Abstract
18F-sodium fluoride (18F-NaF) has been used to access aortic stenosis in clinical research setting. It is known that its uptake is related with microcalcification. The purpose of this study was to assess the relationship between 18F-NaF uptake by the aortic valve and cardiovascular risk. Twenty-five patients with risk factors for cardiovascular disease, without known cardiovascular disease or aortic stenosis underwent PET-CT with 18F-NaF. Cardiovascular risk was assessed through the ASCVD (Atherosclerotic Cardiovascular Disease) risk calculator. Aortic valve 18F-NaF (AoVCUL) uptake was evaluated through the corrected uptake per lesion (CUL = max SUV − mean blood-pool SUV). Calcium score was obtained through cardiac CT. The patients present a mean age of 63.90 ± 8.60 years and 56% males. The mean ASCVD was of 28.76 ± 18.96 (M 25, IQR 38.50). The mean aortic valve calcium score (AoVCaSc) was of 53.24 ± 164.38 (M 6; IQR 29.75) and the AoVCUL was of 0.50 ± 0.10 (M 0.52, IQR 0.15). The patients were classified according to the ASCVD: patients with a risk greater or equal than the 50th percentile of the ASCVD risk and patients with a risk lower than the 50th percentile. The AoVCUL was evaluated in both groups: AoVCUL = 0.56 ± 0.10 vs 0.42 ± 0.15, p = 0.02; AoVCaSc was of 0 in 11 patients (44%) and those with an ASCVD greater or equal than the 50th percentile had a mean AoVCaSc of 8.00 ± 13.80, and those with an ASCVD risk lower than the 50th percentile had a mean AoVCaSc of 95.00 ± 223.45; p = 0.09. In this study microcalcification, evaluated through 18F-NaF on PET-CT, was related with cardiovascular risk. Although the score of calcium seems to be higher in higher cardiovascular risk patients, no significant difference was found between groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aortic stenosis became the most common primary valve disease in the western world mainly due to the progressive aging of the population. Symptomatic aortic stenosis has a high mortality rate and carries a significant healthcare burden [1,2,3].
It is already established that the degenerative disease affecting the aortic valve is the result of an active process where inflammation and calcification, associated with cardiovascular risk factors, play a key role [1, 4,5,6].
The positron emission tomography-computed tomography (PET-CT) with 18F-sodium fluoride (18F-NaF) has long been used to evaluate bone metastases [7]. Recently this tracer has been applied, in clinical research, to characterize atherosclerotic plaques and aortic valve disease [8,9,10,11]. It is specific for microcalcification through ion changes between the hydroxyl group and the hydroxyapatite chrystals. It is known that calcification is a common pass way in aortic valve degeneration and atherosclerotic plaque progression [12]. Vascular calcification occurs, mainly, through osteogenic conversion of mesenchymal tissue into calcified bone. Regulators of bone formation are upregulated by activation of immune cells recruited to sites of chronic inflammation. Lipid oxidation promoted by cytoquines and free radicals intervene in the activation of osteogenic regulatory genes leading to the differentiation of mesenchymal progenitor cells. The mesenchymal-derived osteoblasts secrete a collagen proteoglycan matrix with the ability of binding calcium and phosphate salts, forming hydroxyapatite minerals [12].
Our aim was to characterize through PET-CT the uptake of 18F-NaF by the aortic valve in patients with risk factors for cardiovascular disease and evaluate its relation with cardiovascular risk assessed by the ASCVD risk calculator [13].
Material and methods
Population
Hypertensive patients, age over 40 years old, were recruited from the outpatient clinic of a tertiary university hospital. The inclusion was made upon the acceptance to participate in this prospective and exploratory study from May 1, 2014 to June 1, 2015.
Inclusion criteria
Besides hypertension patients were included if they had other primary risk factors, chronic kidney disease with a glomerular filtration rate below 60 ml/min [according Modification of Diet in Renal Disease equation—(MDRD)], diabetes mellitus or a markedly abnormal single risk factor.
