Abstract
Objective
To investigate the prospective relationships between television viewing time and weight gain in the 3 years following colorectal cancer diagnosis for 1,867 colorectal cancer survivors (body mass index (BMI) ≥ 18.5 kg/m2).
Methods
BMI, television viewing time, physical activity, and socio-demographic and clinical covariates were assessed at baseline (5 months), 24 months and 36 months post-diagnosis. Multiple linear regression was used to study independent associations between baseline television viewing time and BMI at 24 and 36 months post-diagnosis.
Results
At both follow-up time points, there was a significant increase in mean BMI for participants reporting ≥5 h/day of television viewing compared to those watching <3 h/day at baseline (24 months: 0.72 kg/m2 (0.31, 1.12), p < 0.001; 36 months: 0.61 kg/m2 (0.14, 1.07), p = 0.01), independent of baseline BMI, gender, age, education, marital status, smoking, cancer site, cancer disease stage, treatment mode and co-morbidities. Additional adjustment for baseline physical activity did not change results.
Conclusions
These findings suggest that a greater emphasis on decreasing television viewing time could help reduce weight gain among colorectal cancer survivors. This, in turn, could contribute to a risk reduction for co-morbid conditions such as type 2 diabetes and cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer survivors have an elevated risk of developing other chronic diseases, such as type 2 diabetes, cardiovascular disease and additional primary cancers [1]. The risk of developing such co-morbid conditions is exacerbated by overweight and obesity and by physical inactivity [2–5]. Colorectal cancer is one of the most commonly diagnosed cancers, particularly in developed countries [6, 7]. Overweight and obesity and physical inactivity are associated with poorer long-term survival amongst colorectal cancer survivors. Prospective studies have shown that an increase in body mass index (BMI) is associated with an elevated mortality risk from colorectal cancer [8]. Recent studies in people diagnosed with colorectal cancer have reported a positive association between physical activity and survival [9–11].
In general adult population studies, sedentary behaviors, particularly television viewing, have been associated with overweight and obesity, independent of physical activity levels. For example, a recent cross-sectional study of 6,241 Australian adults reported that television viewing of 14 or more hours per week was independently associated with obesity [12]. A prospective study of 18,583 postmenopausal women demonstrated that non-occupational time spent sitting (watching television, reading, etc.) was significantly associated with weight gain among women who were not overweight at baseline [13]. Sedentary behavior (television viewing) was also shown to have a positive prospective relationship with obesity in the nurses’ health study [14].
Sedentary behaviors are not simply the lack of physical activity. They have distinct biological consequences [15], have some distinct social and environmental correlates [16, 17], and are deleteriously associated with metabolic biomarkers, even among adults who meet public health recommendations on physical activity [18]. There is the need to understand possible relationships between sedentary behavior and BMI amongst cancer survivors. Should sedentary behaviors have an independent effect on BMI amongst cancer survivors, such behaviors might have an effect on cancer survival and on other health outcomes that are influenced by adiposity. We examined the prospective associations between television viewing time and BMI, controlling for physical activity, in the 3 years following colorectal cancer diagnosis.
Materials and methods
Participants and procedures
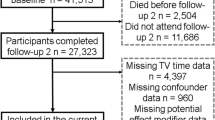
Data were collected by telephone interview as part of the colorectal cancer and quality of life study, the methods of which are described in detail elsewhere [19]. In brief, all persons resident of Queensland, Australia, with a histologically confirmed diagnosis of a first, primary colorectal cancer, who notified to the Queensland cancer registry between 1 January 2003 and 31 December 2004, were eligible for the study. Eligibility criteria also included speaking English; having no hearing, speech, or cognitive disabilities that would prevent completing a telephone interview; and being aged between 20 and 80 years at the time of diagnosis. A flow diagram describing recruitment to, and participation in, the study is presented in Fig. 1. The sample slightly under-represented colorectal cancer survivors who were older (ages 70–80), those with rectal cancer, and those with more advanced disease: a more comprehensive description of the study sample is available [19]. All patients who provided written, informed consent were telephoned by a trained interviewer, at ~5, 24 and 36 months post-diagnosis. For the present study, only participants who were categorized as healthy weight, overweight or obese at baseline (n = 1,867) were included, as those who are underweight might actually benefit from gaining weight and would typically not be candidates for interventions to prevent weight gain. The University of Queensland’s Behavioural and Social Science Ethical Review Committee approved procedures of the study. The study was conducted in accordance with the Helsinki Declaration.
