Abstract
Background
Ecological studies in predominantly European populations have reported higher cancer survival in areas of higher solar ultraviolet (UV) B irradiation, perhaps due to a cancer protective effect of vitamin D synthesized photochemically in the skin. Such studies have not been done in developing countries, perhaps because of lack of cancer registries that can do outcome follow-up. One minus the mortality-to-incidence ratio (1−MIR), however, can be used as a measure of survival, and MIR as a measure of fatality, in developing country cancer registries. We analyzed the association between ambient solar UVB and MIR in China.
Methods
National cancer registration data in 32 counties of China in 2004–2005 were used to estimate MIR by age, sex, and area. The accuracy of 1−MIR as a measure of survival was assessed in the Cixian County cancer registry. Contemporary satellite measurements of cloud-adjusted ambient UVB intensity at 305 nm were taken from an NASA database and spatial Kriging methods used to estimate the average daily irradiance in each county. We estimated mortality hazard ratios (HRs) per 10 mW/m2 of UVB for all cancers together, and the ten commonest cancer types by fitting a generalized linear model assuming mortality had a binomial distribution conditional on the sum of mortality and incidence, adjusted for sex, age, and location.
Results
The 5-year survival proportions for the main cancer types were in good agreement with 1−MIR in Cixian County. MIR ratios for all cancers combined were inversely associated with ambient UVB in men (HR = 0.96, 95 % CI 0.93–0.99) and women (HR = 0.91, 95 % CI 0.88–0.94) and in urban (HR = 0.95, 95 % CI 0.94–0.96) and rural areas (HR = 0.90, 95 % CI 0.87–0.93). Similar inverse associations were present for cancers of esophagus, stomach, and bladder in both sexes together and breast cancer in women. They were present in urban residents for all major cancers except liver cancer, bladder cancer, and breast cancer in women. For rural residents, most HRs were <1.0 but, with the exception of breast cancer, their upper 95 % confidence bounds were >1.0.
Conclusion
Ambient UVB was significantly inversely associated with MIR for all cancers together and four of ten cancer types. Solar UVB may increase survival from some cancers in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A number of studies have suggested that season of diagnosis, considered to be a surrogate for ambient solar UV irradiance at the time of diagnosis, is associated with survival from breast cancer and lung cancer, and possibly colon cancer and prostate cancer [1–4]. Patients diagnosed with these cancers in summer or autumn tended to have longer survival than those diagnosed in winter or spring, and it has been suggested that higher serum 25-hydroxyvitamin D concentrations due to high solar UV irradiance in summer and autumn may explain these observations [5, 6]. Other explanations have been offered for them, and some conflicting results have been reported [7–9]. These studies have all been done in populations of mainly European origin.
We have previously shown that ambient solar UVB intensity is inversely associated with mortality and incidence of a number of different cancer types in China [10]. Given the results summarized above, we considered it to be of interest to examine the association between ambient solar UVB and cancer survival in China. Since there are very few cancer registries in China that are currently able to report cancer survival, we have chosen to consider “one minus the cancer mortality-to-cancer incidence ratio (MIR),” or 1−MIR, as a surrogate for 5-year relative survival, for which it has been shown to provide a good approximation across most, but not all, types of cancer in a number of countries [11]. We have used cancer incidence and mortality registration data in 2004–2005 from 32 cancer registries in China and estimates of ambient solar UVB irradiance relevant to vitamin D synthesis from NASA satellites and, for statistical convenience, to analyze the association between MIR (not 1−MIR), effectively a surrogate for cancer fatality, and solar UVB.
Materials and methods
Cancer incidence and mortality
The National Central Cancer Registry (NCCR) of China is responsible for collecting cancer registration data from population-based cancer registries in China. Cancer registry reports have been published annually since 2007 [12], providing information for anticancer strategies. Few Chinese cancer registries have run for more than 40 years; most have been established in the last 10 years. In 2008, the national cancer registry program was established by the Ministry of Health and its population coverage is gradually increasing. There are now nearly 200 registries covering all provinces and a population of about 190 million. However, only a few of the registries have met the quality criteria to be accepted in the annual report, and they do not yet provide representative coverage of the population, especially the rural population [13].
