxide implicated in causing adverse outcomes in respiratory diseases. SO2 is an air pollutant derived from combustion of fossil fuels. Although SO2 is primarily produced by fossil fuel-fired power plants, it is also a by-product of numerous industrial processes; therefore, significant occupational exposures can occur in addition to environmental exposures.
Disease Development
While the adverse effect of SO2 on respiratory morbidity has been more completely defined, the association between exposure and asthma development has been more difficult to identify. Although mechanistic studies in humans are lacking, multiple animal studies have explored the mechanism by which SO2 affects airway hyperresponsiveness (AHR). One particular study investigated the effects of chronic SO2 exposure on AHR, airway inflammation, tissue remodeling, cell stiffness, and contractility of the airway smooth muscle on newborn rats. Comparisons were made between two groups of rats, those sensitized to ovalbumin (used as a model to mimic asthmatic symptoms) and normal rats. Ovalbumin-sensitized rats exposed to SO2 exhibited increased AHR, airway smooth muscle mass, contractility, and stiffness compared to normal rats. In humans, occupational exposures to SO2, such as in petroleum refineries, can lead to exposure to very high levels of the gas, which has been associated with nearly six times the risk of being diagnosed with asthma as compared to a nonexposed population. Exposure to the much lower levels of SO2 found in the atmosphere is also associated with allergic disease and asthma. In school-aged children in France, a positive association was found between increasing levels of SO2 exposure and the odds of being diagnosed with asthma or allergic rhinitis.
Disease Exacerbation
Studies evaluating the effects of SO2 on respiratory morbidity have produced convincing evidence for an adverse association. According to the National Ambient Air Quality Standards put forth by the Environmental Protection Agency, a large body of evidence shows a causal relationship between SO2 exposure and respiratory morbidity. Elevated SO2 levels have been shown to increase the rate of hospitalization for asthma exacerbations in school-aged children. Further evidence has shown that the bronchoconstrictive response to SO2 in asthmatic patients is concentration dependent, with increased responses to SO2 concentrations between 0.2 and 1.0 ppm. As with O3, this lag period until the onset of symptoms in certain individuals indicates that the effects of SO2 on asthma exacerbations are complex and likely involve both bronchospastic and immunologic effects. One study sought to identify possible mechanisms for these effects by examining asthma-related gene expression in human bronchial epithelial cells exposed to SO2. Exposure to SO2 resulted in higher ICAM-1 levels and increased EGF and EGFR expression, both of which have been implicated in the pathogenesis of asthma.
Much of the difficulty in finding associations between SO2 exposure and asthma outcomes has been the difficulty in separating the effects of SO2 from other pollutants. Furthermore, ambient SO2 can lead to the formation of sulfuric acid aerosols which may themselves contribute to asthma exacerbations leading, in turn, to difficulties in gauging the true effects of SO2.
In studies where individuals are intentionally challenged with SO2, exposure has been shown to lead to bronchospasm and drops in measurements of pulmonary function. These findings have been accompanied by symptoms of wheezing and dyspnea. Furthermore, exposure to other pollutants, such as O3, can increase the severity of adverse effects asthmatics experience upon exposure to SO2.
Conclusions
Indoor and outdoor pollutants can lead to both the development and exacerbation of allergic disease and asthma. The effects of these pollutants can occur in utero or in early childhood, potentially leading to lifelong morbidity from allergic disease or asthma. Furthermore, these pollutants can lead to exacerbations of disease throughout an individual’s life. Public policy changes to curb the adverse effects of airborne pollutants can lead to significant public health benefits by decreasing the morbidity associated with allergic and respiratory diseases.
Evidence-Based Medicine
The adverse effects of exposure to ultrafine PM were recently investigated by Peters et al. Ambulatory electrocardiograms were obtained on 64 individuals with type 2 diabetes and impaired glucose tolerance on 191 occasions over a 5–6-h time period. Personal exposure to particle number concentrations (PNC) during a 5-min time period was measured on each individual, as well as central monitoring of acquired PM <2.5 μm on an hourly basis. The results of the study showed heart rate variation associated with personally measured PNC and ambient PM <2.5 suggesting freshly emitted ultrafine PM and aged aerosol in urban areas are associated with changes in cardiac function.
