Abstract
Background
Over the past few decades, an increase in the incidence of thyroid cancer has been recorded in many countries around the world including Australia. Heightened medical surveillance and increased technological sensitivity could be contributing to greater detection of asymptomatic disease.
Objectives
To describe the pathways to diagnosis of thyroid cancer for a cohort of newly diagnosed patients in New South Wales (NSW), Australia, and compare these pathways by age, sex, place of residence, ethnic background, medical insurance status, and disease characteristics.
Methods
A total of 452 newly diagnosed cases of thyroid cancer were recruited through the population-based NSW Central Cancer Registry. Participants completed a questionnaire and diary of doctor visits and investigations that led to their diagnosis. Tumor characteristics were obtained from pathology reports.
Results
Forty percent of patients initially presented to their doctor with a lump or symptom specific to thyroid cancer and 60% had their cancer detected incidentally during a medical encounter. Men were more likely than women to be diagnosed after imaging for another health concern versus reporting a thyroid lump or symptom (p = 0.001). Thyroid cancer diagnosis after imaging for another health concern increased with age (p = 0.023), and larger tumors were less likely to be diagnosed after treatment for a benign thyroid disease (p = 0.040).
Conclusion
As the majority of participants had incidental diagnoses, the reported incidence of thyroid cancer is likely to be influenced by diagnostic technology and medical surveillance practices. This, however, probably only partly explains the observed rise in the incidence of thyroid cancer in NSW.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An increase in the incidence of thyroid cancer has been reported in many countries over the past few decades [1–5] and has been particularly marked in the Australian state of New South Wales (NSW) [5]. The age-standardized thyroid cancer rate in NSW women increased from 2.3 per 100,000 person-years in the period 1973–1977 to 8.1 per 100,000 in 1998–2002, a 252% increase, while for the same period in the USA (SEER: White data), the rates in women increased from 5.4 to 10 per 100,000, an 85% increase [5]. The age-standardized thyroid cancer rate in NSW men increased from 0.9 per 100,000 person-years in the period 1973–1977 to 2.5 per 100,000 in 1998–2002, a 178% increase. In the USA (SEER: White data), a 52% increase in the incidence of thyroid cancer occurred over this same period [5].
Internationally, the increasing thyroid cancer incidence has been found to be primarily due to an increase in the incidence of the papillary type of thyroid cancer and, in many cases, has been found to be due to a rise in the diagnosis of microcarcinomas [1, 2, 4, 6, 7].
The reason for these changes remains unclear; however, a common hypothesis is that changes in diagnostic, surgical, and pathological practices have made it easier to identify small, asymptomatic thyroid nodules that may never have progressed to become clinical disease [4, 8]. Autopsy studies suggest that the prevalence of small thyroid carcinomas is many times that of clinically apparent cancer [9], so it is possible that the increase in thyroid cancer incidence is due to increased detection of these tiny, asymptomatic tumors rather than any increase in the real incidence of the disease. This theory is somewhat supported by the observed stable mortality rates [10] and the finding that in many countries the increase in thyroid cancer has been greatest for smaller tumors [4, 6, 11, 12].
Other research, however, supports the alternative hypothesis that there has been a real increase in thyroid cancer incidence [13–15]. As survival from well-differentiated thyroid cancer is generally very high, and the disease is treated with a well-established and successful protocol, it is possible that a stable mortality rate despite an increasing incidence rate does not indicate overdiagnosis of subclinical disease to the degree that it does for other, more aggressive cancers. A real increase in thyroid cancer could be due to the general population’s exposure to a known or unidentified risk factor, but the particular exposure(s) is/are not known [15, 16]. The known risk factors for thyroid cancer are exposure to ionizing radiation and a history of benign thyroid nodules and goiter [17]. There is also some evidence that dietary iodine intake and hormonal factors influence the etiology of thyroid cancer, but results from studies examining these factors remain inconsistent [18, 19].
Fortunately, the mortality rate for thyroid cancer is very low, but the striking increase in thyroid cancer incidence experienced in NSW and elsewhere over the past 30 years is still of great concern. If the increase is real, and due to an environmental exposure, action may be taken to reduce the population’s exposure to this risk factor. If, however, the increase in thyroid cancer incidence is due to increased medical surveillance and diagnostic sensitivity, then there may be concerns about the personal and public cost of overtreatment that need to be addressed.
