Abstract
Sterilisation of allografts are a crucial step in ensuring safety and viability. Current sterilisation standards such as 25 kGy gamma irradiation (γ) can have adverse effects on the ultrastructure and biomechanical properties of allograft tissue. Supercritical CO2 (SCCO2) technology, represents an improved sterilisation process that potentially preserves tissue properties. This study aimed to test the effect of SCCO2 sterilisation on the biomechanical and histological properties of the meniscus and compare this to the current standard of γ. Thirty-two 18-month old ovine menisci were randomly assigned into three groups for sterilisation (SCCO2, γ and control). After treatment, biomechanical indentation testing (stiffness and stress relaxation) or histological analysis [percentage of void, cells and extracellular matrix (ECM) per slide] was undertaken. Both SCCO2 and gamma groups displayed an increase in stiffness and stress relaxation as compared to control, however, this difference was lesser in samples treated with SCCO2. No significant histological quantitative differences were detected between SCCO2 and control specimens. Gamma-treated samples demonstrated a significant increase in void and decrease in ECM. Interestingly, both treatment groups demonstrated a decreasing mean void and increasing ECM percentage when analysed from outer to inner zones. No significant differences were detected in all-endpoints when analysed by section. SCCO2 sterilisation represents a potential feasible alternative to existing sterilization techniques such as γ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The menisci of the knee are two C-shaped wedges of fibrocartilage secured onto the tibial surface. They are crucial to the healthy operation of the knee joint (Brindle et al. 2001; Harner and Lo 2009). Current treatments for meniscal tears in the avascular, inner “white zone” in the knee are ineffective, as first line treatments such as partial meniscectomy can lead to degeneration and osteoarthritis (Englund et al. 2012; Lee et al. 2012). Meniscal allograft transplantation (MAT) is an emerging technique which has had promising results (Lubowitz et al. 2007; Rijk 2004; Stone et al. 2010; Verdonk et al. 2005).
Sterilisation of allografts are a crucial step in ensuring safety and viability. Sterilization is defined as the process of killing all forms of life, especially microorganisms (McAllister et al. 2007). It is measured as a sterility assurance level (SAL) of 10−6, or SAL−6, meaning there is less than 1 in 1,000,000 chance of a contaminating organism surviving the treatment (TGA 2011; Vangsness and Dellamaggiora 2009; White et al. 2006). The ability of connective tissue allografts, including menisci, to transmit disease is well documented (Ireland and Spelman 2005; McAllister et al. 2007; Nemzek et al. 1994). Whilst the incidence of confirmed donor-derived infection from allograft is low, 0.00015 % (Vangsness and Dellamaggiora 2009), transmission of microbes such as human immunodeficiency virus (HIV), hepatitis C virus, bacteria and prions remains a concern since (1) MAT is not a life-saving procedure and (2) the high volume of surgeries represents a large potential burden (McNickle et al. 2009; Rijk 2004).
Recently, a review article by Mickiewicz et al. (2014) analysed the sterilisation methods available for MAT. However many are unsuitable for MAT due to adverse graft or clinical effects (Lee et al. 2012). The industry standard for terminal sterilisation, γ, is effective against bacteria and viruses and penetrates whole tissues (Russell et al. 2012b; Vaishnav et al. 2009; Vangsness and Dellamaggiora 2009). However, dosages of radiation required to kill viruses cause deleterious changes in allograft mechanical properties, including stiffness, tensile strength and elastic response (Campbell and Li 1999; Vangsness and Dellamaggiora 2009). Many surgeons still have concerns about the tissue quality and biomechanical properties related to gamma sterilisation (McAllister et al. 2007) and a sterilisation method that preserves the mechanical and biological performance of meniscal allograft is necessary.