Proportion of morphological verification (MV %), percentage of cancer cases identified with death certification only (DCO %), mortality-to-incidence ratio (MI), percentage of uncertified cancer (UB %), and percentage of cancer with undefined or unknown primary site (secondary) (O&U %) were used to evaluate the completeness, validity, and reliability of cancer statistics. Thirty-two population-based cancer registries reported high-quality cancer incidence and mortality data in 2004–2005, which were used for this analysis. The registries identified new cancer cases and deaths from all hospitals, community health centers, death registries, and the Civil Administration Bureau, which holds cremation records. Causes of death were obtained from death certificates completed by doctors for people who died in hospital and through verbal autopsies conducted by medical experts for people who died at home. Population information was obtained from official registration records. For this study, the data on cancer site (coded using ICD-10), sex, and age at diagnosis were retrieved from each cancer registry’s database. Site-, sex-, and age-specific cancer incidence rates were calculated for all cancer registries, and the analysis was limited to the cancer types used in the analysis of the National Death Survey [14]. Cancer registries’ locations were also classified as either urban or rural.
Local validation of 1−MIR as an estimator of relative survival
To see how well 1−MIR compared with corresponding relative survival estimates for different cancers, data on both were obtained from the Cixian County Cancer Registry, Hebei Province, which was established in 1974 and covers a population of 633,802 people. New cancer cases in 2000–2002 were followed up passively to the end of 2007 by matching them with the vital statistics database. In addition, cancer registry staff actively followed up cancer patients annually by phone, and home visits if they were not found to have died, and sought information from the local doctors when necessary. Because the County is largely rural, doctors are familiar with residents and almost always know their vital status, even when they have died outside the County. The follow-up rate was close to 100 %. The analysis was limited to the main cancer types: lung cancer, esophageal cancer, liver cancer, stomach cancer, colorectal cancer, breast cancer, cervical cancer, leukemia, and lymphoma. Due to the limited numbers of cancer cases, the sexes were combined for the analyses.
Ultraviolet B measurements
The estimated daily cloud-adjusted ambient solar UVB irradiance at 305 nm, expressed in milliwatts per meter squared (mW/m2), was obtained on a 1° of latitude by 1° of longitude grid for the whole of China from an NASA Goddard Space Flight Center Data Archive Center database of readings from the total ozone mapping spectrometer (TOMS) mounted on the Nimbus-7 satellite [15]. TOMS measures solar radiation scattered back from the atmosphere in six wavelength channels and extraterrestrial solar radiance in the same six wavelength channels from which UV irradiances at the earth’s surface at the time of the satellite overpass, among other things, can be estimated [16]. We estimated the UV measure used for analysis by averaging daily estimates from 2004 to 2005, which made the assumption that the relative distribution of annual UV irradiance for counties in China was stable over time. ArcGIS 9.1 (http://www.esri.com/software/arcgis/index.html) software was used for spatial modeling of the UVB data, and the Kriging method of interpolation was used to obtain County-level average daily irradiance over the whole year. UVB at 305 nm was chosen because it is the available wavelength that corresponded most closely to the peak in the action spectrum for UVB-caused vitamin D production in skin [17]. We have previously used similar data for an analysis of the association of cancer incidence and mortality with UVB irradiance in China [10].
