Abstract
The aim of the study was to evaluate the ability to detect extra-cardiac foci by means of whole-body 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) in patients with definite endocarditis (IE) according to the modified Duke criteria and investigate the clinical impact of the findings. From January 2011 to December 2015 we included 178 patients (mean age 66 ± 14 years, 25% female) with IE in this multicentre study. FDG-PET/CT was part of the work-up for extra-cardiac foci in the including hospitals and was performed at a median of 9 days (IQR 10) after IE was diagnosed. In 114 patients FDG-PET/CT identified 166 lesions: 52 (31%) infectious lesions, 21 (13%) cases of cancer, 7 (4%) cases of embolism, 60 (36%) reactive findings, and 26 (16%) other types of lesions. A total of 74 new extra-cardiac findings, not previously discovered by other modalities, were identified in 62 patients and resulted in additional investigations in 29 patients and a change in treatment in 18 patients (10%). The most frequent diagnoses discovered by FDG-PET/CT were colon polyps, cancer, and spondylodiscitis. There was a higher rate of findings leading to a change in treatment in patients above 67 years of age infected with other bacterial aetiologies than streptococci. FDG-PET/CT was useful to detect extra-cardiac foci. FDG-PET/CT findings may lead to unnecessary investigations. One out of 10 the patients with definite endocarditis had underwent a change in treatment regimen based on the FDG-PET/CT findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE) is a rare disease with a poor prognosis despite improvements in treatment [1]. The course and prognosis of the disease may be influenced by extra-cardiac manifestations, such as cerebral embolism, vasculitis, spondylodiscitis, abscesses, gastrointestinal or other cancers, and septic arthritis, which are frequently associated with or seen as complications of IE [2,3,4,5]. Extra-cardiac foci may necessitate additional or adjusted treatment or require further diagnostic work-up or follow-up, and findings may influence the indications for surgery [6,7,8]. The identification of extra-cardiac foci in patients with IE is therefore essential but can be challenging [9].
In 18F-fluoro-deoxyglucose positron emission tomography (FDG-PET), FDG accumulates in organ tissues and lesions with enhanced glucose metabolism. The modality may be useful to detect infectious and inflammatory foci and unknown malignancies in IE patients, which are known to be associated with IE. The sensitivity and specificity of FDG-PET/CT vary depending on location [2,3,4,5, 10,11,12,13,14]. In the 2015 European Society of Cardiology (ESC) guidelines, FDG-PET/CT was suggested as a tool for the detection of peripheral embolic and non-cardiac infectious complications, and endocardial FDG accumulation has been included as a major criterion in the diagnosis of IE [15]. Furthermore, two recent reviews addressing imaging in IE patients recommended integrating FDG-PET/CT into the standard work-up for all patients diagnosed with endocarditis [16, 17]. However, the clinical value of using FDG-PET/CT for identification of extra-cardiac foci in patients with IE has only been examined in a few minor studies, and the results are conflicting [2, 12,13,14, 18,19,20].
The primary aim of this study was to examine the clinical usefulness of FDG-PET/CT for the detection of extra-cardiac foci in a larger cohort of patients with definite endocarditis. The secondary aim was to examine if any baseline variables or characteristics of the disease were associated with the number of clinically significant findings detected by FDG-PET/CT.
Methods
Cohort selection
The patients were recruited from three teaching hospitals in the capital region of Denmark (Rigshospitalet, Hillerød Hospital, and Herlev-Gentofte Hospital). Local IE guidelines at the three centres included whole body FDG-PET/CT for extra-cardiac work-up in all patients with a definite diagnosis of IE. IE was diagnosed by an expert team according to the modified Duke criteria [15, 21]. All adult patients diagnosed with IE and examined by FDG-PET/CT as part of the IE work-up between January 1, 2011, and December 31, 2015 were included in the study and retrospectively evaluated. The patients were treated in accordance with the ESC guidelines [15, 21]. Clinical data, laboratory data, and the FDG-PET/CT results were collected from the patients’ medical records in October 2016. The patients’ medical records were systematically reviewed, and medical history, symptoms, findings, comorbidities, microbiology, echocardiographic findings, and treatment were registered.