This study explored the possibility that thyroid cancer incidence in NSW is influenced by the detection of asymptomatic disease. The aims were to describe the pathways to the diagnosis of thyroid cancer for a cohort of newly diagnosed thyroid cancer patients in NSW and to compare pathways in groups of people defined by age, sex, place of residence, ethnic background, medical insurance status, and disease characteristics.
Materials and methods
Study design
The study was a population-based cross-sectional study of newly diagnosed cases of thyroid cancer in NSW, Australia. The study was approved by the Cancer Council NSW and Cancer Institute NSW’s Human Research Ethics Committees.
Subjects and recruitment
Patients with thyroid cancer were ascertained directly from notifications to the population-based NSW Central Cancer Registry (CCR). Patients were eligible to participate if they were diagnosed in the period May 1, 2006, to August 31, 2008, aged between 18 and 79 years at diagnosis, had a pathologically confirmed diagnosis of papillary, follicular, or medullary cancer, and were able to provide written informed consent. These histological types were included because the observed increases in thyroid cancer incidence have primarily been driven by increases in papillary thyroid cancer, because these three types of thyroid cancer make up more than 90% of all new thyroid cancer cases in NSW [20], and because the excluded, rare types of thyroid cancer (including anaplastic carcinoma) behave very differently from the majority of thyroid cancers.
The CCR asked eligible patients’ diagnosing doctors for consent to contact their patients about the study and then contacted patients to obtain their consent to pass their details on to the researchers. The researchers then provided patients with additional information and the study materials. After 21 days, non-responding patients were followed up by telephone or with a second letter if telephone contact was unsuccessful.
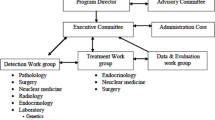
Of the 1024 eligible patients identified by the CCR, 556 (54%) agreed to have their contact details passed on to the researchers, and 452 (81%) of these patients then participated in the study (44% participation rate), as shown in Fig. 1.
The median time from thyroid cancer diagnosis to completing the study questionnaire was 6 months (interquartile range [IQR] 3–9).
Sample size
Sample size calculations were based on 2001 incidence rates of thyroid cancer in NSW [21]. It was estimated that approximately 663 new cases of papillary, follicular, or medullary thyroid cancer would occur in 18 months. Experience from previous studies using a similar recruitment process predicted that 60–70% of all new eligible cases would be recruited [22], resulting in at least 400 participants. This number of participants would provide at least 80% power to detect small differences in dichotomous comparisons.
Data collection
Participating patients self-completed a two-part questionnaire. The first part of the questionnaire requested information on patients’ demographic characteristics (age, education, country of birth, etc.), diet, past exposure to risk factors, medical history, and reproductive history (for women only). The second part of the questionnaire was a structured diary that sought information on the patients’ medical appointments and procedures prior to their thyroid cancer diagnosis.
To test the accuracy of the self-report questionnaire, a small validation study was completed during the early stages of recruitment. With doctor and patient consent, the self-reported responses to questions regarding the medical history and diagnostic pathway for 46 study participants were compared with the information recorded in their medical records. A high level of agreement was found (data not reported).
Information on a pre-operative diagnostic fine-needle aspiration (FNA), details of the surgical procedure, type and focality of tumors, other thyroid disease in the sample, primary tumor size, spread of disease, invasion, lymph node involvement, and number of blocks taken and sampled was obtained from pathology reports held by the CCR.
Additional data were obtained from the CCR for all study participants including age at diagnosis, date of diagnosis, local government area (LGA) and area health service (AHS) of residence at the time of diagnosis, tumor morphology code, and spread of disease. Aggregate data for eligible non-participants were provided so the two groups could be compared.
