Abstract
Objective
To investigate whether people diagnosed with cancer have an increased risk of death from non-cancer causes compared to the general population.
Methods
The non-cancer mortality of people diagnosed with cancer in Queensland (Australia) between 1982 and 2002 who had not died before 1 January 1993 was compared to the mortality of the total Queensland population, matching by age group and sex, and reporting by standardised mortality ratios.
Results
Compared to the non-cancer mortality in the general population, cancer patients (all cancers combined) were nearly 50% more likely to die of non-cancer causes (SMR = 149.9, 95% CI = [147–153]). This varied by cancer site. Overall melanoma patients had significantly lower non-cancer mortality, female breast cancer patients had similar non-cancer mortality to the general population, while increased non-cancer mortality risks were observed for people diagnosed with cervical cancer, colorectal cancer, prostate cancer, non-Hodgkin lymphoma and lung cancer.
Conclusions
Although cancer-specific death rates underestimate the mortality directly associated with a diagnosis of cancer, quantifying the degree of underestimation is difficult due to various competing explanations. There remains an important role for future research in understanding the causes of morbidity among cancer survivors, particularly those looking at both co-morbid illnesses and reductions in quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A combination of increasing incidence of cancer and improved survival have resulted in an increase in the number of people living with a diagnosis of cancer [1–4]. This pattern can be at least partly explained by the aging of the population and improvements in management and early detection of cancer.
While it is well established that a cancer diagnosis will increase the risk of premature death from cancer-related causes, cancer patients may also have increased susceptibility to other types of non-cancer mortality. The various forms of cancer treatment, such as surgery, radiation therapy or hormone therapy can, in and of themselves, increase mortality risk [5–9]. In addition, known risk factors for cancer such as smoking, obesity and physical inactivity are also common to other non-cancer diseases such as heart disease [10–14], and may therefore increase the risk of death from causes other than cancer.
There have been a number of studies looking at the long term health of childhood and adolescent cancer patients [15–20] which suggest that they have increased risks of developing other chronic health problems in later life, usually as a result of their cancer treatment. However published data looking at non-cancer mortality among adults diagnosed with cancer is very limited.
One study [21], using data from the United States between 1973 and 1987, found that for all cancers combined, cancer patients had a 37% higher rate of non-cancer mortality than the general population. The most common causes of non-cancer death were circulatory and respiratory diseases. However, given the changes over the past three decades in both cancer management strategies [22–26] and the population prevalence of various risk factors [27–31], it is important to investigate whether this increased risk of non-cancer mortality among cancer patients remains.
In this study, we compared non-cancer mortality rates of a cohort of cancer patients diagnosed in Queensland (Australia) to those of the general population, looking at the most common non-cancer outcomes in all cancers combined, as well as in seven specific cancers.
Material and methods
Data sources
Cohort
The cohort of patients considered in this study were those people diagnosed with cancer in Queensland, Australia, between 1982 and 2002 who had not died before 1 January 1993. Data on cases were obtained from the Queensland Cancer Registry (QCR) in non-identifiable format. Notifications to this population-based registry, which commenced in 1982, are required by law. Non-melanoma skin cancers are not included in the notifications. In the year 2002 there were 17,938 incident invasive cancers registered in Queensland, which had a population of approximately 3.7 million people.
Incident cases are routinely matched to the national death registration dataset, and for this study, cases not known to have died before 31 December 2002 were considered to be still alive. The QCR routinely records detailed information about cancer causes of death and all other deaths are coded as “Non Cancer Death”. The QCR database is matched to the more detailed Registrar-general births deaths and marriages (RGBD) dataset to obtain more data on the non-cancer deaths.
We obtained ethics approval to conduct this study from the Behavioural & Social Sciences Ethical Review Committee at the University of Queensland. Government gazettal approval was obtained to access the data from the QCR, while separate written approval was obtained from the Registrar-general to access the additional data on non-cancer deaths.
Coded death information was available using ICD-9 and ICD-10 classifications. Due to the complexity of matching the different classifications, we used previously published mortality concordances [32, 33] to categorise the non-cancer mortality groups. The specific ICD-9 and ICD-10 codes for the major causes of death are detailed in Table 3. Groupings were not necessarily mutually exclusive. Codes were not available for approximately 3.3% of the non-cancer causes of death for the final cancer cohort. Although text-based descriptions of these non-coded deaths were available, we did not manually code these deaths for the purposes of this study. When cause of death information for cancer-related deaths was available from both the QCR and RGBD datasets, we gave priority to the QCR coding due to the additional information they have available when coding.