Measures
Baseline predictor variables (assessed at 5 months post-diagnosis)
Television viewing time
Participants provided an estimate of their total time spent watching television, on an average day, over the past month. Seven possible response options were provided: never, <1 h, 1–2 h, 3–4 h, 5–6 h, 7–10 h, or 11 h or more. This was later re-categorized to the following options: <3 h, 3–4.9 h, or 5 or more hours. Self-reported television viewing time has been found to be reliable in Australian population surveys (ICC = 0.82) [17].
Physical activity
The active Australia survey, a standard instrument developed to monitor physical activity participation in the Australian adult population [20, 21], was used. Participants were asked to report the amount of time that they spent each week walking for transport or recreation, in other moderate-intensity physical activities (e.g., gentle swimming, social tennis, golf), and in vigorous-intensity physical activities (e.g., jogging, cycling, aerobics, competitive tennis). Total weekly physical activity was calculated by adding together the time spent in each of these categories. Consistent with the active Australia study, vigorous activity was double-weighted to account additional energy expenditure associated with this activity level [20]. Current Australian public-health guidelines recommend achieving the equivalent of 150 min of moderate-intensity activity per week [22]. Based on these guidelines, participants were categorised as either being inactive (0 min per week), insufficiently active (1–149 min per week), or sufficiently active (150 or more min per week).
Socio-demographic and clinical variables
Gender, age, cancer site and cancer disease stage were collected from pathology reports. Marital status, educational attainment, smoking behavior, mode of treatment received and current co-morbid conditions were assessed by interview.
Outcome variable (BMI assessed at 5, 24, and 36 months post-diagnosis)
Height and weight were self-reported at 5 months post-diagnosis; weight was also self-reported at subsequent interviews. BMI was calculated for each time point and used as a continuous outcome variable to maximize statistical power [23]. For descriptive purposes, participants were categorized as healthy weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), or obese (BMI ≥ 30.0 kg/m2) [24].
Statistical analysis
Multiple linear regression analyses were used to examine the independent effect of baseline television viewing time on BMI change from baseline to 24 months post-diagnosis and from baseline to 36 months post-diagnosis; unstandardized regression coefficients are provided. Only individuals with complete data for all variables in these multiple linear regression models were included. Therefore, these analyses were conducted with a subsample of the initial 1,867 participants who had a BMI ≥ 18.5 kg/m2 at baseline. The analyses examining BMI change from baseline to 24 months post-diagnosis included 1,202 participants, and those examining BMI change from baseline to 36 months post-diagnosis included 1,028. For both time points, the first model (Model A) was adjusted for baseline BMI to minimize regression to the mean [25] and for baseline gender, age, educational attainment, marital status, smoking, cancer site, cancer disease stage, mode of treatment, and co-morbidities. In a second model (Model B), additional adjustment for baseline physical activity time was made in order to examine whether any association between baseline television viewing time and BMI change was independent of baseline physical activity time. In a third model (Model C), an interaction term (gender*baseline television viewing time) was added to examine possible gender differences in the associations between television viewing time and BMI change. Lastly, an additional model (Model D) was used to examine any (baseline television viewing*physical activity) interaction effect on BMI change, adjusted for the same confounding variables as Model B.
Results
Baseline (5 months post-diagnosis) socio-demographic and medical characteristics of (healthy weight, overweight and obese) participants included in this study are described in Table 1. Mean (SD) BMI was 26.3 (5.0) kg/m2 at baseline (n = 1,867), 27.4 (5.0) kg/m2 at 24 months post-diagnosis (n = 1,202), and 27.6 (5.0) kg/m2 at 36 months post-diagnosis (n = 1,028).
Association between baseline television viewing time and BMI at 24 months post-diagnosis
The first multiple linear regression models examined the associations between baseline television viewing time and BMI at 24 months post-diagnosis (Table 2). After adjustment for baseline BMI, socio-demographic and clinical variables, a significant positive association between 5 or more hours per day of television viewing at baseline and BMI at 24 months post-diagnosis was found. Additional adjustment for baseline physical activity level did not attenuate this association. Compared to those watching <3 h per day, those who watched 5 or more hours per day had an average increase in BMI of 0.71 kg/m2 from 5 to 24 months post-diagnosis. No significant (gender * baseline television viewing time) interaction was found (Model C: p = 0.95).
