Abstract
Objectives
The present review summarizes epidemiological evidence on risk factors for thyroid cancer (TC), in particular, nutritional factors.
Methods
Searches of articles on the issue were conducted using MEDLINE.
Results
Exposure to ionizing radiation, particularly during childhood, is the best-established risk factor for TC. There is also a strong association with history of benign nodules/adenoma or goiter. Iodine deficiency may induce an increasing incidence of benign thyroid conditions, but very high iodine intake also affects thyroid function and, possibly, TC risk. Among dietary factors, fish—the major natural source of iodine in human diet—is not consistently related to TC risk. High intake of cruciferous vegetables shows a weak inverse association with TC. Among other food groups, vegetables other than cruciferous are the only food group showing a favorable effect on TC, with an approximate 20% reduction in risk for subjects with the highest consumption. No effect on TC risk of alcohol, coffee, or other food-groups/nutrients emerged. Height and weight at diagnosis show a moderate positive association with TC risk.
Conclusion
At present, the only recognized measures for reducing TC risk is to avoid ionizing radiation and iodine deficiency, particularly in childhood and young women, and to increase vegetable consumption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer (TC) represents about 1% of all malignancies diagnosed worldwide, with approximately 140,000 cases and 35,000 deaths occurring in 2002 [1]. Most TC are indolent malignancies with estimated five-year relative survival of approximately 85% in Europe [2] and 95% in United States [3]. The cumulative risk of developing TC before age 64 has been estimated as 0.2% in women and 0.1% in men.
In humans, TC arises mostly from the epithelial elements of the gland, generally from follicular cells [4]. The traditional separation of TC into the two major groups of differentiated (including papillary, follicular, and medullary) and undifferentiated (anaplastic) carcinoma, based on morphology and clinical features, is strongly supported by advances in molecular studies [4]. Papillary carcinomas represent approximately two-thirds of TC in men and in women. The corresponding figures are 10–20% for follicular carcinomas, 5–10% for medullary carcinomas, and less than 5% for anaplastic carcinomas, while other subtypes account for less than 1% of all TCs [4]. The distribution of histological subtypes of TC, as reported by epidemiological surveillance in several countries, is shown in Table 1 [5].
There is a 10-fold difference in incidence among different parts of the world in women, but only a 3-fold difference in men [5]. Incidence rates are more than 2-fold higher in developed countries as compared to developing countries both in men (2.2/100,000 and 1.0/100,000, respectively) and in women (5.5/100,000 and 2.6/100,000, respectively) [1]. Worldwide estimates for mortality rates are 0.8/100,000 women and 0.4/100,000 men [1].
An increasing incidence of TC has been consistently reported worldwide over the last 30 years [6–8] notably in the United States [9]. Given the lack of increase in TC mortality, the current rise in incidence seems predominantly due to improved diagnostic activity and increased ability to detect small (<2 cm) papillary carcinomas with an excellent prognosis [7, 9].
Iodine intake is essential for thyroid functioning, and ecological studies suggested that TC is more frequent in areas with iodine deficiency and, possibly, iodine excess [10]. However, analytical studies showed a less clear association, since iodine levels in the same type of food vary substantially by production area, and serum markers of iodine intake are poorly defined.
The aim of the present study is to review epidemiological evidence on major risk factors for TC, with particular focus on nutritional factors.
Materials and methods
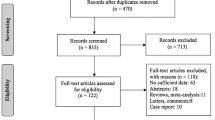
A search strategy was conceived to be run on the PubMed interface of the MEDLINE database to identify all relevant papers on the issue published up to July 2007. The following search terms were included in the strategy: Thyroid cancer AND (diet*[tiab] OR nutrient*[tiab] OR food and beverages[MeSH Terms] OR food*[tiab] OR vegetable*[tiab] OR fruit*[tiab] OR meat[tiab] OR fish[tiab] OR fat*[tiab] OR bread[tiab] OR shellfish[tiab] OR seafood[tiab] OR sugar[tiab] OR alcohol[tiab] OR dietary carbohydrates[MeSH Terms] OR salt[tiab] OR starch[tiab] carbohydrate*[tiab] OR vitamins[MeSH Terms] OR physical activity*[tiab] OR energy intake[tiab] OR anthropometry[tiab] OR height[tiab] OR body mass[tiab] OR BMI[tiab] OR obesity[tiab] OR obese[tiab] OR overweight[tiab] OR waist hip ratio*[tiab]).
The results from 42 original papers contributed to the present review (in some cases more than one paper was published for each study), including: (1) a comprehensive pooled-analysis of individual data from the 14 case–control studies carried out on TC before 1998 and including over 2,725 TC cases (2,247 women and 478 men) and 4,776 controls (3,699 women and 1,077 men) [11, 12]; (2) six case–control studies [13–18] and three prospective studies published subsequently [19–21].
