Abstract
Liver fibrosis is characterized by an activation of hepatic stellate cells (HSC). During primary culture HSC evolve from a quiescent into an activated phenotype which is characterized by α-smooth muscle actin (α-SMA) up-regulation, increase in cell growth, and extracellular matrix secretion. HSC culture with trans-resveratrol can lead to deactivation of myofibroblast-like HSC. We used an HSC line, PAV-1, to check the role of retinol and palmitic acid in the deactivation process of HSC. Using mass and metabolic-based methods, Western blot and immunocytochemistry assays, we demonstrated that treatment with palmitic acid (75 μM) alone or in combination with retinol (2 μM) significantly decreased cell proliferation and α-SMA expression. We also established that the association of both compounds strongly decreased collagen type I expression. Our results suggest the potential use of palmitic acid alone or in combination with retinol to induce HSC deactivation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
During in vitro primary culture or during in vivo liver fibrosis, hepatic stellate cells (HSCs) evolve gradually from a “quiescent” into an “activated” phenotype also called a “myofibroblast-like” phenotype which is characterized by (i) α smooth-muscle (α-SMA) actin up-regulation, (ii) loss of lipid droplets containing retinoid stores, and (iii) an increase in cell growth, accompanied by (iv) an increase in extracellular matrix (ECM) protein synthesis and secretion [1, 2].
Because of its importance in the fibrotic process, there is considerable interest in establishing cellular or animal models that allow studies of the activation process.
HSC deactivation is an issue frequently raised in the literature but not yet fully elucidated. Recent studies [3–5], using primary human myofibroblast-like cells, have shown that HSC culture with trans-resveratrol, basement membrane, or relaxin leads to a “reversal of activation” or a “deactivation” of myofibroblast-like HSC.
Long-term therapeutic vitamin A administration in humans causes liver damage such as perisinusoidal fibrosis [6–9]. In rat models, a retinoic acid analogue promoted porcine serum-induced fibrosis by inducing TGF-ß and thus collagen levels in the liver, although the retinoic acid analogue alone was not fibrogenic [10]. Supplementation with retinyl palmitate in experimental hepatic fibrosis suppresses fibrogenesis [11–19] and a high level of vitamin A has the potential to increase the hepatic toxicity of CCl4 [20]. These studies showed that retinoids are clearly involved in fibrogenesis but the results seem contradictory and more data are necessary to understand their roles [21, 22].
Two types of cellular model can be used to study the mechanisms involved in HSC activation: (i) primary HSC culture, which enables cells close to physiology to be obtained, but with a low yield and poor reproducibility between different isolations, and (ii) HSC line culture, which allows easier practical study, with numerous resistant cells leading to greater homogeneity between experiments. In spite of their activated phenotype, HSC lines can nevertheless be considered a useful tool for investigating the biology of HSC and especially precise cellular and molecular events involved in the regulation of HSC activation. Indeed, several groups have developed HSC lines as an alternative model to primary HSCs. The first established HSC line was GRX, obtained from spontaneous immortalization of HSC using limiting dilution cloning of primary cells obtained from murine liver [23]. HSC lines have also been established from species others than the mouse: (i) from human tissues (GREF-X, LI 90, LX-1, LX-2) (24–27) and (ii) from rat tissues (NFSC, CFSC, CFSC-2G, PAV-1, HSC-T6) [28–31].
In previous studies, we have established PAV-1, an immortalized rat HSC line, as a useful tool for studying retinoid metabolism [30, 32]. Indeed, treatment of these cells with physiological concentrations of retinol (Rol) and palmitic acid (PA) increases vitamin A stores and affects their phenotype. Therefore, the aim of this study was to determine whether treatment of PAV-1 with Rol and PA could lead to deactivation of HSC by modifying the main characteristics of activated HSCs, i.e., (i) cell growth, (ii) expression of phenotypic markers such as α-SMA, and (iii) expression of ECM protein, such as type I collagen.
Materials and methods
Chemicals
DMEM, glutamine, penicillin, streptomycin, and fetal calf serum (FCS) were purchased from Life Technologies (Eragny, France). All-trans retinol (Rol), palmitic acid (PA), resveratrol, essential fatty acid-free bovine serum albumin (BSA), 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT), monoclonal anti-α-SMA (mouse IgG2a, A2547), TRITC conjugate (T6778) goat anti-rabbit immunoglobulins; 4’,6-diamidino-2-phenylindole (DAPI), and 1,4-diazabicyclo[2.2.2]octane (DABCO) were purchased from Sigma-Aldrich (St-Quentin Fallavier, France). Biotinylated rabbit anti-mouse immunoglobulins (E0464) were supplied by Dako (Trappes, France). FITC goat anti-mouse immunoglobulins (SC 2079) were purchased from Tebu-Santa Cruz (Le Perray-en-Yvelines, France). The 5-bromo-2’ deoxyuridine (BrdU) ELISA kit was purchased from Roche (Mannheim, Germany). Rabbit anti-rat type I collagen was supplied by Novotec (Lyon, France).