For patients readmitted with IE during the study period, only the first admission was included. The study was conducted in accordance with the Declaration of Helsinki and approved by the Danish Data Protection Agency [j.nr. 2012-58-0004 (3-3013-1464/1/)].
FDG-PET/CT
Whole body FDG-PET/CT was performed using Siemens dedicated PET/CT scanners (Biograph 64 True D or mCT) at Herlev-Gentofte Hospital and Rigshospitalet and a Philips Gemeni TF scanner at Hillerød Hospital. A dose of 4 MBq 18F-FDG per kilogram body weight was injected 60 min prior to the whole-body PET/CT scan and after a fasting period of at least 6 h. Contrast-enhanced CT was performed immediately before PET. The PET acquisition time was dependent on body mass index. The CT and PET data were reconstructed in all three dimensions and the fused images interpreted by specialists in nuclear medicine and radiology, the results were evaluated, and a clinical report was made during hospitalisation.
FDG-PET/CT data and evaluation
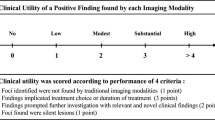
In the FDG-PET/CT scans each abnormal extra-cardiac finding was categorized as a suspected infectious focus, cancer, peripheral embolism, reactive finding, or other finding. Reactive findings were slightly positive PET foci, which the specialists in nuclear medicine and radiology did not consider to be of infectious or malignant nature. If a FDG-PET/CT finding had not been identified previously, suspected by other diagnostic modalities or mentioned in the medical records, it was considered a new finding. A new finding leading to further diagnostic work-up, a change in treatment, or a new additional diagnosis during 6 months of follow-up was considered clinically significant. Other findings were considered clinically insignificant. Whether the individual clinically significant finding was detected by PET, CT, or both modalities was evaluated by reviewing the scan results described by specialists in nuclear medicine and radiology. Findings mentioned exclusively in the PET report or exclusively in the CT report were designated new PET and new CT findings, respectively. For a lesion identified by both modalities, the focus was interpreted as a combined PET and CT finding.
Statistical analysis
Continuous data are presented as means ± standard deviation (SD) or as median with interquartile range (IQR), as appropriate. Categorical data are presented as n (%). Continuous variables were compared using the Student’s t test, and categorical variables using chi-squared. A two-sided p value < 0.05 indicated statistical significance. All analyses were performed using SPSS software version 22.0 (IBM Corp., USA).
Results
Patient characteristics
From three hospitals a total of 178 patients [(Rigshospitalet (80 patients), Hillerød Hospital (39 patients), and Herlev-Gentofte Hospital (59 patients)] diagnosed with IE were enrolled in the study. Baseline characteristics are shown in Table 1. The most frequent causative bacteria were streptococci, Staphylococcus aureus, and enterococci (Table 2). Cardiac surgery was performed in 71 (40%) of the patients during the disease-course. At clinical follow-up 6 months after discharge, five patients had experienced a relapse of IE, and in five other patients reinfection with other bacteria had occurred. Thirteen patients (7%) died during hospitalization and 31 (17%) had died 1-year after the diagnosis of IE.