Finally, 17 papers not selected by the search strategy, mainly discussing biological mechanisms, were included in the present review, as well as results from several reviews, related to TC, from the International Agency for Research on Cancer (IARC) and other institutions [1, 4, 5, 22–30].
Main characteristics of epidemiological studies published on TC (including type of design, subjects age, sex, and histologic distribution) are shown in Table 2.
Non-dietary risk factors for TC
Ionizing radiation
The best-established cause of TC is exposure to ionizing radiation, particularly during infancy or early childhood. A pooled-analysis on this issue, based on five cohorts and two case–control studies with 58,000 exposed individuals, 61,000 unexposed, 700 TCs, and 3 million person-years, found a significant dose-risk for exposure during childhood [31]. Even at a dose of 0.1 Gray, the dose–risk relationship was consistent with linearity and appeared to level off at doses higher than 10 Gray. In the pooled-analysis, women had an approximately 2-fold higher risk (measured as excess relative risk per Gray of exposure) than men. A latent period of 5–9 years emerged with highest risk 15–29 years after exposure, which continued to be elevated 40 or more years after exposure. The relative risk (RR) also decreased significantly with increasing age at exposure, with still some excess risk after age 20 years.
Further confirmation emerged after the Chernobyl nuclear power plant accident in April 1986, where a large increase in the incidence of childhood TC was reported in contaminated areas [32]. Although almost all studies were cross-sectional, there was strong evidence that TC in children rose as a consequence of the Chernobyl accident [32].
Cardis et al. [33] carried out a population-based case–control study of TC in Belarus and in the Russian Federation to evaluate the risk of TC after exposure to radioactive iodine in childhood and to investigate environmental and host factors that could modify this risk. Cases were 276 TCs and controls were 1,300 matched subjects, all below age 15 years at the time of the accident. For a dose of 1 Gray, an approximately 7-fold excess risk for TC was estimated and a linear dose–risk relationship was observed at least up to 2 Gray. For higher doses, the number of subjects exposed was low and did not allow reliable estimates of dose–response relationship. The study also showed that the risk of radiation-related TC was 3-fold higher in iodine-deficient areas than elsewhere, and that administration of potassium iodide as a dietary supplement reduced the risk of radiation-related TC by a factor of 3.
Among adults exposed to Chernobyl accident, as in previous studies on adult populations [31], the evidence of an association between ionizing radiation exposure and TC is inconsistent, suggesting that the adult thyroid is less radiosensitive than the child one [32].
In brief, susceptibility to radiation-induced TC is strongly inversely related to age at exposure, and directly related to background iodine deficiency, and, to a lesser extent, to gender (being higher in women) [31, 32].
Genetic susceptibility
Familial susceptibility for medullary carcinoma has been known for a long time, and genetic factors are reported to be responsible for 20–25% of this type of TC [4]. In particular, germ-line mutations in the RET gene are responsible for the hereditary tumor syndrome (i.e., multiple endocrine neoplasia type 2, MEN 2) which includes three subgroups, MEN 2A, MEN 2B, and familial medullary thyroid carcinoma, depending on the tissue involved [34]. The common disease for all three subtypes of MEN 2 is medullary TC (100%) and phaeochromocytoma (50%).
For the commonest types of TC (i.e., non-medullary forms) the association with genetic susceptibility is weaker, but also present. In a study including all TCs diagnosed between 1958 and 2002 in Sweden, the familiar RRs for papillary carcinoma were 3 and 6 when TCs were diagnosed in a parent or a sibling, respectively [35]. TC risk was approximately 5-fold higher in first-degree relatives of TC patients compared to the general population (i.e., one of the most elevated RR among all cancer sites in the Swedish study).
Some genetic mutations have been described as strongly associated with non-medullary TC risk [36, 37]. BRAF mutation is the most common genetic alteration in TC occurring in about half of the sporadic papillary TCs in adults. This mutation is mutually exclusive with other common genetic alterations, such as RET mutation. RET mutations are present in about one-third of cases and they are particularly common (50–90%) in pediatric papillary carcinomas linked to radiation exposure. The link between certain RET alterations and ionizing radiation is strongly supported by the high incidence of RET rearrangements in childhood papillary carcinomas following the Chernobyl accident [37].
BRAF mutation has not been associated with radiation exposure and is not found in benign thyroid tumors. Etiological correlates of BRAF mutation are presently unknown.
Inactivation of the p53 tumor-suppressor gene is rare in patients with differentiated thyroid carcinomas, but common in those with undifferentiated (anaplastic) thyroid carcinomas [4, 38].
Benign thyroid conditions
Goiter and benign nodules/adenomas have been consistently shown to be major risk factors for TC (Table 3). The pooled-analysis of all case–control studies conducted before 1998 reported a RR of 6 in women who had a history of goiter and of 30 in those with a history of benign nodules/adenomas [39]. The RR associated with goiter and nodules was even stronger in men. Goiter and nodules have a higher prevalence in women and the main risk factor for these conditions is iodine deficiency [40]. Other factors associated with benign thyroid conditions are high levels of goitrogens in foods and, possibly, smoking [41, 42]. Prior hyperthyroidism and hypothyroidism were not significantly associated with TC risk after adjustment for history of goiter [39].
