Abstract
Infectious endocarditis (IE) is a serious condition with a high morbidity and mortality. The optimal management of IE depends not only on correct antibiotic therapy and surgery when needed, but involves identification of the portal of entry and detection of extracardiac infectious manifestations. To discover the latter an (18)F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET)/CT examination has been proposed. However, the diagnostic value of a PET/CT in this setting remains unresolved. Thus, we wished to assess the usefulness of a PET/CT study in patients with IE as a supplemental method to standard work-up in evaluating primary and distant infective foci. A retrospective cohort study of 72 IE patients admitted from 2008 to 2010, which had an 18F-FDG-PET/CT performed. Findings were assessed in relation to the routine work-up, which served as the “gold standard”. One hundred-fifty-nine infectious lesions were identified. 18F-FDG-PET identified 64 of these, and suggested another 50. Overall sensitivity and positive predictive value was 40 and 56 %, respectively, in detecting both cardiac and extracardiac infective foci. When excluding lungs and organs with high physiological FDG-uptake/secretion, the corresponding values increased to 87 and 52 %, respectively. 18F-FDG-PET/CT may be an important diagnostic tool in detecting extra cardiac infections in patients with IE, particularly in organs with low physiological glucose uptake.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE) is a well-known and greatly feared entity, with high morbidity and mortality. The clinical presentation and clinical course of IE varies enormously, depending on the comorbidity, the nature of the bacteria and possible complications. One of the major clinical problems in the work up of IE patients is identifying extracardiac manifestations, which might be the portal of entry, the result of embolization, or metastatic infection. The overall embolic rate is estimated to approximately 20–50 %, silent events are noted in 20 % [1]. Therefore, all patients, with IE are subjected to an extensive patient-tailored examination strategy according to international recommendations. Basically, this consists of patient history, physical examination, the use of conventional and/or advanced imaging modalities, and weekly interdisciplinary conferences between cardiologists, microbiologists, surgeons, and infectious disease specialists to optimize the therapeutic management [1, 2].
Currently, the role of (18)F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) in this clinical setting remains unanswered in international guidelines. 18F-FDG-PET, mainly used in cancer investigation, is a modality with potentially increasing clinical indications. 18F-FDG, being a radioactive glucose derivate, has predilection for cells with high glucose consumption and makes it non-specific for cancer, infection and inflammation [3]. Combining PET with CT adds an accurate anatomical localization of the metabolic process. However, the on-going assessment of this technique has no standard Ref. [4]. Nonetheless, in clinical practice 18F-FDG-PET imaging has become increasingly used and the preferred method in the diagnosis of unknown infections. This clinical approach is supported by accumulating evidence favouring the use of 18F-FDG-PET imaging as first line imaging approach in patients with certain infectious processes [5].
Since the diagnostic value of 18F-FDG-PET/CT in the setting of IE remains unresolved, we wanted to assess the usefulness of the method as a supplemental method to standard work-up in evaluating primary and distant infective foci.
Method
Study population
This retrospective single centre study comprises 72 patients with definite IE according to Duke’s modified criteria [1]. They were admitted to the Department of Cardiology, Odense University Hospital from January 2008 to December 2010 and underwent at least one 18F-FDG-PET/CT. The indication of the 18F-FDG-PET/CT was set by the attending physician. During the same time period another 104 patients with IE were admitted to the department, without having an 18F-FDG-PET/CT performed. The patients’ condition varied from critically ill to less severe courses set to conservative strategy or elective surgery. All patients received treatment in accordance to the guidelines from the European Society of Cardiology (ESC). Two physicians (CÖ and AA) were responsible for gathering all relevant and pre-specified data from the medical records. Each case was discussed in the entire study group and in cases with doubt about the clinical relevance of a finding final data was made up as a consensus decision.