Statistical analysis
For comparison between values of 1−MIR and relative 5-year survival rates in Cixian County, we calculated the observed 5-year survival rate for all cancers and for each cancer type for males and females together. Life table data from the Fifth National Census 2000 for China as a whole were then used to calculate expected 5-year survival rates using the Ederer II method with 1-year intervals [18]. Relative survival rates were then calculated as the ratio of the observed survival rate in people diagnosed with cancer or a specific cancer type to their expected survival rate, based on the overall survival probabilities in the general population. Five-year relative survival is approximately equal to the corresponding cancer-specific survival rate and is used in preference to the latter when cause of death may not be accurately determined. The Z test was used to evaluate the statistical significance of differences between 1−MIR and relative survival, with Z calculated by the formula, where the number of deaths is M and the number of incidence cases is I:
Given the total number N = M+I for mortality and incidence combined, the number of deaths M has a binomial distribution with probability M/N for N trials. Using the delta method,
A generalized linear model was fitted to evaluate the relationship between the excess mortality hazard (mortality in excess of that expected from general population mortality rates) and UVB irradiance, with the relationship expressed as the ratio of the excess mortality hazard after a ten mW/m2 increase in UVB relative to the excess mortality hazard at the previous UVB level. In the model, counts of cancer deaths for each registry, specific to cancer type, sex, age group (5-year age groups for age over 25, i.e., 25–29, 30–34, 35–39,…, 85+), and location (urban or rural), were modeled as binomial outcomes, conditional on the sum of the incident cancer cases and deaths, with age, sex, location, and UVB values as covariates. We assumed that cause-specific survival was estimated by S = 1−M/I, with the mortality binomially distributed conditional on (M + I) trials with probability p = M/(I + M). Then, S = (1−2p)/(1−p) and p = (1−S)/(2−S). We modeled the survival function using a complementary log–log function, such that S = exp (−exp(α + β*UVB + γ*age + ψ*sex + ϕ*location)), where α, β, γ, ψ, and ϕ were the estimated parameters. Then, β is interpreted as a log (hazard ratio) for a unit increase in UVB. The forward link function for the generalized linear model is defined as follows:
p = (1−exp(−exp(α + β*UVB + γ*age + ψ*sex + ϕ*location)))/(2−exp(−exp(α + β*UVB + γ*age + ψ*sex + ϕ*location))).
Separate analyses were performed by cancer type, with sex, age, and location used as explanatory factors; analyses were also performed for each sex and for each location. Interactions in the association with UVB exposure by sex and by location were formally assessed using likelihood ratio tests comparing models with main effects only with models with an interaction term between either UVB exposure and sex or UVB exposure and location.
For ease in presentation and understanding, we have expressed the hazard ratios in the text as the excess mortality hazard ratio (EMHR) expressed in percentage terms. For example, an EMHR of 5 % indicates that the hazard of death after diagnosis from the cancer in question is estimated to increase by 5 % with an increase in ambient UVB of 10 mW/m2 (i.e., the hazard ratio is estimated to be 1.05 per 10mW/m2 increase in UVB).
SAS version 9.2 (SAS Institute, Cary, NC) was used for the statistical analyses.
Results
Validation study
In our limited validation of 1−MIR as a surrogate for relative survival in Cixian County, 1−MIR for all cancers in males and females was 0.17. The 5-year relative survival rate for all cancers was very similar at 18.2 % (0.182), and this close similarity was seen across all nine individual cancer types studied, with the possible exception of lymphoma, for which there were the fewest incident cases (Table 1). There was a strong linear association between 1−MIR and 5-year relative survival for the different cancer types (intercept = 0.55, 95 % CI −2.77, 3.87 %; slope = 0.99, 95 % CI 0.83, 1.15; adjusted R 2 = 0.94).
UVB study
In the 32 cancer registries in 2004–2005, there were 267,433 incident cases and 175,676 cancer deaths in 104,204,536 person-years of experience, with a crude annual cancer incidence rate of 256.64 per 100,000 and mortality rate of 168.59 per 100,000. The person-years of experience were substantially less in rural (28,487,546 person-years) than urban areas (75,736,593 person-years). Age standardized to Segi’s world population, the overall cancer incidence rate was 182.8 per 100,000, ranging from 66.0 to 462.2 across the 32 registries, which compares with an estimated global range, by country, of 54.9–317.0 [19], and mortality rate was 115.4 per 100,000, ranging from 45.4 to 350.5 (global range 48.9–154.2). While these ranges may include some under estimation of the lowest and over estimation of the highest rates, the 32 registries are distributed across the whole country and the regions they cover vary widely in their environmental, the cultural, and behavioral characteristics of their populations and the nature of their health services. The crude 1−MIR for all cancers was 0.34; it ranged from 0.13 to 0.47 and was 0.37 age-adjusted, range 0.14–0.49.