All subsequent studies (Table 3) conducted on the topic in different countries provided consistent findings [14, 16, 17, 19, 43].
Hormonal and reproductive factors
Since the excess risk for TC is 3-fold in women compared to men, and it is largest during women’s reproductive years (Table 1), events related to reproductive and menstrual history have been suggested to be of relevance in TC etiology. However, the thyroid gland is not obviously related to female sex hormones in the way breast, ovary, and uterus are, and epidemiological studies have provided inconsistent results [25].
Menarche, pregnancy, and oral contraceptive use are associated with enlargement of the thyroid gland and with increases in serum levels of total T4 and T3 caused partly by a rise in the concentration of thyroxine-binding globulin (TBG) [44]. Increased levels of female hormones may cause an elevation of thyroid-stimulating hormone (TSH) levels, leading in turn to thyroid hyperplasia and possibly cancer. Experimentally, increased TSH secretion induces thyroid tumors in rodents [45].
The pooled-analysis of case–control studies published before 1998 showed that the associations between TC and menstrual or reproductive factors were generally weak and not statistically significant (Table 4), although they appeared to be stronger among women diagnosed with TC at a young age [46]. Number of births, spontaneous or induced abortions, and history of infertility were not associated with TC risk. Age at first birth was, however, weakly positively associated with TC (RR = 1.1, 95% CI: 1.0–1.3 for five-year delay), as was artificial menopause (RR = 1.8; 95% CI: 1.4–2.4).
In the same pooled-analysis, there was a modest increase in the risk of TC for ever use of oral contraceptives (RR = 1.2, 95% CI: 1.0–1.4), which declined with increasing time since stopping [47]. A small increase in risk was also seen among women who took drugs for fertility treatment (RR = 1.6, 95% CI: 0.9–2.9) or lactation suppression (RR = 1.5, 95% CI: 1.1–2.1). No increased risk was seen for hormone replacement therapy use (RR = 0.8, 95% CI: 0.6–1.1).
Later studies confirmed that hormonal and reproductive factors were weakly associated with TC (Table 4) [15, 17, 18, 20, 48, 49].
Dietary risk factors for TC
The wide geographical variation of TC incidence (Table 1) suggests a relevant impact of one or more environmental exposures, and nutrition-related factors are candidates for such exposures. Agents causing thyroid enlargement are known as goitrogens, and a number of naturally occurring goitrogens in foods have been described. Moreover, several chemicals and pollutants (e.g., thiocyanates, lithium, phthalate ester derivatives) occasionally present in foodstuff have been suspected to play a role on thyroid diseases [50].
Only a relatively small number of epidemiological studies have provided information on the potential role of dietary factors in TC etiology, and only a few were specifically designed to investigate dietary correlates of TC. Moreover, available studies included a limited number of subjects, and had thus limited statistical power to detect probably weak associations as dietary ones. The great variability in the number of food items investigated in available studies and dietary patterns in different parts of the world limit the possibility of comparing or combining data from different studies.
Iodine intake
Iodine deficiency influences thyroid function directly, as well as indirectly, through a reduction in the level of thyroid hormones and a consequent rise in TSH secretion. Chronic iodine deficiency is firmly established as a risk factor for goiter and follicular TC [10, 51–53], while some ecological studies suggested that iodine supplementation programs could increase the incidence of papillary TC by inducing iodine excess [54, 55]. Increased surveillance and improvement in the quality of diagnostic tools are, however, likely responsible for the increase. Supplementation effects are likely to be confounded by diagnostic improvements and therefore, no biological explanation is probably needed. [ 7, 55].
In 1990, iodine deficiency still affected almost one-third of the world population and was the most important single cause of preventable brain damage and mental retardation [54]. In 1999, programs of iodine supplementation by iodization of salt or, less commonly, milk were implemented by the governments of 75% of the affected countries, and 68% of the affected populations had access to iodized salt [54]. The prevalence of iodine deficiency dramatically decreased in most countries, including many developing countries, and adverse effects were rare. The main adverse effect was iodine-induced hyperthyroidism in elderly people with nodular goiters. The incidence of hyperthyroidism was usually low and reverted spontaneously to the background rate after 1–10 years of iodine supplementation.
Iodine-induced hyperthyroidism and other adverse effects can be almost entirely avoided by adequate monitoring of iodine supplementation which should also confirm adequate iodine intake at a population level. Thus, available evidence shows that the benefits of correcting iodine deficiency outweigh by far any possible risk of iodine supplementation [54, 55].
