Abstract
Background
Understanding of the physical activity and sedentary behavior of cancer survivors is limited by reliance on self-reported data. Here, we report the correlates, and patterns of accumulation, of physical activity (light, and moderate-vigorous; MVPA) and sedentary behavior, in colon cancer survivors, using accelerometer-based assessments.
Methods
Colon cancer survivors from Alberta, Canada (n = 92), and Western Australia (n = 93) (overall response rate = 21 %) wore an Actigraph® GT3X+ accelerometer for seven consecutive days and completed a questionnaire in 2012–2013. Accelerometer data (60 s epochs) were summarized using Freedson activity cutpoints and were adjusted for wear time. Linear regression analyses, conducted 2014–2015, examined correlates for different intensities of activity.
Results
Younger age, being employed, higher family income, and lower BMI were significantly correlated with MVPA, while gender, educational attainment, and BMI were correlated with light-intensity physical activity. Gender, comorbidities, and BMI were correlated with sedentary time. MVPA did not vary by day of the week, whereas the remaining time (as a sedentary/light ratio) showed significant variation, with Saturdays being more sedentary than average. When considering time of day, we found that evenings were when the likelihood of both MVPA and sedentary time was highest.
Conclusions
The low level of MVPA and high volume of sedentary time demonstrated by these objective data highlight the need for intervention in colon cancer survivors. The correlates and accumulation patterns described by this study may better inform interventions and translational research designed to increase physical activity and reduce sedentary behavior in colon cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colon cancer survivorship is associated with decrements in health status and an increased risk of death from noncancer causes [1]. However, modifiable health behaviors can redress such morbidity. Participating in moderate- to vigorous-intensity physical activity (MVPA) after diagnosis has been associated with prolonged survival [2–5], diminished treatment side effects, and enhanced health-related quality of life [6–8]. Sedentary behavior is another risk factor that is additional to, and distinct from, the hazards of too little MVPA [9]. Sedentary behaviors are defined by low energy expenditure and a sitting or lying posture [10]. For colon cancer survivors, sedentary behavior has been associated with poorer survival [11], increased risk of heart disease [12], increased body mass index (BMI) [13], and lower quality-of-life scores [14].
Research indicates that adults spend the vast proportion of their day sitting or in light-intensity physical activity; however, these behaviors are difficult to measure accurately and reliably by questionnaire [15]. Objective monitoring devices, such as accelerometers, provide detailed data on the frequency, intensity, and duration of physical activities performed across the day, and how these activities are accumulated over the course of the day and across the week. A clearer understanding of the physical activity and sedentary behavior of cancer survivors is important for making recommendations about frequency, intensity, and duration necessary to enhance health outcomes. It is also important to understand how these behaviors are accumulated throughout the day, so as to inform future intervention studies.
Few published studies have objectively characterized the sedentary time of cancer survivors. Two previous studies using accelerometer data from the National Health and Nutrition Examination Survey (NHANES, 2005–2006) examined the physical activity and sedentary time of breast [16] and prostate cancer survivors [17]. The results of these studies suggest that the physical activity of cancer survivors derived from self-reported measures appears to be substantially inflated relative to objective assessments, although the extent to which this is over-reporting of activity or under-detection by the devices is not clear. In the NHANES studies, breast cancer survivors recorded 4 min of MVPA per day, on average; for prostate cancer survivors, it was 6 min [16, 17]. A more recent, prospective study used accelerometers to quantify activity in breast cancer survivors and concluded that this population is highly sedentary across the first year following primary treatment for breast cancer. At each three-monthly assessment over the year, women recorded nearly 11 h of sedentary time per day (78 % of their recorded waking hours), but only between 14 and 16 min per day of moderate-vigorous physical activity [18].