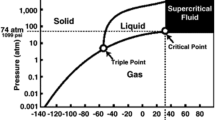
Supercritical CO2 (SCCO2) technology represents a potentially improved sterilisation process that preserves tissue properties (Cinquemani et al. 2007; Fages et al. 1998; Mun et al. 2011; Russell et al. 2012b; Tarafa et al. 2010; White et al. 2006; Zhang et al. 2006). At relatively low pressures and temperatures (Fig. 1) SCCO2’s properties allow it to act as an organic solvent; dissolve materials into their component parts; and deeply penetrate tissue (Brunner 2005). Whilst the chemical, industrial and food industries have used this technology to extract valuable materials from solid substrates for the last two decades, it is only recently that they have been applied to medical devices (Kim et al. 2013; Tarafa et al. 2010). Recently, laboratories have been able to deactivate spores and viruses by dissolving sterilants such as peracetic acid and hydrogen peroxide into SCCO2, ensuring SAL 10−6 sterility of tissues (Christensen et al. 2004; Furukawa et al. 2009; Melo Silva et al. 2013; Perrut 2012; Russell et al. 2012b; Zhang et al. 2006). In view of these findings, this study aims to test the effect of SCCO2 sterilization on the biomechanical and histological properties of the meniscus and compare this to the current standard of gamma irradiation (γ). Our null hypothesis was that menisci treated with SCCO2 will have no significant differences in histological and/or biomechanical properties to native controls.
Phase diagram of carbon dioxide, demonstrating critical point (White et al. 2006)
Materials and methods
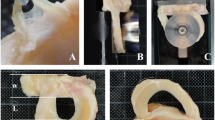
Thirty-two 18-month old ovine menisci were harvested from recently euthanized 18 month old wethers. The sheep were from ethically approved studies that did not involve the hind or forelimbs, and where movement was not impaired. The ovine model was chosen for its anatomical similarity to the human meniscus (Chevrier et al. 2009; Proffen et al. 2012). After trimming excess connective tissue, the menisci were studied macroscopically for any traumatic or degenerative changes and weighed. Only menisci with intact cartilage and meniscal surfaces were investigated. Selected samples were randomly divided into three groups (SCCO2, γ and control), kept moist by wrapping in PBS soaked gauze, and frozen for storage at −20 °C until treatment. Non-treated control specimens were thawed, weighed and proceeded straight to the testing stage. Specimens in gamma irradiated group were sent to an external laboratory for irradiation at 25 kGy using a cobalt irradiation source under well-defined operating procedures (Steritech Wetherill Park, Australia). Samples were placed on dry ice and sealed in a styrofoam box to maintain temperatures during treatment between −20 and −50 °C. Samples were thawed at room temperature for testing. The SCCO2 group menisci were thawed and treated whole with an in-house supercritical fluid set-up (Fig. 2) and the Novasterilis© Supercritical CO2 sterilisation protocol proven to reach SAL−6. Our protocol isolated the effect of SCCO2 treatment, independent of common allograft cleaning and washing techniques, with the goal of evaluating the mechanical and histological effect of SCCO2 when utilized as a terminal sterilization methodology.
Biomechanical testing and histological testing of each group was undertaken (Fig. 3). Each testing method utilised a different sampling method. For the biomechanical section of the protocol, one core was taken from the anterior, middle and posterior sections of each meniscus using a 6 mm dermal core biopsy punch (Stiefl, United Kingdom), resulting in three cores per meniscus. A scalpel blade was used to square off the sloped meniscal surface of each core, resulting in dowels of approximately 1.5 mm in height. Heights were recorded using a digital caliper.
The viscoelastic properties of the menisci were examined based on Maier et al. (2007) that allowed reliable measurement of stiffness and stress relaxation. Samples were tested via minimally constraint cyclic indentation tests in displacement control. The investigators used a Mach-1 Micromechanical Tester (Biomentum, Canada), with a steel ball-bearing 3 mm in diameter, which avoided notch effects and stress concentrations. Meniscal samples were placed horizontally on a smooth and flat metallic circular sink (diameter 6 mm, depth 0.1 mm) to achieve lateral stabilisation during axial loading as described (Maier et al. 2007). The meniscus samples were kept moist throughout testing using a phosphate buffer saline (PBS) bath. Calibration of the indenter position and load occurred prior to the testing of each sample. The specific protocol involved four phases: (1) Preloading of the sample to 0.5 N; (2) Ramp compression in displacement control by 10 % of the height of the sample at a rate of 83.33 μm/s; (3) Stress relaxation for 60 s; (4) Retraction of the actuator. The four phases were repeated for a total of 5 times to simulate physiologic stress.
The stiffness defined as the resistance to deformation (N/mm) under the applied force was determined from the gradient of the linear elastic region on the load–displacement curve. Stress relaxation was calculated from the difference in maximum and minimum load over the 60 s stress relaxation period. The data for each repetition of the protocol was averaged within each specimen.