Variables extracted for the cohort dataset included year of diagnosis, year of death, age (5 year age groups to 85 plus), sex, cancer site, time since diagnosis and cause of death. Time since diagnosis was taken to be the difference between date of diagnosis and date of death for people who have died, and between date of diagnosis and the censor date (31 December 2002) for people still alive at the censor date.
Cohort exclusions/inclusions
Only people who were diagnosed between the ages of 20 and 79 were included in the analysis. We also censored all subjects at the age of 80 years to allow a focus on premature mortality, and remove the perceived difficulties of coding cause of death information among the eldest of the elderly [21, 34]. We also excluded those people for whom the date of death was not greater than the date of diagnosis, since these were primarily death certificate only cases (i.e. no histological confirmation) or cases discovered at autopsy and so they did not contribute person-time to either the numerator or the denominator.
Initially we considered the cohort of people diagnosed with any invasive cancer (All cancers combined). In addition, we looked at cancer-specific cohorts. These specific cancers were those cancers currently considered Australian “National Health Priority Area” (NHPA) cancers [35]; these cancers are prostate cancer, melanoma, cervical, female breast cancer, non-Hodgkin lymphoma (NHL), lung cancer and colorectal cancer. The NHPA cancers were chosen to reflect those that cause the greatest burden to the community and have potential for health gains and improved outcomes.
The QCR only records the first (primary) cancer on each cancer site (according to the 3-digit ICD rubric and histology code) [36]. However there were 1,721 people diagnosed since 1982 who had more than one primary invasive cancer. That is, these people had a primary cancer on more than one site. Since the main outcome in this study is mortality, including all these multiple cancers would reduce the independence of the data. Therefore for those people with multiple primary invasive cancers, we included only the first cancer diagnosis recorded on QCR.
Comparison data
Mortality of the cohort of cancer patients was compared to the mortality of the total Queensland population. Unit record mortality data for the total Queensland population for each year between 1993 and 2002 (inclusive) was obtained from the Australian Bureau of Statistics (ABS). Cause of death information was coded by the ABS according to the ICD-9 and ICD-10 classifications. This mortality data were then categorised into the same mortality groupings as for the cancer cohort described above.
Estimated resident population data for Queensland between 1993 and 2002 (inclusive) was obtained from the Australian Bureau of Statistics.
Analysis
Standardised mortality ratios
The analysis focuses on indirectly age-standardised mortality ratios (SMR). This is, in effect, the ratio of the cause-specific mortality rate among the cohort of cancer patients to the corresponding cause-specific mortality rate among the Queensland population. This ratio was calculated after matching both rates by age group and sex.
We calculated the cause-specific mortality rate for cancer patients by dividing the total number of deaths (cause-specific) between 1993 and 2002 by the total number of prevalent cancer patients in the same period, according to the specific cancer diagnosis, year, sex, age group and time since diagnosis. Cases were considered prevalent if they had been diagnosed since 1982 (i.e. recorded on the QCR database) and were alive on 31 December of the relevant year (1993–2002). The “prevalent age” was calculated based on the age at diagnosis and the time from the year of diagnosis to the prevalent year. People diagnosed prior to the commencement of the registry (pre-1982) were not included. Time since diagnosis was measured in single year periods, as well as all years combined.
A similar process was used for the comparison mortality rate in the Queensland population, except that rather than using prevalent cases as the denominator, we used the estimated resident population for each year. All analysis was carried out using SAS® [37].
Results
Description of the cohort
There were a total of 144,679 cancer patients in Queensland that met the eligibility criteria outlined above. Of these, 52.9% were male, and 73.0% were over 50 years of age when diagnosed. About one-third of these cancer patients (51,346 or 35.6%) had died of some cause between 1993 and 2002. Of those that had died, about one in six (8123 or 15.8%) had died of a non cancer-related cause. The majority (96.0%) of patients who died of a cancer-related cause died of the cancer they were first diagnosed with.
For the comparison cohort, there were a total of 125,124 deaths of people in Queensland aged 20–79 between 1993 and 2002, and of these 80,016 (or 63.9%) were of non-cancer related causes.
The percent of deaths caused by non-cancer causes varied with age (Table 1). For cancer patients diagnosed in their 20 s, 30 s and 40 s, the proportion of deaths coded to non-cancer causes was around 10%. However for people diagnosed in their 60 s and 70 s, among whom the majority of deaths occurred, the proportion was closer to 20%. The median survival time (or time to death) was significantly higher among those who died of non-cancer causes (median = 3.1 years for 20–79 years combined) compared to those who died of cancer- related causes (median = 0.9 years) (Wilcoxon two-sample test, p<0.0001).
