Abstract
Purpose of Review
This article reviews the current imaging role of 18F–fluordeoxyglucose positron emission computed tomography (18F–FDG-PET/CT) combined with cardiac CT angiography (CTA) in infective endocarditis and discusses the strengths and limitations of this technique.
Recent Findings
The diagnosis of infective endocarditis affecting prosthetic valves and intracardiac devices is challenging because echocardiography and, therefore, the modified Duke criteria have well-recognized limitations in this clinical scenario. The high sensitivity of 18F–FDG-PET/CT for the detection of infection associated with the accurate definition of structural damage by gated cardiac CTA in a combined technique (PET/CTA) has provided a significant increase in diagnostic sensitivity for the detection of IE.
Summary
PET/CTA has proven to be a useful diagnostic tool in patients with suspected infective endocarditis. The additional information provided by this technique improves diagnostic performance in prosthetic valve endocarditis when it is used in combination with the Duke criteria. The findings obtained in PET/CTA studies have been included as a major criterion in the recently updated diagnostic algorithm in infective endocarditis guidelines.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE) is a serious condition that remains associated with a poor prognosis, despite major advances in the related diagnostic and therapeutic approaches. The mortality rates associated with this condition have not decreased in the last 30 years [1]. The diagnosis of IE, which poses a challenge because of its variable clinical presentation, is best achieved using a collaborative approach by a multidisciplinary IE unit [2]. Approximately 20% of IE patients have intracardiac devices or prosthetic valves, a clear predisposing factor that makes them a special population with a different epidemiological profile and higher mortality [2, 3]. The capability of the modified Duke criteria (DC) for diagnosing IE is limited in these patients since it relies on interpretation of their complex echocardiographic (ECHO) studies [4]. As a result, a conclusive diagnosis is not reached in many cases of suspected IE, creating a problem for therapeutic decision-making that can lead to a delay in starting appropriate treatment.
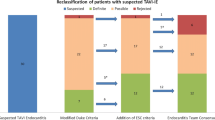
Positron emission computed tomography with 18F–fluordeoxyglucose (18F–FDG-PET/CT) detects activated inflammatory cells in infection (leukocytes, monocyte macrophages, and CD4+ T lymphocytes), which express a high density of glucose transporters [5,6,7]. Recent studies have reported promising results with the use of these techniques in the diagnosis of prosthetic valve [8••] and cardiac device [9, 10••, 11] endocarditis. The precise anatomical definition of cardiac computed tomography angiography (CTA) enables visualization of IE lesions [12, 13] as well as preoperative evaluation of the coronary arteries [14]. Furthermore, the most recent PET/CT systems can perform cardiac CTA (PET/CTA), thus combining the high sensitivity of 18F–FDG-PET/CT to detect inflammation with the high spatial resolution of CTA to define structural damage (Fig. 1) [15••]. The difficult interpretation of ECHO studies in patients with suspected IE of prosthetic valves and intracardiac devices reduces the sensitivity and specificity of the modified DC. There is a considerable improvement in diagnostic sensitivity (from ≈50 to ≈90%) when the DC and PET/CT are used in combination, and the addition of PET/CTA provides further important benefits. By reclassifying most possible IE cases into a more conclusive group (definite or rejected), PET/CT may have a major impact on the therapeutic strategies used and the clinical outcomes in this population.
A 70-year-old patient with early (3 months postimplantation) bioprosthetic aortic valve infective endocarditis due to Staphylococcus epidermidis. a Fused PET/CTA transverse view of the aortic valve shows intense (SUVmax 6.81, SUVratio 3.01), focal/heterogeneous periprosthetic hypermetabolic activity (arrow) and a large multiloculated perivalvular pseudoaneurysm (arrowheads). b The high spatial resolution of CTA allows better definition of the structural damage and evaluation of the coronary artery. Note that the pseudoaneurysm (asterisks) is in close proximity to the left main coronary artery (arrowhead)
Current guidelines have recently included PET/CTA findings as a major criterion in the diagnostic algorithm of IE [16]. This technique is especially recommended to reach a prompt IE diagnosis in patients with a normal or doubtful ECHO and a persistently high clinical suspicion of IE, as it may detect infection before significant damage has occurred.
Technical Considerations
Patient Preparation
To facilitate visualization of presumed sites of infection in the heart, suppression of 18F–FDG uptake by normal myocardium must always be encouraged. This is done by combining a high-fat/low-carbohydrate diet [17], followed by a fasting period of at least 14 to 18 h [18], and intravenous administration of 50 IU/kg heparin 15 min before tracer injection [19] and after checking the blood glucose level (<180 mg/L). The only clinical restriction to perform the study is severe hemodynamic instability.