We recently published the first study to document objectively assessed MVPA and sedentary time among colon cancer survivors, examining associations with health-related quality of life and fatigue [8]. Here, we present the distributions and correlates of a range of accelerometer-derived estimates of physical activity and sedentary time for colon cancer survivors. Describing the characteristics of colon cancer survivors who are most/least likely to engage in these behaviors may facilitate delivery of interventions to those most likely to benefit. We also explore the patterns of MVPA and the degree to which remaining accelerometer wear time is spent sedentary or engaged in light physical activity, over the days of the week and across hours of the day. Such insights may inform optimal timing for when interventions might be targeted. Specifically, the aims of this study are to: (1) describe the distribution of accelerometer-derived physical activity (light, moderate, vigorous, MVPA, and MVPA accrued in bouts of 10 min or more) and sedentary time (including sedentary time accrued in prolonged bouts of at least 20 or 30 min); (2) to identify the sociodemographic and medical correlates of MVPA, light-intensity physical activity, and sedentary time; and (3) to examine daily and hourly patterns of accelerometer-derived MVPA and sedentary time/light physical activity balance, in a sample of colon cancer survivors recruited from two population-based registries.
Methods
Recruitment procedures
The methods of this study have previously been reported [8]. In brief, we recruited colon cancer survivors through the Alberta Cancer Registry (Canada) and the Western Australian Cancer Registry (Australia). The study was approved by Ethics Boards at Alberta Health Services (Alberta Cancer Research Ethics Committee), Athabasca University, Department of Health Western Australia and The University of Western Australia. The cancer registries identified individuals with histologically confirmed stage I–III diagnosis of a first, primary colon cancer. Eligibility criteria included: being between the ages of 18 and 80; having completed cancer treatment; speaking English; being able to provide written informed consent; and being able to wear an accelerometer for seven consecutive days. Upon providing consent, participants were each sent a package containing a written questionnaire, an Actigraph GT3X+® tri-axial accelerometer (Actigraph, LLC, Pensacola, Florida), written instructions describing how to use the accelerometer, and a postage-paid envelope to return the questionnaire and accelerometer to the study team.
Measures
Physical activity and sedentary time were derived from data recorded by an accelerometer. Participants wore the accelerometer on an elastic belt over their right hip during waking hours for seven consecutive days. Accelerometer data were downloaded using ActiLife 3.2.2 software and summarized using SAS 9.2. To be considered valid, days of data collection required at least 600 min (10 h) of wear time and no excessive counts (>20,000 counts per minute; cpm). Nonwear periods were excluded from analyses; these were defined as intervals of at least 60 consecutive minutes of zero counts, with allowance for up to 2 min of observations of <50 cpm within the nonwear interval [19].
Activity counts (vertical) were categorized as: sedentary (<100 cpm) [20], light-intensity (100–1,951 cpm) [21], moderate-intensity (1,952–5,724 cpm) [21], or vigorous-intensity physical activity (≥5,725 cpm) [21], using data recorded in 60-s epochs. Moderate- and vigorous-intensity physical activities were also collapsed (≥1,952 cpm) and MVPA examined as total time accumulated, time in strict ‘bouts’ of ten consecutive minutes or more with no allowance for an interruption, and time in modified bouts (ten consecutive minutes of more with an allowance of up to 10-min interruption). Prolonged bouts of sedentary time were defined as: 20 consecutive minutes or more, corresponding to clinical changes in cardio-metabolic biomarkers [22]; and, 30 consecutive minutes or more, corresponding to occupational health and safety guidelines [23].
Date of diagnosis (month, year), tumor site, and stage were obtained from the cancer registries. Demographic and medical information including sex, age, employment, marital status, family income, education, height, and weight, cancer therapies received, and comorbid conditions were collected via the self-administered questionnaire sent to participants. All accelerometer and self-reported data were collected in 2012–2013.
Statistical analyses
Analyses were conducted in 2014–2015 using Stata version 12 (Statacorp, College Station, TX, USA) and SPSS version 22 (IBM Corporation, USA). Significance was set as p < 0.05 (two-tailed).
Sample characteristics were described as mean and standard deviation for continuous variables, and count and percentage for categorical variables. Median, plus 25th and 75th percentiles, was also reported for moderate-intensity physical activity, vigorous-intensity physical activity, and MVPA. Correlations between time spent at each activity intensity level were examined using Spearman’s or Pearson’s correlation coefficients (as appropriate).
Linear regression was used to identify the independent correlates of MVPA, light activity, and sedentary time, assuming a normal distribution for light and sedentary variables and a gamma distribution (with a log link) for MVPA. Models initially included a broad range of sociodemographic (sex, age, employment status, marital status, household income, educational attainment, smoking status, BMI) and medical characteristics (time from diagnosis, stage of disease, cancer therapies received, number of comorbid conditions). Variables not significant at p < 0.2 were eliminated.