Only two case–control studies could quantify total iodine intake through a comprehensive food-frequency questionnaire and an ad hoc nutrient database, and study the relation between iodine intake and TC risk [14, 56]. A study conducted in Hawaii (a high iodine intake area) [56], including 191 TC cases, showed a statistically non-significant increased RR (1.6) in women with the highest dietary iodine consumption, and only a modest increase (1.3) in men. Conversely, a study conducted in California [14], including 608 women with papillary TC, showed that high dietary intakes of iodine were associated with a reduced (halved) risk of papillary TC in women without any of the established risk factors. However, when toenail clipping was used as a biomarker of iodine exposure, no association with TC risk was observed. Nonetheless, this biomarker should be taken with caution, since correlations between dietary iodine and nail levels of iodine were low (Pearson correlation; r = 0.07), probably due to a substantial non-dietary (i.e., supplements) iodine intake in this population. The usefulness of other biomarkers of iodine intake for assessing the risk of TC is still uncertain [42].
Fish consumption
The association between fish and TC was intensively examined [27] since fish, especially salt-water fish and shellfish, are a major natural source of iodine in the diet. In some coastal areas, a diet rich in fish and other seafood was associated with an increased incidence of TC [53, 56, 57]. On the other hand, it is conceivable that fish may differentially affect the risk of TC and its various histological types with a protective effect only in endemic goiter areas with suboptimal iodine intake [53].
A pooled-analysis of all case–control studies of TC conducted before 1998 reconsidered this issue [58]. The variables considered in that pooled-analysis were salt-water fish, shellfish, and overall fish consumptions. Since consumption of fresh-water fish and other fish products was generally low and collected in few studies, all fish intake was assessed. Dietary questionnaires of the studies included were of very different lengths (ranging from 4 to 150 items). The combined analysis indicated that relatively elevated fish consumption (≥3 times per week, compared to <1 per week) does not appreciably increase TC risk (RR = 0.9, 95% CI: 0.7–1.1). Interestingly, some differences emerged between studies conducted in endemic goiter areas compared to high-iodine-intake areas with significantly reduced RR for high levels of fish consumption in endemic goiter areas (0.7, 95% CI: 0.5–0.9), but no association in iodine-rich ones (RR = 1.1, 95% CI: 0.9–1.5). No significant heterogeneity in the overall results was found between papillary and follicular TC or when studies were grouped according to the quality of their questionnaires. When analysis considered specific fish types, the pattern of risk for salt-water fish consumption was not substantially different from that observed for total fish consumption. A direct association between high shellfish consumption and TC risk emerged in a few studies, although the RR estimates were not significant [58].
Two subsequent studies showed results on the association between fish and TC (Table 5). One study, conducted in Kuwait (a high TC incidence area) and including 313 TC cases, showed a protective effect for high fish consumption (RR = 0.60, 95% CI: 0.3–1.0) [43]. Conversely, in the same study, there was no association with shellfish, while a significant threefold increased RR (95% CI: 1.6–5.3) of TC for high consumption of processed, canned, or frozen fish products was reported. A large multiethnic investigation conducted in California on 608 TC cases [14] showed no association between consumption of fish/shellfish and TC risk, with the exception of fish sauce/dried or salted fish, seasonings commonly used in Asian cuisine, which were found to be directly related to TC risk (RR = 2.3; 95% CI: 1.3–4.0). In the same study, cooked seaweed, a food rich in iodine, was inversely associated with TC risk (RR = 0.6; 95% CI: 0.4–0.8).
Vegetable consumption
Besides iodine itself and fish, some other aspects of diet have been related to TC risk including, in particular, consumption of cruciferous vegetables which contain thioglucosides that may be degraded to form goitrogens and induce thyroid tumors in rats [59]. Although historical reports of adverse effect of very high consumption of cabbages and other cruciferous vegetables exist, modern epidemiological studies exploring the association between cruciferous vegetables and TC gave only limited support to this hypothesis [27].
The association between cruciferous or other vegetables and TC risk was re-evaluated using data from the pooled-analysis of all case–control studies on TC conducted before 1998 [60]. In that combined analysis, cruciferous vegetables (including cabbages, broccoli, Brussels sprouts, cauliflowers, etc.) and vegetables other than cruciferous were considered and analyzed separately (Table 5). High intakes of cruciferous vegetables were inversely, though not significantly, associated with TC risk (RR = 0.9, 95% CI: 0.8–1.1). The results were similar in studies conducted in iodine-rich and in endemic goiter areas. The pattern of risk was also consistent when papillary and follicular carcinomas or women and men were assessed separately.
An inverse association between vegetables other than cruciferous and TC risk was observed in most of the studies, with an overall significantly reduced RR of 0.8 (95% CI: 0.7–1.0) for the highest level of consumption as compared to the lowest one.
Besides goitrogenic substances, cruciferous vegetables contain a variety of constituents (such as flavonoids, phenols, isothiocyanates) known to inhibit carcinogenesis in animal models [61, 62]. Moreover, many of these vegetables are also sources of carotenoids, such as β-carotene, and other antioxidant substances, which appear to be protective against certain, but not all other, forms of cancer [22, 23]. Thus, if any unfavorable effect exists for goitrogenous vegetables, this seems to be outweighed by the protective effects of other compounds in this class of vegetables.
