Abstract
First generation drug-eluting stents (DES) are associated with reduced in-stent restenosis but significant increased risk of very late stent thrombosis (VLST). The absence of polymer in DES systems may reduce the occurrence of VLST. Optic coherence tomography (OCT) has been used for stent analysis as a surrogate safety endpoint. This study aimed to assess the long-term follow up of strut apposition and tissue coverage of BioMatrix™ DES by OCT. 20 patients undergoing BioMatrix™ DES (n = 15) or S-Stent™ BMS (n = 5) implantation were followed for at least 5 years and evaluated by quantitative coronary angiography, intravascular ultrasound, and OCT. The difference between the stent types was evaluated by nonparametric Mann–Whitney U test while categorical variables were evaluated by Fisher exact test. Rates of in-stent late loss were similar between groups [0.40 (0.21;0.77) vs. 0.68 (0.66; 0.82) mm, p = 0.205, for BioMatrix™ and S-Stent™, respectively]. The vessel, stent and lumen volumes did not differ between groups. Patients treated with BioMatrix™ had significantly less stent obstruction [5.6 (4.4;9.7) vs. 28.6 (24.7;29.0) %, p = 0.001]. OCT analysis of 12 stents (Biomatrix™ = 9 and S-Stent™ = 3) demonstrated 126 (8.7 %) uncovered struts in the BioMatrix™ group compared to 23 (4.0 %) in the S-Stent™ group (p = 0.297), being the majority of them well apposed (117/126 and 21/23, respectively, p = 0.292). Only 9 (0.6 %) struts in the DES and 2 (0.4 %) struts in the BMS groups were simultaneously uncovered and malapposed (p = 0.924). BioMatrix™ DES was associated with lower rates of in-stent obstruction, and similar percentage of neointimal coverage on struts and of complete strut apposition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Drug-eluting stents (DES) have emerged as a strategy to prevent in-stent restenosis (ISR) [1–7]. First generation DES are associated with reduced ISR and need for target vessel revascularization (TVR) when compared to bare metal stents (BMS); but at the expense of a slightly but significant augment of the risk of very late stent thrombosis (VLST) [8–11]. Uncovered and malapposed struts, secondary to healing delay and positive remodeling, respectively, may be associated with both late (LST) (between 30 days and 1 year) and very late (>1 year) ST. It has been hypothesized that the absence of polymer in DES systems may enhance long-term safety by reducing the occurrence of late and very late ST. The second generation BioMatrix™ DES incorporates a biodegradable polymer that releases a potent anti-inflammatory agent (Biolimus A9) and is subsequently absorbed into local cells leaving only a BMS platform at the treated site. Given its high accuracy and reproducibility with precise analysis of complete strut apposition, optical coherence tomography (OCT) has been used as the modality of choice for stent analysis, as a potential surrogate safety endpoint. We sought to determine whether de use of BioMatrix™ DES is associated with higher rates of strut coverage and apposition in the very long-term follow up (>5 years), compared to S-Stent™ BMS.
Methods
Study population
All consecutive patients with previous angioplasty and stent implantation with either BioMatrix™ DES or S-Stent™ BMS performed at least 5 years before the enrollment were invited to participate in the study. All enrolled patients underwent OCT, quantitative coronary angiography (QCA) and intravascular ultrasound (IVUS) examination between August 2009 and May 2010.
The inclusion criteria were as follows: (1) patients aged between 18 and 80; (2) who were asymptomatic or with symptoms of stable angina; (3) who underwent an elective BioMatrix™ DES or BMS S-Stent at least 5 years before the enrollment; (4) and who agreed to participate in the study after detailed review of the protocol.
Exclusion criteria were: (1) acute coronary syndrome at the time of enrollment; (2) pregnant patients; (3) history of severe contrast allergy; (4) renal failure with creatinine levels >2,0 mg/dl or glomerular filtration rate <30 ml/min; (5) severe left ventricular dysfunction, defined by LV ejection fraction ≤30 % measured by ventriculography; (6) patients undergoing percutaneous revascularization for target-vessel lesion treated with either a new stent or only balloon angioplasty during the late follow up and (7) unsuitable lesions for OCT procedure (proximal lesion at 10 mm from ostium of each artery). The study protocol was approved by the institutional Ethics Committee and written informed consent was obtained from all patients.