Routine culture conditions for PAV-1
PAV-1 cells were obtained as described by Sauvant et al [30]. Under routine culture conditions, PAV-1 cells were cultured on Falcon dishes in routine DMEM supplemented with 20 mM glutamine, 10 IU/mL penicillin, 100 μg/mL streptomycin, and 10% FCS. For all experiments, cells were maintained in a humidified incubator with 5% CO2, 95% air at 37°C and medium was changed every day.
Experimental culture conditions for PAV-1
Retinol-supplemented medium. Rol was stored at –20°C under nitrogen in 1000× stock solution in absolute ethanol (Riedel-de Haën, Seelze, Germany). Rol-treated cells were cultured in DMEM-Rol, i.e., DMEM supplemented with Rol to a final concentration of 2 μM (less than 0.1% ethanol final concentration).
Palmitic acid-supplemented medium. A stock solution of 390 mM PA was prepared in ethanol and conserved at room temperature. Before dilution, this solution was warmed in a 37°C bath to avoid palmitic acid crystallization. Stock solution was then diluted in DMEM to give a final concentration of 75 μM PA (DMEM-PA). DMEM-Rol-PA was prepared by the addition of 2 μM Rol in DMEM-PA.
Control media. DMEM supplemented with the same amount of ethanol as DMEM-Rol-PA was used . Rol and PA concentrations were previously choosen according to the levels of these compounds found in human physiology and the amount of esterification observed in the PAV-1 cell line [32].
For all experiments, media were changed daily. The cytotoxicity of Rol, PA, and ethanol (at maximal concentrations used in our study) was assayed by MTT [33] according to the manufacturer’s instructions. No toxicity greater than 5% was observed.
Cell growth
Cell growth was estimated first by mass-based and then by metabolic-based methods. Mass-based methods were used to quantify amounts of cellular material such as cell number and protein or DNA content. Metabolic-based assays were used to measure proliferation rate.
Mass-based methods. Three million cells were seeded in 100-mm Falcon petri dishes. The cells were allowed to settle overnight before the different treatments were started (see above). Before counting in Malasez cell, cells were washed twice in PBS, then trypsinized and resuspended in PBS. For protein and DNA content measurements, cells were washed twice with PBS, scraped off in PBS with a rubber policeman, and homogenized using ultrasound. Protein was assayed on this cell suspension as described by Lowry et al. [34] and DNA content measured as described by Labarca and Paigen [35].
Metabolic-based methods. For BrdU incorporation assay, cells were seeded in 96-well culture plates. The cells were allowed to settle overnight before the different treatments were started and proliferation was assayed using a BrdU/ELISA proliferation kit according to the manufacturer’s instructions.
Western blot
HSC were harvested in 50 mM Tris/HCl buffer containing 25 mM NaCl, 2.5 mM EDTA, 1 mM dithiotreitol, pH 7.4. Proteins were assayed using the method described by Lowry et al. [34]. Thirty micrograms of proteins was submitted to SDS-PAGE, 15% acrylamide, under denaturing conditions [36]. After electrophoresis, the proteins were transferred onto nitrocellulose sheets [37] for detection of α-SMA by Western blotting. Equal loading of protein in each lane was confirmed with Ponceau staining. The nitrocellulose sheets were incubated with monoclonal anti-α-SMA (1:200 in PBT, PBS with 2% Tween 20) and then with biotynylated rabbit anti-mouse immunoglobulins (1:400 in PBT). Immunoreactive bands were visualized with vectastain ABC reagents (Vector Laboratories, Burlingame, CA) using diaminobenzidine as substrate according to the manufacturer’s instructions. Densitometry was performed on a scanned nitrocellulose sheet with Melany 3.0 software (Genebio, Geneva, Switzerland).
Immunocytochemistry
PAV-1 cells were cultured with the experimental media during 48 hr in petri dishes. Cells were then trypsinized and 30,000 cells/well were seeded in four-well Falcon culture slides (Elvetec, Genas, France) during a further 24 hr.
Cells were washed twice with PBS and fixed with acetone and formaldehyde (4%) in PBS. They were incubated overnight at room temperature with monoclonal anti-α SMA (1:40 in PBT) or with rabbit anti-rat type I collagen (1:40 in PBT). After a 4-hr incubation with FITC goat anti-mouse immunoglobulins (1:400 in PBT) or TRITC conjugate goat anti-rabbit immunoglobulins (1:200 in PBT), slides were counterstained with DAPI and mounted in 1% DABCO diluted in PBS/glycerol (90/10; v/v). Slides were then observed with a Zeiss Axiophot microscope (Karl Zeiss Microscopy, Jena, Germany). Images were acquired using an Axiocam camera (Carl Zeiss Vision, Hallbergmoos, Germany) by means of the Axio Vision processing and analysis system.
Chromatographic analysis of retinoids
Rol and retinyl esters were measured as previously described [32].
