Abstract
A lack of habituation in visual-evoked potentials (VEPs) is the main abnormality observed in migraineurs. However, no study of steady-state VEPs has yet evaluated pattern-reversal stimuli with respect to habituation behavior or spatial frequency. The aim of this study was to clarify habituation behavior in migraineurs between attacks and to establish characteristics of VEPs in these patients. Steady-state VEPs were sequentially recorded as checkerboard patterns in four consecutive blocks from 12 patients with migraine without aura (MO), 12 patients with migraine with aura (MA), and 12 healthy controls (HC) at four spatial frequencies of 0.5, 1.0, 2.0, and 4.0 cycles per degree (cpd) with a stimulus rate of 7.5 Hz (15 reversal/s). VEP amplitudes were consistently higher in migraineurs. However, habituation was not demonstrated in HCs, and migraineurs did not reveal a clear lack of habituation. MAs exhibited high-amplitude VEPs, depending on spatial frequency. In the MA patients, amplitude differences reached statistical significance at 2.0 cpd. The sequential amplitude changes at 0.5 cpd were significantly different in MAs compared with HCs. Migraine patients exhibited high-amplitude VEPs, which were dependent on spatial frequency, and may be related to altered excitability in pre-cortical and cortical visual processing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormal cortical excitability may play an important role in predisposition to the spontaneous, cortical spreading depression that has been suggested to represent the pathophysiology of migraine aura [1, 2]. To date, a lack of habituation in migraineurs has been the principal and reproducible interictal abnormality observed in studies of evoked potentials, such as visual-evoked potentials (VEPs) [3–10]. Previous VEP studies revealed heterogeneous results; a lack of VEP habituation may correlate with metabolic abnormalities and decreased thalamo-cortical activity [11, 12]. The increased VEP amplitude that is revealed in migraine with aura (MA), but not in migraine without aura (MO), suggests abnormal excitability in the visual cortex [13–15].
There have been a number of reports on steady-state VEPs induced by flash stimuli [16–27], including an habituation study [28]. These studies suggest a general modification in the pattern of visual reactivity. However, no study of steady-state VEPs (SSVEPs) has yet evaluated pattern-reversal stimuli with respect to habituation behavior or spatial frequency. The present study hypothesized that various spatial frequencies would differentially affect SSVEPs in MO and MA. The aim of the present study was to clarify habituation behavior in MO and MA at four different spatial frequencies to determine the spatial and temporal characteristics of VEP by means of SSVEP.
Methods
Subjects
Thirty-six subjects participated in the study: 12 patients with MO, 12 patients with MA, and 12 healthy controls (HC). Migraine diagnosis was based on criteria of ICHD-II [29]. Demographic and clinical characteristics of patients and HC are shown in Table 1. At the time of investigation, all patients were in an interictal state, with at least 72 h from a migraine attack. The interval before the next headache was also monitored to avoid including patients who experienced a migraine in the 72 h following the experimental task. The patients and HCs exhibited normal or corrected-to-normal visual acuity and were drug-free. Informed consent was obtained from all subjects.
Visual stimulation
Black and white checkerboard patterns were generated on a 17-inch monitor, which subtended 21° × 17° at a viewing distance of 90 cm. SSVEPs were performed using Neuropak Λ (Nihon Kohden, Tokyo, Japan). Four spatial frequencies of 0.5, 1.0, 2.0, and 4.0 cycle per degree (cpd) were presented. The contrast in each spatial frequency was set to 90%, with a mean luminance of 14 cd/m2. The stimulus pattern was alternated at 7.5 Hz (15 reversal/s). Four different spatial frequencies of SSVEPs were randomly presented. The subjects were comfortably seated and asked to maintain eyes on a fixed central point.
Recording
Silver–silver chloride electrodes were attached to the scalp with collodion. Electrode impedance was maintained below 5000 Ω. Binocular SSVEPs were recorded from a mid-occipital electrode (2.5 cm above the inion) with a mid-frontal reference (12 cm above the nasion). Analog data were filtered between 0.1 and 70 Hz, and were digitized at a sampling rate of 1,000 Hz. Inputs from scalp electrodes were fed into preamplifiers adjusted to a bandwidth of 1–250 Hz. Artifact rejection was automatically controlled to avoid contamination of the signal by eye movement. For each spatial frequency, a total 80 consecutive VEP responses were collected and averaged off-line 4 blocks of 20 (30 s duration per block). The blocks were acquired sequentially. Under each spatial frequency condition, presentation of visual stimuli was separated by at least 2 min.