Outcome measures
The responses recorded in the diary section were used to categorize patients into one of five distinct pathways to diagnosis: (1) Initially presented due to patient’s concern about a mass in their neck or obstructive symptom (Patient detected), (2) A doctor noticed a lump in the patient’s neck of which they were unaware (Doctor detected), (3) Tumor incidentally found during diagnostic imaging for another health problem (Imaging), (4) Cancer diagnosed after surgery for a benign thyroid disorder (After benign disease), or (5) Any other pathway (Other). Patients categorized in pathways 1 to 3 specifically described the reasons for their first medical appointment and subsequent treatment. Patients in group 4 reported a diagnosis of benign thyroid disease at least 2 months prior to their thyroid cancer diagnosis, and their responses to questions regarding benign thyroid disease history were consistent with this pathway. The fifth group comprised any patients whose diagnostic pathway did not clearly follow the other defined pathways.
Statistical analysis
Participants’ characteristics were summarized using proportions for categorical variables or medians and interquartile ranges for continuous variables. Diagnostic pathways were compared across groups of patients using chi-squared tests. Multinomial logistic regression was used to identify the variables that were significantly and independently related to the pathways to diagnosis. The Patient detected pathway was the base outcome category for comparisons with the Doctor detected, Imaging, and After Benign disease categories. The Other pathway was excluded from the regression analysis due to small numbers of participants. Covariates related to the study objectives were included in the regression model. Age and tumor size were included as continuous variables to allow finer adjustment for confounding and to avoid wide categories and small cell sizes for some covariate/pathway combinations. All pairwise interaction terms were fitted individually and none reached statistical significance.
We used an adaptive algorithm described in detail elsewhere [23] to examine the appropriateness of the assumptions of linear effects for the continuous covariates of age and tumor size. Briefly, this involved fitting a number of exploratory models in which the functional forms of age and tumor size were modeled as first- or second-degree fractional polynomials with powers −2, −1,−0.5, 0, 0.5, 1, 2, or 3. The deviance of each exploratory model was then compared with the deviance of the linear model for evidence of significantly better model fit. No evidence was found against the assumptions of linearity for age and tumor size.
Initial statistical analysis was performed using the statistical software package SPSS v15.0 (SPSS for Windows, Rel. 15.0.1. Chicago: SPSS Inc., 2006), and multinomial logistic regression analyses were performed using STATA 11 software (StataCorp 2010 Statistical Software: release 11.0, STATA: College Station, TX, USA).
Modeling the effects of pathways to diagnosis on thyroid cancer incidence over time
To investigate how changes in thyroid cancer patients’ diagnostic pathways might have influenced the reported incidence of the disease, we used the estimated proportions of cases diagnosed via the different pathways to estimate the additional numbers of cases that may have been diagnosed and their impact on the incidence rates of thyroid cancer in NSW from 1980 to 2006. We assumed that in 1980 all thyroid cancer cases were patient detected, so that the equivalent of the proportion of patients who were diagnosed via the Doctor detected, Imaging, After benign disease, and Other pathways in our cohort would have gone undiagnosed. If the increase in thyroid cancer incidence over the period 1980–2006 was driven entirely by the diagnosis of additional cases via these incidental pathways, then adding the ‘potential cases’ to the 1980 incidence rates and applying these to the 2006 population should provide incidence rates similar to those recorded in 2006. As the assumption that there were no patients diagnosed via the non-patient-detected pathways in 1980 is unlikely, this model should overestimate the ‘potential’ 2006 incidence rate and therefore underestimate any real increase in thyroid cancer incidence.
We calculated the number of ‘potential cases’ in each 10-year age group in 1980 by adding to the reported numbers of thyroid cancer cases [24] additional cases equivalent to the proportions of patients diagnosed via the non-patient-detected pathways. Using the 1980 age-specific populations, the potential age-specific incidence rates for 1980 were estimated. These new rates were then applied to the estimated 2006 population [25] to calculate the ‘potential’ incidence rate in 2006, which was then compared to the reported 2006 rate [25].
Results
Characteristics of the sample
The majority of the participants were women (76%). The median age at diagnosis was 48 years for women (IQR 40–57) and 53 years for men (IQR 42.5–63). The median tumor size for women and men was 10 mm (IQR 4–20) and 15 mm (IQR 5–35), respectively. Table 1 shows the characteristics of the sample.