SMRs
The proportion of patients who died of either cancer or non-cancer deaths varied depending on the specific cancer diagnosis (Table 2). The proportion of patients who died from non-cancer deaths ranged from 3.0% among female breast cancer patients to 10.3% among men with prostate cancer. Across all cancers, 5.6% of cancer patients had died from a non-cancer cause of death. Compared to the non-cancer mortality in the general population, cancer patients (all cancers combined) were nearly 50% more likely to die of non-cancer causes (SMR = 149.9). The non-cancer mortality for people diagnosed with melanoma (SMR = 93.5) was statistically significantly less than the general population, while the lower non-cancer mortality risk for female breast cancer patients (SMR = 94.2) was not statistically different to the general population. People diagnosed with any of the remaining NHPA cancers were all significantly more likely to die of a non-cancer cause of death than the age and sex-matched Queensland population. The greatest increased risk was for people diagnosed with lung cancer, with the non-cancer mortality rate being over 4 times that of the general population (SMR = 429.4).
Cause-specific data
Cardiovascular disease was the greatest cause of non-cancer mortality among the cancer cohort (Table 3), being responsible for over half of the non-cancer mortality. Included in this group were coronary heart disease and stroke. Other major non-cancer causes of death included respiratory diseases, diseases of the digestive system, injury and poisoning and endocrine, nutritional and metabolic diseases. Among the cancer cohort who died of non-cancer causes, a greater proportion of males died of coronary heart disease than females (36.9% versus 30.9% respectively, χ2 = 27.9, df = 1, p<0.001) and COPD (10.5% versus 7.4%, χ2 = 19.0, df = 1, p<0.001), while more females were more likely to have died of stroke (12.6% versus 10.0%, χ2 = 12.2, df = 1, p<0.001. Among the cancer cohort who died of non-cancer causes, the proportion of deaths due to cardiovascular disease increased with age, while the proportion due to injury and poisoning decreased with age.
Cause-specific age-standardised mortality ratios
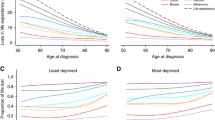
The age-standardised mortality ratios for non-cancer causes of death were calculated, comparing the cancer cohort to the total Queensland population, matched by age group and sex (Figure 1). To increase the stability of the estimates we have only presented those SMRs for cancers that had at least 100 observed deaths for all cancers combined.
All cancers combined
Compared to the general population, the cancer cohort had a significantly increased risk of mortality from diseases of the digestive system (SMR = 187.1), respiratory diseases (SMR = 155.5), diseases of the genitourinary system (SMR = 155.4), injury and poisoning (SMR = 147.8), cardiovascular disease (SMR = 138.6) and endocrine, nutrition and metabolic diseases (SMR = 136.3).
Colorectal cancer
The overall risk of non-cancer mortality among colorectal cancer patients was nearly 40% higher than the general population (SMR = 136.7). Compared to the general population, colorectal cancer patients had over twice the risk of dying from diseases of the digestive system (SMR = 231.7), and increased risks of dying from injury and poisoning (SMR = 186.9), cardiovascular disease (SMR = 125.9) and respiratory diseases (SMR = 120.3).
Lung cancer
Lung cancer patients had the highest comparable risk of dying from non-cancer causes of death (SMR = 429.4) than the other cancers considered in this study. In particular, increased risks were observed for diseases of the digestive system (SMR = 721.6), respiratory diseases (SMR = 6141), injury and poisoning (SMR = 424.3), cardiovascular disease (SMR = 390.9), diseases of the genitourinary system (SMR = 346.6) and endocrine, nutrition and metabolic diseases (SMR = 233.4).
Melanoma
Overall, the rates of non-cancer mortality among people diagnosed with melanoma was significantly less than the general population (SMR = 93.5). There were very few non-cancer causes of death for which the risk of melanoma patients dying from was significantly greater than the general population, and those that did have significantly increased risks, Parkinson’s disease (SMR = 199.2) and Falls (SMR = 206.1), were based on very small numbers of deaths (12 and 11 deaths respectively). Significantly reduced risks were observed for cardiovascular disease (SMR = 90.4) and respiratory disease (SMR = 77.8).
Female breast cancer
The rates of non-cancer mortality among women diagnosed with breast cancer was not significantly different to that of the general (female) population (SMR = 94.2). There were no non-cancer causes of death (with more than 10 deaths) for which the risk of female breast cancer patients dying from was greater than the general female population. Reduced risks were observed for cardiovascular disease (SMR = 83.9).