Data analysis
The amplified electroencephalogram, which was synchronized to temporal modulation of the stimulus, was digitized and stored on a computer for further analysis. Fast Fourier transforms (FFTs) were used to calculate amplitude (μV) for double the checkerboard reversal frequency of 7.5 Hz, i.e., the second harmonic response (2F = 15 Hz). According to our previous study on SSVEPs [30], because there were no significant phase differences between MO, MA, and HC, only the 2F amplitude was analyzed.
Statistical analysis
Statistical analysis was performed using the SPSS 11.0 statistical software package for Windows. The results were compared using repeated-measures analysis of variance (ANOVA). The within-subject factor was spatial frequency, and between-subject factors served as the diagnosis and the four blocks. Mauchly’s sphericity test was performed prior to ANOVA. When appropriate, the number of degrees of freedom was adjusted according to Greenhouse and Geisser. The post hoc test analysis was performed using Tukey’s HSD test. Habituation, i.e., sequential amplitude changes, was calculated using a relative value, and amplitudes of blocks 2–4 were divided by the amplitude of block 1. The level of significance was set at P < 0.05.
Results
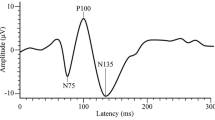
Figure 1 shows representative VEP waveforms from a normal subject and FFTs in four sequential blocks at 2.0 cpd. VEPs were characterized by two dominant waveform frequencies that corresponded to a reversal frequency. In the FFTs, the second harmonic response (2F, 15 Hz) was predominant.
Representative VEP waveforms and fast Fourier transformations (FFTs) in a healthy control during four sequential blocks at 2.0 cpd. Steady-state responses are shown in the upper column. The FFTs demonstrate that 2F is clearly distinguishable in the amplitude spectrum (arrow head, lower column). The 2F amplitude was evaluated at each block as 1.4, 1.6, 1.6, and 1.3 μ, respectively
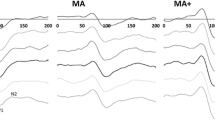
Figure 2 shows sequential mean amplitudes at each spatial frequency in the migraineurs and HC. In the first block, the mean amplitude in MO at 0.5 cpd was less than in the other blocks. However, amplitudes were greater in migraineurs at all spatial frequencies. A significant interaction between spatial frequency and diagnosis was observed (Table 2), showing that spatial frequency affected HC and migraineurs differently. In the MA patients, a post hoc test revealed that amplitude differences reached statistical significance at 2.0 cpd [F(8, 258) = 5.0, P < 0.001 for MO, P < 0.05 for HC]. There was no interaction between block and diagnosis or spatial frequency. HC and migraine patients did not show clear habituation or a lack of habituation. Figure 3 shows sequential amplitude changes at each spatial frequency in migraineurs and HC. A significant interaction between diagnosis and spatial frequency was observed (Table 3). In the MA patients, when a lower spatial frequency (0.5 cpd) was presented, the amplitude tended to increase over the blocks. In a post hoc test, the sequential amplitude changes in MA were significantly different from HC ([F(12, 262) = 2.4, P < 0.05]). These results indicated that MA showed increased sequential amplitude changes only at lower spatial frequency.
Discussion
Interictal SSVEPs at 7.5 Hz exhibited no habituation in HCs, and migraine patients did not show a clear lack of habituation. The mean amplitude in each block, as well as sequential amplitude changes and average amplitude, were influenced by spatial frequency. At 2.0 cpd, MA patients exhibited greater VEP amplitude in all four blocks, and 0.5 cpd resulted in increased sequential amplitude changes.
Results from the present study were not consistent with previous reports [3–5, 7], which demonstrated deficient habituation in migraineurs recorded by check size 8′ and 3.1 Hz, i.e., higher spatial frequency and non-flickering higher temporal frequency of transient-type pattern-reversal VEP (TVEP). The TVEP alteration in migraine-dependent pattern spatial frequency was reported to be 2.0 Hz or less, which was a slower temporal frequency [14, 15, 31–33]. These studies failed to detect habituation abnormalities. To date, habituation phenomena in normal subjects have not been evaluated in a SSVEP study. The present results are, however, consistent with steady-state VEPs using flash stimuli in a low frequency range of 3, 6, and 9 Hz [28]. These VEP studies are supported by habituation characteristics that show a relationship among stimulus repetition rates, stimulus characteristics, and degree of habituation [34]. Accordingly, the faster and smaller check-size stimulation by TVEP may play a crucial role in habituation behavior [14].