Using aggregated data provided by the CCR, the study sample (n = 452) was compared to the non-participating eligible thyroid cancer patients (n = 572). There were no significant differences in proportions for sex, age at diagnosis, cancer type, or disease spread at diagnosis between participants and eligible non-participants (see Table 2). There was, however, a significant difference in place of residence (p < 0.001), with an over-representation of residents from rural and other urban areas in the study sample.
Pathways to the diagnosis of thyroid cancer
Forty percent of patients were diagnosed after they noticed a lump or obstruction in their neck (Patient detected), 16% were diagnosed after a doctor noticed a lump in their neck (Doctor detected), 11% had their tumor discovered as an incidental finding of an imaging procedure for some other health problem (Imaging), 26% were diagnosed with thyroid cancer after they had been diagnosed and treated for a benign thyroid disorder (After benign disease), and 7% had experienced another pathway (Other) (Table 3).
The weighted proportions across pathways adjusting for the differences in the distribution by place of residence between the sample and all eligible thyroid patients were very similar to those in the sample (Table 3).
Only 38.5% of patients had received a definitive cancer diagnosis prior to thyroid surgery. A non-statistically significant larger proportion of women (63%) were diagnosed after surgery than men (55%, p = 0.15).
Factors associated with pathways to diagnosis
From bivariable analysis, the pathways to diagnosis varied significantly by age group (p = 0.009), sex (p < 0.001), tumor size (p < 0.001), spread of cancer at diagnosis (p = 0.006), treatment for another disease at the time of diagnosis (p = 0.02), and current work status (p = 0.001).
Variables that were not statistically significantly associated with the pathways to diagnosis included health insurance status, education level, smoking, alcohol consumption, number of other illnesses, previous cancer, family history of thyroid cancer, time from last pregnancy for women, and cancer type. Although not statistically significant, there were some differences in cancer types across the pathways in women, where papillary tumors were more often discovered after diagnosis for a benign thyroid disorder than follicular and medullary type tumors (p = 0.14). These other types were more common for patients who initially noticed a symptom or thyroid mass.
Results from the multinomial logistic regression model including age (continuous), sex, place of residence, place of birth, medical insurance status, and disease characteristics (treatment for another disease at the time of diagnosis, cancer type, tumor size (continuous) and spread of disease at diagnosis) are shown in Table 4. While the pathways to diagnosis varied significantly according to current work status, this variable was not included in the model as it was strongly associated with age. After adjusting for all factors in the model, pathways to diagnosis varied significantly in men and women (p = 0.001) and by age (p = 0.023) and tumor size (p = 0.040). Men were more likely than women to be diagnosed after the doctor noticed a lump (vs. patient detected) (OR 2.14, 95% CI 1.06, 4.30) or as an incidental finding of imaging (OR 2.37, 95% CI 1.11, 5.09). The odds of thyroid cancer being diagnosed as an incidental finding of imaging (vs. patient detected) increased with age (per year increase, OR 1.05, 95% CI 1.02, 1.08). Larger tumor size decreased the odds of being diagnosed after treatment for benign thyroid disease (vs. patient detected) (per mm increase, OR 0.97, 95% CI 0.95, 0.99).
The effect of disease spread at diagnosis was marginally non-significant (p = 0.056). The odds of patients with tumor spread beyond the thyroid having their cancer initially detected by a doctor (vs. patient detected) were 57% lower (OR 0.43, 95% CI 0.19, 0.95) than patients with cancer localized to the thyroid. Patients with cancer spread beyond the thyroid also had 62% lower odds (OR 0.38, 95% CI 0.19, 0.76) of having their cancer diagnosed after treatment for a benign thyroid disease (vs. patient detected) than patients with localized cancer.
Although pathways to diagnosis did not vary significantly with place of residence overall, people living in rural areas had 51% lower odds (OR 0.49, 95% CI 0.25, 0.98) of being diagnosed after treatment for a benign thyroid disease (vs. patient detected) than people living in metropolitan areas.
Effects of pathways to diagnosis on incidence over time
The estimated potential thyroid cancer incidence rates in 2006, calculated by adding the potential additional cases diagnosed via the non-patient-detected pathways (an additional 63.9% of male patients and 59.3% of female patients) to the reported 1980 incidence rates, were 3.90 and 10.78 per 100,000 in men and women, respectively. These rates are below the reported rates in 2006 of 4.44 and 14.77 per 100,000 [25].