Flow cytometry
PAV-1 cells were cultured with the experimental media during 48 hr in petri dishes. Cells were then trypsinized and a fresh cell suspension was analyzed with Cytoron Absolute, equipped with a 488-nm argon laser (Ortho Diagnostic System). For ploidy analysis, cells were stained with propidium iodure (DNAcon3 Dako Kit).
Image cytometry
PAV-1 cells were cultured with the experimental media during 48 hr in petri dishes. Cells were then trypsinized and 30000 cells were seeded in one-well culture slides (Elvetec, Genas, France) during 24 hr.
Cells were washed twice with PBS and air-dried at ambient temperature during 24 hr. They were then fixed with Bohm Sprenger, dehydrated, and maintained at 4°C temperature. For ploidy analysis cells were colored with Feulgen stain and analyzed with Samba Technologies software 4.23.
Statistical analysis
Data are expressed as mean ± SE. Data were analyzed by analysis of variance (ANOVA) or paired t test. The level of significance was set at P < 0.05.
Results
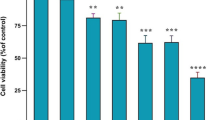
In order to determine the roles of retinyl esters (more particularly, retinyl palmitate) in HSC deactivation, we first checked the effect of Rol and PA on PAV-1 cell proliferation, using global experimental assays. As we obtained before [29], treatment of PAV-1 cells with Rol (2 μM) and PA (75 μM) induced an increase in Rol esterification and retinyl palmitate storage (data not shown). We first studied proliferation by cell counting and cell weight measurement on PAV-1 cells seeded at the same density for all treatment conditions and treated or not with 2 μM Rol and 75 μM PA. When cells were treated with ethanol (control cells), the cell number showed a 3.4-fold increase between day 1 and day 5, statistically more important than the increase of cells treated with DMEM-Rol-PA (i.e., 2.4-fold). Using weight measurement, a complementary experimental access to proliferation study, we observed a similar decrease in cell proliferation with DMEM-Rol-PA (3.4- versus 2.6-fold increase for control and Rol-PA-treated cells respectively). These first results were confirmed using mass- and metabolic-based methods. Protein and DNA content were statistically lower in cells treated with DMEM-Rol-PA than in control cells, suggesting a decrease in the cellular proliferation rate. This decrease was also found with the metabolic-based method: BrdU incorporation (Fig. 1).
PAV-1 growth measured by mass-based methods (protein and DNA contents: results are expressed as mean±SE; n=3) or metabolic-based methods (BrdU incorporation; results are expressed as mean±SE; n=12) in control and retinol (2 μM)-, palmitic acid (75 μM)-, and retinol plus palmitic acid-treated cells. * P < 0.05 and ** P < 0.01: control vs. treated cells (cells treated the same day)
To further investigate the involvement of both compounds, we tested Rol and PA effects on PAV-1 proliferation separately. The effect observed with DMEM-Rol-treated cells on total cellular protein content, DNA content, and BrdU incorporation was not statistically different from controls. By contrast, a drastic decrease in cell growth (checked by the three assays) was observed after 3 days of treatment with DMEM-PA (Fig. 1). This decrease was maintained for up to 5 days: decreases of 30, 44, and 46% for DNA content, BrdU incorporation, and protein content, respectively (P < 0.0001). No statistical difference was noted for cellular proliferation between PAV-1 treated either with PA alone or with the combination of Rol and PA, suggesting a major role of PA in the PAV-1 proliferation rate decrease. To investigate the PA-dependent mechanism involved in the decrease in cell numbers, we analyzed the cell cycle by flow cytometry and image analysis. The percentage of cells in phase G0/G1 increased from 51% in control cells to 65% in cells treated with PA (P < 0.02). No modification was observed in phase G2/M. A decrease in the S phase was also observed (Fig. 2). Using image analysis, we confirmed that the percentage of cells in phase G0/G1 increased in cells treated with PA (Fig. 3).
The second step of our work was to check the expression of α-SMA after treatment with ethanol, Rol, PA, and Rol-PA. Control treatment (ethanol) does not affect α-SMA expression during 72 hr (Fig. 4A). Rol significantly decreases the expression of α-SMA after 48 hr of treatment (P < 0.0001) (Fig. 4B). The expression of α-SMA was reduced earlier, after 24 hr of treatment, by PA (P < 0.0001) (Fig. 4C). The same timing (effect observed after 24 hr) was observed with Rol-PA (P < 0.0001) (Fig. 4D). The expression of α-SMA was strongly reduced by Rol-PA (almost not detectable by our analytical method) after 48 hr of treatment. Compared to Rol or PA treatment, there is a significant decrease in alpha-SMA protein levels, suggesting a synergic effect of PA and Rol on the regulation of alpha-SMA expression (p < 0.0001). This synergic effect of Rol and PA on α-SMA could also be visualized by immunocytochemistry assay (Fig. 5). Collagen type 1 expression was also used as another well-established marker of activation of the stellate cell line to confirm the effect of Rol and PA. No effect was observed with Rol treatment. A strong reduction of collagen type 1 expression was also observed with the association of the two compounds (Fig. 6), highlighting the role of the combination of Rol and PA on phenotypic markers of activation.