Exclusion criteria
Patients under 40 years old and childbearing age women were excluded. Patients with cardiovascular disease (previous cardiac disease, cerebrovascular disease or peripheral vascular disease), with symptoms suggestive of disease (angina, heart failure symptoms, neurological complaints or claudication), aortic stenosis, severe renal impairment (GFR < 30 ml/min), moderate to severe hepatic failure (Child–Pugh class B or C), chronic inflammatory or neoplasic diseases were also excluded.
Upon inclusion, a baseline assessment of CVR was performed and for that purpose a blood sample was drawn to evaluate the levels of total cholesterol, LDL and HDL cholesterol, triglycerides, fasting blood glucose, creatinine, hemoglobin A1c (HbA1c) and C-reactive protein (CRP).
All patients underwent an 18F-NaF PET-CT to assess the uptake of the tracer in the aortic valve in the same day of clinical, echocardiographic and biochemical evaluation. Echocardiography was performed to rule out aortic valve disease, namely, aortic stenosis.
All the procedures were done with the approval of the ethics committee of the Faculty of Medicine of the University of Coimbra, in accordance with the Declaration of Helsinki and upon the written informed consent of each participant.
PET-CT
A 16-slice PET-CT system was used (Gemini GXL Philips) and images were acquired 60 min after intravenous administration of 185 MBq of 18F-NaF (5 mCi). The enrolled patients underwent cardiac PET-CT imaging. After the performance of an attenuation correction CT scan (non-enhanced 120 kV and 50 mA), PET images were acquired. Iterative reconstruction was obtained in multiple phases. A matrix of 144 × 144 was applied for reconstruction of transversal PET slices. Voxel size was of 4 × 4 × 4 mm and the spatial resolution of 8 mm. Focal uptake of the tracer was determined by PET-CT fusion images. Aortic valve uptake was evaluated in a 3-dimensional multiplanar mode and 4 mm slices, in horizontal transaxial planes, were considered top to bottom of the aortic valve for the establishment of circular regions of interest (ROI) around the valve. Semi-quantitative analysis was accomplished using the standardized uptake values (SUV) estimated for each slice and for the whole valve (Fig. 1). These values were corrected for blood-pool activity by subtraction—corrected uptake per lesion (CUL) as previously described by the authors [11]. Blood-pool SUV was estimated as the mean of five ROI in the mid lumen of superior vena cava. From the CT images, Agatston calcium score of the aortic valve was also evaluated.
Statistical analysis
Continuous data was tested for normality with the Shapiro-Wilks test and was represented by their mean, median, and interquartile range. Student’s t test and the Mann–Whitney test were applied to compare continuous variables as appropriate. Correlations between normally distributed data were performed with Pearson correlation and presented as r2 values. Spearman correlation was used for nonparametric data.
Data analysis was performed by StatView 5.0.1, version for Macintosh and Windows, SAS Institute.
Results
All the included 25 patients were followed by the outpatient clinic due to hypertension. Their mean age was of 63.9 ± 8.6, minimum of 48 and maximum of 80 years old. Figure 2 shows the distribution by gender and cardiovascular risk factors. Clinical evaluation and biochemical parameters are expressed in Table 1. In general, this is a high cardiovascular risk population where 80% have diabetes and 72% hyperlipidemia. The median BMI was also of 29.56. Total cholesterol, LDL cholesterol, fasting blood glucose and triglycerides were also above the normal values in almost all patients.
Echocardiographic assessment of the aortic valve showed no significant stenosis as the maximum velocity was inferior to 2 m/s in all patients [14].
The calcium score of the valve was of 0 in 11 patients (44%), with a mean of 44.40 ± 165.7, median 6.00 and IQR 29.75. 18F-NaF uptake was estimated through the corrected uptake by lesion (CUL)and was 0.5 ± 0.1, median 0.52 and IQR 0.15.