Clinical and laboratorial evaluation
All patients underwent initial clinical examination, 12-lead electrocardiogram (EKG) and laboratorial evaluation (fasting plasma glucose, potassium, creatinine, hemogram and CK-MB). For the purpose of coronary risk factors assessment, diabetes mellitus was considered present if fasting plasma glucose concentration was higher than 126 mg/dl or if the patient was taking insulin or glucose-lowering medications; systemic hypertension was considered to be present if the blood pressure was higher than 140/90 mmHg, or if the patient was taking antihypertensive medication; and, finally, hyperlipidemia was considered to be present if a patient’s low-density lipoprotein level was >120 mg/dl or the patient was taking hypolipemiant drugs.
Following the angiogram, EKG, CK-MB sample and physical examination with special focus to arterial assess were repeated.
Angiographic analysis
The quantitative coronary angiography was performed using the Qangio-XA™ version 7.2 (Medis™, Leiden, The Netherlands). A single individual, who was blinded to the patient’s information and the type of stent used, measured the reference vessel diameter (RVD) and the minimal lesion diameter (MLD). The percentage of vessel stenosis was calculated. The late lumen loss (LL) was then calculated by the difference between the MLD at the time of stent implantation and at the long-term follow-up.
Intravascular ultrasound analysis
All IVUS images were obtained with Ilab™ (Boston Scientific™, Natick, Massachusetts, USA) and were analyzed by two different observers blinded to patients’ clinical background or angiographic lesion characteristics, and according to the ACC Clinical Expert Consensus [12], using the Echoplaque™ version 3.0 (Indec Systems™, Mountain View, California, USA) software. For each millimeter, the lumen, stent and external elastic membrane cross-section areas were evaluated. Vessel volume (VV), stent volume (SV) and lumen volume (LV) were calculated by the Simpson method.
In-stent neointimal hyperplasia (NIH) was measured by the difference between the stent volume and lumen volume.
In-stent neointimal hyperplasia index (NIHi) was calculated by dividing the NIH by stent extension (SE).
The percentage of stent obstruction (SO) was calculated by dividing the neointimal volume by the stent volume × 100.
Optical coherence tomography examination
For the OCT examination, a Light-Lab M3 TD-OCT™ (LightLab™, Westford, Massachusettes, USA) system was used. The occlusion balloon catheter was advanced distally to the region of interest over a conventional angioplasty guidewire (0.014″, 300 cm). The guidewire was then replaced by the OCT Image/Wire and the occlusion balloon catheter was withdrawn proximaly, leaving the Image/Wire distal to the segment of interest. For image acquisition, the balloon was inflated at 0.4–0.7 atm. and the coronary blood flow was removed by continuous flush of Ringer’s lactate solution via the end-hole of the occlusion balloon catheter at a flow rate of 3 ml/s. The pullback speed was 1–3 mm/s. Immediately after image acquisition, the balloon was deflated and complete coronary flow was restored.
Optical coherence tomography analysis
The OCT image acquisition has been previously described [13, 14]. All OCT images were analyzed by two independent investigators who were unaware of the clinical presentation and the stent type. All cross-sectional images were initially screened for quality assessment and excluded from analysis if any portion of the stent was out of the screen; or if the image had poor quality caused by residual blood, artifact, or reverberation. Quantitative strut level analysis and morphometric analysis were performed at every 0.5 mm interval along the entire target segment. Strut-level intimal thickness (SIT) was determined based on automated measurements performed from the center of the luminal surface of each strut blooming and its distance to the lumen contour [15]. Struts covered by tissue had positive SIT values, whereas uncovered or malapposed struts had negative SIT. Strut malapposition was defined when the negative value of SIT was higher than the sum of strut thickness plus abluminal polymer thickness, according to stent manufacturer specifications, plus a compensation factor of 20 μm to correct for strut blooming [16].
All quantitative coronary angiography and IVUS analysis were performed at Dante Pazzanese Institute of Cardiology. The OCT analyses were performed along with the Case Western Reserve University School of Medicine Cardiovascular Imaging Laboratory, Cleveland, Ohio, USA.