Image Acquisition
The technical requisites for performing PET/CTA with a hybrid PET/CT scanner are cardiac gating for both techniques and at least 64-detector row CT. Images should be acquired after the patient has rested for 60 min. In negative cases with a high suspicion of IE, a delayed acquisition (3 h) may improve the diagnostic sensitivity of the technique [20].
The following sequential acquisition protocol is recommended: (1) whole-body PET/CT at 2-min acquisition time per bed position, uncorrected and corrected for attenuation; (2) a localized 8-min ECG-gated cardiac bed to improve evaluation of the region of interest (preferably, PET images should be reconstructed using an iterative algorithm, which will apply all possible corrections); and (3) ECG-gated cardiac CTA in all patients without renal impairment (glomerular filtration rate <60 mL/min/m2) [21] and able to perform a breath hold. The use of intravenous beta-blockers is indicated in patients with a fast heart rate (more than 65 bpm) and no contraindications (septic and unstable patients). The routine iodinated contrast injection protocol should be adjusted individually to the patient’s body mass index and the scan duration. A typical injection consists of 50–120 mL of isomolar iodinated contrast medium at a flow rate of 4–7 mL/s, followed by a 30–50-mL saline chaser [22]. When PET/CTA is performed to diagnose device infection, a prospective, ECG-gated, venous phase CTA sequence is recommended to evaluate local soft tissue changes, lead vegetations, and venous thrombosis of the vascular accesses.
The radiation exposure derived from PET/CTA examinations is not negligible and should be addressed with radiation dose reduction measures. However, the potential advantages of PET/CT overcome this limitation in seriously ill patients in whom an early diagnosis may have a critical impact on the prognosis. The calculated median effective radiation dose of PET/CTA studies is approximately 25.32 mSv (IQR 18.57–33.41) [15••].
Image Interpretation
The metabolic images are fused with the CT images and analyzed, whole-body PET images with the unenhanced, non-ECG-gated whole-body CT images and gated cardiac PET images with the cardiac CTA images.
Metabolic Images
Visual Analysis
Focal or heterogeneous hypermetabolic activity related to the prosthetic material or cardiac lesions is identified in both the attenuation-uncorrected and attenuation-corrected images. Metal implants produce streak artifacts that can significantly degrade CT images by obscuring anatomical structures and disease features. In PET/CT, these artifacts may also propagate to CT-based attenuation maps causing inaccuracies in the quantification of tissue tracer uptake in the attenuation-corrected PET images. Software-based metal artifact reduction (MAR) techniques are now available, and these algorithms should be enabled to reduce the risk of erroneously increased tracer uptake, which may inaccurately infer the presence of infection or inflammation [23].
Semi-Quantitative Analysis
The intensity of 18F–FDG uptake can be measured as the maximum standardized uptake value (SUVmax) in the abnormal area. The ratio of the prosthetic material SUVmax to the mean standardized uptake value of a 3-cm2 region of interest (ROI) in the blood pool or a 30-cm2 ROI in the liver (SUVratio or target-to-background ratio) overcomes bias related to individual differences in FDG metabolism [24]. Semi-quantitative assessment of FDG uptake may add support to the visual information, but the causes of SUV variability must be taken into account in the interpretation, such as the 18F–FDG circulation time, the prescan blood glucose levels, the uptake parameters, the injected 18F–FDG dose, and the PET/CT system used, among other factors. Hence, the diagnosis should not rely exclusively on the semi-quantitative values, which should be considered only a guide and not conclusive data [25]. In a cohort of 92 patients, cutoff values of ≥3.7 for the SUVmax and ≥1.69 for the SUVratio enabled identification of positive cases with a sensitivity of 90.74% and specificity of 78.95%. A specificity of 100% for confirming infection was reached with a cutoff value of ≥6.87 for the SUVmax and ≥3.45 for the SUVratio [15••]. Semi-quantitative assessment in cardiac device infection is relatively easy in pocket IE but controversial in lead infection because the SUVmax values may be too close to the patient’s background metabolic activity, leading to a very low specificity (50%) [15••].
CT and CTA Images
Infectious endocarditis-related cardiac lesions include vegetations (soft-tissue lesions attached to valves or leads), perivalvular extension of the infection in the form of abscesses (non-cavitated, extra-luminal soft tissue lesions) or collections (fluid-filled cavities), pseudoaneurysms (saccular enlargement of a vascular structure or contrast-filled soft tissue cavitation arising from it), and fistulae (abnormal contrast-filled tracts or communications between vascular structures) [12, 13]. Infective involvement of the coronary arteries and coronary artery disease can be ruled out depending on the quality of the CTA images [14].