18F-FDG-PET/CT scanning
Examinations were conducted on dedicated PET/CT systems (GE Discovery VCT XT, GE Discovery RX or GE Discovery STE; GE Healthcare, Milwaukee, WI, USA). Patients were fasting 6 h (diabetes patients only 4 h) prior to injection and were given a weight adjusted dose of 4 MBq/kg (min 200 and max 400 MBq) 18F-FDG 60 min prior to PET/CT acquisition. The duration of the PET scan was at least 2.5 min per bed position increasing to 3.5 min in extremely overweight patients. Different CT scan protocols were used according to type of disease. Diagnostic scans (≈12 mSv) with intravenous contrast media (Iopromide 370 mg iodine/ml) were used when pathological conditions were suspected in the abdomen or in the head/neck region, whereas low-dose CT scans (≈5 mSv) without contrast media were used when pathological conditions were suspected in other regions. The standard field of view for the PET/CT involved the base of the skull to the mid thighs, unless it was specified differently. The analysis of the 18F-FDG-PET/CT for infection and inflammation relied on visual assessment of the distribution and intensity of the tracer. The 18F-FDG-PET was interpreted by two nuclear medicine physicians and the diagnostic CT by a radiologist. A mutual conclusion was achieved.
18F-FDG-PET/CT versus other modalities
Since no gold standard in the work-up of extracardial manifestations in IE exists, the result of each 18F-FDG-PET/CT was compared to the results of the clinical standard work-up according to ESC Guidelines for IE, which at the same time served as gold standard. Depending on the clinical setting, the work-up included patient history, physical examination (including examination by a dentist), laboratory tests, X-ray, CT, ultrasound, magnetic resonance imaging (MRI), nuclear techniques, histopathological studies, microbiological cultures, endoscopies and clinical assistance from other specialities. All patient courses were reviewed weekly at a conference with participants from cardiology, surgery, anaesthesia, infectious disease, and microbiology departments regarding optimizing patient treatment, diagnostics and indication for surgery.
All lesions identified by the 18F-FDG-PET/CT were evaluated, regardless of localization, and the data were described on a per-lesion analysis. This means that any patient could potentially display more than one lesion. A 18F-FDG-PET/CT lesion was considered true positive, if the finding was in agreement with result from other modalities. False positive was defined as a 18F-FDG-PET/CT lesion, which could not be confirmed by the standard work-up. 18F-FDG-PET/CT was classified as true negative, when both 18F-FDG-PET/CT and standard work up showed up negative. False negative was considered to be the result, when 18F-FDG-PET/CT missed a significant lesion detected by the standard work-up. In this study, the imaging modality and/or expert evaluation closest in time to the 18F-FDG-PET/CT were selected for comparison.
Statistical analysis
Data were analysed and compared in order to calculate sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV). Descriptive measures for continuous variables are presented as mean ± SD or median values and range. Categorical variables are presented as absolute numbers or percentage. Excel software (Microsoft) was used for statistical calculations.
Results
Patient characteristics
The mean age was 63 ± 17 (range 15–89), and 71 % were males. See Table 1 for baseline characteristics. The majority of patients were diagnosed within 1 month from the onset of symptoms, and the 18F-FDG-PET/CT was conducted at a median of 6 days (range 5 days before to 58 days after the diagnosis was established). Left sided IE was seen in the majority of cases. Staphylococci (40 %) and streptococci (29 %) were the most prominent bacteria, as seen in Table 2. Surgery was applied in almost half of the study population (44 %). Valve regurgitation was the main indication for surgery (91 %). In-hospital mortality was 15 %. With a mean follow-up of more than one year (469 days), 6 % had relapse, 3 % reinfection, and long-term survival rate was 72 %.
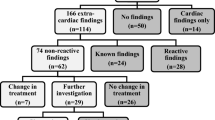
18F-FDG-PET/CT
Overall study population
A total of 159 lesions were identified by standard work-up and used as reference. 18F-FDG-PET identified 64 of these lesions, and suggested another 50 infectious lesions, that could not be verified by other examinations. The indiscriminating analysis of the overall study population merely showed a sensitivity and PPV of 40 and 56 %, respectively.
Organs with low physiological FDG uptake
When excluding organs with high physiological FDG uptake (central nervous system, heart, and urinary tracts), gingiva and the lungs a total of 38 lesions were left. 18F-FDG-PET identified 33 of these lesions but also demonstrated 31 other lesions suggestive of infection or inflammation, leading to a sensitivity and PPV of 87 and 52 %, respectively. For details see Table 3.