Cervical cancer
The overall rate of non-cancer mortality among women diagnosed with cervical cancer was about 50% higher (SMR = 153.0) than that of the general (female) population. Since the numbers of cervical cancer diagnoses (and deaths) were much fewer than for the other cancers examined, the ability to detect statistically significant differences for specific causes of non-cancer death was limited. However there was an significantly increased risk of diseases of the digestive system (SMR = 332.5), endocrine, nutrition and metabolic diseases (SMR= 328.8) and cardiovascular disease (SMR = 146.1) among cervical cancer patients compared to the total female population.
Prostate cancer
Overall, the rates of non-cancer mortality among men diagnosed with prostate cancer were about 30% higher (SMR = 132.6) than the age-matched male general population. Increased rates were observed for injury and poisoning (SMR = 196.8), respiratory diseases (SMR = 136.0), diseases of the digestive system (SMR = 135.1) and cardiovascular diseases (SMR = 126.7).
Non-Hodgkin lymphoma
The overall rate of non-cancer mortality among people diagnosed with NHL was nearly 90% higher (SMR = 187.8) than that of the general population. Increased risks of death due to injury and poisoning (SMR = 224.3), respiratory disease (SMR = 159.7) and cardiovascular disease (SMR = 159.4) were observed among NHL patients.
SMRs by time since diagnosis
As shown in Figure 2, the majority of the increased risk for non-cancer causes of death is generally in the first year after diagnosis and then quickly decreases to be equivalent to that of the general population. Exceptions to this pattern were for lung cancer and cervical patients, where the non-cancer mortality risk remained higher than the general population as time after diagnosis increased. The other exception was for prostate cancer patients, whose non-cancer mortality risk decreased quickly after the first year but then started to increase over time.
Of the 2,261 non-cancer deaths in the first year after diagnosis, 54.2% were due to cardiovascular disease and 13.5% were due to respiratory disease. Although only 4.9% (110) of these deaths were due to injury and poisoning, this included 50 deaths by suicide, and 18 deaths by firearm injuries. There were 21 cases of death from HIV-AIDS, primarily among younger patients, and in these cases this underlying cause of death may also have caused the cancer (13 were due to NHL). There were only a few causes of non-cancer death which potentially could have been a direct complication of the cancer or treatment of the cancer. These include 29 (1.2%) deaths due to septicaemia and 35 (1.5%) deaths due to diseases of blood and blood forming organs.
Discussion
Summary of results
Overall, cancer patients were at about a 50% higher risk of mortality from non-cancer causes of death than the general population, with the increased risk particularly evident within 2 years after diagnosis. However this varied depending on the specific cancer diagnosis, with lung cancer patients having more than a 4-fold increased risk of dying from non-cancer causes than the general population, while melanoma patients were significantly less likely to die of non-cancer causes of death.
The major cause of non-cancer deaths among cancer patients were cardiovascular disease, in particular coronary heart disease and stroke. This is not surprising, since cardiovascular disease is the second most common cause of death (behind cancer) among the Australian population [38]. However, apart from people diagnosed with melanoma or female breast cancer, the risk of mortality due to cardiovascular disease among cancer patients was still higher than the risk in the general population.
There is little information in the literature on the non-cancer causes of death in cancer patients. Studies of the prevalence of co-morbidities in cancer patients have shown that the most frequent diseases in cancer patients are cardiovascular conditions, hypertension, chronic obstructive pulmonary disease and diabetes [39, 40]. This is consistent with findings from this study pertaining to the entire cancer cohort, which also showed increased death rates from cardiovascular disease, and endocrine and metabolic disease. However, it is difficult to explain the increased risk of death from digestive system diseases, particularly among lung cancer patients. A closer examination of the small number of digestive system deaths revealed that these deaths were from a number of causes including cirrhosis of the liver, peptic ulcer and diverticular disease.
As with the overall findings, NHL patients had increased risks of death from respiratory and cardiovascular diseases, similar to the prevalent conditions in NHL patients in other studies [41]. Prostate cancer patients in our study had increased risk of death from conditions of the nervous, respiratory and digestive system, as well as cardiovascular diseases. While the increased prevalence of cardiovascular disease among prostate cancer patients has been reported previously [42], the increased risk for the other conditions has not.
A recent study [43] reported evidence of increased risk of mortality due to Amyotrophic Lateral Sclerosis (ALS) and Parkinson’s disease among melanoma patients. We found a similar increased mortality risk in this study (although not significant for ALS), however the very small numbers of deaths (9 and 12 respectively) for these conditions, and the resulting wide confidence intervals for the risk estimates, made any definitive interpretation difficult.