For histology sampling one cross-sectional wedge was taken from the anterior, middle and posterior sections of each meniscus, resulting in three wedges per meniscus. Wedges were fixed in formalin for at least 1 week and processed for routine paraffin histology and haematoxylin and eosin (H&E) staining. Tissue organisation was analysed qualitatively in inner, middle and outer thirds (zones), as well as between anterior, middle and posterior samples (sections), resulting in two representative photos per zone, per section taken for quantitative analysis. Quantitative endpoints were calculated using an in-house histomorphometry program, specifically focusing on the percentage of dead space, cells and extracellular matrix (ECM). Mechanical and histological data was processed using SPSS 21.0 Software (SPSS Inc, IL, USA). A univariate analysis with Tukey’s post hoc test was used to detect differences between groups.
Results
The SCCO2 and gamma irradiated (γ) groups displayed an increase in stiffness and stress relaxation compared to control, however, this difference was lesser in samples treated with SCCO2 (Fig. 4). The mean stiffness of samples in the treated groups [SCCO2 (2.21 g/μm), γ (2.50 g/μm)] were found to be greater than control [1.68 g/μm] (P < 0.05). Similar results were demonstrated in stress relaxation, whereby the mean stress relaxation of treated samples [SCCO2 (299.8 g/s), γ (407.8 g/s)] were recorded significantly greater than control [223.0 g/s] (P < 0.05). Control meniscal specimens, demonstrated no significant differences in stiffness or stress relaxation between cycles (P > 0.05). Conversely, in both SCCO2 and γ groups, significant increases were detected in stiffness [SCCO2 (P < 0.01), γ (P < 0.05)] (Fig. 5). Specifically, statistically significant differences were detected between the first cycle and fourth cycle (SCCO2: 1.36 g/μm, γ: 1.43 g/μm) and first cycle and fifth cycle (SCCO2: 1.32 g/μm, gamma: 1.37 g/μm). These differences were greater in specimens treated with γ than SCCO2, with an 18.9 % increase when analysing first and fourth cycles and 10.7 % increase when analysing first and fifth cycles. No significant differences were detected [SCCO2 (P = 0.08), γ (P = 0.06)] for stress relaxation between groups. No significant difference was detected between anterior, middle and posterior sections when analysed by treatment type (P > 0.05).
Histologically, control samples demonstrated normal extracellular and cellular architecture, as compared to the literature. SCCO2 treated samples demonstrated similar tissue organisation to control, with added areas of “smoothed” collagen (dotted arrow) and “bubble” voids (black arrow) (Fig. 6). Conversely, organisation of tissue was markedly disrupted in the γ group with cellular debris noted (circles) and increased void. No significant differences were detected between the control and SCCO2 groups in all quantitative histological endpoints: namely percentage void, percentage cells and percentage ECM. Conversely, γ irradiated samples demonstrated a significant increase in percentage void [γ (20.5 %), control (10.9 %)] and significant decrease in ECM [γ (79.3 %), control (89.1 %)] in comparison to control (P < 0.01) (Fig. 7).
By zone, a number of significant relationships were revealed (Fig. 8). Regarding percentage void, all groups displayed significant differences between zones (P < 0.01), with a trend for decreasing percentage void when analysed from outer to inner zones. Zonal analysis in ECM percentage identified a reversed trend whereby outer zones contained less ECM than middle zones, which contained less than inner zones, in all three groups studied. Quantitative cellular analysis revealed no significant differences between zones. No significant differences were detected in all endpoints when analysed by section.
Discussion
Improved allograft sterilisation has become an increasingly important area of research, due to a number of limitations with current best practice (Mickiewicz et al. (2014). It is well documented that at doses required for sterilisation (commonly 25 kGy) γ adversely affects the biomechanical and biological properties of allografts in an additive and dose-dependent manner (Akkus et al. 2005; Cheung et al. 1990; Grieb et al. 2006; Naal et al. 2008; Vaishnav et al. 2009). Gamma irradiated tissue results were consistent with the literature reports that purport excess free radical production resulting in tissue damage (Cheung et al. 1990; McAllister et al. 2007; Vaishnav et al. 2009). Specifically these demonstrated histological qualitative disruption of collagen ultrastructure and quantitative increase in percentage void and decrease in percentage ECM, compounded by significantly higher stiffness and stress relaxation in gamma irradiated tissue as compared to control.