False negative results
Compared with MRI, 18F-FDG-PET/CT missed two cases with spondylodiscitis. One was misinterpreted as being degenerative changes (Fig. 1), and in the other there was no FDG-uptake. Two cases had an infection with staphylococcus aureus in the skin; one had a large infected wound on the finger (Fig. 2), and another had multiple wounds located on face and back. 18F-FDG-PET/CT missed these findings. One false-negative lesion in the spleen was diagnosed by a regular CT of abdomen, indicating infarction.
69-year-old male with prolapsed mitral valve and rupture of chordae. He had a history of rheumatoid arthritis treated with salazopyrine and prednisone. He had diffusely increased FDG-uptake in pulmonary infiltrations, interpreted as pneumonia (TP, blue arrow). There was activation of bone marrow and spleen, probably due to infection. At lumbar level L2/L3, the patient had severe scoliosis and slightly elevated metabolism, mistakenly interpreted as degeneration (FN, green arrows). Magnetic resonance imaging was indicative of spondylodiscitis but biopsy was never performed. There was inhomogeneous FDG-avidity of the prostate (FP, purple arrow) but neither infection nor malignancy could be verified
This 48-year-old male with staphylococcal aortic and mitral valve endocarditis had cut the left fourth finger (FN) on a piece of glass during work. This information was not available when interpreting the 18F-FDG-PET/CT. Retrospectively there was a faint FDG-avidity on the left fourth finger (green arrows) which could easily be mistaken by, for instance, urine contamination. The patient also had FDG-avid, localized pulmonary infiltrates (FP, blue arrows), which could not be verified by chest X-ray (which served as standard!). In case-reports similar patterns of FDG-avid pulmonary lesions have been described in septic embolisms. By contrast enhanced CT of the abdomen, two spleen infarctions (FN) were identified and by MR of the brain, infarctions (FN) were demonstrated, both findings were not visualized by 18F-FDG-PET and low dose CT without contrast enhancement. Neither were the infected valves (FN)
False positive results
In ten patients, variable FDG-uptake was found in the hip, shoulder, knee, sacroiliac, acromioclavicular and sternoclavicular joints. However, clinical evaluation based on microbiology, histopathology, X-rays or ultrasonography concluded unspecific findings, thus it was speculated, that all these lesions were non-infectious. Nonetheless, one patient with a history of deep venous thrombosis of the right lower limb revealed no signs of infection or inflammation, but 18F-FDG-PET/CT raised suspicion of bursitis of the knee. The patient recovered without further interference (Fig. 3). Additionally six false-positive cases, with FDG-uptake extending from mild to intense hot spots, were seen in the muscles surrounding the shoulder (Fig. 4), arm, gluteus, pelvic and thighs. Neither clinical evaluation, including ultrasonography, bone scintigraphy, nor microbiological cultures could confirm this. Five patients had various degrees of FDG uptake in the intestinal region (gall bladder, colon, coecum, appendix, sigmoideum, rectum, and anal region). Diagnostic endoscopy was normal in three patients. The fourth patient had just a CT verified calcification of the prostate, while in the last case, small amounts of FDG was localized in the appendix, and no supplementary diagnostic procedures were performed. Former median sternotomy was associated with four false-positive lesions, where standard clinical judgment disproved infections. Another three patients had increased FDG-uptake in the genitals, but all were considered as false-positive; one patient (Fig. 1) had inhomogeneous FDG-uptake in both lobes of prostate. Prostate specific antigen (PSA) was only slightly elevated, also at followed up. The second patient had a similar PSA-level but was never followed up by PSA. The third patient had a faint FDG-uptake in the major labia but no changes by CT—it seemed not to represent urinary contamination and misalignment, though this would be a possible explanation. One patient had indication of a possible abscess in the vicinity of the iliac artery, but this was rejected by clinical judgment and more likely sequelae to hemorrhage after invasive angiography. Further one patient had a peripheral FDG-uptake in a hepatic cyst, as revealed by ultrasonography. Yet a patient had mild FDG uptake in a wedge shaped lesion in the spleen, but further investigations were not employed.