FDG-PET/CT results
FDG-PET/CT was performed as part of the routine work-up at a median of 9 days (interquartile range [IQR] 10) after IE diagnosis. FDG-PET/CT identified 166 extra-cardiac foci in 114 patients; another 14 patients only had a cardiac focus and 50 (28%) patients had no lesions on FDG-PET/CT (Fig. 1). Among the 166 extra-cardiac findings, 52 (31%) were interpreted as infectious findings, 21 (13%) cancer, 7 (4%) peripheral embolisms, 60 (36%) reactive findings, and 26 (16%) other types of lesions. Other types of lesions included pleural effusion, pneumothorax, infarction, pericardial effusion, FDG-negative infiltrate, cholecystolithiasis, diverticulosis, fistula, aortic aneurysm, cholestasis, arthritis urica, hydronephrosis, enlarged prostate, polyp, and discus prolapse.The 166 foci were localized in the bones (n = 31; 16%), intestines (n = 30; 16%), lungs (n = 25; 13%), lymph nodes (n = 20; 10%), kidneys (n = 15; 8%), muscles (n = 13, 7%), spleen (n = 11; 6%), liver (n = 9; 5%), oral cavity (n = 7; 4%), and other localizations (n = 31; 16%).
In 24 patients (13%), the foci were known already from the patients’ medical history. Lesions described as reactive foci (n = 60) were not clinically significant according to the treating physician. Out of 166 extra cardiac findings, 74 foci (in 62 patients) were considered new and unknown extra-cardiac findings.
Clinical implications of FDG-PET/CT findings
Immediately changes in treatment after FDG-PET/CT evaluation
In the 62 patients with 74 new and unknown FDG-PET/CT findings, seven patients underwent an immediate change in treatment: two with spondylodiscitis (resulting in prolonged antibiotic treatment), one with infection in an endovascular stent graft in the aorta (resulting in prolonged antibiotic treatment), one with pleural effusion (resulting in pleural drainage), one with pulmonary embolism (treated with rivaroxaban), one with a suspected infection in a knee prosthesis (surgery), and one with hydronephrosis due to prostate hyperplasia (urinary catheterization). The suspected infection of a knee prosthesis was ruled out after further microbial investigation of the knee graft after surgery; thus, the patient had an unnecessary knee surgery due to a positive FDG-PET/CT scan.
Additional diagnostic work-up and changes in treatment
Twenty-nine patients with newly discovered foci required further investigations. The investigations included magnetic resonance imaging (MRI), CT, ultrasound, colonoscopy, and biopsy, among others. Based on these investigations, 17 patients (10%) were given a new diagnosis, resulting in new treatment for 11 patients: four with colon polyps (resected during the colonoscopy), two with cancer [one had surgery for adenocarcinoma in the colon and one chemotherapy for diffuse large B-cell lymphoma (Fig. 2)], three with spondylodiscitis (prolonged antibiotics), one mycotic aortic aneurysm (prolonged antibiotics), and one with epididymitis (antibiotic treatment). The six new diagnoses that did not alter treatment were two colon polyps, two tumours (one urothelial carcinoma and one thyroid adenoma; patients refused treatment), one fibroma, and one loose hip prosthesis.
A total of 17 (10%) patients were considered to have their therapy changed due to positive FDG-PET/CT results (five with spondylodiscitis, four with colon polyps, two with a cancer, one with an infection in an endovascular stent graft, one with a mycotic aortic aneurysm, one with pleural effusion, one with a pulmonary embolism, one with hydronephrosis, and one with epididymitis), 18 (10%) patients underwent further investigation that excluded suspicion of infection or malignancy, and 1 (1%) patient had potentially futile surgery.
Comparison of PET and CT results
Of the 62 patients with 74 new non-reactive foci, 13 (18%) foci were detected by PET only, 10 (14%) by CT only, and 51 (69%) by both modalities (PET and CT). Of the 29 patients with 34 foci, which required further investigation, 6 (18%) foci were detected by PET only, 1 (3%) by CT only, and 27 (79%) were discovered by both modalities. Among the 18 diagnoses that led to a change in treatment, 3 (17%) foci were discovered by PET only, 2 (11%) by CT only, and 13 (72%) by both modalities.
Value of FDG-PET/CT in subgroups of IE patients
Patients with IE can develop skin manifestations, which could be observed on the FDG-PET/CT. In this study, 19 (11%) patients had skin manifestations described as splinters. Of these, none had FDG uptake in the skin.