Systemic mechanisms through which vegetables can contribute to cancer prevention have been reviewed [24]. They included inhibition of endogenous carcinogen formation, inhibition of damage from macromolecules, and modulation of immune functions. How these effects could act specifically on thyroid carcinogenesis, however, remains unclear.
Since some flavonoids—a group of chemicals naturally produced by plants with structural similarities to estrogens—showed potent antiproliferative in vitro activity against thyroid carcinoma cell lines [61], the relationship between TC risk and dietary phytoestrogens has been suggested. A multiethnic population-based case–control study conducted in the San Francisco Bay Area [63], including 608 TC cases and 558 controls, found a reduced risk of TC for consumption of soy-based foods (mainly tofu) and sprouts; the consumption of “western” foods with added soy flour or soy protein (such as bread), however, did not affect TC risk. Of the seven specific phytoestrogenic compounds examined, only two isoflavones (i.e., daidzein and genistein) and a lignan (i.e., secoisolariciresinol) showed a borderline reduced risk for the highest vs the lowest quintile of intake. Findings were similar for white and Asian women and for pre- and postmenopausal women. Since only one epidemiological study examined the topic, additional research is needed to confirm these results.
Other food and nutrient consumption
Other foods, which can be rich in iodine depending upon local characteristics and manufacturing practices, include bread products (iodine may be added as a dough conditioner), dairy products (iodophors may be used in the dairy industry as a disinfectant), and salt. No consistent association with TC risk emerged in the studies where these foods were evaluated [14, 43, 56, 64–66].
Four case–control studies reported the relationship between fruit consumption and TC. Three of them [43, 65, 66] showed no association, while a Greek study [67] reported a significant protective effect for fresh fruit.
In several studies, including a pooled-analysis of 10 case–control studies [13, 20, 68], no association of TC risk with alcohol intake emerged. The same pooled-analysis [68] showed no association between TC risk and consumption of coffee or tea.
Published results on single nutrients, foods, or vitamins are scant and inconsistent [43, 64, 69–74] and no conclusion could be drawn on the association with TC [22, 23].
Body mass and physical activity
Thyroid hormones are crucial to the development of several body tissues, and anthropometrical measures (i.e., height, weight, body fat) are affected by thyroid disorders [25]. Vice versa, body size might affect the iodine requirement and, hence, indirectly TC risk. A relation between anthropometric factors and TC risk has therefore been suggested [28].
A pooled-analysis of all case–control studies on the topic was conducted before 1998, and showed a weak positive association with height in women, with an overall RR of 1.2 (95% CI: 1.0–1.4) for those in the highest category of height as compared to the lowest one [75]. In men, the corresponding figure was 1.5 (95% CI: 1.1–2.1). The RR of TC increased linearly according to height in both genders (RR = 1.1 for a 5-cm increase of height in both genders combined) (Table 6). A similar risk pattern emerged for papillary and follicular TC [75], while medullary subtype showed a significant RR increase (2.6, 95% CI: 1.2–5.4) in subjects in the highest category of height [76].
With reference to weight at diagnosis the RR was 1.2 (95% CI: 1.0–1.4) in women in the highest category vs the lowest one, with a significant trend in risk. No association was, however, observed in men [75].
In women, self-reported body mass index (BMI) at diagnosis was also directly related to TC risk, with a RR of 1.2 for the highest category and of 1.1 for an increase of 5 BMI units in continuous analysis (Table 6). No consistent association was observed in men. BMI at age 20 years and weight gain from the same age was not associated with TC risk in either women or men.
The association with weight or BMI was of similar magnitude in younger women and in postmenopausal ones, but significant heterogeneity in RR estimates was observed across studies for height, weight, and BMI.
Two other reports explored the influence of anthropomeric measures after the publication of the pooled-analysis (Table 6). A cohort study conducted in California including 196 TC cases, found no association between BMI, height, and weight gain and TC risk [19], while a Norwegian Record Linkage Study including 3,046 TC cases, reported an increased risk of TC (particularly well differentiated TC) with increasing BMI and height in both genders [21].
The association with height in both genders may indicate a potential influence of some growth factors or hormones during childhood/adolescence, but the potential role of growth factors in thyroid carcinogenesis is still poorly defined [77, 78].
Physical activity has also been hypothesized to influence cancer risk through a variety of mechanisms including hormonal, metabolic, and immunologic effects [28]. However, only very few studies analyzed the association with TC. In Hawaii, Kolonel et al. [56] collected information on occupational physical activity and reported no association with TC risk. Three other studies compared sedentary vs heavy occupational physical activity providing mixed results; however, these studies were designed to address other study hypotheses [16, 18, 79].