The studies can be classified using the following criteria: positive for active infection, intense focal or heterogeneous hypermetabolic activity related to the prosthetic material or to cardiac lesions if present; negative for active infection, absence of hypermetabolic activity in the prosthetic material or cardiac lesions (non-infectious postoperative complications or lesions related to past or currently cured endocarditis); and doubtful, mild homogenous FDG uptake, especially in recently operated patients.
Finally, the whole-body fused images must be carefully reviewed to detect IE-related peripheral findings, embolic events, alternative diagnoses other than IE, and incidental neoplastic lesions that could be the source of infection.
PET/CTA in Prosthetic Valves
In a contemporary cohort of suspected prosthetic valve IE patients, Saby et al. [8••] suggested that the sensitivity of the modified DC could be increased to 97% if 18F–FDG-PET/CT results were included together with the clinical, microbiological, and echocardiographic parameters. The same findings have been reported for 18F–FDG-PET/CTA [15••]. The main added value of these techniques is the significant reduction in the rate of misdiagnosed IE cases, classified in the possible category using the DC when IE is suspected. Reclassification of most possible IE cases into a more conclusive diagnosis of definite or rejected IE leads to a significant increase in the diagnostic sensitivity (91–97%), which could have important impact on IE outcomes. Hence, the main indication to perform PET/CTA in prosthetic valve IE is a possible/rejected IE evaluation according to the DC, with persistently high clinical suspicion after the routine evaluation. Furthermore, when IE has been conclusively diagnosed as definite with the DC, 18F–FDG-PET/CTA can be performed to depict perivalvular extension of the infectious process in cases where ECHO findings are inconclusive.
PET/CTA has yielded important additional benefits over PET/CT in these patients (Fig. 1). First, PET/CTA enables identification of a larger number of anatomic lesions than non-gated PET/CT (pseudoaneurysm, fistula, thrombosis, and coronary involvement); many of which may be relevant for clinical and surgical decision-making. Second, PET/CTA provides an additional 18% reduction in doubtful studies after PET/CT [15••]. On non-gated PET/CT, focal FDG uptake in the myocardium can be wrongly attributed to the prosthetic material in cases of incomplete myocardial suppression and incorrect fusion of metabolic and anatomic images. Finally, in patients with an indication for surgery, CTA provides useful preoperative information about coronary artery disease [15••].
PET/CTA in Cardiac Devices
Cardiac implantable electronic device infection is a severe disease that often affects older patients with numerous co-morbidities and is associated with high mortality [26]. The clinical presentation can vary considerably. Sometimes patients show only mild, non-specific local signs or fever of long-term evolution [27]. With regard to clinical decision-making, misdiagnosis of an infected device can lead to severe sepsis, but unnecessary removal of an uninfected device also carries a high clinical risk. Furthermore, there are no specific diagnostic criteria to evaluate patients with suspected cardiac device infection, since the DC are completely extrapolated from valve IE. Hence, a non-invasive test to confirm or rule out infection would be desirable in this clinical scenario.
PET/CT provides added diagnostic value to the modified DC, particularly in the subset of possible cardiac device infections [11, 15••, 28], and it has the capability to cover the whole device. However, a distinction should be made between infection confined to the generator pocket and/or the extra-cardiac portion of the lead and infection of the intravascular lead portion. Diagnostic accuracy is very high in generator pocket infection, in which mild inflammatory changes after device implantation usually do not extend beyond 6 weeks and are easily differentiated from infection after this period (Fig. 2). All the related studies have shown an almost 100% accuracy for infection of the generator pocket and for the extra-cardiac portion of the lead [8••, 9, 10••, 29•, 30].
Pacemaker pocket and generator infection on a device implanted 8 months previously. PET/CTA shows significant (SUVmax 6.15, SUVratio 2.56) FDG uptake around the pacemaker generator (a, b). No metabolic activity is visualized at the leads. c Prospective ECG-triggered cardiac CT angiography in the venous phase ruled out filling defects suggestive of vegetations or thrombi along the electrode path
Regarding lead infection, PET/CT is very specific when tracer uptake is visualized. However, a negative result does not completely exclude the presence of small vegetations with low metabolic activity (limited sensitivity and negative predictive value) [29•, 30]. Delayed acquisition (3 h) may improve the results in this group, especially when the infection is related to the leads, as was recently proposed by Leccisotti et al. [20]. These authors found that the lower blood pool activity in a delayed acquisition for detecting cardiac device infection resulted in an increase in the SUVratio and higher diagnostic accuracy (from 51 to 74%).