Discussion
We have described the pathways to diagnosis in a cohort of recently diagnosed thyroid cancer patients in NSW. We found that only 40% of cases presented to their doctor with a concern specifically related to thyroid cancer. Conversely, the majority (60%) of patients had their thyroid cancer discovered incidentally, without initially being aware of a neck mass or compressive symptom. The pathways to diagnosis differed significantly in men and women and by age and tumor size. Thyroid cancer in men was more likely to be detected by a doctor or diagnosed after imaging for another health problem than in women. Larger tumors were less often diagnosed after treatment for a benign thyroid disease. The incidental diagnosis of thyroid cancer after imaging for another health problem increased with age. People living in metropolitan areas tended to be more often diagnosed after incidental findings than people living in rural areas.
NSW is Australia’s most populous state, making up approximately a third of the Australian population, and is generally representative of the ethnic, social, and economic characteristics of the country’s population, so it is likely that these patterns are occurring across Australia. Also, although healthcare systems vary internationally, we have no reason to suspect that the approach to thyroid cancer diagnosis and treatment in NSW is markedly different from that of other developed countries. In addition, as a rise in thyroid cancer incidence has been recorded in many developed countries, we believe that our findings would be similar to those in other developed countries.
To our knowledge, this is the first study to describe pathways to the diagnosis of thyroid cancer in this way, so comparison with previous findings is not possible.
The study has some limitations. The classification of the pathways was complex for some patients. A benign thyroid disorder is often given as an initial diagnosis during workup for a thyroid nodule, or if an FNA is inconclusive, so patients may have reported benign diagnoses without actually following that pathway to diagnosis. To make a clear distinction between pathways, a time period of more than two months was required between the initial diagnosis of a benign thyroid disorder and the later cancer diagnosis for a patient to be classified as having a previous benign thyroid disease. Responses recorded in the first part of the questionnaire regarding benign thyroid disease history were also checked to confirm the pathway for these patients. However, it is possible that there are misclassified patients in this group who did not ever receive a definitive diagnosis of a benign thyroid disease.
The two-stage recruitment process through the NSW Central Cancer Registry, mandated by the ethics committees, resulted in a 44% participation rate. However, we believe that our sample is highly likely to be representative of all eligible patients diagnosed in NSW during the study period in terms of age, sex, cancer type, and disease spread. Although place of residence differed between participants and non-participants, we are satisfied that our results are still representative of all thyroid cancer patients in NSW, as weighting the study results to have the same distribution by place of residence as all eligible thyroid cancer patients resulted in differences of less than 1% in the proportions detected via each pathway.
Further support for this was found when the estimated age- and sex-specific proportions of patients diagnosed via the different pathways in our study were applied to the numbers of patients by age and sex diagnosed with thyroid cancer in NSW. This yielded the same overall proportions diagnosed via these pathways in the population as the crude proportions observed in our study, and confirms the representativeness of the study sample.
Another potential limitation of the study is the reliance on self-reported information from participants. However, there was a high level of agreement between the self-reported information and that extracted from medical records regarding procedures and circumstances leading to the thyroid cancer diagnosis for a sample of participants.
Increasing use of primary diagnostic tests for thyroid cancer has been reported [7, 26, 27], but without knowing the reasons for the instigation of these tests, it is difficult to know whether the increase in these tests is due to an increasing number of patients presenting with symptoms of thyroid cancer or whether the tests are being used for other reasons. The use of self-reported data is therefore a strength of this study, as it allowed us to capture the initial reasons for thyroid investigations that may not have been available from medical records.