51-year-old overweight male of 140 kg had a recent history of deep venous thrombosis of the right lower limb (green arrows). By 18F-FDG-PET/CT an intensely increased metabolism was demonstrated beneath the right quadriceps tendon and patella, believed to represent bursitis (FP, blue arrows). However aspiration from the knee was never done, and thus the diagnosis never properly established. The patient responded well on antibiotics
A 45-year-old female with systemic lupus erythematosus and a prosthetic aortic valve through 1 year was admitted to the hospital with fever of unknown origin and malaise. She was diagnosed with septicemia caused by pneumococci. Transesophageal echocardiography was without signs of infection and was redone after PET/CT, still without proven infection. However, the condition was treated as infective endocarditis. Two years later, she suffered from increasing periannular leak from the exact location of increased FDG-avidity, clearly demonstrated by 18F-FDG-PET (TP, green arrow). She also had a pathological 18F-FDG accumulation in the soft tissue of the neck, misinterpreted as phlegmonous infection of the neck (FP, blue arrows). It was most likely a haematoma after removal of central venous catheter
True positive results
18F-FDG-PET/CT was successful in diagnosing spondylodiscitis in eight cases, including one with additional epidural abscess in the lumbar region. 18F-FDG-PET/CT accomplished a sensitivity of 100 % in the intestinal region (n = 8). Another five cases with hot spots in the muscles were true-positive and identified as psoas abscess and abscess in the paravertebral muscle. Three patients had evidence of relevant liver lesions, which were confirmed or suggested by CT and/or ultrasonography. Two patients had osteomyelitis, and both were correctly identified by 18F-FDG-PET/CT. One were located to the left clavicle head, and confirmed by MRI, while the other was detected in a diabetic foot and confirmed by X-ray, but missed by bone scintigraphy. Two lesions of significance were diagnosed in spleen, where CT of abdomen verified sequela to splenic abscess. Moreover, FDG uptake corresponding to infection was further observed in the adrenal gland, knee prosthesis and in a bifurcational prosthesis in three different patients. 18FDG-PET/CT demonstrated also high FDG-uptake in the hip joint in one patient. The only positive finding regarding the eye and its surroundings was a basal cell carcinoma on the lateral corner of the left eye.
Pulmonary lesions
Using clinical examination, a plain X-ray and in some cases a CT scan as the reference, the sensitivity and PPV were 82 and 53 %, respectively.
False negative results
Four patients had false-negative pulmonary findings. One of these had excessive pleural effusion and atelectasis by 18F-FDG-PET/CT, but no FDG avid pulmonary infiltrates, whereas the other three had neither infiltrates nor FDG-avid lesions.
False positive results
Sixteen patients had pulmonary lesions, which could not be confirmed by the clinical judgment or other modalities. In this context, it is important to acknowledge the inappropriateness of the reference method used.
True positive results
18F-FDG-PET/CT identified 18 of 22 pulmonary lesions diagnosed by X-ray and CT.
Organs with high physiological uptake/secretion and infective cardiac vegetations
The brain, heart, and kidneys are known to have a high physiological FDG uptake or secretion, whereas gingival lesions may go unrecognized by PET, due to partial volume effect, which may also be superimposed by salivary secretion. In these organs the values of sensitivity and PPV were 13 and 81 %, respectively, (Table 3).
False negative results
18F-FDG-PET/CT was not able to detect IE in 59 cases. In a similar way 18F-FDG-PET/CT performed poor in detection of relevant foci in the oral cavity. In all but nine patients, an oral evaluation was performed by a dentist resulting in following diagnosis; Parodontitis apicalis chronica (n = 5), Parodontitis marginalis/profund parodontit (n = 4), Redix relicta (n = 1), Cystis residualis (n = 1), ulcus decubitale (n = 1), and unspecified dental foci (n = 10). Dental extractions were applied in almost all cases. Altogether 18F-FDG-PET/CT had 22 false-negative findings with respect to the oral cavity, particularly the teeth and gums. Stroke events in the form of septic embolism at the time of the 18F-FDG-PET/CT was overlooked in four cases, and this also applied in one patient with infection in the kidney.
False positive results
Three patients showed signs of FDG uptake in the oral cavity, but these were not reproducible by dentist examination.
True positive results
18F-FDG-PET/CT was able to visualize compelling and non-physiological hot spots in the heart (eight prosthetic valve IE, four native valves, and one lead infection), of whom one had no echocardiographic evidence of vegetation and another had newly developed advanced atrioventricular block.