PET/CTA in Patients with Both Prosthetic Valves and Devices
There is no clear consensus about the management of patients with prosthetic valve IE who additionally have a cardiac device with no signs of infection. In the same sense, the indications are not at all precise regarding the management of patients with device infection who also have a prosthetic valve. The AHA guidelines recommend (class IIa/evidence level B) complete removal of pacemaker or defibrillator systems in patients about to undergo valve surgery for valve IE caused by Staphylococcus aureus or fungi, even when there is no evidence of device or lead infection. In patients with device infection, close follow-up or echocardiography of the prosthetic valves is indicated [31]. In contrast, the ESC guidelines do not provide specific recommendations for these patients [16]. PET/CTA may clarify the site of the infection and avoid unnecessary removal of uninfected material in patients with both prosthetic valves and cardiac devices.
PET/CTA in Special Groups
Aortic Grafts
In patients with aortic grafts in whom ECHO is often unable to determine the true extension of the infectious process, PET/CTA can give an overall evaluation of the prosthetic structure (Fig. 3). The most common infected graft pattern consists of intense, heterogeneous peritube FDG uptake involving the entire tube that is more intense than uptake at the sutures (tube > sutures pattern), associated with a peritube soft tissue lesion in the CTA images (peritube abscess). Another possible infectious manifestation is a peritube-infected collection, visualized as a low-attenuation collection with an enhancing wall. Leaflet thickening/vegetations, pseudoaneurysms, and fistulae are also seen in these patients.
A 57-year-old man with a bicuspid aortic valve and dilated ascending aorta had required Bentall-De Bono surgery with an aortic valved graft replacement 2 months previously. He was hospitalized due to persistent fever. Fused PET/CTA axial image (a) and multiplanar reconstruction (b) depict findings consistent with tube infection and a peritube abscess. A peritube fluid-filled collection (a, b, asterisks) showing intense, heterogeneous wall uptake (a, b, arrows) extends to the distal tube suture (b, arrowhead). FDG uptake is seen to extend anteriorly and affect the sternotomy (a, open arrow)
Congenital Heart Disease
A growing number of patients with congenital heart disease are reaching adulthood, and IE is a major complication in this group [32]. Patients with CHD have a complex anatomy, and their surgical treatment often requires implantation of a large amount of prosthetic material, which makes them a special IE population with a clear predisposing factor [33]. Use of the modified DC including ECHO findings is limited for diagnosing these patients, as the lesions visualized are difficult to interpret. Hence, many cases of suspected IE are left without a conclusive diagnosis [34], which means that the expected impact of PET/CTA in this group may be greater than in the general IE population. There is an evident need for additional diagnostic tools for this complex population in such a severe condition, and it seems reasonable to encourage the use of PET/CTA in these patients whenever possible (Fig. 4).
A 48-year-old man with repaired tetralogy of Fallot, a recent pulmonary valve replacement, and early (5 months postimplantation) bioprosthetic pulmonary valve infective endocarditis (Staphylococcus epidermidis). a Fused PET/CTA transverse view of the pulmonary valve shows intense (SUVmax 8.04, SUVratio 4.49), heterogeneous hypermetabolic activity at the valve ring (arrows), and a periprosthetic hypermetabolic soft tissue mass extending to the anterior mediastinum (arrowheads), suggesting a periprosthetic abscess. b Oblique coronal view depicts prosthetic and periprosthetic metabolic activity (arrows) in close contact with a ventricular septal defect closure patch (open arrow)
Patients at High Surgical Risk
Some patients with IE are at a high risk of surgical mortality because of a complex anatomy or previous interventions, and medical treatment is decided. When metabolic activity and the anatomic lesions (valve vegetations or periannular complications) are observed to stabilize or improve on PET/CTA seriated studies in these patients, the conservative treatment decision is reinforced, and the findings may help to establish the duration of the antibiotics administered (Fig. 5). Although the use of control PET/CTA is not a formal clinical indication, we believe that it can support clinical decisions in very complex patients with established IE and a high risk of surgery, in whom it could be used to monitor the response to antimicrobial treatment. However, the currently available data do not suffice for a general recommendation in this line [35].
A 79-year-old woman with late (7 years postimplantation) prosthetic aortic valve endocarditis due to Staphylococcus aureus. PET/CTA 1 (diagnosis) transverse (top) and oblique coronal (bottom) views of the aortic valve show intense (SUVmax 6.76), focal, periprosthetic hypermetabolic activity (arrows), consistent with a periprosthetic abscess. She also had a mechanical mitral valve, implanted 24 years previously that showed no morphometabolic signs of infection. Due to the patient’s high surgical risk, medical treatment with 12 weeks of antibiotics was decided. A second PET/CTA (control) showed near resolution of the previously observed metabolic activity
Native Valve IE
The use of 18F–FDG-PET/CT is currently limited in native valve IE. Because of several reasons, such as limitations in the spatial and metabolic resolution of the systems and unsuccessful suppression of myocardial 18F–FDG uptake in some cases, the sensitivity of 18F–FDG-PET/CT in native valve IE is too poor to recommend routine use in this scenario [36, 37].