The present SSVEP study is in accordance with previous studies [30, 35] that demonstrated greater migraine amplitude between attacks. Furthermore, the amplitude tended to increase depending on spatial frequency. Generally, the response to higher spatial frequency preferentially stimulates the macular region, which has a much larger cortical representation, as opposed to lower spatial frequency that preferentially stimulates the periphery of the retina [36, 37]. The increased response to higher spatial frequency could be explained by altered excitability of the visual cortex in migraine patients [30]. A number of studies have not observed consistent MA versus MO, or migraine versus control, amplitude differences [38–43]. However, the present data suggested that increased amplitude was a general phenomenon, in particular in MA patients [13–15, 30]. Although the lack of habituation could be a result of a pre-cortical site [11, 12], high VEP amplitude could be explained in the present study by the concept of cortical hyper-responsiveness in the visual cortex [1, 44, 45]. The discrepancy between these studies might be explained by different recording conditions, such as the use of spatial and temporal frequency.
The visual system is subdivided into two parallel channels of visual processing—the magnocellular (M) and parvocellular (P) pathways, which specialize in different visual functions. The M pathway, which receives input primarily from the retinal periphery, is more sensitive to high-temporal and low-spatial frequency stimuli, while the P pathway receives input primarily from the foveal and perifoveal areas and is preferentially activated by low-temporal and high-spatial frequency stimulation [14, 46, 47]. Spatial and temporal frequency has been suggested to play an important role in visual processing of migraine [30, 37, 48–53]. Psychophysical tests identified a pre-cortical site of action in the pathophysiology of migraine [49, 50, 52]. Previous reports have suggested that migraine affects the M [50, 54], or both the M and P [53, 55], pathways, while other studies did not confirm M pathway deficits [56]. Using TVEP, Oelkers et al. [14] hypothesized that migraine patients have a relatively impaired P pathway and a predominant M pathway. Different involvement of the P and M pathways may play a role in habituation behavior.
In this study, the HC did not show habituation, but there were increased sequential amplitude changes in MA patients at lower spatial frequency of 0.5 cpd. This suggests the excitability change cannot be interpreted as “lack of habituation”. In accordance with our study, Chen et al. [33] reported that migraineurs showed a larger amplitude increment than controls in sequential blocks only at lower spatial frequency. The findings may suggest “augmented potentiation” or “relative habituation deficit”. A recent study by Omland et al. [57] also revealed that habituation may not be detectable in healthy subjects using large 65′ checks, i.e., lower spatial frequency and reversal rate had less influence than lower spatial frequency on habituation. The difference in excitability of the visual cortex in migraine may preferentially involve the M pathway [33].
A previous study [28] reported that steady-state VEP, induced by flash stimuli at low frequency range, altered amplitude in a complex way, which could be explained by a variability phenomenon. Increased variability with response to low-temporal frequency in migraine could be interpreted as an overactive regulation mechanism, and this effect may result from activation of the M extrastriate pathways. Unstructured flash stimuli are likely to be processed primarily in the M pathway [36]. Therefore, increased sequential amplitude changes in MA might be due to stimulation conditions at a low-spatial frequency and flickering, which are similar to M pathway conditions. The current findings might be linked to predominance of the M system in MA and suggest that P–M imbalance plays a role in migraine pathophysiology. This is consistent with previous reports of VEPs [30] and psychophysical findings [45, 58]. Although the question of predominance of P or M neuronal dysfunction remains, it is likely that migraine patients have pre-cortical dysfunctions, in addition to altered excitability of the visual cortex [28].
Our previous TVEP study [37] demonstrated high-spatial frequency (4.0 cpd) with a high-contrast (98%) pattern, which was preferable to stimulate the P pathway. These conditions were determined to be effective for revealing abnormal reactivity in MO and MA patients [58, 59]. However, using these conditions, a low-contrast (29%) pattern also resulted in increased amplitude. Similar to previous results [60], hyperreactivity of the P pathway is not likely to result in migraine.
Our previous SSVEP study at 5 and 10 Hz [30] demonstrated that MA patients exhibited high-amplitude VEPs, but no significant amplitude differences were detected at 2.0 cpd. The discrepancy between this and the current study may be due to the different temporal frequencies utilized. A checkerboard VEP pattern is very complex in terms of FFTs, and a 0.5 cpd pattern includes other components of cpd [61]. Furthermore, a temporal frequency of 7.5 Hz does not selectively stimulate the M pathway in high-contrast (90%) vs. low-contrast (20%) conditions [62, 63]. VEPs induced by square-wave gratings are required to determine amplitude changes at each frequency, as well as to determine P pathway functions [59].