A non-significant interaction effect between baseline television viewing and baseline physical activity time was found (Model D: p = 0.09). Figure 2a shows the effect of baseline television viewing on BMI according to baseline physical activity category. Compared to those who were sufficiently active and watched television for <3 h per day (reference group), a significantly greater increase in BMI was found in those who were inactive (0 min of physical activity per week) and watched television for 5 or more hours per day at baseline. A marginally significantly greater increase in BMI was also found in those being insufficiently active (1–149 min of physical activity per week) and watching 3–4.9 h of television per day.
Regression coefficients (95% CI) for BMI change at (a) 24 and (b) 36 months post-diagnosis according to baseline television viewing and physical activity level; adjusted for gender, age, education, marital status, smoking, cancer site, cancer disease stage, treatment mode and co-morbidities. Television viewing: <3 h/day: circles; 3–4.9 h/day: triangles; ≥5 h/day: squares
Association between baseline television viewing time and BMI at 36 months post-diagnosis
The second series of multiple linear regression models examined the independent association between baseline television viewing time and BMI at 36 months post-diagnosis (Table 2). Similarly to the results for BMI at 24 months post-diagnosis, 5 or more hours per day of television viewing time at baseline was significantly associated with BMI at 36 months post-diagnosis (Model A). This association was unchanged after baseline physical activity was added to the model (Model B). The (gender * baseline television viewing time) interaction again was not significant (Model C: p = 0.13).
A significant interaction between baseline television viewing and physical activity time was found (Model D: p = 0.02). Figure 2b shows a comparable pattern to Fig. 2a. Compared to the reference group, a significantly greater increase in BMI was found in physically inactive participants who also watched 5 or more hours of television per day and in the insufficiently active participants who watched 3–4.9 h per day.
Additional analyses including participants who were underweight at baseline did not reveal substantially different results for BMI measured at either 24 months or 36 months post-diagnosis (results not shown).
Discussion
We observed a deleterious relationship between television viewing time and change in BMI among colorectal cancer survivors. Watching television for 5 or more hours per day at 5 months post-diagnosis was independently associated with a higher BMI at 24 and 36 months post-diagnosis.
At both follow-up time points in our study, stronger associations were observed between the highest category of television viewing time (5 or more hours per day) and BMI than for the middle category of television viewing time (3–4.9 h per day), where there was a positive but non-significant association with BMI. Our findings are consistent with studies of television viewing time and BMI among the general population. Blanck et al. [13] also found that stronger relationships emerged as television viewing time increased to more extreme levels. Their study found that compared to those who watched <3 h of television per day, participants had an increased likelihood of gaining more than 4.5 kg if they watched between 3 and 5 h per day [Odds ratio (OR) = 1.16], or more than 6 h per day (OR = 1.47). Hu et al. [14] showed that each 2-h-per-day increase in television viewing time was associated with a 23% increase in obesity among participants of the nurses’ health study.
One hypothesis to explain the effect of television viewing time on BMI is that high exposure to high-calorie food advertisements might stimulate individuals to consume such foods during television watching (through snacking) and also potentially increase overall daily food consumption, both giving rise to a higher energy intake [26]. Second, although we adjusted for physical activity category at baseline, there might still be residual confounding for physical activity, as we did not separately adjust for time spent in different intensities of physical activity. Previous research has shown that time spent sedentary and in light-intensity physical activity are strongly inversely correlated [27]. This suggests that watching 5 or more hours of television per day might displace a fair amount of time spent in light-intensity physical activity. Furthermore, Hu et al. [14] showed a protective effect of light-intensity activities on later obesity risk. Therefore, due to a lack of light-intensity physical activity, watching television might cause a reduction in total energy expenditure and subsequently give rise to weight gain. Prospective studies in cancer survivors, using objective measures for sedentary behavior and physical activity and measuring dietary intake are needed to further examine these potential mechanisms.