Additional Benefits of Whole-Body PET/CT
Peripheral Findings
As PET/CT examines the whole body in a single acquisition, it is of value for detecting peripheral embolic and metastatic infectious events in most anatomical locations, with the exception of the brain. A variable incidence of embolisms has been reported in IE (15–40%), with the most common locations being the spleen, spine, and lung. Many of these embolic lesions are clinically silent, and they can cause persistent bacteremia and reinfection of a new prosthesis in patients requiring surgery. Nevertheless, the finding of silent peripheral embolisms should not lead to changes in the therapeutic management (extending antibiotic treatment or delaying an indicated surgery) in all cases [15••, 16,17,18,19,20,21,22,23,24,25,26,27,28, 29•, 30,31,32,33,34,35,36,37,38,39]. Careful evaluation of the lung fields is important in IE of the leads to detect septic pulmonary embolisms that may be present in right-sided IE.
Alternative Diagnosis
In patients in whom a diagnosis of IE is rejected, PET/CT can provide an alternative diagnosis of an infectious process (e.g., pneumonia, diverticulitis, urinary tract infection) or non-infectious condition (e.g., postoperative periprosthetic pseudoaneurysm, postpericardiotomy syndrome, pleuro-pericarditis).
Detection of Unsuspected Neoplastic Lesions
As patients with IE are an elderly population, it is reasonable that tumors might be incidental findings on PET/CT examination (5% incidence in our study). Many of those diagnosed in early stages are potentially curable. Some of these neoplastic lesions can be the source of infection in IE caused by certain pathogens, such as colon cancer-related microorganisms (Streptococcus bovis group or Enterococcus faecium).
Inflammation Versus Infection in the Early Postoperative Period
18F–FDG-PET/CT shows high sensitivity for detecting infection and inflammatory activity, and caution is advised when interpreting images acquired in patients who have recently undergone cardiac surgery. The postoperative inflammatory response may result in non-specific 18F–FDG uptake in the immediate postoperative period. Previous studies with pacemakers have shown very little inflammatory activity at 6 weeks postimplantation, suggesting that intense FDG uptake after this period must always be considered to indicate an infection. There is little available data on the morphologic and metabolic features following prosthetic valve or valve-tube graft surgeries and their short-term evolution. The inflammatory reaction after surgery is idiosyncratic in each patient and depends on the extent of surgery and the type of materials used. Certain specific situations generate a significant inflammatory response, such as combined ascending aortic surgery in which BioGlue is used to seal aortic graft anastomoses, a recognized cause of FDG uptake [40], and valve replacements requiring extensive removal of cardiac tissue and calcifications. To avoid false-positive diagnoses due to early postoperative inflammation, the guidelines recommended delaying PET/CT until 3 months after surgery. However, recent experience by our group suggests that the metabolic and anatomic patterns that help differentiate between inflammation and infection can be distinguished in these patients (Table 1 and Fig. 6) [41•].
Examples of postoperative inflammation in two patients, one with recent bioprosthetic aortic valve replacement (a, b) and the other with mechanical mitral valve replacement (c, d). Fused PET/CTA aortic planimetry (a) and three-chamber view (b) show thin valve leaflets and mild, homogeneous perivalvular FDG uptake (arrows). Fused PET/CTA image at the mitral plane (c) and three-chamber view (d) show mild, homogeneous FDG uptake (SUVmax 2.2) at the perivalvular suture (arrowheads)
Other Differential Diagnoses
As PET/CTA is a new technique, cardiac imaging specialists should be aware of certain confounders that can lead to misdiagnoses. Inadequate or unsuccessful myocardial suppression, which can be very focal in the basal anteroseptum, close to the prosthetic valves, may be wrongly interpreted as infection. In atrial fibrillation, the uncoordinated contraction of the atrial myocardium leads to high-energy consumption and consequent up-regulation of glucose metabolism, leading to increased 18F–FDG uptake of the atrial wall, even though ventricular myocardial glucose metabolism may be completely suppressed. The accumulation of 18F–FDG in the atrial myocardium may lie adjacent to the device leads and be hard to differentiate from infectious foci [42•].
As was mentioned above, surgical adhesive materials applied to ensure homeostasis, such as BioGlue used to seal aortic graft anastomoses and cannulation sites, generate a sterile inflammatory reaction and are a recognized cause of FDG uptake [40]. Other postoperative complications such as acute prosthetic thromboses and postpericardiectomy inflammatory syndromes can imply increased valve 18F–FDG uptake [43, 44].