Previous studies in SCCO2 sterilisation have demonstrated less disruption of tissue in SCCO2 groups compared to gamma irradiated specimens with no significant differences between SCCO2 and Control groups (Nichols et al. 2009; Russell et al. 2012a, b). However, these studies utilised sterilization in tendon and bone, and cannot be transferred directly due to the unique properties of meniscal tissue (Adams and Hukins 1992; Brindle et al. 2001). To our knowledge there are no studies investigating biomechanical and histological effects of SCCO2 in meniscal tissue.
SCCO2 sterilisation does have an effect on the biomechanical properties of the meniscus, however these effects are lessened as compared to γ of meniscal tissue. Significant difference was not established and it is likely that more samples are required. Histologically, no significant differences were observed. This may translate to in vivo benefits including improved performance of the graft after transplantation in the short, medium and long-term. In addition to a reduction in biomechanical deficits in sterilisation, there are a number of other benefits to the use of SCCO2 sterilisation over γ. SCCO2 has significant expediency for allograft processing and sterilization due to its unique properties, extraction potential and efficacy in killing spores and viruses (e.g. Adenovirus, HIV) in musculoskeletal tissues (Perrut 2012; Qiu et al. 2009). SAL−6 terminal sterilisation has been demonstrated in SCCO2, putting the sterilisation effectiveness at least on par with existing methods. This method, with its lack of ionising radiation is advantageous from a safety perspective being non flammable, non toxic, chemically inert and physiologically safe (Tarafa et al. 2010; White et al. 2006). This is mirrored from the point of view of manufacturing staff as well as the community at large through lack of radioactive waste.
Additionally, SCCO2 technology has been proposed in the literature as a “green alternative” (Perrut 2012), given the availability of CO2, which may rise further due to the implementation of CO2 recapture systems. From an economic point of view, SCCO2 potentially represents a significant cost saving through the availability of CO2, its mild critical temperature, and importantly, the ability to utilise the technology on-site, for example, in tissue banks themselves, saving money on transport costs to sterilisation plants which would have been associated with γ.
Previous studies in allograft bone are consistent in noting less disruption of tissue (measured biomechanically and histologically) in SCCO2 specimens as compared to γ (Nichols et al. 2009; Russell et al. 2012b). However, it appears that SCCO2 is more gentle in bone, as no significant biomechanical differences were detected between SCCO2 bone grafts and control in a previous study (Russell et al. 2012a, b). It is encouraging that the overall collagen organisation was intact in the SCCO2 group, as compared to the gamma treated group in our qualitative study. The presence of “bubble” voids can be explained by the properties of SCCO2 treatment, which has been shown to have the potential to induce porosity, nucleation and cracking in various polymers (Barry et al. 2006; Kim et al. 2013; Tarafa et al. 2010) particularly during depressurization. Our histological void percentage results are consistent with this notion. Logically, an increase in void should be correlated with a decrease in ECM, which was quantitatively observed in both treatment groups. The biomechanical increase in stiffness and stress-relaxation in the SCCO2 group is likely a result of these structural changes. Therefore, by decreasing the rate of depressurisation, we hypothesise lesser incidence of “bubble voids”, lesser structural changes and lesser differences in compressive properties as compared to control. Conversely, this finding may open another unforseen avenue in allografts: scaffold creation. SCCO2 treatment has been used to create scaffolds in polymers (Kim et al. 2013). It has been hypothesised that this same technology can create effective scaffolds in tissue to sustain in vitro cell adhesion and proliferation for possible applications in tissue engineering and regenerative medicine (Barry et al. 2006; Kim et al. 2013; Sandmann et al. 2009; Temtem et al. 2009). Our SCCO2-treated meniscal samples contain larger porosities which we speculate have the potential for infiltration after implantation.