Statistical analyses
All statistical analyses were performed using SPSS™ (v.16.0) and SAS (v.9.2) software. Statistical significance was considered at p values <0.05. Categorical variables were expressed as counts and percentages, and continuous variables as mean ± standard deviation and/or median and interquartile range. For per-patient level comparison, the difference between two stent types was evaluated by nonparametric Mann–Whitney U test while categorical variables were evaluated by the Fisher exact test. Multilevel mixed model which can address random effects at frame and patient levels were used for binary and continuous outcomes comparison between the two stent types.
Results
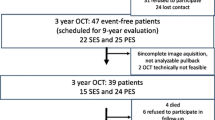
Forty-eight patients underwent either BioMatrix™ (n = 32) or S-Stent™ (n = 16) implantation between November 2003 and March 2004. Twenty patients (15 BioMatrix™ and 5 S-Stent™) were included in the study. Twenty-eight patients were excluded for the following reasons (N/BioMatrix™ DES/S-Stent™): death (5/3/2), severe renal impairment (1/0/1), severe left ventricular dysfunction (1/0/1), need of target-vessel revascularization with another new stent implantation (3/2/1), stent placed in the ostium of either right coronary artery or left descending artery (6/3/3), refuse of participation (5/3/2), and lost of follow up (7/3/4). All included patients underwent QCA, IVUS and OCT analysis between August 2009 and May 2010.
Baseline characteristics
No significant differences in the baseline characteristics were found between the groups. The mean age was 61.25 ± 6.58 years old and the average time between stent implantation and OCT examination was 69.31 ± 3.91 months. Although this did not reach statistical difference, previous acute myocardial infarction was more commonly seen in the Biolimus-A9 group (8 vs. 1, p = 0.055). Clinical data for the two groups are listed in Table 1.
Angiographic data
Angiographic characteristics are represented in Table 2. The stent distribution was similar among the coronary arteries, and proximal or mid segments. The mean diameter and length were 3.12 ± 0.22 mm (variation of 3.0–3.5 mm) and 19.10 ± 5.56 (variation of 14–28 mm), respectively. There were no significant differences in implanted stent diameter or length between the groups. Most patients had preserved left ventricular systolic function. One patient was found to have circumflex artery aneurysm in a segment treated with DES.
Immediate clinical results
No major procedure-related complications such as death, myocardial infarction or need of target-vessel revascularization were reported. No electrocardiographic abnormalities occurred and all patients were discharged after the pre-determined bed rest period.
Follow up data results
Quantitative coronary angiography findings
The results of initial and long-term QCA are represented in the Table 3. No significant differences in RVD, MLD and diameter stenosis (DS) were seen between the BioMatrix™ and the S-Stent™ groups.
IVUS findings
There were no significant differences in VV, SV and LV between the two groups. Patients treated with BioMatrix™ DES had significant less NHI, HNIi and SO compared to those treated with S-Stent™ (Table 4).
OCT findings
Optic coherence tomography findings are summarized in Table 5. Eight patients had more than 50 % of stent length with inappropriate image quality (4 residual blood, 1 out-of-screen portion, 2 artifacts, or 1 reverberation) and were excluded from the OCT analyses.
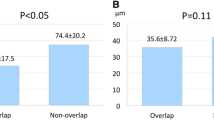
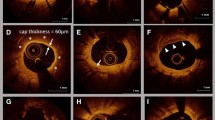
Optic coherence tomography images of 12 stents (Biomatrix™ = 9 and S-Stent™ = 3) from 12 patients, resulting in a total extension of 194.95 mm, 417 cross-section and 2,016 struts were analyzed. The overall rates of uncovered struts in the BioMatrix™ and S-Stent™ groups were 8.7 and 4.0 %, respectively (p = 0.297), being the majority of them well apposed (117/126 e 21/23, respectively, p = 0.292). Only 9 (0.6 %) struts in the DES and 2 (0.4 %) in the BMS groups were simultaneously uncovered and malapposed (p = 0.924). Among the BioMatrix™ patients, 55.6 % (5/9) had more than 95 % of covered struts and in only 1 (11.1 %) patient all struts were covered. Conversely, among the S-Stent™ patients, 66.7 % (2/3) had complete covered struts (p = 0.127). The area and volume analysis (stent, lumen and NIH) as well as the stenosis and obstruction percentages were similar between the groups.