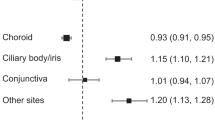
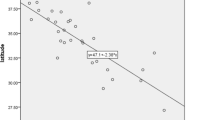
The estimated annual average daily UVB irradiance in the studied cancer registry regions ranged from 26.57 to 71.25 mW/m2, which compares with an approximately global range for major cities from 8.56 in Helsinki to 82.47 in Singapore (Appendix Tables 4, 5). The hazard ratios for a 10 mW/m2 increase in solar UVB (Table 2) suggested that, for all cancers, the hazard of death from the cancer fell with increasing UVB irradiance (EMHR −8 % per 10 mW/m2), as they also did for some major cancer types: esophagus cancer, stomach cancer, female breast cancer, and bladder cancer (EMHR varied from −10 to −20 % per 10 mW/m2) (Table 2). Illustrative scatter plots of the relationship of 1−MIR with UVB irradiance are shown in Fig. 1 for all cancers together and cancers of the breast and bladder, the two strongest associations. Trends in EMHRs for other cancers studied varied from −9 to +5 % per mW/m2 but had 95 % confidence intervals that included the null value. For only two did it appear that EMHR increased with increasing UVB irradiance (liver and leukemia). The apparent downtrend in EMHR with increasing UVB was stronger in females than males for all cancers (p = 0.02), perhaps because of a strong downtrend for breast cancer.
The EMHR for all cancers together appeared to fall with increasing UVB in both urban and rural areas, but more strongly in rural (−10 % per 10 mW/m2) than urban areas (−5 %) (p = 0.034; results not shown). Among the different cancer types, EMHRs appeared to fall consistently with increasing UVB in urban areas, with weak or no evidence of this pattern only for liver cancer, breast cancer, and leukemia. The pattern was similar in rural areas, although the evidence for associations of EMHR for individual cancer types with UVB was weaker, perhaps due to the smaller rural than urban population covered by this analysis. There was strong evidence, though, for discordance in the EMHR for breast cancer between urban and rural areas, which appeared to increase in urban areas with increasing UVB (4 % per mW/m2, 95 % CI 1, 8 %) but to fall when UVB was increasing in rural areas (−12, 95 % CI −20, −4 %) (Table 3).
Discussion
Previous studies have found evidence of an inverse association between solar UVB exposure and cancer incidence or mortality in China [10, 20, 21]. The results of this analysis suggest that there is also an inverse association between UVB exposure and fatality after a diagnosis of cancer or, as more commonly expressed, a direct association between solar UVB exposure and survival from cancer.
Arguably, our study is limited by the use of MIR as a surrogate for cancer fatality. MIR is commonly used as an indicator of completeness of cancer registration [22]. 1−MIR could be used as a surrogate for 5-year survival because cancer deaths usually occur within 5 years after diagnosis, and it can be very close to the 5-year survival rate obtained by following up new cancer cases [23]. In a recent seven country evaluation, 1−MIR was found to give a good approximation to 5-year relative survival for most cancers, but underestimated or overestimated survival for some cancers, such as breast cancer, esophageal cancer, liver cancer, and oral cavity cancer [11]. However, 1−MIR probably cannot be used as general substitute for directly estimated survival [24]. It is only really suitable for measuring survival when cancer registration and recording of deaths are complete and when incidence and survival are comparatively stable [22, 25], conditions that probably rarely obtain, particularly in registries for which follow-up of cancer patients is not feasible.
Notwithstanding these issues, the comparisons we have made between 1−MIR and 5-year relative survival from cancer in Cixian County have shown very good agreement (Table 1). Therefore, we would argue that 1−MIR or MIR can be used as surrogates for survival or fatality in China in analyses such as this one, with the expectation that valid results will be obtained.