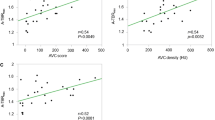
The uptake of the tracer and the calcium score of the valve were correlated with ASCVD considering the risk as a continuous variable and as a categorical variable with two defined risk groups: less than the 50th percentile or greater or equal than the 50th percentile. The results are presented in Fig. 3 and Table 2. Simple regression analysis didn’t show a significant relationship between the assessed variables but a trend is noticed between cardiovascular risk and 18F-NaF uptake by the aortic valve (Fig. 3). When the population was divided in two groups according to the 50th percentile of the ASCVD, the 18F-NaF uptake by the valve was significantly higher in higher risk patients, while the calcium score didn’t show a significant difference between the groups (Table 2). We also analyze the uptake of the tracer regarding the presence of calcium and no significant differences were found. Those without any calcium had an uptake of 0.47 ± 0.18 (median 0.48; IQR 0.22) comparing with 0.51 ± 0.11 (median 0.52; IQR 0.12) of those with some degree of valve calcification by the calcium score (p = 0.54).
Discussion
The natural history of aortic valve degeneration comprises a long asymptomatic period during which occurs fibrotic thickening of the aortic leaflets with progression to calcification which is the most common cause of aortic stenosis affecting 0.4% of the general population. The asymptomatic period is variable and is usually associated with a risk of sudden death of less than 1% [1].
Aortic valve leaflets comprise three layers: covering the aortic side, a collagen rich fibrosa, a middle proteoglican-rich spongiosa and covering the ventricular side, the elastin-rich ventricularis. The leaflets are covered by valvular endothelial cells (VEC) and fibroblast-like cells, the valvular interstitial cells (VIC), are spread between the described layers. The remodeling of the valve begins by the action of several factors such age, biochemical, genetic and mechanical risk factors. Activation of VEC, inflammation, angiogenesis and VIC transformation by osteogenic differentiation contribute to the degeneration process [15,16,17].
The association between aortic valve disease and cardiovascular risk factors suggests that aortic stenosis has an atherosclerotic-like progression. Nowadays it is known that a more complex process is involved with specific-cell signaling pathways regulating valvular calcification [15,16,17].
Fluorine-18 fluorodeoxyglucose(18F-FDG) and 18F-NaF uptake have been used to evaluate inflammation and microcalcification in aortic valve disease and the results are promising since they target key mediators for disease progression [18]. In what respects 18F-FDG it seems that its uptake was higher in patients with mild to moderate aortic stenosis in comparison with controls or with those with severe disease [19]. Abdelbaky A et al. concluded that 18F-FDG uptake was a marker of disease progression as those patients with higher rates of valve calcification were those with higher 18F-FDG early uptake [20]. In observational retrospective studies, on oncologic and rheumatologic patients, 18F-NaF uptake by the aortic valve was higher in patients with aortic calcification and stenosis [21].
Dweck et al.in a prospective study published in 2012 showed that 18F-FDG has a higher uptake in aortic stenosis patients than in controls increasing discreetly with the severity of the disease [6]. In comparison the 18F-NaF uptake was higher in patients with sclerosis and aortic stenosis than in controls and increases with disease severity. In this study 35% and 91% of patients with aortic stenosis had 18F-FDG and 18F-NaF uptake, respectively [6]. They also conclude through the follow-up of a subset of these patients that the uptake of 18F-NaF correlates with calcium deposition seeming to predict disease progression [8]. This follow-up study comprises a group of patients in whom aortic valve surgery was performed and on those an association between 18F-NaF signal and markers of calcification (alkaline phosphatase and osteocalcin) was found [8].
Giving the above results we aimed to assess, as far as we know by the first time, the uptake of 18F-NaF by the aortic valve of patients with high cardiovascular risk. Aortic stenosis was excluded in all of them. We used the CUL instead of TBR in the quantification of aortic valve uptake of the tracer considering the results already published [11, 22].
It was found that 18F-NaF uptake and though microcalcification were related with ASCVD risk leading to the hypothesis that sodium fluoride could be a biomarker of disease onset. Calcification estimated by calcium score was not related with ASCVD risk and several patients had a score of 0 in spite of their cardiovascular risk.
These results seemed to support the association between risk factors and aortic valve microcalcification [23, 24]. In fact, before stenosis, aortic valve sclerosis was found to be related with 18F-NaF uptake [6]. In this study, 18F-NaF uptake was observed in patients with no detected calcification and no stenosis of the aortic valve.