A limitation of this study is the stimulus time of VEPs. Previous VEP habituation studies used longer recording sessions of 3–15 min [3, 4, 14, 15, 33, 57], compared with 2 min in our study. The criteria of habituation proposed that a high repetition rate speeds up the habituation, and a low repetition rate slows it down [34]. A future study with a longer SSVEP stimulus time is required to clarify the habituation behavior in migraine.
In conclusion, interictal migraine patients exhibited high-amplitude SSVEPs, which were dependent on spatial frequency, and may be related to altered excitability in pre-cortical and cortical visual processing.
References
Welch KM (2003) Contemporary concepts of migraine pathogenesis. Neurology 61:S2–S8
Berger M, Speckmann E-J, Pape HC, Gorji A (2008) Spreading depression enhances human neocortical excitability in vitro. Cephalalgia 28:558–562
Schoenen J, Wang W, Albert A, Delwaide PJ (1995) Potentiation instead of habituation characterizes visual evoked potentials in migraine patients between attack. Eur J Neurol 2:115–122
Áfra J, Cecchini AP, De Pasqua V, Albert A, Schoenen J (1998) Visual evoked potentials during long periods of pattern-reversal stimulation in migraine. Brain 121:233–241
Sándor PS, Áfra J, Cecchini AP, Albert A, Schoenen J (1999) Familial influences on cortical evoked potentials in migraine. Neuroreport 26:1235–1238
Wang W, Wang GP, Ding XL, Wang YH (1999) Personality and response to repeated visual stimulation in migraine and tension-type headaches. Cephalalgia 19:718–724
Bohotin V, Fumal A, Vandenheede M, Gérard P, Bohotin C, Maertens de Noordhout A, Schoenen J (2002) Effects of repetitive transcranial magnetic stimulation on visual evoked potentials in migraine. Brain 125:912–922
Fumal A, Coppola G, Bohotin V, Gérardy PY, Seidel L, Donneau AF, Vandenheede M, Maertens de Noordhout A, Schoenen J (2006) Induction of long-lasting changes of visual cortex excitability by five daily sessions repetitive transcranial magnetic stimulation (rTMS) in healthy volunteers and migraine patients. Cephalalgia 26:143–149
Coppola G, Ambrosini A, Di Clemete L, Magis D, Fumal A, Gérard P, Pierelli F, Schoenen J (2007) Interictal abnormalities of gamma band activity in visual evoked responses in migraine: an indication of thalamocortical dysfunction? Cephalalgia 27:1323–1330
Magis D, Allena M, Coppola G, Di Clemente L, Gérard P, Schoenen J (2007) Search for correlations between genotypes and electrophysiological patterns in migraine: the MTHFR C677T polymorphism and visual evoked potentials. Cephalalgia 27:1142–1149
Schoenen J, Ambrosini A, Sándor PS, de Noordhout AM (2003) Evoked potentials and transcranial magnetic stimulation in migraine: published data and viewpoint on their pathophysiologic significance. Clin Neurophysiol 114:955–972
Coppola G, Pierelli F, Schoenen J (2007) Is the cerebral cortex hyperexcitable or hyperresponsive in migraine? Cephalalgia 27:1429–1439
Shibata K, Osawa M, Iwata I (1997) Pattern reversal visual evoked potentials in classic and common migraine. J Neurol Sci 145:177–181
Oelkers R, Grosser K, Lang E, Geisslinger G, Kobal G, Brune K, Lötsch J (1999) Visual evoked potentials in migraine patients: alterations depend on pattern spatial frequency. Brain 122:1147–1155
Sand T, Zhiniy N, White LR, Stovner LJ (2008) Visual evoked potential latency, amplitude and habituation in migraine: a longitudinal study. Clin Neurophysiol 119:1020–1027
Simon RH, Zimmerman AW, Tasman A, Hale MS (1982) Spectral analysis of photic stimulation in migraine. Electroencephalogr Clin Neurophysiol 53:270–276
Nyrke T, Lang AH (1982) Spectral analysis of visual potentials evoked by sine wave modulated light in migraine. Electroencephalogr Clin Neurophysiol 53:436–442
Nyrke T, Kangasniemi P, Lang AH, Petersen E (1984) Steady-state visual evoked potentials during migraine prophylaxis by propranolol and femoxetine. Acta Neurol Scand 69:9–14