Figures 1, 2 represent 2 cases: the first underwent a DES Biomatrix™ and the second a BMS S-Stent™. Both underwent coronary angiography, IVUS and CTO analysis.
Discussion
We demonstrated a high prevalence of tissue covered (91.3 %) and apposed (99.4 %) struts in patients with BioMatrix™ stents. This is the first study that evaluated the very long-term results of DES using the OCT. The longest DES follow-up with OCT analysis was published by Ishigami et al. [17] in which 60 patients undergoing sirolimus-eluting stent (SES) implant were classified into 3 groups: G1 (follow-up period <9 months, n = 27), G2 (9-24 months, n = 18), and G3 (>25 months, n = 15). The authors showed that the longer the follow-up, the higher the increase in mean neointimal area and neointimal thickness and the more reduction in the number of uncovered stent struts (G1: 14.8 %, G2: 11.7 %, and G3: 4.1 %, p < 0.001). However, only 17.6 % of implanted stents were completely covered by neointima at 3 years after implantation, even in the G3 period.
The BioMatrix™ stent elutes the sirolimus derivative Biolimus A-9 from a biodegradable polymer. Biolimus A-9 possesses enhanced both anti-inflammatory and anti-proliferative activity with an improved pharmacokinetic profile. Its efficacy have been proved by both QCA and IVUS evaluations of the STEALTH [18] and the LEADERS [19] studies. The in-stent late loss reported in the STEALTH trial was 0.26 ± 0.43 mm in the BES group compared to 0.74 ± 0.45 mm in the control group (p < 0.001) [18] At 5 years, we found a late lumen loss of 0.40 (0.21;0.77) mm in the Biolimus group, which was higher than the frequent mean average of most studies that used either sirolimus or similar anti-proliferative agents.
In spite of significant reduction in neointimal hyperplasia obtained with DES, this finding may be related to late catch-up, initially described with braquitherapy [20]. Recently, a few studies have also suggested the occurrence of this phenomenon with first generation DES. Park et al. [21] demonstrated that early lumen loss was higher in PES compared with SES (0.56 vs. 0.20 mm, p < 0.01), whereas delayed lumen loss occurring after the first angiographic follow-up was higher in SES (0.10 vs. 0.28 mm, p < 0.01), suggesting more prominent late catch-up in SES. In a serial angiographic study, Kuriyama et al. [22] reported a significant decrease in MLD between 8 and 2 years follow-up after SES implantation (2.56 ± 0.56 vs. 2.35 ± 0.71 mm, p < 0.001). Multivariate analysis demonstrated in-stent restenosis before SES implantation and MLD at 8 months follow-up as independent predictors of late restenosis.
The 9 months follow-up sub study of the LEADERS trial showed that the diameter stenosis in the BES group was non-inferior to the SES group (20.9 vs. 20.0–2.2 % difference [95 % CI-6.0–1.6], p for non-inferiority = 0.001, p for superiority = 0.26) [23]. Although no statistically significant, we found a numerically lower DS in the BES group (17.9 ± 9.7 vs. 26.2 ± 3.4 %, p = 0.089). Possibly a larger sample would result in different late lumen loss and DS results.
Chamie et al. [24] demonstrated a non-significant increase in in-stent late loss from 0.10 ± 0.18 to 0.15 ± 0.30 mm (p = 0.38) at 8 and 20 months following SES implantation. Similarly, a slight increase in the percent in-stent hyperplasia obstruction (1.03 ± 2.13 to 1.76 ± 1.87 %, p = 0.12) was detected. We found a lower percentage of stent obstruction in the BioMatrix™ group compared to S-Stent™ group after 5 years follow up [5.6 (4.4; 9.7) vs. 28.6 (24.7; 29.0) %, p = 0.001], which is in agreement to previously published data.
The safety and efficacy of the BES stent was supported by the 12 months clinical follow-up of the LEADERS trial, which showed no differences in the primary endpoint (composite of cardiac death, myocardial infarction and clinical-indicated target vessel revascularization) between BES and SES (10.6 vs. 12.0 %, HR:0.88, 95 % CI:0.66–1.17, p = 0.37). Rates of cardiac death, myocardial infarction and clinically-indicated TVR were similar for BES and SES and there was no difference in the incidence of stent thrombosis between the groups [25]. In 2010, Serruys reported maintenance of the results. Importantly, the occurrence of very late thrombosis was found to be an uncommon event (BES 0.2 % vs. SES 0.9 %, p = 0.43). In 2011, Stefanini et al. [26] published the LEADERS study 4 years follow up, and showed that biodegradable polymer BES was non-inferior to durable polymer SES and, by reducing the risk of cardiac events associated with very late ST, might improve long-term clinical outcomes for up to 4 years compared with durable polymer SES.