Previous studies targeting the relation between cardiovascular risk factors and aortic disease had no positive results [25,26,27] and this was probably linked with the presence of advanced disease characterized by calcification and stenosis. In fact, the presence of advanced degeneration of the valve imposes mechanical stress and osteogenic differentiation that further increase disease progression [15, 16]. Microcalcification, according to our results, seemed to be associated with cardiovascular risk assessed by the ASCVD risk calculator and could be an early marker of valve degeneration.
Limitations
The number of patients studied was small, and so, our results and conclusions should be considered hypothesis generating needed to be validated in a larger population. In order to evaluate aortic disease progression, a long follow-up period is required.
The ideal dose of F18-NaF for this kind of study remains to be established, quantification of sodium fluoride uptake is still controversial and the used outcome measure could influence conclusions.
New knowledge gained
In patients with no significant valvular disease, microcalcification, in particularly, from aortic valve could be measured with 18F-NaF PET-CT.
18F-NaF uptake of aortic valve was correlated with cardiovascular risk measured with ASCVD score.
No significant correlation was found between aortic valve calcium score and 18F-NaF uptake or with ASCVD score.
Conclusion
As far as we know this study was the first attempt to characterize the aortic valve in high cardiovascular risk patients. In spite of the small sample size it shows the existence of a link between aortic uptake of sodium fluoride and cardiovascular risk. Further studies with larger populations are required to confirm the described results.
Abbreviations
- 18F-NaF:
-
18F-sodium fluoride
- AoVCaSc:
-
Aortic valve calcium score
- AoVCUL:
-
Aortic valve 18F-NaF uptake
- ASCVD:
-
Atherosclerotic cardiovascular disease score from American College of Cardiology
- CVR:
-
Cardiovascular risk
- MDRD:
-
Modification of diet in Renal disease equation
- PET-CT:
-
Positron emission tomography-computed tomography
References
Bonow RO, Greenland P (2015) Population-wide trends in aortic stenosis incidence and outcomes. Circulation 131(11):969–971
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R et al (2017) Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 135(10):e146–e603
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M (2006) Burden of valvular heart diseases: a population-based study. Lancet 368(9540):1005–1011
Mohler ER 3rd, Gannon F, Reynolds C, Zimmerman R, Keane MG, Kaplan FS (2001) Bone formation and inflammation in cardiac valves. Circulation 103(11):1522–1528
Dweck MR, Khaw HJ, Sng GK, Luo EL, Baird A, Williams MC et al (2013) Aortic stenosis, atherosclerosis, and skeletal bone: is there a common link with calcification and inflammation? Eur Heart J 34(21):1567–1574
Dweck MR, Jones C, Joshi NV, Fletcher AM, Richardson H, White A et al (2012) Assessment of valvular calcification and inflammation by positron emission tomography in patients with aortic stenosis. Circulation 125(1):76–86
Beheshti M, Mottaghy FM, Paycha F, Behrendt FFF, Van den Wyngaert T, Fogelman I et al (2015) (18)F-NaF PET/CT: EANM procedure guidelines for bone imaging. Eur J Nucl Med Mol Imaging 42(11):1767–1777
Dweck MR, Jenkins WS, Vesey AT, Pringle MA, Chin CW, Malley TS et al (2014) 18F-sodium fluoride uptake is a marker of active calcification and disease progression in patients with aortic stenosis. Circ Cardiovasc Imaging 7(2):371–378
Joshi NV, Vesey AT, Williams MC, Shah AS, Calvert PA, Craighead FH et al (2014) 18F-fluoride positron emission tomography for identification of ruptured and high-risk coronary atherosclerotic plaques: a prospective clinical trial. Lancet 383(9918):705–713