The link between TC and recreational physical activity was explored in 410 California women with papillary TC [80]. The RR of TC was slightly reduced (RR = 0.8; 95% CI: 0.6–1.0) among women who reported a regular recreational exercise during the two years before diagnosis as compared to women who did not report exercise during the same period. However, no clear trends emerged according to duration of exercise or weekly energy expenditure.
Methodological considerations on epidemiologic studies of nutrition and (thyroid) cancer
Many methodological difficulties may limit estimation of nutritional effects on (thyroid) cancer risk [81, 82]. In general, diets are multidimensional exposures and cannot be measured with complete accuracy in free-living populations. Moreover, foods and drinks that people consume every day contain thousands of constituents, some well known, others unknown and unmeasured. The relationships between food, nutrition, physical activity, and health and disease are complex and difficult to estimate. People’s dietary intake varies from day to day and over the course of their lives. Diet histories are usually collected by means of food-frequency questionnaires, which collect information typically over the previous year. All dietary assessment methods that rely on self-reporting are subject to measurement error. Further errors are introduced by the conversion of food data into nutrient data, using tables on chemical composition of foods, which give average nutrient contents for defined foods. All the aforementioned issues are especially severe in respect to the assessment of iodine intake. Iodine contents of foods and drinks vary enormously according to local levels of iodine in soil and water and, therefore, no generalizable food composition tables are available for iodine. Long-distance food trading has generally improved iodine status of formerly iodine-deficient populations, but it has further complicated any estimate of iodine intake. Finally, the intake of iodized salt and iodized dairy products at an individual and population level is hard to assess and can blur the influence of dietary habits on iodine status.
In addition, data on dietary correlates of thyroid cancer are limited and dietary information collected in the original studies differed substantially with regard to the frequency of intake of the foods, the level of detail of the questionnaires, the food queries, and the measurement of frequency of intake. These differences prevented pooled-analyses from defining common cut-points for food consumption across all studies [58, 60]. Also important, nearly all studies included in the present review were carried out in high-income countries and their findings may have limited application in developing countries where dietary deficiencies, notably very low iodine intake, exist [13–18, 58, 60, 81].
Conclusions
Recent findings are reassuring with respect to the concern that iodine supplementation may increase the risk of papillary TC, the less aggressive TC subtype, while they confirm its benefits [7]. Iodine deficiency is, in fact, associated with an increased TC incidence, largely via benign thyroid conditions such as goiter and nodules, which are, in turn, strongly associated with TC. Clinical or subclinical iodine deficiency is still present in some areas in Europe and, to a greater extent, Central Asia and Africa where often statistics on TC are not available.
The epidemiological studies exploring dietary correlates of TC showed that the impact of different levels of fish consumption on TC seemed negligible. Only for high-iodine-intake populations, a direct association emerged with salt-water fish.
The hypothesis of a possible carcinogenic effect of cruciferous vegetables is not supported by epidemiological studies in well-nourished populations, while a moderate favorable effect of high intake of vegetables other than cruciferous was the only dietary factor inversely associated with TC risk in a large pooled-analysis.
Height and weight at TC diagnosis appear to be directly associated with a small increase in TC risk, but the heterogeneity across studies complicates the picture.
BMI seemed related to TC only in women. Conversely, height was more strongly related to risk of TC in men than women and in the medullary histological subtype. Findings on anthropometrical measures point to the possibility of some link between diet in childhood/adolescence and TC risk, but this hypothesis needs to be confirmed.
A limitation of current knowledge on the etiology of TC is that nearly all available epidemiological studies have a case–control design and are thus prone to recall bias in relation to dietary measurements. A lack of new promising hypotheses, which can be tested in epidemiological studies, is also a serious obstacle to planning new investigations despite the concerning increases in TC incidence in United States and elsewhere [1].
In general, improvements are needed in the design of future studies on TC. In particular, there is a need to: (a) develop methods to assess the impact of diet over longer periods of life in order to capture important relationship between cancer risk in childhood and in early adulthood; (b) incorporate the use of objective markers of diet, metabolism, and thyroid function from serum and other types of biological samples (e.g., nails) [81, 82]; (c) develop studies on the interaction between environmental exposures (including diet) and genetic susceptibility; (d) systematically collect information on diagnostic modalities and clinical and histological characteristics of TC, in order to assess separately the influence of potential risk factors in more or less aggressive cancers.
In conclusion, at present, the only recognized chance of reducing TC risk is to avoid ionizing radiation and iodine deficiency, particularly in childhood. Adopting a diet rich in vegetables may play a role in TC but the association identified warrants more investigation into food, nutrition, and TC [81].