Effect of retinol (Rol; 2 μM), palmitic acid (PA; 75 μM), and combined Rol and PA (Rol+PA) on the expression of α-SMA measured by Western blot (densitometry was performed on a scanned nitrocellulose sheet). Equal loading of protein in each lane was confirmed with Ponceau staining. The results presented are the mean±SE of four experiments. Ethanol (EtOH) had no effect on α-SMA expression. Rol, PA, and Rol+PA significantly decreased the expression of α-SMA after 24 hr of treatment. Rol+PA induced a more important decrease in α-SMA expression. *Significantly different from H0; P < 0.0001
Effect of retinol (Rol; 2 μM), palmitic acid (PA; 75 μM), and the combination of Rol and PA (Rol+PA) on the expression of α-SMA measured by immunocytochemistry. α-SMA was stained with FITC goat anti-mouse immunoglobulins (green). The nucleus was counterstained with DAPI (blue). Ethanol (EtOH) had no effect on α-SMA expression after 48 hr of treatment. Rol decreased the expression of α-SMA. PA also decreased the expression of α-SMA. Rol/PA acid nearly abolished the expression of α-SMA after 48 hr of treatment. (Original magnification, ×63)
Effect of ethanol and palmitic acid (75 μM) on the expression of collagen I measured by immunocytochemistry. Collagen I was stained with goat anti-rabbit immunoglobulin TRITC conjugate (orange). The nucleus was counterstained with DAPI (blue). Ethanol (A) had no effect on collagen I expression after 72 hr of treatment. The combination retinol/palmitic acid nearly abolished the expression of collagen I after 72 hr of treatment (B). (Original magnification, ×63)
Discussion
HSCs are the main storage site for vitamin A. Eighty to ninety percent of the body’s vitamin A is stored in these cells as retinyl esters. In quiescent cells, retinyl palmitate represents 62% of the retinyl esters [38]. In vivo studies have clearly shown that administration of retinyl palmitate (total dose administered to every rat, ≤200000 IU) protects the liver from fibrosis in different models of fibrosis [11, 17, 18]. In vitro experiments [39–48] have mainly focused on the effects of Rol and/or retinoic acid on HSC. Surprisingly few works have studied the effect of PA and retinyl palmitate on HSC proliferation. Using 10 μM PA, some authors found no effect on proliferation of activated HSCs [50]. Two groups checked the effects of retinyl palmitate on HSC proliferation. In the first study, no effect was observed [43], in contrast with the second work, where a decrease in proliferation was established [17]. In Mizobuchi’s study, it was not possible to determine if the decrease in proliferation was due to the retinoids, to the fatty acid, or both. In our work, we showed, that PA induces a significant decrease in proliferation of α-SMA and collagen I expression, strongly suggesting that PA plays an important role to maintain HSCs in the quiescent state. The synergistic effect observed between Rol and PA on the expression of α-SMA and collagen highlights the cooperation between retinoids and fatty acids and does not involve only retinoids as previously suggested [44].
The choice to use first mass-based methods to establish the global effect of PA and Rol on proliferation was supported by the work of Tronstad et al. [51] demonstrating that cell density modifies the response to lipids. They proposed the use of mass-based methods to study the effect of lipids on proliferation since these methods are insensitive to metabolic changes caused by confluence. In our study, the results obtained by mass-based methods and metabolic-based methods were correlated and we observed a decrease in proliferation with both methods. Albumin/fatty acid ratio could also modify the response to fatty acid by decreasing the free fatty acid concentration. We previously compared the effect (using mass- and metabolic-based methods) of PA, dissolved in ethanol or bound to albumin, on PAV-1 cell line proliferation (data not shown). Both forms of PA administration were efficient for HSC proliferation, but we observed a less potent effect of PA dissolved in albumin (albumin/palmitic acid ratio=4/1). The decrease in DNA synthesis induced by PA observed in our study could be the result of growth arrest and/or apoptosis. We clearly demonstrated using two different methods (FACS and image analysis) that PA induces growth arrest of PAV-1 cells. This biological effect was already observed in an insulin-secreting cell line, presenting important growth inhibition (48% of control growth) induced by 50 μM PA [52]. Kliewer et al. [53] previously demonstrated that PPAR-α and -γ are activated by fatty acids including PA. The PPAR-γ ligand troglitazone induces cell cycle arrest of hepatocellular carcinoma cell lines [54]. Thus, pPA could induce growth arrest by activating PPAR-γ, which we found to be expressed in the PAV-1 cell line (preliminary results). An alternative cellular pathway for PA to induce growth arrest in the PAV-1 cell line could be an increase in the concentration of ceramide [55]. Indeed, C6-ceramide can induce cell cycle arrest in MOLT-4 leukemia cells by dephosphorylating the Retinoblastoma gene product (Rb) [56]. The effect of PA on the ceramide pathway needs further biological explorations. No evident apoptosis was observed using morphology. MTT test did not show any effect on viability when we incubated Rol and PA for 24 hr with PAV-1 cells. Moreover, the apoptotic peak before G1 phase cells was not detected by flow cytometry. The effect of palmitic acid on apoptosis induction seems to be cellular dependent. It could induce apoptosis in different type cells (hepatocellular cancer line and pancreatic ß cells) [54, 55] but not in Caco-2 cells [57] or primary fibroblasts [58].