Possible explanations for risk differentials
There are a number of possible reasons for the observed risk differentials in this study. The first is that the treatments used for the management of cancer had a side effect of causing another fatal condition. If this side effect was directly related to the cancer (for example death during surgery for the cancer), then this would usually be coded as being due to the specific cancer. However some treatments can have longer term side effects; examples include immune suppression due to chemotherapy which may result in a later death due to infection, or scarring from radiotherapy resulting in obstruction of the bowel. The excess of non-cancer deaths in the cancer cohort immediately after diagnosis may be interpreted as being due to the short-term effect of treatment. This is the explanation previously proposed by Brown and colleagues [21]. However, closer examination of the non-cancer causes of death in the 12 months after diagnosis of cancer suggests that only a small proportion of these deaths were closely related to the cancer, and so it is unlikely that short-term side-effects of treatment can explain much of the observed results. Rather, considering the results of studies looking at the long-term health of childhood cancer survivors suggests that any treatment side effects are more likely observed in the long-term.
A second plausible explanation is that, rather than the non-cancer death being directly related to the cancer (or its treatment), the diagnosis of cancer could have been made almost incidentally while treating the other (fatal) condition. This may also explain why the non-cancer mortality rate was highest soon after diagnosis, because more detailed medical tests and/or invasive procedures are more likely as the non-cancer condition gets more serious. Additional evidence supporting this hypothesis could be obtained using stage information – if most of the cancers diagnosed in the year before death were early stage cancers, then it is more likely they were incidentally diagnosed, rather than contributing to the person’s death. Unfortunately stage information is not routinely collected by cancer registries in Australia.
The third possible reason is that the demographics of the cancer cohort are not representative of the general population. An example of this could be the reduced risk of non-cancer mortality among melanoma patients. Previous studies have shown that incidence of melanoma is typically higher among more affluent people [44] who also have better general health [45]. Since the majority of melanomas in Queensland are diagnosed when thin [46] and can be treated with curative intent, it is unlikely they would impact on the person’s general health. Therefore the reduced risk of non-cancer death among melanoma patients could be attributed to the increased proportion of affluent people in this sub-cohort compared to the general population. A similar effect could potentially explain the lack of difference in non-cancer mortality among female breast cancer patients, who are also more likely to be of higher socio-economic status [47].
The fourth possible reason is that the risk factors that contributed to the development of a specific cancer can be the same as those for other potentially fatal conditions. Cigarette smoking is responsible for the development of the majority of all lung cancers [48]. However it is also responsible for an increased risk of ischaemic heart disease, chronic obstructive pulmonary disease and stroke [49]. We would expect, therefore, that a population who have had lung cancer would contain more smokers than the general population and therefore would be at higher risk of other smoking-related diseases. This is reinforced by the results of this study, in which the major causes of non-cancer deaths among lung cancer patients were also smoking related.
A fifth possible reason is the potential for interaction between these two above reasons. That is, some subgroups of the population are more likely to have higher prevalence of specific risk factors. For example smoking and obesity have been more prevalent in lower socio-economic groups [29, 50]. Therefore the impact of the increase in these risk factors and the lower general health, could both impact on the observed risk of non-cancer mortality.
Study quality
This was a population-based study with large numbers of cancers and deaths, thus giving us confidence in the results. It was based on routinely collected and coded data so, although there would be some errors, these are likely to be random. The cancer cohort was compared with the general population that also would contain some people with cancer; however the proportion of the comparison cohort (total Queensland population) that is also in the cancer cohort (those diagnosed with cancer) in a single year is less than 1%.
Further research/implications
We have found that cancer patients are at greater risk, compared to the general population, of dying of causes which are, at least superficially, unrelated to their cancer. Our results, and those of previous studies [21] suggest that cancer-specific death rates underestimate the mortality directly associated with a diagnosis of cancer. However quantifying the amount of underestimation is problematic due to the inability to separate the abovementioned possible reasons for the observed results. There remains an important role for future research in understanding the causes of morbidity among cancer survivors, particularly studies that characterise the extent of disease burden in terms of both comorbid illnesses as well as reductions in quality of life. The role of potentially modifiable risk factors such as smoking, obesity and physical inactivity also warrants attention; as such factors will likely play a role in improving the quality of life of the growing number of cancer survivors.