In Table 3, characteristics of patients with significant new findings are compared to characteristics in patients without clinically relevant findings. The vegetation size measured during echocardiography (echo) at time of IE diagnosis, did not reach level of significant. Older female patients and patients with non-streptococcal IE seemed to have a higher frequency of significant new findings, but it did not reach statistical significance. Only in the subgroup of female patients older than the median age of the cohort (67 years) with non-streptococcal IE, 53% had significant new findings, compared to 20% of patients with streptococcal IE, who were younger than 68 years of age (p = 0.02). Of the patients who had a change in treatment, 50% were > 67 years old and infected with non-streptococcal bacteria. None of the patients with a change in treatment were younger than 68 years old and infected with streptococcal IE.
Discussion
The present study is the largest and first multicentre trial to date describing the value of routine FDG-PET/CT undertaken in patients with Duke defined IE for detection of extra-cardiac foci. FDG-PET/CT identified new foci in 35% of patients and the findings led to a change in treatment in 10% of patients. It seems that female gender and possibly higher age and non-streptococci were associated with a higher detection rate of significant new findings. In 28% of the patients the scan did not disclose any findings, and in almost half of the patients the lesions revealed by FDG-PET/CT were already known or reactive findings. In addition, FDG-PET/CT led to unnecessary investigations in 18 (10%) patients due to false-positive findings.
One of the main FDG-PET/CT findings resulting in a change in treatment was spondylodiscitis. All patients with FDG-PET/CT-diagnosed spondylodiscitis had back pain recorded in their medical records, and further investigations would likely have been carried out anyway. MRI is an equally effective diagnostic tool as FDG-PET/CT for the diagnosis of spondylodiscitis [22, 23] but is less expensive and does not use radiation. Another relatively frequent finding was colon polyps (4%). Polyps are benign, but some have the potential to become malignant over time. In addition, polyps have been described as potential portals of entry for bacteraemia, and potentially secondary development of IE [24].
Unknown cancers were discovered in 4 (2%) patients. The incidence of cancer in assumingly healthy participants has been investigated in other studies. Tong et al. performed prospective screening of 1.572 (mean age 55 years) and Minamimoto et al. performed retrospective study on a four-year screening program of 155.456 (mean age unknown, a majority in the age group of 50 s and 60 s) on asymptomatic volunteers, and found 1.2–1.7% unknown cancers, 78–85% of which were detected by FDG-PET/CT [25, 26]. The mean age of the patients in our study was higher than in the other two studies. As the incidence of cancer increases with age, the incidence of FDG-PET/CT-identified cancers in our study seems to be of the same order of magnitude as observed in asymptomatic, apparently healthy populations.
Previous FDG-PET/CT studies in IE patients were smaller single center studies (n = 24–72 patients) (2.12–14.18–20). In a study by Ozcan et al. [12], FDG-PET/CT disclosed 114 extra-cardiac manifestations in 72 patients. Some of the findings were false-positive (44%) or false-negative (60%) and were identified by standard work-up. Asmar et al. [18] examined the clinical impact of FDG-PET/CT scanning of patients with endocarditis and reported that 15% of their cohort had clinically important, unknown lesions detected by the FDG-PET/CT scan. The baseline characteristics and results of these two studies were comparable those of the present study. From these two studies, it appears that further investigation of positive FDG-PET/CT findings is necessary in a large proportion of patients, and that half of the lesions represent false positive findings. A few studies have compared FDG-PET/CT and leucocyte single-photon emission computed tomography (SPECT)/CT. Rouzet et al. [27] and Lauridsen et al. [19] found leucocyte SPECT/CT more specific than FDG-PET/CT for the detection of IE and extra-cardiac infectious foci, but FDG-PET/CT had higher sensitivity. Lauridsen et al. [19] concluded that FDG-PET/CT has a greater clinical impact than leucocyte SPECT/CT. Based on the findings from our study and previous studies [2, 12,13,14, 18,19,20, 28] it seems that the clinical benefit of FDG-PET/CT screening of patients with IE for extra cardiac findings are limited. The majority of the clinical relevant findings were symptomatic and would probably have been found anyway. On the other hand, FDG-PET/CT does discover a wide variety of extra-cardiac lesions with only one imaging technique, some of the lesions were significant and led to a changed treatment. In the considerations of imposing screening with FDG-PET/CT in the for standard work-up in IE guidelines to identify extra-cardiac foci, we need to reflect on the clinical gain from the scan compared with false positive finding and unnecessary further investigations and treatment.