Several authors have studied the effect of Rol and retinoic acid on HSC proliferation but the results were controversial [39, 43–45]. Davis et al. [39] have shown that HSCs treated with 0.1 μM Rol present decreased proliferation. Sato et al. [45], using activated HSCs, found no decrease in DNA content in cells treated with 1 to 25 μM retinol. No proliferation modification was observed in the PAV-1 cell line treated with a physiological level of vitamin A (2 μM). It has been shown that the sensitivity of stellate cells to retinoic acid decreases with the number of passages [42]. The state of differentiation could also explain the differences observed between the different studies. However, the GRX cell line, which also has a myofibroblastic-like phenotype, responds to Rol [44]. Variable conditions of culture (plastic versus collagen, physiological or pharmacological retinol concentrations, presence or absence of serum in the medium) and specific expression patterns of retinoic acid receptors, RAR and RXR, could also explain the differences observed between the previous studies [59–62]. Indeed, RAR-α and RXR-α were expressed in PAV-1 cells [30], compared to the presence of RAR-α, -ß, and -γ and RXR-α and -ß in rat HSC [60].
Retinol induces a decrease in α-SMA expression in PAV-1 cell line after 48 hr of treatment. Using 1 μM all-trans retinoic acid, Davis et al. [42] found no change in the expression of α-SMA on Western blot. Xu et al. [63] have found a down-regulation of α-SMA in skin fibroblasts treated with all-trans retinoic acid in 10% serum and an up-regulation of α-SMA in cells treated without serum. We postulate that fatty acids (more particularly, PA) contained in serum (or under our culture conditions) could modulate the response to retinoic acid. We also showed that PA decreases the expression of α-SMA after 24 hr of treatment. Moreover, the addition of Rol and PA leads to an undetectable expression of α-SMA after 24 hr of treatment, suggesting that Rol and PA have a synergic effect. It has previously been shown [49] that the PPAR-γ ligand ciglitizone down-regulates the expression of α-SMA and decreases the proliferation of human HSCs. Treatment with 9-cis-retinoic acid, the ligand of the RXR (which could form a heterodimer with PPAR-γ), caused a further reduction of proliferation when used with the PPAR-γ ligand ciglitazone. The synergy observed for proliferation between the RXR ligand and the PPAR-γ ligand and the formation of the heterodimer PPAR-γ/RXR-α could explain the synergistic effect on the regulation of the target gene expression, α-SMA. A similar conclusion could be applied to the modulation by Rol and PA of the expression of collagen type I, another well-established marker of the HSC phenotype. We also showed that Rol did not modify the expression of collagen I. Geerts et al. [40] also did not find any effect on collagen expression when cells were treated with Rol. On the contrary, Margis and Sato [44, 45] found a decrease in the expression of collagen. We established that PA reduced collagen I expression and the combination of Rol and PA strongly decreased the expression of collagen I in PAV-1 cells, implicating PPAR-γ/RXR- α (expressed in PAV-1 cells) in this molecular regulation of the target gene. In addition, our results are in accordance with in vivo studies. Several studies have shown that treatment with retinyl palmitate decreases the amount of fibrosis [11, 14, 17, 18], but treatment with Rol alone [64] or with acyclic retinoid [10] induces an increase in fibrosis. Moreover, Andreola et al. [65] showed a decrease in collagen deposition in livers from aryl hydrocarbon receptor null (AHR –/–) mice fed a vitamin A-deficient diet compared to AHR –/– mice fed a diet containing a standard amount of vitamin A.
In conclusion, our study clearly shows that PA decreases PAV-1 proliferation and α-SMA and collagen expression. Synergistic effects were observed between Rol and PA on α-SMA and collagen type 1 expression, suggesting an important role of the heterodimer PPAR-γ /RXR-α in target gene regulation. Based at the cellular and molecular levels, our results support the combined use of Rol and PA to lead to a deactivation of HSCs in terms of liver fibrosis prevention or treatment. Finally, the effect of other fatty acids on HSCs should be studied, as their role could be relevant to the understanding of the pathogenesis of fibrosis induced by liver diseases, in particular, nonalcoholic steatohepatitis.