The observation of no significant differences between anterior, middle and posterior sections in both SCCO2 and gamma treatment groups encourages the theory that both sterilisation modalities penetrate these sections equally. It is important to take these results in light of their limitations. Whilst it would have been more accurate to use human menisci, the ovine model was deemed most appropriate for our uses. Due to ethical reasons, human tissue for sterilisation studies is either procured from cadavers in tissue banks or total knee replacements (Lewis et al. 2008; Vangsness et al. 2003). Donors from both of these sources are aged and often have comorbid OA, especially in the latter. Since osteoarthritis can cause degenerative tears of the meniscus (Englund et al. 2009, 2012), and the environment itself decreases their ability to heal (Fernandes et al. 2002; Wilusz et al. 2008), there are limitations to the usefulness of these studies. By using an animal model, we were able to procure menisci that were representative of skeletally mature, healthy adults in plentiful supply.
The SCCO2 sterilisation protocol was adopted from the proprietary Novasterilis protocol, which was originally designed for bone. Our results demonstrate that the meniscus is able to withstand the rigors of such a technique. However, given the structural differences between bone and the menisci, sterility cannot be guaranteed. The cyclic biomechanical testing procedure was adopted to simulate physiological loading conditions as used widely in the literature (Maier et al. 2007; McNickle et al. 2009; Naal et al. 2008). However, there were several methodological limitations. It would have been more accurate to test the whole meniscus rather than cores of tissue, however there were pragmatic concerns. Further, menisci were cut to approximate parallel planes in relation to the undersurface i.e. the distal part of the meniscus, and thus there was some heterogeneity of the compressive surface.
Conclusion
SCCO2 sterilisation represents a potential gentle alternative to existing sterilization techniques such as γ. Our results demonstrate that the meniscus can stand rigors of SCCO2 based end sterilisation techniques for bone, displaying lesser biomechanical deficits than the standard gamma irradiated treatment, and no significant quantitative histological differences compared to control. Further testing with immunohistochemistry, comparative testing with human menisci, sterility testing of the current protocol in menisci, and larger sample sizes are warranted.
References
Adams M, Hukins D (1992) The extracellular matrix of the meniscus. In: Mow VC, Arnoczky SP, Jackson DW (eds) Knee meniscus: basic and clinical foundations. Raven Press, New York
Akkus O, Belaney RM, Das P (2005) Free radical scavenging alleviates the biomechanical impairment of gamma radiation sterilized bone tissue. J Orthop Res 23:838–845. doi:10.1016/j.orthres.2005.01.007
Barry JJ, Silva MM, Popov VK, Shakesheff KM, Howdle SM (2006) Supercritical carbon dioxide: putting the fizz into biomaterials. Philos Trans Ser A Math Phys Eng Sci 364:249–261. doi:10.1098/rsta.2005.1687
Brindle T, Nyland J, Johnson DL (2001) The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train 36:160–169
Brunner G (2005) Supercritical fluids: technology and application to food processing. J Food Eng 67:21–33. doi:10.1016/j.jfoodeng.2004.05.060
Campbell DG, Li P (1999) Sterilization of HIV with irradiation: relevance to infected bone allografts. Aust N Z J Surg 69:517–521
Cheung DT, Perelman N, Tong D, Nimni ME (1990) The effect of gamma-irradiation on collagen molecules, isolated alpha-chains, and crosslinked native fibers. J Biomed Mater Res 24:581–589. doi:10.1002/jbm.820240505
Chevrier A, Nelea M, Hurtig MB, Hoemann CD, Buschmann MD (2009) Meniscus structure in human, sheep, and rabbit for animal models of meniscus repair. J Orthop Res 27:1197–1203. doi:10.1002/jor.20869