References
D Forman D Stockton H Moller et al. (2003) ArticleTitleCancer prevalence in the UK: results from the EUROPREVAL study Ann Oncol 14 648–654 Occurrence Handle10.1093/annonc/mdg169 Occurrence Handle1:STN:280:DC%2BD3s7jsVSitQ%3D%3D Occurrence Handle12649115
JM Lutz S Francisci E Mugno et al. (2003) ArticleTitleCancer prevalence in Central Europe: the EUROPREVAL Study Ann Oncol 14 313–322 Occurrence Handle10.1093/annonc/mdg059 Occurrence Handle1:STN:280:DC%2BD3s%2Flt12qsA%3D%3D Occurrence Handle12562661
KJ Brameld CDA Holman TJ Threlfall DM Lawrence NH Klerk ParticleDe (2002) ArticleTitleIncreasing ‘active prevalence’ of cancer in Western Australia and its implications for health services Aust New Zeal J Public Health 26 164–169
InstitutionalAuthorNameMMWR (2004) ArticleTitleCancer Survivorship – United States, 1971–2001 MMWR 53 526–529
PL Harkonen SI Makela (2004) ArticleTitleRole of estrogens in development of prostate cancer J Steroid Biochem Mol Biol 92 297–305 Occurrence Handle10.1016/j.jsbmb.2004.10.016 Occurrence Handle15663993
JR Mackey AA Joy (2005) ArticleTitleSkeletal health in postmenopausal survivors of early breast cancer Int J Cancer 114 1010–1015 Occurrence Handle10.1002/ijc.20826 Occurrence Handle1:CAS:528:DC%2BD2MXjsFWjs7g%3D Occurrence Handle15645435
N Arber B Levin (2005) ArticleTitleChemoprevention of colorectal cancer: ready for routine use? Recent Results Cancer Res 166 213–230 Occurrence Handle1:CAS:528:DC%2BD2MXos1WisQ%3D%3D Occurrence Handle15648192
PB Bach LD Cramer D Schrag RJ Downey SE Gelfand CB Begg (2001) ArticleTitleThe influence of hospital volume on survival after resection for lung cancer N Engl J Med 345 181–188 Occurrence Handle10.1056/NEJM200107193450306 Occurrence Handle1:STN:280:DC%2BD3Mvht12jsw%3D%3D Occurrence Handle11463014
WE Longo KS Virgo FE Johnson et al. (2000) ArticleTitleRisk factors for morbidity and mortality after colectomy for colon cancer Dis Colon Rectum 43 83–91 Occurrence Handle10.1007/BF02237249 Occurrence Handle1:STN:280:DC%2BD3c3ntFagtQ%3D%3D Occurrence Handle10813129
M Ezzati AD Lopez (2004) ArticleTitleRegional, disease specific patterns of smoking-attributable mortality in 2000 Tob Control 13 388–395 Occurrence Handle1:STN:280:DC%2BD2crpt1eisw%3D%3D Occurrence Handle15564623
M Ezzati AD Lopez (2003) ArticleTitleEstimates of global mortality attributable to smoking in 2000 Lancet 362 847–852 Occurrence Handle13678970
MN Rashid F Fuentes RC Touchon PS Wehner (2003) ArticleTitleObesity and the risk for cardiovascular disease Prev Cardiol 6 42–47 Occurrence Handle12624562
Y Oguma T Shinoda Tagawa (2004) ArticleTitlePhysical activity decreases cardiovascular disease risk in women: review and meta-analysis Am J Prev Med 26 407–418 Occurrence Handle10.1016/j.amepre.2004.02.007 Occurrence Handle15165657
RS Paffenbarger SuffixJr SN Blair IM Lee (2001) ArticleTitleA history of physical activity, cardiovascular health and longevity: the scientific contributions of Jeremy N Morris, DSc, DPH, FRCP Int J Epidemiol 30 1184–1192 Occurrence Handle10.1093/ije/30.5.1184 Occurrence Handle11689543
MM Hudson AC Mertens Y Yasui et al. (2003) ArticleTitleHealth status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study JAMA 290 1583–1592 Occurrence Handle10.1001/jama.290.12.1583 Occurrence Handle1:CAS:528:DC%2BD3sXnvVals7c%3D Occurrence Handle14506117
KC Oeffinger MM Hudson (2004) ArticleTitleLong-term complications following childhood and adolescent cancer: foundations for providing risk-based health care for survivors CA Cancer J Clin 54 208–236 Occurrence Handle15253918
LL Robison AC Mertens JD Boice et al. (2002) ArticleTitleStudy design and cohort characteristics of the Childhood Cancer Survivor Study: a multi-institutional collaborative project Med Pediatr Oncol 38 229–239 Occurrence Handle10.1002/mpo.1316 Occurrence Handle11920786