References
Friedman SL (2000) Molecular regulation of hepatic fibrosis, an integrated cellular response to tissue injury. J Biol Chem 275:2247–2250
Geerts A (2001) History, heterogeneity, developmental biology and functions of quiescent hepatic stellate cells. Semin Liver Dis 21:311–335
Godichaud S, Krisa S, Couronne B, Dubuisson L, Merillon JM, Desmouliere A, Rosenbaum J (2000) Deactivation of cultured human liver myofibroblasts by trans-resveratrol, a grapevine-derived polyphenol. Hepatology 31:922–931
Sohara N, Znoyko I, Levy MT, Trojanowska M, Reuben A (2002) Reversal of activation of human myofibroblast-like cells by culture on a basement membrane-like substrate. J Hepatol 37:214–221
Bennett R, Kharbanda K, Tuma D (2003) Inhibition of markers of hepatic stellate cell activation by the hormone relaxin. Biochem Pharmacol 66:867–874
Russell RM, Boyer JL, Bagheri SA, Hruban Z (1974) Hepatic injury from chronic hypervitaminosis A resulting in portal hypertension and ascites. N Engl J Med 291:435–440
Geubel AP, De Galocsy C, Alves N, Rahier J, Dive C (1991) Liver damage caused by therapeutic vitamin A administration: estimate of dose related toxicity in 41 cases. Gastroenterology 100:1701–1709
Jorens PG, Michielsen PP, Pelckmans PA, Fevery J, Desmet V, Geubels AP, Rahier J, Van Maercke YM (1992) Vitamin A abuse: development of cirrhosis despite cessation of vitamin A. A six-year clinical and histopathologic follow-up. Liver 12:381–386
Kowalski TE, Falestiny M, Furth E, Malet PF (1994) Vitamin A hepatotoxicity: a cautionary note regarding 25,000 IU supplements. Am J Med 97:523–528
Okuno M, Moriwaki H, Imai S, Muto Y, Kawada N, Suzuki Y, Kojima S (1997) Retinoids exacerbate rat liver fibrosis by inducing the activation of latent TGF-β in liver stellate cells. Hepatology 26:913–921
Senoo H, Wake K (1985) Suppression of experimental hepatic fibrosis by administration of vitamin A. Lab Invest 52:182–194
Shiratori Y, Ichida T, Geerts A, Wisse E (1987) Modulation of collagen synthesis by fat-storing cells, isolated from CCl4- or vitamin A-treated rats. Dig Dis Sci 32:1281–1289
Seifert WF, Bosma A, Hendriks HFJ, De Ruiter GCF, Van Leeuwen REW, Knook DL, Brouwer A (1989) Dual role of vitamin A in experimentally induced liver fibrosis. In: Wisse E, Knook DL, Decker K (eds) Cells of the hepatic sinisoids 2. The Kupffer Cell Foundation, Rijswijk, the Netherlands, pp 43–48
Parise E, Chehter L, Nogueira M, Leite-Mor M, Tersariol I, Michelacci Y, Nader H (1992) Effects of vitamin A administration on collagen and sulfated glycosaminoglycans contents in the livers of rats with carbon tetrachloride. J Lab Clin Med 119:676–681
Seifert W, Bosma A, Brouwer A, Hendriks H, Boholl P, van Leeuwen R, van Thiel-de Ruiter, Seifert-Bock I, Knook D (1994) Vitamin A deficiency potentiates carbon tetrachloride-induced liver fibrosis in rats. Hepatology 19:193–201
Seifert WF, Bosma A, Hendriks HFJ, Van Leeuwen REW, Van Thiel-de Ruiter GCF, Seifert-Bock I, Knook DL, Brouwer A (1995) Beta-carotene (provitamin A) decreases the severity of CCl4-induced hepatic inflammation and fibrosis in rat. Liver 15:1–8
Mizobuchi Y, Shimizu I, Yasuda M, Hori H, Shono M, Ito S (1998) Retnyl palmitate reduces hepatic fibrosis in rats induced dimethylnitrosamine or pig serum. J Hepatol 29:933–943
De Freitas Junior S, Bustorff-Silva JM, Castro e Silva Junior O, Jorge Gde L, Leonardi LS (2003) Retinyl-palmitate reduces liver fibrosis induced by biliary obstruction in rats. Hepatogastroenterology 50:146–150
Okuno M, Muto Y, Moriwaki H, Kato M, Noma A, Tagaya O, Nozaki Y, Suzuki Y (1990) Inhibitory effect of acyclic retinoid on hepatic fibrosis in CCl4 treated-rats. Gastroenterol Jpn 25:223–229
Vollmar B, Heckmann C, Richter S, Menger M (2002) High, but not low, dietary retinoids aggravate manifestation of rat liver fibrosis. J Gastroenterol Hepatol 17:791–99
Leo MA, Lieber CS (1999) Alcohol, vitamin A, and β-carotene: adverse interactions, including hepatotoxicity and carcinogenicity. Am J Clin Nutr 69:1071–1085
Okuno M, Kojima S, Akita K, Matsushima-Nishiwaki R, Adachi S, Sano T, Takano Y, Takai K, Obora A, Yasuda I, Shiratori Y, Okano Y, Shimada J, Suzuki Y, Muto Y, Moriwaki H (2002) Retinoids in liver fibrosis and cancer. Front Biosci 7:204–218