Limitations
This study has several limitations. First, not all patients diagnosed with IE who were admitted to the three hospitals underwent FDG-PET/CT during the clinical work-up as recommended in the hospitals’ clinical guidelines – which may have led to selection bias. This is probably the main limitation of this retrospective study. It is conceivable that the healthiest patients were not examined by FDG-PET/CT because undiscovered pathological foci were not suspected. Some of the most ill patients probably did not undergo FDG-PET/CT because it was assumed not to have any clinical impact on their general condition, which is supported by the observed low in-hospital mortality. Other patients may have been examined using a variety of different diagnostic tools, and the clinicians may have considered FDG-PET/CT to not provide additional diagnostic value. Having a control group of IE patients without a FDG-PET/CT examination to compare with the included patients in this study would have been valuable.
Second, not all the FDG-PET/CT examinations were performed at the same time after IE diagnosis; if all scans were performed the first day after IE diagnosis, the results might have differed. In our study, infectious lesions may have disappeared before the scan was performed—due to antibiotic treatment or may have become too small to be detected by FDG-PET/CT [15]. However, such lesions may not have been clinically significant, as they disappeared during the current treatment. Furthermore, in our study it did not seem that the day the FDG-PET/CT scan was performed influenced the results (Table 3).
Third, due to the nature of the retrospective research, we were not able to address if any false negative findings were present or the exact number of false positive findings. However, some of the positive FDG-PET/CT findings resulted in further investigations and in 18 (10%) patients the foci turned out to be false positive.
Finally, evaluation of the FDG-PET/CT results was subjective, and it was not the same healthcare professionals who treated all the patients.
This study showed that FDG-PET/CT as part of routine clinical work-up in IE patients is beneficial in some patients but also leads to unnecessary investigations in some patients. Application of FDG-PET/CT in the work-up for patients with IE should probably be focused on subgroups of IE patients. This study did not have enough power to establish which subgroup of patients could clinically benefit the most from FDG-PET/CT investigations. This study showed that older patients infected with bacterial species other than streptococci had the highest frequency of clinically significant findings. Further investigations of the benefit of FDG-PET/CT in different IE subgroups are needed.
Conclusion
In this retrospective cohort study, FDG-PET/CT performed routinely in IE patients led to the discovery of extra-cardiac foci in the majority of patients. FDG-PET/CT led to unnecessary investigations. In one in ten patients the findings had a clinical impact. The use of routine FDG-PET/CT for extra-cardiac foci in patients with IE is debatable.