The large proportion of cases diagnosed incidentally in our study (either as a result of surgery for a benign thyroid disease, discovered through diagnostic medical imaging for another health problem, or after a thyroid lump was first noticed by a doctor) indicates that changes in medical surveillance and diagnostic practices may have contributed to the observed increases in the incidence of thyroid cancer. Also, although pathways to diagnosis did not differ significantly by place of residence overall, our results show a trend toward people living in rural areas being less likely than those living in metropolitan areas to have their cancer diagnosed as an incidental result of unrelated medical surveillance or treatment. This suggests that accessibility to medical services (such as ultrasound, fine-needle biopsy, and specialist medical care) affects how thyroid cancer is diagnosed. It has been suggested that changes in thyroid cancer incidence reflect improvements in diagnostic technology or doctors’ surveillance [4, 28], and our results indicate that in NSW this is indeed possible, although it is unlikely to be the only contributing factor.
If increased detection was the sole reason for increasing thyroid cancer incidence, it would be expected that the increase would be in small tumors only, but several international studies have found that the rise in thyroid cancer incidence has occurred in tumors of all sizes [13, 14]. Our data suggest that larger tumors were most often initially patient detected and were significantly less likely to be detected after benign thyroid disease. This suggests that any increase in the incidence of large thyroid cancers is unlikely to be due to increased detection, and so supports those studies that have concluded that the observed increase in the incidence of larger tumors is evidence of a real increase in the disease.
The cross-sectional design of our study means that we cannot draw any conclusions about changes in the pathways to diagnosis and incidence of thyroid cancer over time. To begin to address this question, we used our results to model the potential influence of changing pathways to diagnosis on the reported incidence of thyroid cancer over time. We found that allowing for the extra cases that could have been diagnosed in 1980 via the non-patient-detected pathways, the potential thyroid cancer incidence rates in 2006 would have been 3.90 and 10.78 per 100,000 in men and women, respectively, rates that are still well below the observed 2006 rates of 4.44 and 14.77 per 100,000 [25]. This suggests that while diagnostic changes are likely to have contributed to the increase in the incidence of thyroid cancer, a real change in cancer incidence may also have occurred.
The potential cause of a real increase in thyroid cancer risk in NSW is unknown. There has recently been some evidence that the NSW population has marginal to mild iodine deficiency [29], but there is no indication that the general population of NSW would have experienced an unusual level of exposure to any of the known thyroid cancer risk factors sufficient to explain the rise in thyroid cancer incidence. Changes in pathology practices or criteria for thyroid cancer diagnosis may be another contributing factor in the rise in thyroid cancer incidence. There is, for example, evidence to suggest that increased sampling of thyroid specimens removed for benign indications has contributed to the more frequent diagnosis of papillary microcarcinoma [30].
Our finding that the majority of thyroid cancer patients are diagnosed without initially presenting with a thyroid mass or symptom specific to thyroid cancer suggests that the incidence of thyroid cancer is influenced by variations in diagnostic and medical practices. It is, however, unlikely that this explains all of the increase in thyroid cancer incidence observed in NSW over the past few decades, and thus, further research is required to investigate other potential causes.
References
Burgess JR (2002) Temporal trends for thyroid carcinoma in Australia: an increasing incidence of papillary thyroid carcinoma (1982–1997). Thyroid 12(2):141–149
Chen AY, Jemal A, Ward EM (2009) Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer 115(16):3801–3807
Colonna M, Grosclaude P, Remontet L et al (2002) Incidence of thyroid cancer in adults recorded by French cancer registries (1978–1997). Eur J Cancer 38(13):1762–1768
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295(18):2164–2167
Kilfoy BA, Zheng T, Holford TR et al (2009) International patterns and trends in thyroid cancer incidence, 1973–2002. Cancer Causes Control 20(5):525–531