Lipomatous hypertrophy of the interatrial septum is associated with a moderate to intense increase in 18F–FDG uptake and may be a confounder in patients with valves in the aortic position. The typical barbell shape and fat density without stranding on CT images argue against infection [45].
Cardiac granulomas visualized in sarcoidosis are highly hypermetabolic lesions. They usually affect the myocardium but can also be found in the valve endothelium [42•]. In the same way, primary and secondary cardiac tumors may present as hypermetabolic lesions [46] and could erroneously identify as infectious lesions.
Possible False Negatives
Some circumstances in which the diagnostic sensitivity of PET/CTA is decreased should be considered when interpreting the images. Small lesions may be below the metabolic/spatial resolution of PET/CT, as sometimes occurs in cardiac lead vegetations; hence, a negative result does not completely exclude the presence of small vegetations with low metabolic activity. The sensitivity of PET/CT may also be affected when the examination is performed some time after the start of antibiotic therapy, as antibiotics may affect the inflammatory response, especially in highly sensitive microorganisms. Although this situation is more likely to occur after 7 days of treatment, the precise time at which sensitivity may be compromised is unknown [35].
Conclusions
18F–FDG-PET/CT is a useful diagnostic tool for patients with prosthetic valves or intracardiac devices and suspected IE. Use of this technique increases the sensitivity of the modified DC up to ≈90%. The combination of the high sensitivity of 18F–FDG-PET/CT for detecting inflammation and the high spatial resolution of cardiac CTA to define structural damage is the best strategy for a prompt diagnosis of IE and its complications. Thus, it seems reasonable to encourage the use of PET/CTA in this population whenever possible. This significant diagnostic improvement, which could have an important impact on IE outcomes, merits further assessment in larger series.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fernández-Hidalgo N, Tornos Mas P. Epidemiology of infective endocarditis in Spain in the last 20 years. Rev Esp Cardiol. 2013;66:728–33.
Habib G. Management of infective endocarditis. Heart. 2006;92:124–30.
Duval X, Selton-Suty C, Alla F, et al. Endocarditis in patients with a permanent pacemaker: a 1-year epidemiological survey on infective endocarditis due to valvular and/or pacemaker infection. Clin Infect Dis. 2004;39:68–74.
Habib G, Badano L, Tribouilloy C, Vilacosta I, Zamorano JL. Recommendations for the practice of echocardiography in infective endocarditis. Eur Heart J. 2010;11:202–19.
Stumpe KD, Dazzi H, Schaffner A, von Schulthess GK. Infection imaging using whole-body FDG-PET. Eur J Nucl Med. 2000;27:822–32.
Gamelli RL, Liu H, He LK, Hofmann CA. Augmentations of glucose uptake and glucose transporter-1 in macrophages following thermal injury and sepsis in mice. J Leukoc Biol. 1996;59:639–47.
Jamar F, Buscombe J, Chiti A, et al. EANM/SNMMI guideline for 18F-FDG use in inflammation and infection. J Nucl Med. 2013;54:647–58.
•• Saby L, Laas O, Habib G, et al. Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J Am Coll Cardiol. 2013;61:2374–82. The use of 18 F-FDG-PET/CT is helpful for diagnosing prosthetic valve endocarditis. The results of this study supported for the first time addition of abnormal FDG uptake as a novel major criterion for prosthetic valve endocarditis.
Bensimhon L, Lavergne T, Hugonnet F, et al. Whole body [18F]fluorodeoxyglucose positron emission tomography imaging for the diagnosis of pacemaker or implantable cardioverter defibrillator infection: a preliminary prospective study. Clin Microbiol Infect. 2011;17:836–44.
•• Sarrazin JF, Philippon F, Tessier M, et al. Usefulness of fluorine-18 positron emission tomography/computed tomography for identification of cardiovascular implantable electronic device infections. J Am Coll Cardiol. 2012;59:1616–25. 18 F-FDG-PET/CT is useful for differentiating between cardiac device infection and recent post-implant changes. It increases the diagnostic capability and may guide appropriate therapy.
Graziosi M, Nanni C, Lorenzini M, et al. Role of 18F-FDG PET/CT in the diagnosis of infective endocarditis in patients with an implanted cardiac device: a prospective study. Eur J Nucl Med Mol Imaging. 2014;41:1617–23.
Feuchtner GM, Stolzmann P, Dichtl W, et al. Multislice computed tomography in infective endocarditis: comparison with transesophageal echocardiography and intraoperative findings. J Am Coll Cardiol. 2009;53:436–44.
Entrikin DW, Gupta P, Kon ND, Carr JJ. Imaging of infective endocarditis with cardiac CT angiography. J Cardiovasc Comput Tomogr. 2012;6:399–405.