References
Ferlay J, Bray F, Pisani P, Parkin DM (2004) GLOBOCAN 2002. Cancer incidence, mortality and prevalence worldwide. IARC CancerBase No.5, version 2.0. IARC Press, Lyon, France
Verdecchia A, Francisci S, Brenner H et al (2007) Recent cancer survival in Europe: a 2000–02 period analysis of EUROCARE-4 data. Lancet Oncol 8:784–796. doi:10.1016/S1470-2045(07)70246-2
Kosary CL (2007) Cancer of the thyroid. In: Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner M-J (eds) SEER survival monograph: cancer survival among adults: U.S. SEER program, 1988–2001, patient and tumor characteristics. National Cancer Institute, SEER Program, Bethesda, MD. NIH Pub. No. 07-6215. Available at: http://seer.cancer.gov/publications/survival/surv_thyroid.pdf
De Lellis RA, Lloyd RV, Heitz PU, Eng C (2004) World Health Organization Classification of tumours. Pathology and genetics of tumours of endocrine organs. IARC Press, Lyon, France
Curado MP, Edwards B, Shin HR et al (eds) (2007) Cancer incidence in five continents, vol IX. IARC Sci Publ No. 160. IARC, Lyon
Liu S, Semenciw R, Ugnat AM, Mao Y (2001) Increasing thyroid cancer incidence in Canada, 1970–1996: time trends and age-period-cohort effects. Br J Cancer 85:1335–1339. doi:10.1054/bjoc.2001.2061
Verkooijen HN, Fioretta G, Pache JC et al (2003) Diagnostic changes as a reason for the increase in papillary thyroid cancer incidence in Geneva, Switzerland. Cancer Causes Control 14:13–17. doi:10.1023/A:1022593923603
Reynolds RM, Weir J, Stockton DL, Brewster DH, Sandeep TC, Strachan MWJ (2005) Changing trends in incidence and mortality of thyroid cancer in Scotland. Clin Endocrinol 62:156–162. doi:10.1111/j.1365-2265.2004.02187.x
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167. doi:10.1001/jama.295.18.2164
Feldt-Rasmussen U (2001) Iodine and cancer. Thyroid 11:483–486. doi:10.1089/105072501300176435
Negri E, Ron E, Franceschi S et al (1999) A pooled analysis of case–control studies of thyroid cancer. I. Methods. Cancer Causes Control 10:131–142. doi:10.1023/A:1008851613024
Preston-Martin S, Franceschi S, Ron E, Negri E (2003) Thyroid cancer pooled analysis from 14 case–control studies: what have we learned? Cancer Causes Control 14:787–789. doi:10.1023/A:1026312203045
Rossing MA, Cushing KL, Voigt LF, Wicklund KG, Daling JR (2000) Risk of papillary thyroid cancer in women in relation to smoking and alcohol consumption. Epidemiology 11:49–54. doi:10.1097/00001648-200001000-00011
Horn-Ross PL, Morris SJ, Lee MM et al (2001) Iodine and thyroid cancer risk among women in a multiethnic population: the Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev 10:979–985
Memon A, Darif M, Al-Saleh K, Suresh A (2002) Epidemiology of reproductive and hormonal factors in thyroid cancer: evidence from a case–control study in the Middle East. Int J Cancer 97:82–89. doi:10.1002/ijc.1573
Zivaljevic V, Vlajinac H, Jankovic R, Marinkovic J, Diklic A, Paunovic I (2006) Case–control study of anaplastic thyroid cancer. Tumori 90:9–12. doi:10.1159/000091608
Troung T, Orsi L, Dubourdieu D, Rougier Y, Hémon D, Guénel P (2005) Role of goiter and of menstrual and reproductive factors in thyroid cancer: a population-based case–control study in New Caledonia (South Pacific), a very high incidence area. Am J Epidemiol 161:1056–1065. doi:10.1093/aje/kwi136
Wong EY, Ray R, Gao DL et al (2006) Reproductive history, occupational exposures, and thyroid cancer risk among women textile workers in Shanghai, China. Int Arch Environ Health 79:251–258. doi:10.1007/s00420-005-0036-9
Iribarren C, Haselkorn T, Tekawa IS, Friedman GD (2001) Cohort study of thyroid cancer in a San Francisco Bay Area population. Int J Cancer 93:745–750. doi:10.1002/ijc.1377
Navarro Silvera SA, Miller AB, Rohan TE (2005) Risk factors for thyroid cancer: a prospective cohort study. Int J Cancer 116:433–438. doi:10.1002/ijc.21079
Engeland A, Tretli S, Akslen LA, Bjørge T (2006) Body size and thyroid cancer in two million Norwegian men and women. Br J Cancer 95:366–370. doi:10.1038/sj.bjc.6603249
IARC Working Group on the Evaluation of Cancer-preventive Agents (1998) IARC handbooks of cancer prevention. Vitamin A. IARC WHO, Lyon, France
IARC Working Group on the Evaluation of Cancer-preventive Agents (1998) IARC handbooks of cancer prevention. Carotenoids. IARC WHO, Lyon, France