Christensen TW, Burns D, White A, Ganem B, Eisenhunt A (2004) Sterilization methods and apparatus which employ additive-containing supercritical carbon dioxide sterilant. US 7108832 B2, 2006
Cinquemani C, Boyle C, Bach E, Schollmeyer E (2007) Inactivation of microbes using compressed carbon dioxide: an environmentally sound disinfection process for medical fabrics. J Supercrit Fluids 42:392–397. doi:10.1016/j.supflu.2006.11.001
Englund M, Guermazi A, Lohmander SL (2009) The role of the meniscus in knee osteoarthritis: a cause or consequence? Radiol Clin N Am 47:703–712. doi:10.1016/j.rcl.2009.03.003
Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A (2012) Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol 8:412–419. doi:10.1038/nrrheum.2012.69
Fages J et al (1998) Viral inactivation of human bone tissue using supercritical fluid extraction. ASAIO J 44:289–293
Fernandes JC, Martel-Pelletier J, Pelletier JP (2002) The role of cytokines in osteoarthritis pathophysiology. Biorheology 39:237–246
Furukawa S, Watanabe T, Koyama T, Hirata J, Narisawa N, Ogihara H, Yamasaki M (2009) Inactivation of food poisoning bacteria and Geobacillus stearothermophilus spores by high pressure carbon dioxide treatment. Food Control 20:53–58. doi:10.1016/j.foodcont.2008.02.002
Grieb TA et al (2006) High-dose gamma irradiation for soft tissue allografts: high margin of safety with biomechanical integrity. J Orthop Res 24:1011–1018. doi:10.1002/jor.20079
Harner CD, Lo MY (2009) Future of allografts in sports medicine. Clin Sports Med 28: 327–340, ix. doi:10.1016/j.csm.2008.10.010
Ireland L, Spelman D (2005) Bacterial contamination of tissue allografts: experiences of the donor tissue bank of Victoria. Cell Tissue Bank 6:181–189. doi:10.1007/s10561-005-7365-5
Kim SH, Jung Y, Kim SH (2013) A biocompatible tissue scaffold produced by supercritical fluid processing for cartilage tissue engineering. Tissue Eng Part C Methods 19:181–188
Lee AS, Kang RW, Kroin E, Verma NN, Cole BJ (2012) Allograft meniscus transplantation. Sports Med Arthrosc 20:106–114. doi:10.1097/Jsa.0b013e318246f005
Lewis PB, Williams JM, Hallab N, Virdi A, Yanke A, Cole BJ (2008) Multiple freeze-thaw cycled meniscal allograft tissue: a biomechanical, biochemical, and histologic analysis. J Orthop Res 26:49–55. doi:10.1002/jor.20473
Lubowitz JH, Verdonk PCM, Reid JB, Verdonk R (2007) Meniscus allograft transplantation: a current concepts review. Knee Surg Sports Traumatol Anthrosc 15:476–492. doi:10.1007/s00167-006-0216-5
Maier D et al (2007) In vitro analysis of an allogenic scaffold for tissue-engineered meniscus replacement. J Orthop Res 25:1598–1608. doi:10.1002/jor.20405
McAllister DR, Joyce MJ, Mann BJ, Vangsness CT Jr (2007) Allograft update: the current status of tissue regulation, procurement, processing, and sterilization. Am J Sports Med 35:2148–2158. doi:10.1177/0363546507308936
McNickle AG, Wang VM, Shewman EF, Cole BJ, Williams JM (2009) Performance of a sterile meniscal allograft in an ovine model. Clin Orthop Relat Res 467:1868–1876. doi:10.1007/s11999-008-0567-y
Melo Silva J, Rigo AA, Dalmolin IA, Debien I, Cansian RL, Oliveira JV, Mazutti MA (2013) Effect of pressure, depressurization rate and pressure cycling on the inactivation of Escherichia coli by supercritical carbon dioxide. Food Control 29:76–81. doi:10.1016/j.foodcont.2012.05.068
Mickiewicz P, Binkowski M, Bursig H, Wrobel Z (2014) Preservation and sterilization methods of the meniscal allografts: literature review. Cell Tissue Bank 15:307–317. doi:10.1007/s10561-013-9396-7
Mun S, Hahn JS, Lee YW, Yoon J (2011) Inactivation behavior of Pseudomonas aeruginosa by supercritical N2O compared to supercritical CO2. Int J Food Microbiol 144:372–378. doi:10.1016/j.ijfoodmicro.2010.10.022
Naal FD, Schauwecker J, Steinhauser E, Milz S, von Knoch F, Mittelmeier W, Diehl P (2008) Biomechanical and immunohistochemical properties of meniscal cartilage after high hydrostatic pressure treatment. J Biomed Mater Res B 87B:19–25. doi:10.1002/Jbm.B.31059
Nemzek JA, Arnoczky SP, Swenson CL (1994) Retroviral transmission by the transplantation of connective-tissue allografts. An experimental study. J Bone Joint Surg Am 76:1036–1041