Nyrke T, Kangasniemi P, Lang AH (1989) Difference of steady-state visual evoked potentials in classic and common migraine. Electroencephalogr Clin Neurophysiol 73:285–294
Nyrke T, Kangasniemi P, Lang AH (1990) Transient asymmetric of steady-state visual evoked potentials in classic migraine. Headache 30:133–137
Genco D, de Tommaso N, Prudenzano AM, Savarese M, Puca FM (1994) EEG features in juvenile migraine: topographic analysis of spontaneous and visual evoked brain electrical activity: a comparison with adult migraine. Cephalalgia 14:41–46
Puca FM, de Tommaso M, Tota P, Sciruicchio V (1996) Photic driving in migraine: correlations with clinical features. Cephalalgia 16:246–250
de Tommaso M, Sciruicchio V, Guido M, Sasanelli G, Specchio LM, Puca FM (1998) EEG spectral analysis in migraine without aura attacks. Cephalalgia 18:324–328
de Tommaso M, Sciruicchio V, Guido M, Sasanelli G, Puca F (1999) Steady-state visual-evoked potentials in headache: diagnostic value in migraine and tension-type headache patients. Cephalalgia 19:23–26
de Tommaso M, Marinazzo D, Guido M, Libro G, Stramaglia S, Nitti L, Lattanzi G, Angelini L, Pellicoro M (2005) Visually evoked phase synchronization changes of alpha rhythm in migraine: correlations with clinical features. Int J Psychophysiol 57:203–210
de Tommaso M, Marinazzo D, Nitti L, Pellicoro M, Guido M, Serpino C, Stramaglia S (2007) Effects of levetiracetam vs. topiramate and placebo on visually evoked phase synchronization changes of alpha rhythm in migraine. Clin Neurophysiol 118:2297–2304
Angelini L, de Tommaso M, Guido M, Hu K, Ivanov PCh, Marinazzo D, Nardulli G, Nitti L, Pellicoro M, Pierro C, Stramaglia S (2004) Steady-state visual evoked potentials and phase synchronization in migraine patients. Phys Rev Lett 93:038103 1–4
de Tommaso M, Stramaglia S, Schoffelen JM, Guido M, Libro G, Losito L, Sciruicchio V, Sardaro M, Pellicoro M, Puca FM (2003) Steady-state visual evoked potentials in the low frequency range in migraine: a study of habituation and variability phenomena. Int J Psychophysiol 49:165–174
Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders, 2nd edn. Cephalalgia 24(suppl 1):1–160
Shibata K, Yamane K, Otuka K, Iwata M (2008) Abnormal visual processing in migraine with aura: a study of steady-state visual evoked potentials. J Neurol Sci 271:119–126
Khalil NM, Legg NJ, Anderson DJ (2000) Long term decline of P100 amplitude in migraine aura. J Neurol Neurosurg Psychiatry 69:507–511
Sand T, Vingen JV (2000) Visual, long-latency auditory and brainstem auditory evoked potentials in migraine: relation to pattern size, stimulus intensity, sound and light discomfort thresholds and pre-attack state. Cephalalgia 20:804–820
Chen WT, Wang SJ, Fuh JL, Lin CP, Ko YC, Lin YY (2009) Peri-ictal normalization of visual cortex excitability in migraine: an MEG study. Cephalalgia 29:1202–1211
Thompson RF, Spencer WA (1966) Habituation: a model phenomenon for the study of neuronal substrates of behavior. Psychol Rev 73:16–43
Diener HC, Sholtz E, Dichgans J, Gerber WD, Jäck A, Bille A, Niederberger U (1989) Central effects of drugs used in migraine prophylaxis evaluated by visual evoked potentials. Ann Neurol 25:125–130
Regan D (1989) Human brain electrophysiology; evoked potentials and evoked magnetic field in science and medicine. Elsevier, Amsterdam
Shibata K, Yamane K, Iwata M, Ohkawa S (2005) Evaluating the effects of spatial frequency on migraines by using pattern-reversal visual evoked potentials. Clin Neurophysiol 116:2220–2227
Kennard C, Gawel M, Rudolph NM, Rose FC (1978) Visual evoked potentials in migraine subjects. Headache 6:73–80
Polich J, Ehlers CL, Dalessio DJ (1986) Pattern-shift visual evoked responses and EEG in migraine. Headache 26:451–456
Mariani E, Moschini V, Pastorino G, Rizzi F, Severgnini A, Tiengo M (1988) Pattern-reversal visual evoked potentials and EEG correlations in common migraine patients. Headache 28:269–271