Time from diagnosis until 18F-FDG-PET/CT: early versus late
The median time from diagnosis of IE until performing 18F-FDG-PET/CT was 6 days, and ≤6 days was thus taken as the cut off between early versus late 18F-FDG-PET/CT. In organs with low physiological uptake sensitivity and PPV were 78 % (CI 52–93) and 54 % (CI 34–73), respectively in the early group (n = 37), while the values for the late group (n = 35) were 95 % (CI 73–100) and 50 % (CI 34–66), respectively, for details see Table 4.
Discussion
A preliminary review conducted by Bertagna et al. [6] reports that 18F-FDG-PET/CT cannot substitute routine investigations in making the final diagnosis of IE, but it might contribute as an added value in evaluating extracardial infective lesions. In this study, we report the observed results of 72 IE patients undergoing 18F-FDG-PET/CT, the so far largest IE population investigated. Accordingly, our study reported both novel and several intriguing findings. First, the performance of 18F-FDG-PET/CT in identifying extracardiac manifestations of IE in organs with low physiological uptake (like liver, spleen, intestinal, adrenal gland, genitals, vertebra, vascular vessel, muscle, joints, bones, orthopedic hardware, and skin) showed very promising results with a high sensitivity. Second, the ability of 18F-FDG-PET/CT to detect infectious foci in organs with high physiological glucose (including the heart and the valves) uptake is poor. A number of mainly relatively small studies have evaluated the value of 18F-FDG-PET/CT in patients with occult infections, which all showed promising results and in several cases the scanning led to a change in treatment management [7–10]. Riet et al. [11] recently conducted the first prospective and so far, the only study (n = 25) to consider the diagnostic role of 18F-FDG-PET/CT in a selected IE population with possible peripheral embolism or distant infectious lesions. Intubated patients, patients referred to immediate surgery and patients with renal impairment were excluded. An 18F-FDG-PET/CT was performed within 2 weeks from diagnosis. Median age was 70 with a male:female ratio of 3:2 and prosthetic valve IE was observed in 40 %. Maybe as a consequence of the exclusion of groups, staphylococcus aureus rate was low (16 %). The 18F-FDG-PET/CT detected embolization and metastatic infection in 44 % of the study population, 28 % of the findings were occult, whilst only 12 % had FDG uptake around the valves. A therapeutic impact in almost one-third of patients was shown. So far, most experience regarding the benefit of 18F-FDG-PET/CT to distinctively detect the IE (the affected valve) is based on casuistic reports [12]. The diagnostic value of 18F-FDG-PET/CT to establish the diagnosis IE is, however, dubious, since lesions may be small, moving and surrounding myocardium may or may not be FDG-avid and disturbed by attenuations artefact from prosthetic valves. These factors may reduce sensitivity and specificity. This issue is discussed in detail by Bertagna et al. [6].
In line with these studies we demonstrated results favoring 18F-FDG-PET/CT as a supplemental tool in the work up of IE patients with distant infective lesions. As opposed to several of the other studies, we enrolled exclusively patients with IE, including those excluded in the study of Riet et al. Although our study population was a selected subgroup of patients admitted with IE, our patients were still comparable with a European cohort [13]. Another crucial difference is that the results estimated in the abovementioned studies appear to be on a per patient basis, which means that for any PET, the final result was either categorized as TP, FP, TN or FN. In fact PET can often report more than one finding. In an attempt to handle this dilemma we based our estimation on a per lesion basis, hence giving us the benefit of providing with a more accurate result. Moreover, 18F-FDG-PET/CT is not definitively able to distinguish between infection, inflammation and cancer, thus in clinical practice, the final report typically contains a combination of significant, insignificant and often dubious findings. In extension of this, we were aware, that 18F-FDG-PET/CT could identify relevant non-infectious abnormalities. Such findings were cancer in the lungs or skin, which could serve as a portal of entry, and therefore we found it reasonable to include these findings as positive lesions.
In order to improve visualization of the lesions (increase the target-to-background ratio) by 18F-FDG-PET/CT, it has been suggested to reduce time between FDG-injection and imaging. Inflammatory cells, in contrast to malignant cells, have an active glucose-6-phosphatase enzyme resulting in escape of FDG out of the inflammatory cells, thereby increasing the target-signal in early images [14].