References
Moreillon P, Que YA (2004) Infective endocarditis. Lancet 363:139–149
Bonfiglioli R, Nanni C, Morigi JJ, Graziosi M, Trapani F, Bartoletti M, Tumietto F, Ambrosini V, Ferretti A, Rubello D, Rapezzi C, Viale PL, Fanti S (2013) 18F-FDG PET/CT diagnosis of unexpected extracardiac septic embolisms in patients with suspected cardiac endocarditis. Eur J Nucl Med Mol Imaging 40:1190–1196
Rizzi M, Ravasio V, Carobbio A, Mattucci I, Crapis M, Stellini R, Pasticci MB, Chinello P, Falcone M, Grossi P, Barbaro F, Pan A, Viale P, Durante-Mangoni E (2014) Predicting the occurrence of embolic events: an analysis of 1456 episodes of infective endocarditis from the Italian Study on Endocarditis (SEI). BMC Infect Dis 14:230
Misra DP, Chowdury AC, Edavalath S, Aggarwal A, Kumar S, Agarwal V (2016) Endocarditis: the great mimic of rheumatic diseases. Trop Doct 46:180–186
Koslow M, Kuperstein R, Eshed I, Perelman M, Maor E, Sidi Y (2014) The unique clinical features and outcome of infectious endocarditis and vertebral osteomyelitis co-infection. Am J Med 127:669
Fabri J Jr, Issa VS, Pomerantzeff PM, Grinberg M, Barretto AC, Mansur AJ (2006) Time-related distribution, risk factors and prognostic influence of embolism in patients with left-sided infective endocarditis. Int J Cardiol 110:334–339
Thuny F, Di Salvo G, Belliard O, Avierinos J-F, Pergola V, Rosenberg V, Casalta J-P, Gouvernet J, Derumeaux G, Iarussi D, Ambrosi P, Calabro R, Riberi A, Colart F, Metras D, Lepidi H, Raoult D, Harle J-R, Weiller P-J, Cohen A, Habib G (2005) Risk of embolism and death in infective endocarditis: prognostic value of echocardiography. A prospective multicenter study. Circulation 112:69–75
Chu VH, Cabell CH, Benjamin DK Jr, Kuniholm EF, Fowler VG Jr, Engemann J, Sexton DJ, Corey R, Wang A (2004) Early predictors of in-hospital death in infective endocarditis. Circulation 109:1745–1749
Millar BC, Habib G, Moore JE (2016) New diagnostic approaches in infective endocarditis. Heart 102:796–807
Meller J, Sahlmann CO, Scheel AK (2007) 18F-FDG PET and PET/CT in fever of unknown origin. J Nucl Med 48:35–45
Bleeker-Rovers CP, de Kleijn EM, Corstens FH, van der Meer JW, Oyen WJ (2004) Clinical value of FDGPET in patients with fever of unknown origin and patients suspected of focal infection or inflammation. Eur J Nucl Med Mol Imaging 31:29–37
Ozcan C, Asmar A, Gill S, Thomassen A, Diederichsen AC (2013) The value of FDG-PET/CT in the diagnostic work-up of extra cardiac infectious manifestations in infectious endocarditis. Int J Cardiovasc Imaging 29:1629–1637
Van RJ, Hill EE, Gheysens O, Dymarkowski S, Herregods MC, Herijgers P, Peetermans WE, Mortelmans L (2010) (18)F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging 37:1189–1197
Amraoui S, Tlili G, Sohal M, Berte B, Hindie E, Ritter P, Ploux S, Denis A, Derval N, Rinaldi CA, Cazanave C, Jais P, Haissaguerre M, Bordenave L, Bordachar P (2016) Contribution of PET imaging to the diagnosis of septic embolism in patients with pacing lead endocarditis. JACC Cardiovasc Imaging 9:283–290
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL (2015) ESC Guidelines for the management of infective endocarditis. The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)
Gomes A, Glaudemans AW, Touw DJ, Van MJP, Willems TP, Maass AH, Natour E, Prakken NH, Borra RJ, Van GPP, Slart RH, Van AS, Sinha B (2017) Diagnostic value of imaging in infective endocarditis: a systematic review. Lancet Infect Dis 17:1–14