Drake ME, Pakalnis A, Hietter SA, Padamandan H (1990) Visual and auditory evoked potentials in migraine. Electromyogr Clin Neurophysiol 30:77–81
Tagliati M, Sabbadini M, Bernardi G, Silvestrini M (1995) Multichannel visual evoked potentials in migraine. Electroencephalogr Clin Neurophysiol 96:1–5
Sener HO, Haktanir I, Demirci S (1997) Pattern-reversal visual evoked potentials in migraineurs with or without aura. Headache 37:449–451
Aurora SK, Barrodale P, Chronicle EP, Mulleners WM (2005) Cortical inhibition is reduced in chronic and episodic migraine and demonstrates a spectrum of illness. Headache 45:546–552
Aurora SK, Wilkinson F (2007) The brain is hyperexcitable in migraine. Cephalalgia 27:1442–1453
Livingstone M, Hubel D (1988) Segregation of form, color, movement, and depth: anatomy, physiology, and perception. Science 240:740–749
Bassi CJ, Lehmkuhle S (1990) Clinical implications of parallel visual pathways. J Am Optom Assoc 61:98–110
Khalil NM (1991) Investigations of visual function in migraine using visual evoked potentials and visual psychophysical tests. PhD thesis, University of London
Coleston DM, Chronicle E, Ruddock KH, Kennard C (1994) Precortical dysfunction of spatial and temporal visual processing in migraine. J Neurol Neurosurg Psychiatry 57:1208–1211
Benedek K, Tajti J, Janáky M, Vécsei L, Benedek G (2002) Spatial contrast sensitivity of migraine patients without aura. Cephalalgia 22:142–145
Huang J, Cooper TG, Satana B, Kaufman DI, Cao Y (2003) Visual distortion provoked by a stimulus in migraine associated with hyperneuronal activity. Headache 43:664–671
Kowacs PA, Piovesan EJ, Werneck LC, Fameli H, Zani AC, da Silva HP (2005) Critical flicker frequency in migraine. A controlled study in patients without prophylactic therapy. Cephalalgia 25:339–343
McKendrick AM, Badcock DR (2003) Contrast-processing dysfunction in both magnocellular and parvocellular pathways in migraineurs both with or without aura. Invest Ophthalmol Vis Sci 44:442–448
McKendrick AM, Vingrys AJ, Badcock DR, Heywood JT (2001) Visual dysfunction between migraine events. Invest Ophthalmol Vis Sci 42:626–633
McKendrick AM, Sampson GP (2009) Low spatial frequency contrast sensitivity deficits in migraine are not visual pathway selective. Cephalalgia 29:539–549
Harle DE, Evans BJW (2005) Frequency doubling technology perimetry and standard automated perimetry in migraine. Ophthal Physiol Opt 25:233–239
Omland PM, Nilsen KB, Sand T (2011) Habituation measured by pattern reversal visual evoked potentials depends more on check size than reversal rate. Clin Neurophysiol (in press)
McKendrick AM, Badcock DR (2004) Motion processing deficits in migraine. Cephalalgia 24:363–372
Porciatti V, Sartucci F (1999) Normative data for onset VEPs to red-green and blue-yellow chromatic contrast. Clin Neurophysiol 110:772–781
Shibata K, Yamane K, Iwata M (2006) Change of excitability in brainstem and cortical visual processing in migraine exhibiting allodynia. Headache 46:1535–1544
Kelly DH (1976) Pattern detection and the two-dimensional fourier transform: flickering checkerboards and chromatic mechanisms. Vis Res 16:277–287
Schechter I, Butler P, Zemon VM, Revheim N, Saperstein AM, Jalbrzikowski M, Pasternak R, Silipo G, Javitt DC (2005) Impairments in generation of early-stage transient visual evoked potentials to magno- and parvocellular-selective stimuli in schizophrenia. Clin Neurophysiol 116:2204–2215
Tobimatsu S, Celesia GG (2006) Studies of human visual pathophysiology with visual evoked potentials. Clin Neurophysiol 117:1414–1433
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shibata, K., Yamane, K., Nishimura, Y. et al. Spatial frequency differentially affects habituation in migraineurs: a steady-state visual-evoked potential study. Doc Ophthalmol 123, 65–73 (2011). https://doi.org/10.1007/s10633-011-9281-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-011-9281-2