Patterns by hour of the day, and day of the week, in sedentary/light balance (i.e., sedentary/light ratio) and MVPA (minutes/hour or minutes/day, accordingly) were examined using generalized linear mixed models (in SPSS) that accounted for repeated measures and adjusted for relevant compositional differences (i.e., who provided data for particular days or times). All sociodemographic characteristics that were previously identified as associated at p < 0.2 with MVPA (MVPA models), light activity, or sedentary time (sedentary/light ratio models) were adjusted. Log transformation, a normal distribution, and identity link were used for daily and hourly sedentary/light ratio. A gamma distribution and log link were used for daily MVPA, and because many hours of the day involved no MVPA, a binary distribution with a logit link was used to model the odds (for each hour) of engaging in any MVPA. Using marginal means from these models, we reported whether any days of the week or hours of the day were significantly above or below average (based on the overall grand mean), with significance adjustment for multiple comparisons (Sidak method).
Results
Participant characteristics
A total of 927 eligible colon cancer survivors received study invitation packages, and 197 responded to this initial mail-out (overall response rate of 21 %). Within the Australian component of the sample, no differences by sex, age group, or time from diagnosis were noted between study participants and nonparticipants (data were not obtained for Canadian participants). One hundred and eighty-five participants completed the questionnaire and had valid accelerometer data. The demographic, health, and medical characteristics of participants are presented in Table 1. Of note , only 9 % of participants reported that they had been provided with advice about physical activity by their doctor(s). Pooling the samples appeared reasonable as no significant or large differences were observed between Canadian and Australian participants, except for time from diagnosis (16.9 vs 20.6 months) and employment status (31.5 vs 45.6 % working, p = 0.046). Notably, Canadian participants did not differ significantly from Australian participants in sedentary time (mean difference = −5.6, 95% CI −32.5, 21.2 min/day, p = 0.680), light-intensity physical activity (mean difference = 6.2, 95% CI −19.0, 31.3 min/day, p = 0.630), or MVPA (RR = 0.98, 95% CI 0.77, 1.24, p = 0.838).
Average daily physical activity and sedentary time are summarized in Table 2. Light-intensity physical activity showed moderate correlation with MVPA (Spearman’s ρ = 0.42) and a strong inverse correlation with sedentary time (Pearson’s r = −0.74). The correlation between MVPA and sedentary time was inverse and moderate (Spearman’s ρ = −0.29).
Correlates of light-intensity physical activity, MVPA, and sedentary time are presented in Table 3. Being male (p = 0.003), having more comorbidities (p = 0.045), and having a higher BMI (p = 0.017) were significantly associated with greater sedentary time . Sedentary time was significantly lower in women than in men (on average, 42 min/day), higher among participants with two or more comorbidities versus none (34 min/day), and higher for obese participants than those in the normal BMI category (44 min/day). Greater light activity was significantly associated with being female (p < 0.001), lower educational attainment (p = 0.018), and lower BMI (p = 0.031). On average, light activity was approximately 46 min/day higher in women than in men, nearly 1 h lower in university graduates than those with a less than secondary school education, and lower by 36 min/day in participants with an obese versus a normal BMI classification. MVPA was significantly associated with age (2 % lower per year of age, p = 0.014), family income (83 % higher in those earning ≥$80,000 than those earning <$40,000, p < 0.001), employment (44 % lower among participants not working compared with working, p = 0.006), and BMI (twofold lower in those with an obese versus normal BMI, p < 0.001).
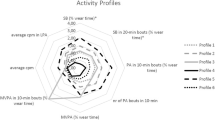
Figure 1 shows the breakdowns of colon cancer survivors’ sedentary/light balance (a, b) and MVPA time (c, d) by day of the week (a, c) and hour of the day (b, d). Sedentary/light balance varied significantly by day of the week (p = 0.005), specifically with the sedentary/light ratio being approximately 10 % lower on Saturdays than the overall average (RR = 0.91, 95% CI 0.84, 0.98, p = 0.007). There was also a nonsignificant tendency for Sundays to have an 8 % higher than average sedentary/light ratio (RR = 1.08, 95% CI 1.00, 1.16, p = 0.063). MVPA did not differ significantly by day of the week (p = 0.771), and all deviations from the mean were small (2 min/day or less) with tight confidence intervals (no more than ±6 min/day).