Studies in Europe and Australia have reported positive associations between solar UV exposure and cancer survival by using season of diagnosis as an indicator of ambient solar UV at the time of diagnosis. They have generally found survival to be greater with diagnosis in summer or autumn than winter or spring, with positive results reported for cancers of the colon, colon and rectum, lung, liver, breast and prostate, cutaneous melanoma, brain cancer, leukemia, and Hodgkin’s lymphoma [3–5, 9, 26–32]. While the numerical balance is in favor of positive studies, some studies have reported negative or contrary findings for colon and rectal cancer [27], breast cancer [7, 9], prostate cancer [7, 27], and cutaneous melanoma [33]. In addition, a detailed reexamination of results from the United Kingdom [27] found that the peak in survival in summer may have been due to underlying seasonal variation in all cause mortality; however, an apparent benefit of diagnosis in autumn persisted [8]. The positive findings gain plausibility from the increasing number of studies, mainly from the United States and Europe, which have reported positive associations between generally prospectively assessed blood 25-hydroxyvitamin D concentrations and survival from cancer: including from cancers of colon and rectum, lung, breast and prostate, cutaneous melanoma, non-Hodgkin’s lymphoma, and leukemia [34–44]. Negative findings for cancers of the lung and breast and cancer in head and neck have been reported [45–47].
There is little concurrence between our results obtained using a geographically based indicator of solar UV exposure and those obtained using season of diagnosis. The only clear concurrence is for breast cancer. There is not clear concurrence for colon and rectal cancer and lung cancer, although our results are in the same direction as those previously reported. No previous studies have reported on cancers of the esophagus, stomach, and bladder, for which we observed inverse associations of fatality with solar UVB.
The inverse associations we observed between solar UVB irradiance and cancer fatality were generally stronger in rural areas than in urban areas, perhaps because outdoor activity is more common in rural residents. Only for nasopharyngeal cancers was there a clear difference in the opposite direction. This may, perhaps, relate to the concentration of this cancer in the south of China, which is probably genetically related [48]. The inverse association was also stronger in females than males, partly, although not exclusively, because of the strong inverse association with breast cancer. This inverse association was exclusive to women resident in rural areas, perhaps because urban women are unlikely to expose themselves very much to the sun.
It is a potential limitation of this study that we did not have information on diet or outdoor activity, both of which are likely to be correlated with ambient UVB exposure and might explain associations between ambient UVB and cancer outcome. Additionally, there were comparatively few registries, with limited coverage of China, on which we could base our analyses. However, the population coverage was over 100 million, and there were 267 thousands new cases and 176 thousands cancer deaths in the period covered, which may be considered large for an ecological study.
Our study results provide support for an inverse relationship between ambient solar UVB radiation and cancer fatality in China. This is the first such study in an Asian population, and it supports the results of studies in largely European origin populations, which suggest that outcome is better for a range of different cancers if diagnosed when or where ambient UV is high. These observations, together with increasing evidence from cohort studies of a positive association between blood vitamin D and longer survival from cancer, should encourage conduct of trials of vitamin D in improving cancer outcome.