In a population-based sample of 8,357 Australian adults aged over 35 years, Dunstan et al. [28] reported that 79% of men and 81% of women watched <3 h of television per day. In our study with colorectal cancer survivors, 48% of men and 46% of women were included in this category of television viewing. This suggests that our sample of colorectal cancer survivors reported higher levels of television viewing time, compared to the general adult population. Our findings suggest a potentially important role for reducing time spent in sedentary behaviors such as television viewing, in the prevention of weight gain among colorectal cancer survivors. Comparing television viewing time between baseline and 24 months post-diagnosis (n = 1,202) and between baseline and 36 months post-diagnosis (n = 1,028), we observed minimal change in reported television viewing over time (results not shown); therefore, it would appear feasible to assess the television viewing habits of colorectal cancer survivors within the first 6 months since their diagnosis, and thus identify those at elevated risk of weight gain in following years. Commonly, during the first 6 months post-diagnosis, most colorectal cancer survivors receive regular follow-up care (and in some cases, adjuvant therapy). During this time, health professionals would be ideally placed to intervene and address negative health behaviors, including higher volumes of television viewing time.
The colorectal cancer and quality of life study is a large prospective study with a sample recruited through a population-based cancer registry. However, some sample bias does exist: fewer than 60% of the total eligible sample completed the first telephone interview, and there was an under-representation of older participants, those with rectal cancer and later stage disease. Additional sample bias occurred as the study progressed, due to missing data and participants leaving the study because they are dead or of ill health. Also, the data utilized by this study, including height and weight (used to calculate BMI), were self-reported and hence may be limited by inaccuracy of reporting and by social-desirability bias. In particular, we acknowledge that adults may underestimate weight and overestimate height [29], which would result in an underestimation of BMI. However, because individuals would be likely to underreport in a similar way at the different time points, and a difference in BMI between two time points will have lower measurement error than one single measurement, the effect of an underestimation of BMI would be expected to be smaller for the findings presented in this study, in which a change in BMI is predicted. If error remained in change in BMI, this would most likely result in the observed associations between television viewing time and weight change being weaker than are the true associations. Another limitation of this study is that not all possible confounding factors were assessed and controlled for in the analyses. In particular, we did not measure the dietary intake of participants.
While some ongoing morbidity is inevitable among cancer survivors, many of the common co-morbidities and declines in functional status may be ameliorated by changes to lifestyle. Our findings suggest that a reduction in television viewing time may have the potential to decrease unhealthy weight gain, and possible associated co-morbid conditions, among colorectal cancer survivors. Recent evidence also suggests that in addition to reducing the total volume of television viewing time, there can be beneficial metabolic effects of breaking up time spent sitting [30]. How such behavioral changes might most appropriately be addressed in colorectal cancer survivors following treatment requires further research.
References
Jones LW, Demark-Wahnefried W (2006) Diet, exercise, and complementary therapies after primary treatment for cancer. Lancet Oncol 7(12):1017–1026. doi:10.1016/S1470-2045(06)70976-7
Dunstan DW, Salmon J, Owen N et al (2004) Physical activity and television viewing in relation to risk of undiagnosed abnormal glucose metabolism in adults. Diabetes Care 27(11):2603–2609. doi:10.2337/diacare.27.11.2603
Patel AV, Rodriguez C, Pavluck AL, Thun MJ, Calle EE (2006) Recreational physical activity and sedentary behavior in relation to ovarian cancer risk in a large cohort of US women. Am J Epidemiol 163(8):709–716. doi:10.1093/aje/kwj098
Blanchard C, Stein K, Baker F et al (2004) Association between current lifestyle behaviors and health-related quality of life in breast, colorectal and prostate cancer survivors. Psychology and Health 19(1):1–13. doi:10.1080/08870440310001606507
Irwin ML, McTiernan A, Baumgartner RN et al (2005) Changes in body fat and weight after a breast cancer diagnosis: influence of demographic, prognostic, and lifestyle factors. J Clin Oncol 23(4):774–782. doi:10.1200/JCO.2005.04.036