Sedentary/light ratio varied significantly across the day (p < 0.001), with the hours from 6 pm onward and before 8 am being significantly less sedentary than average, the hours between 8 am and 3 pm being significantly more sedentary than average, with the remaining hours not deviating significantly from the overall average across the day. Nonetheless, all hours of the day tended to be more sedentary than light; the smallest sedentary/light ratio observed was for 11–11:59 am (1.3, 95% CI 1.0, 1.6), and the highest was for ≥10 pm (3.5, 95% CI 2.8, 4.5).
MVPA varied significantly by hour of the day (p < 0.001). Overall, 63 % (95% CI 60, 65 %) of hours involved some MVPA. The percentage of hours involving physical activity was significantly below average from 10 am to 3 pm (lowest at 11–11:59 am = 49 %, 95% CI 45 %, 53 %), significantly above average from 4 to 4:59 pm and ≥6 pm (highest = 9–9:59 pm = 76 %, 95% CI 73 %, 79 %), and not significantly different to the average at other times.
Discussion
This study provides the first comprehensive description of how colon cancer survivors (on average, 19 months post-diagnosis) allocate their time across different intensities of physical activity, and sedentary behavior. Participants in this study spent approximately 23 min per day (equivalent to 161 min per week) in MVPA. This figure is slightly higher than self-reported estimates of physical activity from previous studies: estimates ranged from 147 min per week for males and 104 min per week for females in a large, population-based cohort of Australian colorectal cancer survivors [24] to 89 min per week for colorectal cancer survivors from Canada [25]. However, it is not possible to determine the extent to which the difference relates to the study, or to the measure used. Studies show limited agreement between accelerometer and self-report physical activity data [26]; there are fundamental differences in how physical activity is measured by each methodology. Accelerometers measure activity at a particular point in time; within our study (using a 60-s epoch), this is at a minute-by-minute level across virtually the entire waking day. Because physical activities are generally stop–start in their nature, questionnaires operationalize physical activity by having respondents report the main type of activity they have engaged in over some specific period of time. In most instances, there is movement above and below the nominated specific intensity of physical activity during that period.
The extent to which these figures indicate colon cancer survivors’ activity appears sufficient relative to guidelines is contentious. In our study, just over half of the participants met physical activity guidelines. Based on all MVPA, 52 % of colon cancer survivors accrued at least 150 min per week. The figures for guideline compliance are much lower when considered (as is sometimes done) based on MVPA occurring in bouts of at least 10 min, defined strictly (16 %). These low figures largely relate to problems capturing bouts of physical activity accurately, and in a meaningful way via accelerometer. Being engaged in activities considered ‘moderate’ or ‘vigorous’ for ten or more minutes at a time is fundamentally different to being continuously active at a moderate or higher intensity for ten or more minutes at a time, because many activities are inherently stop–start in nature (e.g., tennis, soccer). Further, the relative benefits of accruing MVPA sporadically versus in bouts of 10 min or more are still being debated [27]. Regardless, all estimates examined tend to suggest many colon cancer survivors do not reach recommended physical activity levels.
Study participants spent an average of over 5 h performing light-intensity activities, and eight and three quarter hours sedentary each day. The relative volume of these behaviors, which account for 97 % of all waking hours that were monitored by accelerometer, highlights the importance of understanding their impact on health outcomes. Only one previous study (the CanChange trial) has estimated total sedentary time among colorectal cancer survivors. This study found that colorectal survivors self-reported just over 6 h per day of sedentary behavior [28]. To date, there have been no published estimates of light-intensity physical activity within this population.
BMI was the only sociodemographic attribute associated significantly with all three activity outcomes. Sedentary time and light activity (which were strongly inversely correlated) showed some similarities in their independent correlates, such as being significantly associated with both gender and BMI (p < 0.05) and models for retaining both comorbidities (significant only for sedentary) and education (significant only for light). The variables that we found were correlated with MVPA—age, income, employment, and BMI—and were all/sometimes also identified in an earlier study that examined factors associated with colorectal cancer survivors meeting national physical activity guidelines [24]. Due to the small sample size, many of the nonsignificant comparisons had wide confidence intervals encompassing large differences. The absence of a significant difference is not an indication that activity was equal across sociodemographic characteristics that were not identified as independent correlates of activity.