References
Grant WB, Juzeniene A, Lagunova Z et al (2011) Vitamin D levels in Norway may be inadequate to reduce risk of breast cancer. Int J Cancer 128(9):2249–2250
Porojnicu AC, Robsahm TE, Dahlback A et al (2007) Seasonal and geographical variations in lung cancer prognosis in Norway. Does Vitamin D from the sun play a role? Lung Cancer 55(3):263–270
Moan J, Porojnicu AC, Robsahm TE et al (2005) Solar radiation, vitamin D and survival rate of colon cancer in Norway. J Photochem Photobiol, B 78(3):189–193
Robsahm TE, Tretli S, Dahlback A et al (2004) Vitamin D3 from sunlight may improve the prognosis of breast-, colon- and prostate cancer (Norway). Cancer Causes Control 15(2):149–158
Porojnicu A, Robsahm TE, Berg JP et al (2007) Season of diagnosis is a predictor of cancer survival. Sun-induced vitamin D may be involved: a possible role of sun-induced Vitamin D. J Steroid Biochem Mol Biol 103(3–5):675–678
Zhou W, Suk R, Liu G et al (2005) Vitamin D is associated with improved survival in early-stage non-small cell lung cancer patients. Cancer Epidemiol Biomarkers Prev 14(10):2303–2309
Holmberg L, Adolfsson J, Mucci L et al (2009) Season of diagnosis and prognosis in breast and prostate cancer. Cancer Causes Control 20(5):663–670
Roychoudhuri R, Robinson D, Coupland V et al (2009) Season of cancer diagnosis exerts distinct effects upon short- and long-term survival. Int J Cancer 124(10):2436–2441
Teilum D, Bjerre KD, Tjonneland AM et al (2012) Breast cancer survival and season of surgery: an ecological open cohort study. BMJ Open 2:e000358
Chen W, Clements M, Rahman B et al (2010) Relationship between cancer mortality/incidence and ambient ultraviolet B irradiance in China. Cancer Causes Control 21(10):1701–1709
Asadzadeh Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML et al (2011) The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Public Health 21(5):573–577
National Central Cancer Registry (2008) Disease prevention and control bureau ministry of health: 2004 chinese cancer registry annual report. Union Medical College press, Beijing
Li GL, Chen WQ (2010) Representativeness of population-based cancer registration in China—comparison of urban and rural areas. Asian Pac J Cancer Prev 10:559–564
Li GL, Chen WQ (2009) Representativeness of population-based cancer registration in China—comparison of urban and rural areas. Asian Pac J Cancer Prev 10(4):559–564
ftp://toms.gsfc.nasa.gov/pub/eptoms/data/uv_ery_4_wavelengths/uv305/. Accessed on 26/03/2013
Herman JR, Krotkov N, Celarier E et al (1999) Distribution of UV radiation at the Earth’s surface from TOMS-measured UV-backscattered radiances. J Geophys Res Atmos 104(D10):12059–12076
Bjorn LO (2010) Vitamin D synthesis may be independent of skin pigmentation only with UV of short wavelength. J Invest Dermatol 130(12):2848–2850
Ederer F, Heise H: Instructions to IBM 650 programmers in processing survival computations. Methodological note No. 10, End Results section National Cancer Institute, Bethesda, MD (1959)
Ferlay J, Shin HR, Bray F et al (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917
Grant WB (2007) Does solar ultraviolet irradiation affect cancer mortality rates in China? Asian Pac J Cancer Prev 8(2):236–242
Archer VE (1989) Latitudinal variation of digestive tract cancers in the US and China. Nutr Cancer 12(3):213–223
Parkin DM, Bray F (2009) Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer 45(5):756–764
Valean S, Armean P, Resteman S et al (2008) Cancer mortality in Romania, 1955–2004. Digestive sites: esophagus, stomach, colon and rectum, pancreas, liver, gallbladder and biliary tree. J Gastrointestin Liver Dis 17(1):9–14
Pisani P, Parkin DM, Ferlay J (1993) Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int J Cancer 55(6):891–903
Hebert JR, Daguise VG, Hurley DM et al (2009) Mapping cancer mortality-to-incidence ratios to illustrate racial and sex disparities in a high-risk population. Cancer 115(11):2539–2552
Porojnicu AC, Lagunova Z, Robsahm TE et al (2007) Changes in risk of death from breast cancer with season and latitude: sun exposure and breast cancer survival in Norway. Breast Cancer Res Treat 102(3):323–328