Capodanno et al. [27] performed both IVUS and OCT in 20 patients, 6 months following stent implantation and demonstrated measurements of stent length of 16.3 ± 3.0 mm and 16.2 ± 3.8 mm by IVUS and OCT, respectively (p = 0.82) with similar to nominal length (16.3 ± 3.3 mm). Luminal area in the OCT image set was lower than that obtained in the corresponding IVUS image set (3.83 ± 1.60 vs. 4.05 ± 1.44 mm2, p < 0.001), while stent area was significantly higher when measured by OCT (6.61 ± 1.39 vs. 6.17 ± 1.07 mm2, p < 0.001). The percentage of tissue coverage measured by IVUS was lower than that measured in the corresponding OCT image sets (35.5 ± 16.4 vs. 43.4 ± 16.1 %, p < 0.001).
We showed overall rates of uncovered struts in the BioMatrix™ and S-Stent™ groups of 8.7 and 4.0 %, respectively (p = 0.297), being the majority of them well apposed (117/126 e 21/23, respectively, p = 0.292). Only 0.6 % struts in the DES and 0.4 % in the BMS groups were simultaneously uncovered and malapposed (p = 0.924). Among the BioMatrix™ patients, 55.6 % had more than 95 % of covered struts and in only 1 (11.1 %) patient all struts were covered. On the other hand, among the S-Stent™ patients, 66.7 % had complete covered struts (p = 0.127). Therefore, there were 91.3 % covered struts and, among the uncovered struts (8.7 %), only 0.6 % were found to be malapposed. Previous studies have reported uncovered struts rates varying between 0.1 % (ZES, 3 months) and 14.8 % (SES < 9 months) and malapposed rates between 0.08 % (ZES, 9 months) and 1.7 ± 4.5 % (SES, 9 months). We believe that these differences are consequences of both the type of stent used and the follow up period, but the methodology certainly might influence the results. Once it is a new technology, there is no universal standard imaging acquisition method, with frequent variations in the type of equipment and optic fiber traction velocity. Our analyses were performed in an experienced and specialized OCT research laboratory.
We found higher rates of uncovered struts after 5 years follow up (8.7 %) when compared to the only two previous studies that evaluated Biolimus stents by OCT (1.8 % after 9 months and 0.41 % after 6 months follow up). Although Biolimus was used in all studies, we used BioMatrix™ instead of BioMatrix Flex™ used in other studies which may have affected the results.
Also, in spite of the high OCT resolution (10–20 μm in our study) and accuracy when compared to histological analysis, cover tissues with fewer thicknesses (<10 μm) may not be visible by the method.
Limitations
This study has a few limitations. First, the relatively small population could have affected the results. However, the primary objective of this analysis was the strut level evaluation. Although only 12 stents were studied, this resulted in an analysis of a total of 194.95 mm stent extension, 417 frames and 2.016 struts. Second, the OCT analysis was performed only 5 years after the stent implantation. Even though this had no influence in the tissue coverage analysis, it is not possible to distinguish whether the late malapposition was previously present or if it was acquired as a result of positive remodeling during the follow up. And third is the resolution of OCT. Although the spatial resolution of OCT is the highest of all available in vivo intravascular imaging modalities, a single layer of endothelial cells covering stent struts are still bellow OCT’s axial resolution. The M3 TD-OCT™ (LightLab™, Westford, Massachusetts, USA) software was used for this analysis. The new available C7XR FD-OCT™ system with better images acquisition and better axial resolution might lead to different results.
Conclusions
When compared to S-Stent™ BMS, the BioMatrix™ DES was associated with lower rates of in-stent obstruction, and similar percentage of neointimal coverage on struts and of complete strut apposition.