Gahide G, Bommart S, Demaria R, et al. Preoperative evaluation in aortic endocarditis: findings on cardiac CT. AJR Am J Roentgenol. 2010;194:574–8.
•• Pizzi MN, Roque A, Fernández-Hidalgo N, et al. Improving the diagnosis of infective endocarditis in prosthetic valves and intracardiac devices with 18F-FDG-PET/CT-angiography: initial results at an infective endocarditis referral center. Circulation. 2015;132:1113–26. 18 F-FDG-PET/CT improves the diagnostic accuracy of the modified Duke criteria in patients with suspected infective endocarditis and prosthetic valves or cardiac devices, as was seen in previous series. This study found that PET/CTA yields the highest diagnostic performance and provides additional diagnostic benefits. Hence, the use of CTA in combination with PET images should be always encouraged in the evaluation of patients with IE.
Habib G, Lancellotti P, Antunes MJ, et al. ESC guidelines for the management of infective endocarditis. The task force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075–23.
Soussan M, Brillet P-Y, Nunes H, et al. Clinical value of a high-fat and low-carbohydrate diet before FDG-PET/CT for evaluation of patients with suspected cardiac sarcoidosis. J Nucl Cardiol. 2013;20:120–7.
Manabe O, Yoshinaga K, Ohira H, et al. The effects of 18-h fasting with low-carbohydrate diet preparation on suppressed physiological myocardial 18F-fluorodeoxyglucose (FDG) uptake and possible minimal effects of unfractionated heparin use in patients with suspected cardiac involvement sarcoidosis. J Nucl Cardiol. 2016;23:244–52.
Mc Ardle BA, Leung E, Ohira H, et al. The role of F18-fluorodeoxyglucose positron emission tomography in guiding diagnosis and management in patients with known or suspected cardiac sarcoidosis. J Nucl Cardiol. 2013;20:297–306.
Leccisotti L, Perna F, Lago M, et al. Cardiovascular implantable electronic device infection: delayed vs standard FDG PET-CT imaging. J Nucl Cardiol. 2014;21:622–32.
Ellis JH, Cohan RH. Reducing the risk of contrast-induced nephropathy: a perspective on the controversies. AJR Am J Roentgenol. 2009;192:1544–9.
Abbara S, Arbab-Zadeh A, Callister TQ, et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2009;3:190–204.
Ahmed FA, James J, Tout D, Arumugam P, Mamas M, Zaidi AM. Metal artefact reduction algorithms prevent false positive results when assessing patients for cardiac implantable electronic device infection. J Nucl Cardiol. 2015;22:219–20.
Memmott MJ, James J, Armstrong IS, Tout D, Ahmed F. The performance of quantitation methods in the evaluation of cardiac implantable electronic device (CIED) infection: a technical review. J Nucl Cardiol. 2015; doi:10.1007/s12350-015-0293-2.
Bucerius J, Mani V, Moncrieff C, et al. Optimizing 18F-FDG PET/CT imaging of vessel wall inflammation: the impact of 18F-FDG circulation time, injected dose, uptake parameters, and fasting blood glucose levels. Eur J Nucl Med Mol Imaging. 2014;41:369–83.
Rundstrom H, Kennergren C, Andersson R, Alestig K, Hogevik H. Pacemaker endocarditis during 18 years in Goteborg. Scand J Infect Dis. 2004;36:674–9.
Klug D, Lacroix D, Savoye C, et al. Systemic infection related to endocarditis on pacemaker leads: clinical presentation and management. Circulation. 1997;95:2098–107.
Tlili G, Amroui S, Mesguich C, et al. High performances of 18F-fluorodeoxyglucose PET-CT in cardiac implantable device infections: a study of 40 patient. J Nucl Cardiol. 2015;22:800–3.
• Cautela J, Alessandrini S, Cammilleri S, et al. Diagnostic yield of FDG positron-emission tomography/computed tomography in patients with CEID infection: a pilot study. Europace. 2013;15:252–7. This study indicates that 18 F-FDG-PET/CT is highly accurate for the diagnosis of skin and pocket device infection, but much less accurate for detecting lead vegetations in infective endocarditis. The reliability of 18 F-FDG-PET/CT findings in management and decision-making may vary according to the type of device infection.
Ahmed FZ, James J, Cunnington C, et al. Early diagnosis of cardiac implantable electronic device generator pocket infection using 18F-FDG-PET/CT. Eur Heart J Cardiovasc Imaging. 2015;16:521–30.
Nishimura RA, Otto CM, Bonow RO, et al. AHA/ACC guideline for the management of patients with valvular heart disease. J Am Coll Cardiol. 2014;22:57–185.