We examined the distribution of physical activity and sedentary time across the week and across the day in order to better understand how these behaviors are accumulated, and potentially to identify days or times of day to target in future interventions. There were no significant or large differences by day of the week in MVPA. The remaining time (as a sedentary/light ratio) showed significant differences across day of the week, with Saturdays being significantly more sedentary than average and Sundays tending to be more sedentary than average (but not statistically significant). Both MVPA and the balance of the remaining time spent in sedentary/light activity varied significantly across the day. For the most part, the evening hours had an above average chance of containing MVPA, but were also more sedentary than average, while all or some of the morning hours had a less than average chance of containing MVPA, but were also less sedentary. These findings offer interesting and competing possibilities for interventions targeting sedentary time reductions or physical activity increases in colon survivors. All days and times are valid as a target for increasing activity and decreasing sedentary time; however, success might be best achieved targeting the periods with the most opportunity to change (e.g., most sedentary or least active) or alternatively targeting the periods already most active/least sedentary, if these indicate a natural inclination toward activity at certain times or on certain days.
This study has some limitations that must be acknowledged. The modest response rate (21 %) raises questions about the representativeness of the sample. However, aggregate data provided for Australian nonparticipants showed that they were not significantly different from participants by sex, age category, or time from diagnosis. Also, while overcoming self-report biases, accelerometers involve some error in estimating physical activity, such as poor detection of nonambulatory physical activities (e.g., swimming, cycling) and difficulties distinguishing standing from sedentary behavior. If such activities are particularly common on certain days, at certain times, or in certain groups, the patterns observed may be affected in addition to any impact such error may have on the overall mean levels of activity described. Future research into sedentary behavior would benefit from utilization of a separate device to measure sitting time accurately, such as the activPAL (Glasgow, UK) [29].
In conclusion, this study is the first to comprehensively document the objectively assessed physical activity and sedentary time of colon cancer survivors. In light of improved survival and other health benefits associated with MVPA [2–5], and adverse outcomes associated with sedentary behavior [11, 14], the findings of this study highlight the need for intervention in this population.
References
Baade PD, Fritschi L, Eakin EG (2006) Non-cancer mortality among people diagnosed with cancer (Australia). Cancer Causes Control 17(3):287–297
Meyerhardt JA, Giovannucci EL, Holmes MD, Chan AT, Chan JA, Colditz GA et al (2006) Physical activity and survival after colorectal cancer diagnosis. J Clin Oncol 24(22):3527–3534
Meyerhardt JA, Giovannucci EL, Ogino S, Kirkner GJ, Chan AT, Willett W et al (2009) Physical activity and male colorectal cancer survival. Arch Intern Med 169(22):2102–2108
Meyerhardt JA, Heseltine D, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ et al (2006) Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol 24(22):3535–3541
Kuiper JG, Phipps AI, Neuhouser ML, Chlebowski RT, Thomson CA, Irwin ML et al (2012) Recreational physical activity, body mass index, and survival in women with colorectal cancer. Cancer Causes Control 23(12):1939–1948
Courneya KS, Friedenreich CM, Quinney HA, Fields ALA, Jones LW, Vallance JKH et al (2005) A longitudinal study of exercise barriers in colorectal cancer survivors participating in a randomized controlled trial. Ann Behav Med 29(2):147–153
Lynch BM, Cerin E, Owen N, Hawkes AL, Aitken JF (2008) Prospective relationships of physical activity with quality of life among colorectal cancer survivors. J Clin Oncol 26(27):4480–4487
Vallance JK, Boyle T, Courneya KS, Lynch BM (2014) Associations of objectively assessed physical activity and sedentary time with health-related quality of life among colon cancer survivors. Cancer 120(18):2919–2926
Owen N (2012) Sedentary behavior: understanding and influencing adults’ prolonged sitting time. Prev Med 55(6):535–539
Network Sedentary Behaviour Research (2012) Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 37:540–542