Borojevic R, Monteiro AN, Vinhas SA, Domont GB, Mourao PA, Emonard H, Grimaldi G Jr, Grimaud JA (1985) Establishment of a continuous cell line from fibrotic schistosomal granulomas in mice livers. In Vitro Cell Dev Biol 7:382–390
Weill FX, Blazejewski S, Blanc JF (1997) Characterisation of a new human liver myofibroblast cell line: transcriptional regulation of plasminogen activator inhibitor I by transforming growth factor beta 1. Lab Invest 77:63–70
Murakami K, Abe T, Miyazawa M, Yamaguchi M, Masuda T, Matsuura T, Nagamori S, Takeuchi K, Abe K, Kyogoku M (1995) Establishment of a new human cell line, LI 90, exhibiting characteristics of hepatic Ito (fat-storing) cells. Lab Invest 72:731–739
Schnabl B, Choi YH, Olsen JC, Hagedom CH, Brenner DA (2002) Immortal activated human hepatic stellate cells generated by ectopic telomerase expression. Lab Invest 82:223–232
Xu L, Hui A, Arthur MJ, O’Byrne SM, Blaner WS, Mukherjee P, Friedman SL, Eng FJ (2005) Human hepatic stellate cell lines, LX-1 and LX-2: new tools for analysis of hepatic fibrosis. Gut 54:142–151
Greenwel P, Schwartz M, Rosas M, Peyrol S, Grimaud JA, Rojkind M (1991) Characterization of fat-storing cell lines derived from normal and CCl4-cirrhotic livers. Differences in the production of interleukin-6. Lab Invest 65:644–653
Greenwel P, Rubin J, Schwartz M, Hertzberg EL, Rojkind M (1993) Liver fat-storing cell clones obtained from a CCl4-cirrhotic rat are heterogeneous with regard to proliferation, expression of extracellular matrix components, interleukin-6 and connexin 43. Lab Invest 69:210–216
Sauvant P, Sapin V, Abergel A, Schmidt CK, Blanchon L, Alexandre-Gouabau MC, Rosenbaum J, Bommelaer G, Rock E, Dastugue B, Nau H, Azaïs-Braesco V (2002) PAV-1, a new rat hepatic stellate cell line converts retinol into retinoic acid, a process altered by ethanol. Int J Biochem Cell Biol 34:1017–1029
Vogel S, Piantedosi R, Frank J, Lalazar A, Rockey DC, Friedman SL, Blaner WS (2000) An immortalized rat liver stellate cell line (HSC-T6): a new cell model for the study of retinoid metabolism in vitro. J Lipid Res 41:882–893
Sauvant P, Abergel A, Partier A, Alexandre-Gouabau MC, Rock E, Sion B, Motta C, Sapin V, Azaïs-Braesco V (2002) Treatment of the rat hepatic stellate cell line, PAV-1, by retinol and palmitic acid leads to a convenient model to study retinoids metabolism. Biol Cell 94:401–408
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Lowry OH, Rosebrough NJ, Frazer AL, Randall RJ (1951) Protein measurement with Folin phenol reagent. J Biol Chem 193:265–275
Labarca C, Paigen K (1980) A simple and sensitive DNA assay procedure. Anal Biochem. 102:344–352
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680–685
Towbin H, Staehlin T, Gordon J (1979) Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: Procedure and some applications. Proc Natl Acad Sci USA 166:209–214
Troen G, Nilsson A, Norum K, Blomhoff R (1994) Characterization of liver stellate cell retinyl ester storage. Biochem J 300:793–798
Davis B, Vucic A (1988) The effect of retinol on Ito cell proliferation in vitro. Hepatology 8:788–793
Geerts A, Vrijsen R, Schellinck P, Wisse E (1989) Retinol affects the phenotype and protein synthesis of fat-storing cell derived myofibroblasts in vitro. In: Wisse E, Knook DL, Decker K (eds) Cells of the hepatic sinusoids 2. The Kupffer Cell Foundation, Rijswijk, the Netherlands, pp 20–24
Davis B, Kramer R, Davidson N (1990) Retinoic acid modulates rat Ito cell proliferation, collagen, and transforming growth factor beta production. J Clin Invest 86:2062–2070
Davis B, Rapp U, Davidson N (1991) Retinoic acid and trnsforming growth factor beta differentially inhibit platelet-derived-growth-factor-induced Ito-cell activation. Biochem J 278:43–47
Pinzani M, Gentilini P, Abboud H (1992) Phenotypical modulation of liver fat-storing cells by retinoids. J Hepatol 14:211–220
Margis R, Pinheiro-Margis M, da Silva LC, Borojevic R (1992) Effects of retinol on proliferation, cell adherence and extracellular matrix synthesis in a liver myofibroblast or lipocyte cell line (GRX). Int J Exp Pathol 73:125–135
Sato S, Kato R, Tyson C (1995) Regulation of differentiated phenotype on rat lipocytes by retinoids in primary culture. Exp Cell Res 217:72–83
Okuno M, Sato T, Kitamoto T, et al. (1999) Increased 9,13-di-cis-retinoic acid in rat hepatic fibrosis: implication for a potential link between retinoid loss and TGF-beta mediated fibrogenesis in vivo. J Hepatol 30:1073–1080