MC Cardous Ubbink RC Heinen NE Langeveld et al. (2004) ArticleTitleLong-term cause-specific mortality among five-year survivors of childhood cancer Pediatr Blood Cancer 42 563–573 Occurrence Handle1:STN:280:DC%2BD2c3ivVarsg%3D%3D Occurrence Handle15127410
DM Green A Hyland CS Chung MA Zevon BC Hall (1999) ArticleTitleCancer and cardiac mortality among 15-year survivors of cancer diagnosed during childhood or adolescence J Clin Oncol 17 3207–3215 Occurrence Handle1:STN:280:DyaK1MvjvVWqsg%3D%3D Occurrence Handle10506620
AC Mertens Y Yasui JP Neglia et al. (2001) ArticleTitleLate mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study J Clin Oncol 19 3163–3172 Occurrence Handle1:STN:280:DC%2BD3Mzns1Oltg%3D%3D Occurrence Handle11432882
BW Brown C Brauner MC Minnotte (1993) ArticleTitleNoncancer deaths in white adult cancer patients J Nat Cancer Inst 85 979–987 Occurrence Handle1:STN:280:ByyB28jmslI%3D Occurrence Handle8496983
AM Meraney A Haese J Palisaar et al. (2005) ArticleTitleSurgical management of prostate cancer: advances based on a rational approach to the data Eur J Cancer 41 888–907 Occurrence Handle10.1016/j.ejca.2005.02.005 Occurrence Handle15808956
SA Mangar RA Huddart CC Parker DP Dearnaley VS Khoo A Horwich (2005) ArticleTitleTechnological advances in radiotherapy for the treatment of localised prostate cancer Eur J Cancer 41 908–921 Occurrence Handle10.1016/j.ejca.2004.12.028 Occurrence Handle15808957
PD Bonomi (2004) ArticleTitleTherapeutic advances in second-line treatment of advanced non-small-cell lung cancer Clin Lung Cancer 6 154–161 Occurrence Handle15555216
BA Mincey EA Perez (2004) ArticleTitleAdvances in screening, diagnosis, and treatment of breast cancer Mayo Clin Proc 79 810–816 Occurrence Handle15182098
C Faivre Finn AM Bouvier Benhamiche JM Phelip S Manfredi V Dancourt J Faivre (2002) ArticleTitleColon cancer in France: evidence for improvement in management and survival Gut 51 60–64 Occurrence Handle1:STN:280:DC%2BD38zjsVSjsw%3D%3D Occurrence Handle12077093
V White D Hill M Siahpush I Bobevski (2003) ArticleTitleHow has the prevalence of cigarette smoking changed among Australian adults? Trends in smoking prevalence between 1980 and 2001 Tob Control 12 IssueIDSuppl 2 ii67–74 Occurrence Handle12878776
A Molarius RW Parsons AJ Dobson et al. (2001) ArticleTitleTrends in cigarette smoking in 36 populations from the early 1980s to the mid-1990s: findings from the WHO MONICA Project Am J Public Health 91 206–212 Occurrence Handle1:STN:280:DC%2BD3M7ktFejsQ%3D%3D Occurrence Handle11211628
Q Zhang Y Wang (2004) ArticleTitleTrends in the association between obesity and socioeconomic status in U.S. adults: 1971 to 2000 Obes Res. 12 1622–1632 Occurrence Handle15536226
A Bauman T Armstrong J Davies et al. (2003) ArticleTitleTrends in physical activity participation and the impact of integrated campaigns among Australian adults, 1997–99 Aust N Z J Public Health 27 76–79 Occurrence Handle14705272
CL Craig SJ Russell C Cameron A Bauman (2004) ArticleTitleTwenty-year trends in physical activity among Canadian adults Can J Public Health 95 59–63 Occurrence Handle14768744
Public Health Division (2005) The Health of the people of New South Wales – Report of the Chief Health Officer. http://www.health.nsw.gov.au/public-health/chorep/toc/app_icd_diag. htm. Accessed 17th June 2005
ABS (2005) Causes of Death 2003 [Appendix Comparability of data over time]. Canberra, Australian Bureau of Statistics (Catalogue number 3303.0) (www.abs.gov.au)
AE Grulich A Swerdlow I dos Santos Silva V Beral (1995) ArticleTitleIs the apparent rise in cancer mortality in the elderly real? Analysis of changes in certification and coding of cause of death in England and Wales, 1970–1990 Int J Cancer 63 164–168 Occurrence Handle1:STN:280:BymD2cznt1U%3D Occurrence Handle7591198