Ferlay J, Bray F, Pisani P, Parkin D (eds) (2004) GLOBOCAN 2002: cancer incidence, mortality and prevalence worldwide. IARC Press, Lyon
Jemal A, Murray T, Ward E et al (2005) Cancer statistics, 2005. CA-A Cancer J Clin 55(1):10–30. doi:10.3322/canjclin.55.1.10
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 348(17):1625–1638. doi:10.1056/NEJMoa021423
Haydon AMM, MacInnis RJ, English DR, Giles GG (2006) Effect of physical activity and body size on survival after diagnosis with colorectal cancer. Gut 55(1):62–67. doi:10.1136/gut.2005.068189
Meyerhardt JA, Heseltine D, Niedzwiecki D et al (2006) Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol 24(22):3535–3541. doi:10.1200/JCO.2006.06.0863
Meyerhardt JA, Giovannucci EL, Holmes MD et al (2006) Physical activity and survival after colorectal cancer diagnosis. J Clin Oncol 24(22):3527–3534. doi:10.1200/JCO.2006.06.0855
Dunstan D, Salmon J, Owen N et al (2005) Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia 48(11):2254–2261. doi:10.1007/s00125-005-1963-4
Blanck HM, McCullough ML, Patel AV et al (2007) Sedentary behavior, recreational physical activity, and 7-year weight gain among postmenopausal US women. Obesity 15(6):1578–1588. doi:10.1038/oby.2007.187
Hu FB, Li TY, Colditz GA, Willett WC, Manson JE (2003) Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 289(14):1785–1791. doi:10.1001/jama.289.14.1785
Hamilton MT, Hamilton DG, Zderic TW (2007) Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 56(11):2655–2667. doi:10.2337/db07-0882
Owen N, Leslie E, Salmon J, Fotheringham MJ (2000) Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev 28(4):153–158
Salmon J, Owen N, Crawford D, Bauman A, Sallis JF (2003) Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol 22(2):178–188. doi:10.1037/0278-6133.22.2.178
Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N (2008) Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc 40(4):639–645. doi:10.1249/MSS.0b013e3181607421
Lynch BM, Baade P, Fritschi L et al (2007) Modes of presentation and pathways to diagnosis of colorectal cancer in Queensland. Med J Aust 186(6):288–291
Australian Institute of Health and Welfare (2003) The active Australia survey. A guide and manual for implementation, analysis and reporting. AIHW, Canberra
Bauman A, Armstrong T, Davies J et al (2003) Trends in physical activity participation and the impact of integrated campaigns among Australian adults, 1997–99. Aust N Z J Public Health 27(1):76–79. doi:10.1111/j.1467-842X.2003.tb00384.x
Department of Health and Aged Care (1999) National physical activity guidelines for Australians. Australian Government, Canberra
Ragland DR (1992) Dichotomizing continuous outcome variables—dependence of the magnitude of association and statistical power on the cutpoint. Epidemiology 3(5):434–440. doi:10.1097/00001648-199209000-00009
International Agency for Research on Cancer (2001) Weight control and physical activity. IARC Press, Lyon
Barnett AG, van der Pols JC, Dobson AJ (2005) Regression to the mean: what it is and how to deal with it. Int J Epidemiol 34(1):215–220. doi:10.1093/ije/dyh299
Foster JA, Gore SA, West DS (2006) Altering TV viewing habits: an unexplored strategy for adult obesity intervention? Am J Health Behav 30(1):3–14
Healy GN, Wijndaele K, Dunstan DW et al (2008) Objectively measured sedentary time, physical activity, and metabolic risk: the Australian diabetes, obesity and lifestyle study (AusDiab). Diabetes Care 31(2):369–371. doi:10.2337/dc07-1795
Dunstan DW, Salmon J, Healy GN et al (2007) Association of television viewing with fasting and 2-h postchallenge plasma glucose levels in adults without diagnosed diabetes. Diabetes Care 30(3):516–522. doi:10.2337/dc06-1996
Larsen JK, Ouwens M, Engels R, Eisinga R, van Strien T (2008) Validity of self-reported weight and height and predictors of weight bias in female college students. Appetite 50:386–389
Healy GN, Dunstan DW, Salmon J et al (2008) Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care 34(4):661–666. doi:10.2337/dc07-2046
Acknowledgments
This project was funded by the Cancer Council Queensland. Owen is supported by a Queensland Health Core Research Infrastructure grant and by NHMRC Program Grant funding (#301200). Dunstan is supported by a Victorian Health Promotion Foundation Public Health Research Fellowship.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Wijndaele, K., Lynch, B.M., Owen, N. et al. Television viewing time and weight gain in colorectal cancer survivors: a prospective population-based study. Cancer Causes Control 20, 1355–1362 (2009). https://doi.org/10.1007/s10552-009-9356-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9356-5