Chen W, Dilsizian V (2019) FDG PET/CT for the diagnosis and management of infective endocarditis: expert consensus vs evidence-based practice. J Nucl Cardiol 26:313–315
Asmar A, Ozcan C, Diederichsen AC, Thomassen A, Gill S (2014) Clinical impact of 18F-FDG-PET/CT in the extra cardiac work-up of patients with infective endocarditis. Eur Heart J Cardiovasc Imaging 15:1013–1019
Lauridsen T, Iversen KK, Ihlemann N, Hasbak P, Loft A, Berthelsen AK, Dahl A, Dejanovic D, Albrecht-Beste E, Mortensen J, Kjaer A, Bundgaard H, Bruun NE (2017) Clinical utility of 18F-FDG positron emission tomography/computed tomography scan vs. 99mTc-HMPAO white blood cell single-photon emission computed tomography in extra-cardiac work-up of infective endocarditis. Int J Cardiovasc Imaging 33:751–760
Kestler M, Munoz P, Rodriguez-Creixems M, Rotger A, Jimenez-Requena F, Mari A, Orcajo J, Hernandez L, Alonso JC, Bouza E (2014) Role of (18)F-FDG PET in PATIENTS WITH INFECTIOUS ENDOCARDITIS. J Nucl Med 55:1093–1098
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus AM, Thilen U, Lekakis J, Lengyel M, Muller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL (2009) Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J 30:2369–2413
Smids C, Kouijzer IJ, Vos FJ, Sprong T, Hosman AJ, de Rooy JW, Aarntzen EH, de Geus-Oei LF, Oyen WJ, Bleeker-Rovers CP (2017) A comparison of the diagnostic value of MRI and 18F-FDG-PET/CT in suspected spondylodiscitis. Infection 45:41–49
Fuster D, Tomas X, Mayoral M, Soriano A, Manchon F, Cardenal C, Monegal A, Granados U, Garcia S, Pons F (2015) Prospective comparison of whole-body (18)F-FDG PET/CT and MRI of the spine in the diagnosis of haematogenous spondylodiscitis. Eur J Nucl Med Mol Imaging 42:264–271
Delahaye F, M’Hammedi A, Guerpillon B, de Gevigney G, Boibieux A, Dauwalder O, Bouchiat C, Vandenesch F (2016) Systematic search for present and potential portals of entry for infective endocarditis. J Am Coll Cardiol 67:151–158
Tong J, Zou Y, Jiang J, Shi W, Tao R, Ye J, Lu Y, Jiang X, Wang W (2016) Cancer screening of asymptomatic individuals using 18F-FDG PET/CT in China: a retrospective study. Discov Med 22:181–188
Minamimoto R, Senda M, Jinnouchi S, Terauchi T, Yoshida T, Murano T, Fukuda H, Iinuma T, Uno K, Nishizawa S, Tsukamoto E, Iwata H, Inoue T, Oguchi K, Nakashima R, Inoue T (2013) The current status of an FDG-PET cancer screening program in Japan, based on a 4-year (2006–2009) nationwide survey. Ann Nucl Med 27:46–57
Rouzet F, Chequer R, Benali K, Lepage L, Ghodbane W, Duval X, Iung B, Vahanian A, Le Guludec D, Hyafil F (2014) Respective performance of 18F-FDG PET and radiolabeled leukocyte scintigraphy for the diagnosis of prosthetic valve endocarditis. J Nucl Med 55:1980–1985
Swart LE, Gomes A, Scholtens AM, Sinha B, Tanis W, Lam MGEH, van der Vlugt MJ, Streukens SAF, Aarntzen EHJG, Bucerius J, van Assen S, Bleeker-Rovers CP, van Geel PP, Krestin GP, van Melle JP, Roos-Hesselink JW, Slart RHJA, Glaudemans AWJM, Budde RPJ (2018) Improving the diagnostic performance of 18F-Fluorodeoxyglucose positron-emission tomography/computed tomography in prosthetic heart valve endocarditis. Circulation 138:1412–1427
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Holle, S.L.K., Andersen, M.H., Klein, C.F. et al. Clinical usefulness of FDG-PET/CT for identification of abnormal extra-cardiac foci in patients with infective endocarditis. Int J Cardiovasc Imaging 36, 939–946 (2020). https://doi.org/10.1007/s10554-020-01787-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01787-8