Nichols A, Burns D, Christopher R (2009) Studies on the sterilization of human bone and tendon musculoskeletal allograft tissue using supercritical carbon dioxide. J Orthop. 6:9–17
Perrut M (2012) Sterilization and virus inactivation by supercritical fluids (a review). J Supercrit Fluids 66:359–371. doi:10.1016/j.supflu.2011.07.007
Proffen BL, McElfresh M, Fleming BC, Murray MM (2012) A comparative anatomical study of the human knee and six animal species. Knee 19:493–499. doi:10.1016/j.knee.2011.07.005
Qiu QQ, Leamy P, Brittingham J, Pomerleau J, Kabaria N, Connor J (2009) Inactivation of bacterial spores and viruses in biological material using supercritical carbon dioxide with sterilant. J Biomed Mater Res B Appl Biomater 91:572–578
Rijk PC (2004) Meniscal allograft transplantation: part I: background, results, graft selection and preservation, and surgical considerations. Arthroscopy 20:728–743. doi:10.1016/j.arthro.2004.06.015
Russell NA, Pelletier MH, Bruce WJ, Walsh WR (2012a) The effect of gamma irradiation on the anisotropy of bovine cortical bone. Med Eng Phys 34:1117–1122. doi:10.1016/j.medengphy.2011.11.021
Russell NA, Rives A, Pelletier MH, Bruce WJ, Walsh WR (2012b) The effect of sterilization on the mechanical properties of intact rabbit humeri in three-point bending, four-point bending and torsion. Cell Tissue Bank. doi:10.1007/s10561-012-9318-0
Sandmann GH et al (2009) Generation and characterization of a human acellular meniscus scaffold for tissue engineering. J Biomed Mater Res A 91:567–574. doi:10.1002/jbm.a.32269
Stone KR, Adelson WS, Pelsis JR, Walgenbach AW, Turek TJ (2010) Long-term survival of concurrent meniscus allograft transplantation and repair of the articular cartilage A PROSPECTIVE TWO- TO 12-YEAR FOLLOW-UP REPORT. J Bone Joint Surg Br 92B:941–948. doi:10.1302/0301-620x.92b7.23182
Tarafa PJ, Jiménez A, Zhang J, Matthews MA (2010) Compressed carbon dioxide (CO2) for decontamination of biomaterials and tissue scaffolds. J Supercrit Fluids 53:192–199
Temtem M et al (2009) Supercritical CO2 generating chitosan devices with controlled morphology. Potential application for drug delivery and mesenchymal stem cell culture. J Supercrit Fluids 48:269–277. doi:10.1016/j.supflu.2008.10.020
TGA (2011) Regulatory life cycle for biologicals that are included on the Australian Register of Therapeutic Goods vol 1.0, 1 edn. Australian Government, Canberra, Australia
Vaishnav S, Thomas Vangsness C Jr, Dellamaggiora R (2009) New techniques in allograft tissue processing. Clin Sports Med 28:127–141
Vangsness CT, Garcia IA, Mills CR, Kainer MA, Roberts MR, Moore TM (2003) Allograft transplantation in the knee: tissue regulation, procurement, processing, and sterilization. Am J Sports Med 31:474–481
Vangsness CT, Jr, Dellamaggiora RD (2009) Current safety sterilization and tissue banking issues for soft tissue allografts. Clin Sports Med. 28:183–189, vii doi:10.1016/j.csm.2008.10.008
Verdonk PCM, Demurie A, Almqvist F, Veys EM, Verbruggen G, Verdonk R (2005) Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am 87A:715–724. doi:10.2106/Jbjs.C.01344
White A, Burns D, Christensen TW (2006) Effective terminal sterilization using supercritical carbon dioxide. J Biotechnol 123:504–515
Wilusz RE, Weinberg JB, Guilak F, McNulty AL (2008) Inhibition of integrative repair of the meniscus following acute exposure to interleukin-1 in vitro. J Orthop Res 26:504–512. doi:10.1002/jor.20538
Zhang J, Davis TA, Matthews MA, Drews MJ, LaBerge M, An YH (2006) Sterilization using high-pressure carbon dioxide. J Supercrit Fluids 38:354–372. doi:10.1016/j.supflu.2005.05.005
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bui, D., Lovric, V., Oliver, R. et al. Meniscal allograft sterilisation: effect on biomechanical and histological properties. Cell Tissue Bank 16, 467–475 (2015). https://doi.org/10.1007/s10561-014-9492-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-014-9492-3