Engelfriet P, Boersma E, Oechslin E, et al. The spectrum of adult congenital heart disease in Europe: morbidity and mortality in a 5 year follow-up period—the Euro Heart Survey on adult congenital heart disease. Eur Heart J. 2005;26:2325–33.
Loureiro-Amigo J, Fernández-Hidalgo N, Pijuan-Domènech A, et al. Infective endocarditis in adult patients with congenital heart disease. Experience from a reference centre. Enferm Infecc Microbiol Clin. 2016; pii: S0213-005X(16)00029-X doi:10.1016/j.eimc.2016.01.004.
Saiman L, Prince A, Gersony WM. Pediatric infective endocarditis in the modern era. J Pediatr. 1993;122:847–53.
Scholtens AM, Van Aarnhem EE, Budde RP. Effect of antibiotics on FDG-PET/CT imaging of prosthetic heart valve endocarditis. Eur Heart J Cardiovasc Imaging. 2015;16:1223.
Kestler M, Muñoz P, Rodríguez-Créixems M, et al. In collaboration with the Group for the Management of Infectious Endocarditis (GAME). Role of 18F-FDG PET in patients with infectious. Endocarditis. J Nucl Med. 2014;55:1–6.
Granados U, Fuster D, Pericas JM, et al. Diagnostic accuracy of 18F–FDG PET/CT in infective endocarditis and implantable cardiac electronic device infection: a cross-sectional study. 2016. J Nucl Med 57:1726–32.
Van Riet J, Hill EE, Gheysens O, et al. 18F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging. 2010;37:1189–97.
Bonfiglioli R, Nanni C, Morigi JJ, et al. 18F-FDG PET/CT diagnosis of unexpected extracardiac septic embolisms in patients with suspected cardiac endocarditis. Eur J Nucl Med Mol Imaging. 2013;40:1190–6.
Schouten LR, Verberne HJ, Bouma BJ, Van Eck-Smit BL, Mulder BJ. Surgical glue for repair of the aortic root as a possible explanation for increased F-18 FDG uptake. J Nucl Cardiol. 2008;15:146–7.
• Pizzi MN, Roque A, Cuéllar-Calabria H. Infective versus inflammatory patterns in 18F-FDG-PET/CTA of prosthetic cardiac valves and valve-tube grafts. J Am Coll Cardiol Img. 2016;9(10):1224–7. Inflammatory changes are always a concern when images are acquired after recent surgery. In this study, the authors define the characteristic patterns of 18 F-FDG uptake and the typical anatomic changes that can aid in differentiating between inflammation and infection in these patients.
• Scholtens AM, Swart LE, Verberne HJ, Tanis W, Lam ME, Budde RP. Confounders in FDG-PET/CT imaging of suspected prosthetic valve endocarditis. J Am Coll Cardiol Img. 2016; doi:10.1016/j.jcmg.2016.01.024. 18 F-FDG-PET/CT is a novel technique, and the boundaries between normal and abnormal findings are relatively undefined. Awareness of confounding variants is essential in the context of suspected prosthetic valve endocarditis and cardiovascular infection, as this may prevent false-positive or false-negative readings. This article provides an overview of possible confounders which should be borne in mind when interpreting cardiac PET/CT studies.
Yaddanapudi K, Brunken R, Tan CD, Rodriguez ER, Bolen MA. PET-MR imaging in evaluation of cardiac and Paracardiac masses with histopathologic correlation. J Am Coll Cardiol Img. 2016;9(1):82–5.
Salomäki SP, Hohenthal U, Kemppainen J, et al. Visualization of pericarditis by fluorodeoxyglucose PET. Eur Heart J Cardiovasc Imaging. 2014;15:291.
Fan CM, Fischman AJ, Kwek BH, Abbara S, Aquino SL. Lipomatous hypertrophy of the interatrial septum: increased uptake on FDG PET. AJR. 2005;184:339–42.
Rahbar K, Seifarth H, Schäfers M, et al. Differentiation of malignant and benign cardiac tumors using 18F-FDG PET/CT. J Nucl Med. 2012;53:856–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Albert Roque, María N. Pizzi, Hug Cuéllar-Calàbria, and Santi Aguadé-Bruix declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Nuclear Cardiology
Rights and permissions
About this article
Cite this article
Roque, A., Pizzi, M., Cuéllar-Calàbria, H. et al. 18F–FDG-PET/CT Angiography for the Diagnosis of Infective Endocarditis. Curr Cardiol Rep 19, 15 (2017). https://doi.org/10.1007/s11886-017-0824-3
Published:
DOI: https://doi.org/10.1007/s11886-017-0824-3