Hellemans K, Grinko I, Rombouts K, Schuppan D, Geerts A (1999) All-trans and 9-cis retinoic acid alter rat hepatic stellate cell phenotype differentially. Gut 45:134–142
Huang G, Zhang J, Zhang Y (2000) Effects of retinoic acid on proliferation, phenotype and expression of cyclin-dependent kinase inhibitors in TGF-beta 1-stimulated rat hepatic stellate cells. World J Gastroenterol 6:819–823
Galli A, Crabb D, Price D, Ceni E, Salzano R, Surrenti C, Casini A (2000) Peroxisome Proliferator activated receptor gamma transcriptional regulation is involved in PDGF-induced proliferation of human hepatic stellate cells. Hepatology 31:101–108
Hellemans K, Michalik L, Dittie A, Knorr A, Rombouts K, De Jong J, Heirman C, Quartier E, Schuit F, Walter W, Geerts A (2003) PPAR-beta signaling contributes to enhanced proliferation of hepatic stellate cells. Gastroenterology 124:184–201
Tronstad K, Berge K, Flindt E, Kristiansen K, Berge R (2001) Optimization of methods and treatment conditions of fatty acids on cell growth. Lipids 36:305–313
Beeharry N, Lowe J, Hernandes A, Chambers J, Fucassi F, Cragg P, Green M, Green I (2003) Linoleic acid and antioxidants protect against DNA damage and apoptosis induced by palmitic acid. Mutation Res 530:27–33
Kliewer S, Sundseth S, Jones S, Brown P, Wisely B, Koble C, Devchand P, Walter W, Willson T, Lenhard J, Lehmamm J (1997) Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors alpha and gamma. Proc Natl Acad Sci USA 94:4318–4323
Yoshizawa K, Cioca D, Kawa S, Tanaka E, Kiyosawa K (2002) Peroxisome proliferator-activated receptor gamma ligand troglitazone induces cycle arrest and apoptosis of hepatocellular carcinoma cell lines. Cancer 95:2243–2251
Maedler K, Spinas GA, Dyntar D, Moritz W, Kaiser N, Donath M (2001) Distinct effects of satured and monounsatured fatty acids on beta-cell turnover and function. Diabetes 50:69–76
Mathias S, Peña L, Kolesnick R (1998) Signal transduction of stress via ceramide. Biochem J 335:465–480
Nano JL, Nobili C, Girard-Pipau F, Rampal P (2003) Effects of fatty acids on the growth of Caco-2 cells. Prostag Leukotr Ess Fatty Acids 69:207–215
Petit-frere C, Capulas E, Lyon D, Norbury C, Lowe J, Clingen P, Riballo E, Green M, Arlett C (2000) Apoptosis and cytokine release induced by ionizing or ultraviolet B radiation in primary and im-mortalized human keratinocytes. Carcinogenesis 21:1087–1095
Weiner F, Blaner W, Czaja M, Shah A, Geerts A (1992) Ito cell expression of a nucleic acid receptor. Hepatology 15:336–342
Ohata M, Lin M, Satre M, Tsukamoto H (1997) Diminished retinoic acid signaling in hepatic stellate cells in cholestatic liver disease. Am J Physiol 272:G589–G596
Imai S, Okuno M, Moriwaki H, Muto Y, Murakami K, Shudo K, Suzuki Y, Kojima S (1997) 9,13-Di-cis retinoic acid induces the production of tPA and activation of latent TGF-beta via RAR alpha in a human liver stellate cell line, LI 90. FEBS Lett 411:102–106
Ulven SM, Natarajan V, Holven KB, Lovdal T, Berg T, Blomhoff R (1998) Expression of retinoic acid receptor and retinoid X receptor subtypes in rat liver cells: implications for retinoid signalling in parenchymal, endothelial, Kupffer and stellate cells. Eur J Cell Biol 77:111–116
Xu G, Bochaton-Piallat ML, Andreutti D, Low R, Gabbiani G, Neuville P (2001) Regulation of alpha-smooth muscle actin and CRBP-1 expression by retinoic acid and TGF-beta in cultured fibroblasts. J Cell Physiol 187:315–325
Hellemans K, Rombouts K, Quartier E, Dittie A, Knorr A, Michalik L, Rogiers V, Schuit F, Walter W, Geerts A (2003) PPAR-beta regulates vitamin A metabolism-related expression in hepatic stellate cells undergoing activation. J Lipid Res 44:280–295
Andreola F, Calvisis D, Elizondo G, Jakowlew S, Mariano J, Gonzalez F, De Luca L (2004) Reversal of liver fibrosis in aryl hydrocarbon receptor null mice by dietary vitamin A depletion. Hepatology 39:157–166
Acknowledgment
We thank Alexis Desmoulières (Bordeaux, France) for reviewing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abergel, A., Sapin, V., Dif, N. et al. Growth Arrest and Decrease of α-SMA and Type I Collagen Expression by Palmitic Acid in the Rat Hepatic Stellate Cell Line PAV-1. Dig Dis Sci 51, 986–995 (2006). https://doi.org/10.1007/s10620-005-9031-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-005-9031-y