Jenkins WS, Vesey AT, Shah AS, Pawade TA, Chin CW, White AC et al (2015) Valvular (18)F-fluoride and (18)F-fluorodeoxyglucose uptake predict disease progression and clinical outcome in patients with aortic stenosis. J Am Coll Cardiol 66(10):1200–1201
Ferreira MJ, Oliveira-Santos M, Silva R, Gomes A, Ferreira N, Abrunhosa A et al (2017) Assessment of atherosclerotic plaque calcification using F18-NaF PET-CT. J Nucl Cardiol 25:1733–1741
Irkle A, Vesey AT, Lewis DY, Skepper JN, Bird JL, Dweck MR et al (2015) Identifying active vascular microcalcification by (18)F-sodium fluoride positron emission tomography. Nat commun 6:7495
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 74:1376–1414
Gharacholou SM, Karon BL, Shub C, Pellikka PA (2011) Aortic valve sclerosis and clinical outcomes: moving toward a definition. Am J Med 124(2):103–110
Milin AC, Vorobiof G, Aksoy O, Ardehali R (2014) Insights into aortic sclerosis and its relationship with coronary artery disease. J Am Heart Assoc 3(5):e001111
Lerman DA, Prasad S, Alotti N (2015) Calcific aortic valve disease: molecular mechanisms and therapeutic approaches. Eur Cardiol 10(2):108–112
Shen M, Tastet L, Bergler-Klein J, Pibarot P, Clavel MA (2018) Blood, tissue and imaging biomarkers in calcific aortic valve stenosis: past, present and future. Curr Opin Cardiol 33(2):125–133
Jung JJ, Jadbabaie F, Sadeghi MM (2018) Molecular imaging of calcific aortic valve disease. J Nucl Cardiol 25(4):1148–1155
Marincheva-Savcheva G, Subramanian S, Qadir S, Figueroa A, Truong Q, Vijayakumar J et al (2011) Imaging of the aortic valve using fluorodeoxyglucose positron emission tomography increased valvular fluorodeoxyglucose uptake in aortic stenosis. J Am Coll Cardiol 57(25):2507–2515
Abdelbaky A, Corsini E, Figueroa AL, Subramanian S, Fontanez S, Emami H et al (2015) Early aortic valve inflammation precedes calcification: a longitudinal FDG-PET/CT study. Atherosclerosis 238(2):165–172
Hyafil F, Messika-Zeitoun D, Burg S, Rouzet F, Benali K, Iung B et al (2012) Detection of 18fluoride sodium accumulation by positron emission tomography in calcified stenotic aortic valves. Am J Cardiol 109(8):1194–1196
Oliveira-Santos M, Castelo-Branco M, Silva R, Gomes A, Chichorro N, Abrunhosa A et al (2017) Atherosclerotic plaque metabolism in high cardiovascular risk subjects—a subclinical atherosclerosis imaging study with (18)F-NaF PET-CT. Atherosclerosis 260:41–46
Peltier M, Trojette F, Sarano ME, Grigioni F, Slama MA, Tribouilloy CM (2003) Relation between cardiovascular risk factors and nonrheumatic severe calcific aortic stenosis among patients with a three-cuspid aortic valve. Am J Cardiol 91(1):97–99
Le Tourneau T, Marechaux S, Vincentelli A, Ennezat PV, Modine T, Polge AS et al (2007) Cardiovascular risk factors as predictors of early and late survival after bioprosthetic valve replacement for aortic stenosis. J Heart Valve Dis 16(5):483–488
Rossebo AB, Pedersen TR, Boman K, Brudi P, Chambers JB, Egstrup K et al (2008) Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med 359(13):1343–1356
Arsenault BJ, Boekholdt SM, Mora S, DeMicco DA, Bao W, Tardif JC et al (2014) Impact of high-dose atorvastatin therapy and clinical risk factors on incident aortic valve stenosis in patients with cardiovascular disease (from TNT, IDEAL, and SPARCL). Am J Cardiol 113(8):1378–1382
Zhao Y, Nicoll R, He YH, Henein MY (2016) The effect of statins on valve function and calcification in aortic stenosis: A meta-analysis. Atherosclerosis 246:318–324
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Domingues, C., João Ferreira, M., Silva, R. et al. Aortic valve microcalcification and cardiovascular risk: an exploratory study using sodium fluoride in high cardiovascular risk patients. Int J Cardiovasc Imaging 36, 1593–1598 (2020). https://doi.org/10.1007/s10554-020-01854-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01854-0