Since treatment with antibiotics might diminish the infectious foci, it has been suggested, to perform the 18F-FDG-PET/CT early in the disease course [15]. However, if the scan is performed very early, the lesions might be too small to be detected. In our retrospective study, the 18F-FDG-PET/CT was requested by the clinicians mostly in cases without infection control, giving a relative broad time span. We observed a slightly higher sensitivity among those, who underwent a late 18F-FDG-PET/CT. However, since the early versus late scan was not due to randomisation the observed difference may be a coincidence, and should be investigated further in a randomised study.
It is important to emphasize that, in most cases, 18F-FDG-PET/CT findings are dependent on confirmatory tests as the modality is rather unspecific and PPV is rather low. To clarify the value of 18F-FDG-PET/CT in a clinical setting a randomized trial is warranted. 18F-FDG-PET/CT should be performed on the day of diagnosis, together with other relevant diagnostics modalities to perform a comparative analysis without a time difference. Moreover 18F-FDG-PET/CT should be repeated to elucidate any progress or reduction of the lesions. Clinical endpoints should comprise complications, mortality, and recurrence of IE. Since the lack of a gold standard, a microbiological examination for every finding proposed by 18F-FDG-PET/CT is mandatory, however presently not possible. In the future, molecular imaging visualizing bacteria or their products may help in identifying active endocarditis at an earlier stage at the same time perhaps even reporting the responsible type of bacteria [16].
Limitations
Given the retrospective nature of this work, diagnostic performance of 18F-FDG-PET/CT was per se difficult to estimate because comparison relied on the verification of all lesions by other (sometimes inferior) modalities. No well-defined gold standard could be achieved. Indeed the lesions detected by the 18F-FDG-PET/CT may have been misclassified because of missing microbiological culture. Even if microbiological culture had been recruited in all lesions, errors may have been added by aspiration from necrotic regions, by introducing bacteria accidentally or because of effect of antibiotic therapy. Nonetheless, in most of the 159 lesions identified, needle aspiration was not performed and microbiology not assessed. We therefore made large efforts to confirm every finding by discussing each single case in plenum, and making a consensus decision in cases with doubt. This meant that the standard work up and the clinical diagnose served as the reference standard.
Moreover, clinical assessment, chest X-ray and a CT scan might serve as a poor reference for pneumonia. However, a tracheal aspiration was only seldom performed. Furthermore, in certain occasions, the diagnosis was based solely on the results of the 18F-FDG-PET/CT, even though it was the experimental test. Although our patients were comparable with the European cohort, this study only involved patients with IE, in whom 18F-FDG-PET/CT was performed (41 % of all patients) and thus the study is not consecutive.
Conclusion
18F-FDG-PET/CT is feasible and yields a promising future in detecting extra cardiac infections in patients with IE, especially when excluding the central nervous system, the dental region, the lungs and the urogenital system. Future prospective studies may reveal its true potential in locating infectious foci, which would spare the patient for additional non-contributing confirmatory imaging.