Lim HS, Roychoudhuri R, Peto J et al (2006) Cancer survival is dependent on season of diagnosis and sunlight exposure. Int J Cancer 119(7):1530–1536
Boniol M, Armstrong BK, Dore JF (2006) Variation in incidence and fatality of melanoma by season of diagnosis in new South Wales. Australia. Cancer Epidemiol Biomarkers Prev 15(3):524–526
Porojnicu AC, Robsahm TE, Ree AH et al (2005) Season of diagnosis is a prognostic factor in Hodgkin’s lymphoma: a possible role of sun-induced vitamin D. Br J Cancer 93(5):571–574
Grant WB (2012) Ecological studies of the UVB-vitamin D-cancer hypothesis. Anticancer Res 32(1):223–236
Turna A, Pekcolaklar A, Metin M et al (2012) The effect of season of operation on the survival of patients with resected non-small cell lung cancer. Interact Cardiovasc Thorac Surg 14(2):151–155
Hakko H, Rasanen P, Niemela A et al (2009) Season of tumor surgery in relation to deaths among brain tumor patients: does sunlight and month of surgery play a role in brain tumor deaths? Acta Neurochir (Wien) 151(11):1369–1375
Jayasekara H, Karahalios E, Thursfield V et al (2009) Season of diagnosis has no effect on survival from malignant melanoma. Int J Cancer 125(2):488–490
Zhou W, Heist RS, Liu G et al (2007) Circulating 25-hydroxyvitamin D levels predict survival in early-stage non-small-cell lung cancer patients. J Clin Oncol 25(5):479–485
Newton-Bishop JA, Beswick S, Randerson-Moor J et al (2009) Serum 25-hydroxyvitamin D3 levels are associated with breslow thickness at presentation and survival from melanoma. J Clin Oncol 27(32):5439–5444
Ng K, Wolpin BM, Meyerhardt JA et al (2009) Prospective study of predictors of vitamin D status and survival in patients with colorectal cancer. Br J Cancer 101(6):916–923
Tretli S, Hernes E, Berg JP et al (2009) Association between serum 25(OH)D and death from prostate cancer. Br J Cancer 100(3):450–454
Goodwin PJ, Ennis M, Pritchard KI et al (2009) Prognostic effects of 25-hydroxyvitamin D levels in early breast cancer. J Clin Oncol 27(23):3757–3763
Mezawa H, Sugiura T, Watanabe M et al (2010) Serum vitamin D levels and survival of patients with colorectal cancer: post hoc analysis of a prospective cohort study. BMC Cancer 10:347
Vrieling A, Hein R, Abbas S et al (2011) Serum 25-hydroxyvitamin D and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res 13(4):R74
Fedirko V, Riboli E, Tjonneland A et al (2012) Prediagnostic 25-hydroxyvitamin D, VDR and CASR polymorphisms, and survival in patients with colorectal cancer in western European populations. Cancer Epidemiol Biomarkers Prev 21(4):582–593
Tretli S, Schwartz GG, Torjesen PA et al (2012) Serum levels of 25-hydroxyvitamin D and survival in Norwegian patients with cancer of breast, colon, lung, and lymphoma: a population-based study. Cancer Causes Control 23(2):363–370
Drake MT, Maurer MJ, Link BK et al (2010) Vitamin D insufficiency and prognosis in non-Hodgkin’s lymphoma. J Clin Oncol 28(27):4191–4198
Thomas X, Chelghoum Y, Fanari N et al (2011) Serum 25-hydroxyvitamin D levels are associated with prognosis in hematological malignancies. Hematology 16(5):278–283
Heist RS, Zhou W, Wang Z et al (2008) Circulating 25-hydroxyvitamin D, VDR polymorphisms, and survival in advanced non-small-cell lung cancer. J Clin Oncol 26(34):5596–5602
Jacobs ET, Thomson CA, Flatt SW et al (2011) Vitamin D and breast cancer recurrence in the Women’s Healthy Eating and Living (WHEL) Study. Am J Clin Nutr 93(1):108–117
Meyer F, Liu G, Douville P et al (2011) Dietary vitamin D intake and serum 25-hydroxyvitamin D level in relation to disease outcomes in head and neck cancer patients. Int J Cancer 128(7):1741–1746
Wee JT, Ha TC, Loong SL et al (2010) Is nasopharyngeal cancer really a “Cantonese cancer”? Chin J Cancer 29(5):517–526
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, W., Armstrong, B.K., Rahman, B. et al. Relationship between cancer survival and ambient ultraviolet B irradiance in China. Cancer Causes Control 24, 1323–1330 (2013). https://doi.org/10.1007/s10552-013-0210-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0210-4