Abbreviations
- DES:
-
Drug-elluting stents
- ISR:
-
In-stent restenosis
- TVR:
-
Target vessel revascularization
- BMS:
-
Bare metal stent
- VLST:
-
Very late stent thrombosis
- LST:
-
Late stent thrombosis
- ST:
-
Stent thrombosis
- OCT:
-
Optical coherence tomography
- QCA:
-
Quantitative coronary angiography
- IVUS:
-
Intravascular ultrasound
- EKG:
-
Electrocardiogram
- RVD:
-
Reference vessel diameter
- MLD:
-
Minimal lesion diameter
- LL:
-
Lumen loss
- VV:
-
Vessel volume
- ST:
-
Stent volume
- LV:
-
Lumen volume
- NIH:
-
In-stent neointimal hyperplasia
- NIH:
-
In-stent neointimal hyperplasia index
- SE:
-
Stent extension
- SO:
-
Stent obstruction
- DS:
-
Diameter stent
- SES:
-
Sirolimus-eluting stent
- PES:
-
Paclitaxel-eluting stent
- CI:
-
Confidential interval
- NS:
-
Non significant
- SD:
-
Standard deviation
- IQ:
-
Interquartile
- PCI:
-
Percutaneous coronary intervention
References
Sousa JE, Costa MA, Abizaid A, Abizaid AS, Feres F, Pinto IM et al (2001) Lack of neointimal proliferation after implantation of sirolimus-coated stents in human coronary arteries: a quantitative coronary angiography and three-dimensional intravascular ultrasound study. Circulation 103(2):192–195 [Epub 2001/02/24]
Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M et al (2002) A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med 346(23):1773–1780 [Epub 2002/06/07]
Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C et al (2003) Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 349(14):1315–1323 [Epub 2003/10/03]
Stone GW, Ellis SG, Cox DA, Hermiller J, O’Shaughnessy C, Mann JT et al (2004) A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med 350(3):221–231 [Epub 2004/01/16]
Serruys PW, Kutryk MJ, Ong AT (2006) Coronary-artery stents. N Engl J Med 354(5):483–495 [Epub 2006/02/03]
Stone GW, Moses JW, Ellis SG, Schofer J, Dawkins KD, Morice MC et al (2007) Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med 356(10):998–1008 [Epub 2007/02/14]
Kastrati A, Mehilli J, Pache J, Kaiser C, Valgimigli M, Kelbaek H et al (2007) Analysis of 14 trials comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med 356(10):1030–1039 [Epub 2007/02/14]
Garg S, Serruys P (2010) Benefits of and safety concerns associated with drug-eluting coronary stents. Expert Rev Cardiovasc Ther 8(3):449–470 [Epub 2010/03/13]
Nordmann AJ, Briel M, Bucher HC (2006) Mortality in randomized controlled trials comparing drug-eluting vs. bare metal stents in coronary artery disease: a meta-analysis. Eur Heart J 27(23):2784–2814 [Epub 2006/10/06]
Camenzind E, Steg PG, Wijns W (2007) Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation 115(11):1440–1455 Discussion 55. [Epub 2007/03/09]
Lagerqvist B, James SK, Stenestrand U, Lindback J, Nilsson T, Wallentin L (2007) Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med 356(10):1009–1019 [Epub 2007/02/14]
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ et al (2001) American college of cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American college of cardiology task force on clinical expert consensus documents. J Am Coll Cardiol 37(5):1478–1492 [Epub 2001/04/13]
Guagliumi G, Sirbu V (2008) Optical coherence tomography: high resolution intravascular imaging to evaluate vascular healing after coronary stenting. Catheter Cardiovasc Interv 72(2):237–247 [Epub 2008/07/26]
Takarada S, Imanishi T, Liu Y, Ikejima H, Tsujioka H, Kuroi A et al (2010) Advantage of next-generation frequency-domain optical coherence tomography compared with conventional time-domain system in the assessment of coronary lesion. Catheter Cardiovasc Interv 75(2):202–206 [Epub 2009/11/26]
Guagliumi G, Costa MA, Sirbu V, Musumeci G, Bezerra HG, Suzuki N et al (2011) Strut coverage and late malapposition with paclitaxel-eluting stents compared with bare metal stents in acute myocardial infarction: optical coherence tomography substudy of the harmonizing outcomes with revascularization and stents in acute myocardial infarction (HORIZONS-AMI) trial. Circulation 123(3):274–281 [Epub 2011/01/12]