References
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus Antunes M, Thilen U, Lekakis J, Lengyel M, Muller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL (2009) Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the task force on the prevention, diagnosis, and treatment of infective endocarditis of the European Society of cardiology (ESC). Endorsed by the European Society of clinical microbiology and infectious diseases (ESCMID) and the International Society of chemotherapy (ISC) for infection and cancer. Eur Heart J 30(19):2369–2413. doi:10.1093/eurheartj/ehp285
Thuny F, Grisoli D, Collart F, Habib G, Raoult D (2012) Management of infective endocarditis: challenges and perspectives. Lancet 379(9819):965–975. doi:10.1016/S0140-6736(11)60755-1
Kumar R, Basu S, Torigian D, Anand V, Zhuang H, Alavi A (2008) Role of modern imaging techniques for diagnosis of infection in the era of 18F-fluorodeoxyglucose positron emission tomography. Clin Microbiol Rev 21(1):209–224. doi:10.1128/CMR.00025-07
Basu S, Chryssikos T, Moghadam-Kia S, Zhuang H, Torigian DA, Alavi A (2009) Positron emission tomography as a diagnostic tool in infection: present role and future possibilities. Semin Nucl Med 39(1):36–51. doi:10.1053/j.semnuclmed.2008.08.004
Israel O, Keidar Z (2011) PET/CT imaging in infectious conditions. Ann N Y Acad Sci 1228:150–166. doi:10.1111/j.1749-6632.2011.06026.x
Bertagna F, Bisleri G, Motta F, Merli G, Cossalter E, Lucchini S, Biasiotto G, Bosio G, Terzi A, Muneretto C, Giubbini R (2012) Possible role of F18-FDG-PET/CT in the diagnosis of endocarditis: preliminary evidence from a review of the literature. Int J Cardiovasc Imaging 28(6):1417–1425. doi:10.1007/s10554-011-9984-1
Bleeker-Rovers CP, Vos FJ, Wanten GJ, van der Meer JW, Corstens FH, Kullberg BJ, Oyen WJ (2005) 18F-FDG PET in detecting metastatic infectious disease. J Nucl Med 46(12):2014–2019
Simons KS, Pickkers P, Bleeker-Rovers CP, Oyen WJ, van der Hoeven JG (2010) F-18-fluorodeoxyglucose positron emission tomography combined with CT in critically ill patients with suspected infection. Intensive Care Med 36(3):504–511. doi:10.1007/s00134-009-1697-8
Kluge S, Braune S, Nierhaus A, Wichmann D, Derlin T, Mester J, Klutmann S (2012) Diagnostic value of positron emission tomography combined with computed tomography for evaluating patients with septic shock of unknown origin. J Crit Care 27(3):316.e1–316.e7. doi:10.1016/j.jcrc.2011.10.004
Vos FJ, Bleeker-Rovers CP, Sturm PD, Krabbe PF, van Dijk AP, Cuijpers ML, Adang EM, Wanten GJ, Kullberg BJ, Oyen WJ (2010) 18F-FDG PET/CT for detection of metastatic infection in gram-positive bacteremia. J Nucl Med 51(8):1234–1240. doi:10.2967/jnumed.109.072371
Van Riet J, Hill EE, Gheysens O, Dymarkowski S, Herregods MC, Herijgers P, Peetermans WE, Mortelmans L (2010) (18)F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging 37(6):1189–1197. doi:10.1007/s00259-010-1380-x
Vind SH, Hess S (2010) Possible role of PET/CT in infective endocarditis. J Nucl Cardiol 17(3):516–519. doi:10.1007/s12350-009-9174-x
Murdoch DR, Corey GR, Hoen B, Miro JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falco V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH (2009) Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International collaboration on endocarditis-prospective cohort study. Arch Intern Med 169(5):463–473. doi:10.1001/archinternmed.2008.603
De Winter F, Vogelaers D, Gemmel F, Dierckx RA (2002) Promising role of 18-F-fluoro-d-deoxyglucose positron emission tomography in clinical infectious diseases. Eur J Clin Microbiol Infect Dis 21(4):247–257. doi:10.1007/s10096-002-0708-2
Gotthardt M, Bleeker-Rovers CP, Boerman OC, Oyen WJ (2010) Imaging of inflammation by PET, conventional scintigraphy, and other imaging techniques. J Nucl Med 51(12):1937–1949. doi:10.2967/jnumed.110.076232
Panizzi P, Nahrendorf M, Figueiredo JL, Panizzi J, Marinelli B, Iwamoto Y, Keliher E, Maddur AA, Waterman P, Kroh HK, Leuschner F, Aikawa E, Swirski FK, Pittet MJ, Hackeng TM, Fuentes-Prior P, Schneewind O, Bock PE, Weissleder R (2011) In vivo detection of Staphylococcus aureus endocarditis by targeting pathogen-specific prothrombin activation. Nat Med 17(9):1142–1146. doi:10.1038/nm.2423
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özcan, C., Asmar, A., Gill, S. et al. The value of FDG-PET/CT in the diagnostic work-up of extra cardiac infectious manifestations in infectious endocarditis. Int J Cardiovasc Imaging 29, 1629–1637 (2013). https://doi.org/10.1007/s10554-013-0241-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-013-0241-7