CDHA (2005) National Health Priority Areas. Commonwealth Department of Health and Ageing (http://www.health.gov.au/pq/nhpa/) Accessed 15/07/2005
Queensland Cancer Registry (2004) Cancer in Queensland. Incidence and mortality 1982 to 2002. Brisbane, Queensland Health and Queensland Cancer Fund (http://www.health.qld.gov.au/publications/infocirc/StatsTable1982_2002.pdf )
SAS Institute Inc (2004) SAS OnlineDoc®, Version 9.1.2. Cary NC, SAS Institute Inc
ABS (2004) Causes of Death (various years). Canberra, Australian Bureau of Statistics (Catalogue number 3303.0) (www.abs.gov.au)
JW Coebergh ML Janssen-Heijnen PN Post PP Razenberg (1999) ArticleTitleSerious co-morbidity among unselected cancer patients newly diagnosed in the southeastern part of The Netherlands in 1993–1996 J Clin Epidemiol 52 1131–1136 Occurrence Handle10.1016/S0895-4356(99)00098-0 Occurrence Handle1:STN:280:DC%2BD3c%2Fks1OnsA%3D%3D Occurrence Handle10580775
ML Janssen-Heijnen RM Schipper PP Razenberg MA Crommelin JW Coebergh (1998) ArticleTitlePrevalence of co-morbidity in lung cancer patients and its relationship with treatment: a population-based study Lung Cancer 21 105–113 Occurrence Handle10.1016/S0169-5002(98)00039-7 Occurrence Handle1:STN:280:DyaK1M%2FksFSjuw%3D%3D Occurrence Handle9829544
DJ Spronsen Particlevan ML Janssen-Heijnen WP Breed JW Coebergh (1999) ArticleTitlePrevalence of co-morbidity and its relationship to treatment among unselected patients with Hodgkin’s disease and non-Hodgkin’s lymphoma, 1993–1996 Annals Hematol 78 315–319
WH Hall AB Jani JK Ryu S Narayan S Vijayakumar (2005) ArticleTitleThe impact of age and comorbidity on survival outcomes and treatment patterns in prostate cancer Prostate Cancer Prostatic Dis 8 22–30 Occurrence Handle10.1038/sj.pcan.4500772 Occurrence Handle1:STN:280:DC%2BD2M7ktlOrsg%3D%3D Occurrence Handle15700051
DM Freedman LB Travis G Gridley RW Kuncl (2005) ArticleTitleAmyotrophic lateral sclerosis mortality in 1.9 million US cancer survivors Neuroepidemiology 25 176–180 Occurrence Handle16103728
RA Harrison AU Haque JM Roseman SJ Soong (1998) ArticleTitleSocioeconomic characteristics and melanoma incidence Ann Epidemiol 8 327–333 Occurrence Handle10.1016/S1047-2797(97)00231-7 Occurrence Handle1:STN:280:DyaK1czjt1akug%3D%3D Occurrence Handle9669615
Glover J, Harris K, Tennant S (1999) A Social Health Atlas of Australia, 2nd Edn. South Australia: Public Health Information Development Unit, University of Adelaide (http://www.publichealth.gov.au Accessed 18/07/2005)
Coory M, Baade PD, Aitken JF, Smithers M, McLeod GRC, Ring I (in press) Trends for in-situ and invasive melanoma in Queensland, Australia, 1982 to 2002. Cancer Causes and Control 17:21–27
NH Gordon (2003) ArticleTitleSocioeconomic factors and breast cancer in black and white Americans Cancer Metastasis Rev 22 55–65 Occurrence Handle10.1023/A:1022212018158 Occurrence Handle1:CAS:528:DC%2BD3sXpt1WktQ%3D%3D Occurrence Handle12716037
P Boyle P Maisonneuve (1995) ArticleTitleLung cancer and tobacco smoking Lung Cancer 12 167–181 Occurrence Handle10.1016/0169-5002(95)00443-5 Occurrence Handle1:STN:280:ByqA1cvls10%3D Occurrence Handle7655828
Ridolfo B, Stevenson C (2001) The quantification of drug-caused mortality and morbidity in Australia, 1998. Canberra, Australian Institute of Health and Welfare. AIHW Cat. No. PHE 29
EM Barbeau N Krieger MJ Soobader (2004) ArticleTitleWorking class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000 Am J Public Health 94 269–278 Occurrence Handle14759942
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baade, P.D., Fritschi, L. & Eakin, E.G. Non-Cancer Mortality among People Diagnosed with Cancer (Australia). Cancer Causes Control 17, 287–297 (2006). https://doi.org/10.1007/s10552-005-0530-0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-0530-0