Guagliumi G, Musumeci G, Sirbu V, Bezerra HG, Suzuki N, Fiocca L et al (2010) Optical coherence tomography assessment of in vivo vascular response after implantation of overlapping bare-metal and drug-eluting stents. JACC Cardiovasc interv 3(5):531–539 [Epub 2010/05/22]
Ishigami K, Uemura S, Morikawa Y, Soeda T, Okayama S, Nishida T et al (2009) Long-term follow-up of neointimal coverage of sirolimus-eluting stents–evaluation with optical coherence tomography. Circ J 73(12):2300–2307 [Epub 2009/10/01]
Grube E, Hauptmann KE, Buellesfeld L, Lim V, Abizaid A (2005) Six-month results of a randomized study to evaluate safety and efficacy of a Biolimus A9 eluting stent with a biodegradable polymer coating. EuroIntervention 1(1):53–57 [Epub 2005/05/01]
Windecker S, Serruys PW, Wandel S, Buszman P, Trznadel S, Linke A et al (2008) Biolimus-eluting stent with biodegradable polymer versus sirolimus-eluting stent with durable polymer for coronary revascularisation (LEADERS): a randomised non-inferiority trial. Lancet 372(9644):1163–1173 [Epub 2008/09/04]
Feres F, Munoz J, Abizaid A, Staico R, Kuwabara M, Mattos L et al (2005) Angiographic and intravascular ultrasound findings of the late catch-up phenomenon after intracoronary beta-radiation for the treatment of in-stent restenosis. J Invasive Cardiol 17(9):473–477 [Epub 2005/09/08]
Park KW, Kim CH, Lee HY, Kang HJ, Koo BK, Oh BH et al (2010) Does “late catch-up” exist in drug-eluting stents: insights from a serial quantitative coronary angiography analysis of sirolimus versus paclitaxel-eluting stents. Am Heart J 159(3):446–453 e3. [Epub 2010/03/10]
Kuriyama N, Kobayashi Y, Nakama T, Mine D, Nishihira K, Shimomura M et al (2011) Late restenosis following sirolimus-eluting stent implantation. JACC Cardiovasc Interv 4(1):123–128 [Epub 2011/01/22]
Barlis P, Regar E, Serruys PW, Dimopoulos K, van der Giessen WJ, van Geuns RJ et al (2010) An optical coherence tomography study of a biodegradable vs. durable polymer-coated limus-eluting stent: a LEADERS trial sub-study. Eur Heart J 31(2):165–176 [Epub 2009/11/06]
Chamie D, Abizaid A, Costa JR, Jr., Feres F, Almiro da Silva JF, Mattos LA et al (2010) Serial angiographic and intravascular ultrasound evaluation to interrogate the presence of late “catch-up” phenomenon after cypher((R)) sirolimus-eluting stent implantation. Int J Cardiovasc Imaging 27(6):867–874 [Epub 2010/11/18]
Garg S, Sarno G, Serruys PW, de Vries T, Buszman P, Linke A et al (2010) The twelve-month outcomes of a biolimus eluting stent with a biodegradable polymer compared with a sirolimus eluting stent with a durable polymer. EuroIntervention 6(2):233–239 [Epub 2010/06/22]
Stefanini GG, Kalesan B, Serruys PW, Heg D, Buszman P, Linke A et al (2011) Long-term clinical outcomes of biodegradable polymer biolimus-eluting stents versus durable polymer sirolimus-eluting stents in patients with coronary artery disease (LEADERS): 4 year follow-up of a randomised non-inferiority trial. Lancet 378(9807):1940–1948 [Epub 2011/11/15]
Capodanno D, Prati F, Pawlowsky T, Cera M, La Manna A, Albertucci M et al (2009) Comparison of optical coherence tomography and intravascular ultrasound for the assessment of in-stent tissue coverage after stent implantation. EuroIntervention 5(5):538–543 [Epub 2010/02/10]
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Staico, R., Costa, M.A., Chamié, D. et al. Very long-term follow-up of strut apposition and tissue coverage with Biolimus A9 stents analyzed by optical coherence tomography. Int J Cardiovasc Imaging 29, 977–988 (2013). https://doi.org/10.1007/s10554-013-0188-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-013-0188-8