Campbell PT, Patel AV, Newton C, Jacobs E, Gapstur SM (2013) Associations of recreational physical activity and leisure time spent sitting with colorectal cancer survival. J Clin Oncol 31(7):876–885
Hawkes AL, Lynch BM, Owen N, Aitken JF (2011) Lifestyle factors associated concurrently and prospectively with co-morbid cardiovascular disease in a population-based cohort of colorectal cancer survivors. Eur J Cancer 47:267–276
Wijndaele K, Lynch BM, Owen N, Dunstan DW, Sharp S, Aitken JF (2009) Television viewing time and weight gain in colorectal cancer survivors: a prospective population-based study. Cancer Causes Control 20(8):1355–1362
Lynch BM, Cerin E, Owen N, Hawkes AL, Aitken JF (2011) Television viewing time of colorectal cancer survivors is associated prospectively with quality of life. Cancer Causes Control 22(8):1111–1120
Lynch BM, Neilson HK, Friedenreich CM (2011) Physical activity and breast cancer prevention. In: Courneya KS, Friedenreich CM (eds) Physical Activity and Cancer Springer, Berlin 186:13–42. doi:10.1007/978-3-642-04231-7_2
Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N (2010) Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006). Cancer Causes Control 21:283–288
Lynch BM, Dunstan DW, Winkler E, Healy GN, Eakin E, Owen N (2011) Objectively assessed physical activity, sedentary time and waist circumference among prostate cancer survivors: findings from the national health and nutrition examination survey (2003–2006). Eur J Cancer Care 20:514–519
Sabiston CM, Brunet J, Vallance JK, Meterissian S (2014) Prospective examination of objectively assessed physical activity and sedentary time after breast cancer treatment: sitting on the crest of the teachable moment. Cancer Epidemiol Biomark Prev 23(7):1324–1330
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR et al (2008) Amount of time spent in sedentary behaviors in the united states, 2003–2004. Am J Epidemiol 167(7):875–881
Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ et al (2007) Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care 30(6):1384–1389
Freedson PS, Melanson E, Sirard J (1998) Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc 30(5):777–781
Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT et al (2012) Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 35:976–983
Atlas SJ, Deyo RA (2001) Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med 16(2):120–131
Lynch BM, Cerin E, Newman B, Owen N (2007) Physical activity, activity change, and their correlates in a population-based sample of colorectal cancer survivors. Ann Behav Med 34(2):135–143
Peddle CJ, Au HJ, Courneya KS (2008) Associations between exercise, quality of life, and fatigue in colorectal cancer survivors. Dis Colon Rectum 51(8):1242–1248
Boyle T, Lynch BM, Courneya KS, Vallance JK (2015) Agreement between accelerometer-assessed and self-reported physical activity and sedentary time in colon cancer survivors. Support Care Cancer 23(4):1121–1126
Clarke J, Janssen I (2014) Sporadic and bouted physical activity and the metabolic syndrome in adults. Med Sci Sports Exerc 46(1):76–83
Lynch BM, Courneya KS, Sethi P, Patrao TA, Hawkes AL (2014) A randomized controlled trial of a multiple health behavior change intervention delivered to colorectal cancer survivors: effects on sedentary behavior. Cancer 120(17):2665–2672
Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS (2011) Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc 43(8):1561–1567
Acknowledgments
Lynch is supported by a National Breast Cancer Foundation Early Career Fellowship (ECF-15-012). Boyle is supported by a National Health and Medical Research Council (NHMRC) Early Career Fellowship (1072266). Winkler is supported by a NHMRC Centre for Research Excellence grant (1057608). Courneya and Vallance are supported by the Canada Research Chairs program. Vallance is also supported by a Population Health Investigator Award from Alberta Innovates—Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical standard
The study was approved by Ethics Boards at Alberta Health Services (Alberta Cancer Research Ethics Committee), Athabasca University, Department of Health Western Australia and The University of Western Australia. All participants provided written, informed consent.
Rights and permissions
About this article
Cite this article
Lynch, B.M., Boyle, T., Winkler, E. et al. Patterns and correlates of accelerometer-assessed physical activity and sedentary time among colon cancer survivors. Cancer Causes Control 27, 59–68 (2016). https://doi.org/10.1007/s10552-015-0683-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0683-4