Colonna M, Guizard AV, Schvartz C et al (2007) A time trend analysis of papillary and follicular cancers as a function of tumour size: a study of data from six cancer registries in France (1983–2000). Eur J Cancer 43(5):891–900
Leenhardt L, Grosclaude P, Cherie-Challine L (2004) Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 14(12):1056–1060
Verkooijen HM, Fioretta G, Pache J-C et al (2003) Diagnostic changes as a reason for the increase in papillary thyroid cancer incidence in Geneva, Switzerland. Cancer Causes Control 14(1):13–17
Kovacs GL, Gonda G, Vadasz G et al (2005) Epidemiology of thyroid microcarcinoma found in autopsy series conducted in areas of different iodine intake. Thyroid 15(2):152–157
Welch HG, Black WC (2010) Overdiagnosis in cancer. J Natl Cancer Inst 102(9):605–613
Kent WDT, Hall SF, Isotalo PA, Houlden RL, George RL, Groome PA (2007) Increased incidence of differentiated thyroid carcinoma and detection of subclinical disease. CMAJ 177(11):1357–1361
Scheiden R, Keipes M, Bock C, Dippel W, Kieffer N, Capesius C (2006) Thyroid cancer in Luxembourg: a national population-based data report (1983–1999). BMC Cancer 6:102
Yu GP, Li JC, Branovan D, McCormick S, Schantz SP (2010) Thyroid cancer incidence and survival in the National Cancer Institute Surveillance, Epidemiology, and End Results race/ethnicity groups. Thyroid 20:465–473
Zhu C, Zheng T, Kilfoy BA et al (2009) A birth cohort analysis of the incidence of papillary thyroid cancer in the United States, 1973–2004. Thyroid 19(10):1061–1066
Ward EM, Jemal A, Chen A (2010) Increasing incidence of thyroid cancer: is diagnostic scrutiny the sole explanation? Fut Oncol 6:185–188
Enewold L, Zhu K, Ron E et al (2009) Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiol Biomarkers Prev 18(3):784–791
Preston-Martin S, Franceschi S, Ron E, Negri E (2003) Thyroid cancer pooled analysis from 14 case–control studies: what have we learned? Cancer Causes Control 14:787–789
Zivaljevic V, Vlajinac H, Jankovic R et al (2003) Case–control study of female thyroid cancer—menstrual, reproductive and hormonal factors. Eur J Cancer Prev 12:63–66
Dal ML, Bosetti C, La VC, Franceschi S (2009) Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors. Cancer Causes Control 20:75–86
Stavrou E, Baker D, McElroy H, Bishop J (2008) Thyroid cancer in New South Wales. Cancer Institute NSW, Sydney
Tracey EA, Supramaniam R, Chen W (2003) Cancer in New South Wales: incidence and mortality 2001. The Cancer Council NSW, Sydney
Smith DP, Supramaniam R, King MT, Ward J, Berry M, Armstrong BK (2007) Age, health, and education determine supportive care needs of men younger than 70 years with prostate cancer. J Clin Oncol 20:2560–2566
Royston P, Ambler G, Sauerbrei W (1999) The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol 28:964–974
New South Wales Central Cancer Registry (1986) Cancer in New South Wales: incidence and mortality 1980. Department of Health NSW, Sydney
Tracey E, Alam N, Chen W, Bishop J (2008) Cancer in New South Wales: incidence and mortality 2006. Cancer Institute NSW, Sydney
Burgess JR, Tucker P (2006) Incidence trends for papillary thyroid carcinoma and their correlation with thyroid surgery and thyroid fine-needle aspirate cytology. Thyroid 16(1):47–53
Leennhardt L, Bernier MO, Boin-Pineau MH et al (2004) Advances in diagnostic practices affect thyroid cancer incidence in France. Eur J Endocrinol 150(2):133–139
Hall SF, Walker H, Siemens R, Schneeberg A (2009) Increasing detection and increasing incidence in thyroid cancer. World J Surg 33(12):2567–2571
Li M, Eastman CJ, Waite KV et al (2006) Are Australian children iodine deficient? Results of the Australian National Iodine Nutrition Study. Med J Aust 184:165–169
Grodski S, Brown T, Sidhu S et al (2008) Increasing incidence of thyroid cancer is due to increased pathologic detection. Surgery 144(6):1038–1043
Acknowledgments
We are very grateful to the NSW Central Cancer Registry at the Cancer Institute NSW for all their help with recruitment, data extraction from the pathology forms and for providing data for participants and non-participants. We would like to thank Leighna Carmichael and Sam Egger (Cancer Council NSW) for their assistance with statistical analyses. Cancer Council NSW funded the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kahn, C., Simonella, L., Sywak, M. et al. Pathways to the diagnosis of thyroid cancer in New South Wales: a population-based cross-sectional study. Cancer Causes Control 23, 35–44 (2012). https://doi.org/10.1007/s10552-011-9852-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-011-9852-2