Pedersen et al. evaluated the effects of low concentrations of ambient air pollution on low birth weight. Data was pooled from 14 population-based mother cohort studies in 12 European countries. Seventy-four thousand one hundred seventy-eight total women were included in the study from 1994 to 2011. Mean concentrations of PM with aerodynamic diameters of <2.5 μm, <10 μm, and 2.5–10 μm during pregnancy were estimated at home addresses. Results of the study showed that a 5 μm/m3 increase in concentration of PM <2.5 was associated with increased risk of low birth weight at term. These findings suggest air pollution and traffic exposure during pregnancy could contribute to restricted fetal growth.
While atopic dermatitis is one of the most prevalent of all the allergic diseases, it is less commonly the subject of intense research. Several cross-sectional and birth cohort studies have been performed, however, that indicate air pollution may contribute to atopic dermatitis prevalence. In one cross-sectional study involving 4907 French children aged 9–11 years old, with 3 or more years at their current residence, lifetime eczema was significantly associated with 3-year averaged concentrations of CO, NO2, NOx, and PM <10. In addition, two birth cohort studies were performed by Morgenstern et al. in Munich. Two thousand eight hundred sixty children at age 4 years old and 3061 children at age 6 years old were included in the two studies. Long-term exposure to PM <2.5, NO2, and PM <2.5 adsorbance was evaluated using geographical information systems and air pollution measurements. A surrogate for traffic-related air pollution of distance to the nearest main road was used. Results of the studies showed strong positive associations between distance to the nearest main road and presence of atopic dermatitis.
Bibliography
Gilliland FD, Li YF, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med. 2001;163(2):429–36.
Akuete K, Oh SS, Thyne S, et al. Ethnic variability in persistent asthma after in utero tobacco exposure. Pediatrics. 2011;128(3):e623–30.
Oh SS, Tcheurekdjian H, Roth LA, et al. Effect of secondhand smoke on asthma control among black and Latino children. J Allergy Clin Immunol. 2012;129(6):1478–83.e7.
Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2014.
McCarville M, Sohn MW, Oh E, Weiss K, Gupta R. Environmental tobacco smoke and asthma exacerbations and severity: the difference between measured and reported exposure. Arch Dis Child. 2013;98(7):510–4.
McConnell R, Islam T, Shankardass K, et al. Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect. 2010;118:1021–6.
Millstein J, Gilliland F, Berhane K, et al. Effects of ambient air pollutants on asthma medication use and wheezing among fourth-grade school children from 12 Southern California communities enrolled in The Children’s Health Study. Arch Environ Health. 2004;59:505.
Friedman MS, Powell KE, Hutwagner L, et al. Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA. 2001;285:897.
Gehring U, Beelen R, Eeftens M, et al. Particulate matter composition and respiratory health: the PIAMA Birth Cohort study. Epidemiology. 2015;26(3):300–9.
Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, Oldenwening M, Smit HA, Brunekreef B. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010;181(6):596–603.
Song A, Liao Q, Li J, et al. Chronic exposure to sulfur dioxide enhances airway hyperresponsiveness only in ovalbumin-sensitized rats. Toxicol Lett. 2012;214(3):320–7.
Li R, Meng Z, Xie J. Effects of sulfur dioxide derivatives on four asthma-related gene expressions in human bronchial epithelial cells. Toxicol Lett. 2007;175(1–3):71–81.
Peters A, Hampel R, Cyrys J, et al. Elevated particle number concentrations induce immediate changes in heart rate variability: a panel study in individuals with impaired glucose metabolism or diabetes. Part Fibre Toxicol. 2015;12:7.
Pedersen M, Giorgis-Allemand L, Bernard C, et al. Ambient air pollution and low birth weight: a European cohort study (ESCAPE). Lancet Respir Med. 2013;1(9):695–704.
Pénard-Morand C, Raherison C, Charpin D, et al. Long-term exposure to close-proximity air pollution and asthma and allergies in urban children. Eur Respir J. 2010;36(1):33–40.
Morgenstern V, Zutavern A, Cyrys J, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008;177(12):1331–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Casselman, J., Mahmoudi, M., Tcheurekdjian, H. (2016). Smoke, Pollution, and Allergy. In: Mahmoudi, M. (eds) Allergy and Asthma. Springer, Cham. https://doi.org/10.1007/978-3-319-30835-7_28
Download citation
DOI: https://doi.org/10.1007/978-3-319-30835-7_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30833-3
Online ISBN: 978-3-319-30835-7
eBook Packages: MedicineMedicine (R0)