IARC Working Group on the Evaluation of Cancer-preventive Strategies (2003) IARC handbooks of cancer prevention. Fruit and vegetables. IARC Press, Lyon, France
Franceschi S, Dal Maso L (1999) Hormonal imbalances and thyroid cancers in humans. In: Capen CC, Dybing E, Rice JM, Wilbourn JD (eds) Species differences in thyroid, kidney and urinary bladder carcinogenesis. IARC, Lyon, France, pp 33–43
Kane AB, Boffetta P, Saracci R, Wilbourn JD (1996) Mechanisms of fibre carcinogenesis. IARC, Lyon, France
Ron E (1996) Epidemiology of thyroid cancer. In: Schottenfeld S, Fraumeni JR Jr (eds) Cancer epidemiology and prevention. Oxford University Press, Oxford, pp 1000–1021
IARC Working Group on the Evaluation of Cancer-preventive Strategies (2002) IARC handbooks of cancer prevention. Weight control and physical activity. IARC Press, Lyon, France
de Benoist B, Andersson M, Egli I, Takkouche B, Allen H (2004) Iodine status worldwide. WHO global database on iodine deficiency. World Health Organization, Geneva
Willett WC (1998) Nutritional epidemiology. In: Rothman KJ, Greenland S (eds) Modern epidemiology, 2nd edn. Lippincott-Raven Publishers, Philadelphia, pp 623–642
Ron E, Lubin JH, Shore RE et al (1995) Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 141:259–277. doi:10.2307/3579003
Moysich KB, Menezes RJ, Michalek AM (2002) Chernobyl-related ionising radiation exposure and cancer risk: an epidemiological review. Lancet Oncol 3:269–279. doi:10.1016/S1470-2045(02)00727-1
Cardis E, Kesminiene A, Ivanov V et al (2005) Risk of thyroid cancer after exposure to 131I in childhood. J Natl Cancer Inst 97:724–732
Liska J, Altanerova V, Galbavy S, Stvrtina S, Brtko J (2005) Thyroid tumors: histological classification and genetic factors involved in the development of thyroid cancer. Endocr Regul 39:73–83
Hemminki K, Eng C, Chen B (2005) Familial risks for nonmedullary thyroid cancer. Clin Endocrinol Metab 90:5747–5753. doi:10.1210/jc.2005-0935
Xing M (2005) BRAF mutation in thyroid cancer. Endocr Relat Cancer 12:245–262. doi:10.1677/erc.1.0978
Kondo T, Ezzat S, Asa SL (2006) Pathogenic mechanisms in thyroid follicular-cell neoplasia. Nature Rev Cancer 6:292–306. doi:10.1038/nrc1836
Schlumberger MJ (1998) Papillary and follicular thyroid carcinoma. N Engl J Med 338:297–306. doi:10.1056/NEJM199801293380506
Franceschi S, Preston-Martin S, Dal Maso L et al (1999) A pooled analysis of case–control studies of thyroid cancer. IV. Benign thyroid diseases. Cancer Causes Control 10:583–595. doi:10.1023/A:1008907227706
Knudsen N, Laurberg P, Perrild H, Bülow I, Ovesen L, Jørgensen T (2002) Risk factors for goiter and thyroid nodules. Thyroid 12:879–888. doi:10.1089/105072502761016502
Galanti MR, Granath F, Cnattingius S, Ekbom-Schnell A, Ekbom A (2005) Cigarette smoking and the risk of goitre and thyroid nodules amongst parous women. J Intern Med 258:257–264. doi:10.1111/j.1365-2796.2005.01523.x
Rasmussen LB, Ovesen L, Bülow I et al (2002) Relations between various measures of iodine intake and thyroid volume, thyroid nodularity, and serum thyroglobulin1−3. Am J Clin Nutr 76:1069–1076
Memon A, Varghese A, Suresh A (2002) Benign thyroid disease and dietary factors in thyroid cancer: a case–control study in Kuwait. Br J Cancer 86:1745–1750. doi:10.1038/sj.bjc.6600303
Surks MI, Chopra IJ, Mariash CN, Nicoloff JT, Solomon DH (1990) American thyroid association guidelines for use of laboratory tests in thyroid disorders. J Am Med Assoc 263:1529–1532. doi:10.1001/jama.263.11.1529
Williams ED, Doniach I, Bjarnason O, Michie W (1977) Thyroid cancer in iodide rich area: a histopathological study. Cancer 39:215–222. doi :10.1002/1097-0142(197701)39:1<215::AID-CNCR2820390134>3.0.CO;2-#
Negri E, Dal Maso L, Ron E et al (1999) A pooled analysis of case–control studies of thyroid cancer. II. Menstrual and reproductive factors. Cancer Causes Control 10:143–145. doi:10.1023/A:1008880429862
La Vecchia C, Ron E, Franceschi S et al (1999) A pooled analysis of case–control studies of thyroid cancer. III. Oral contraceptives, menopausal replacement therapy and other female hormones. Cancer Causes Control 10:157–166. doi:10.1023/A:1008832513932
Rossing MA, Voigt LF, Wiklund KG, Williams M, Daling JR (1998) Use of exogenous hormones and risk of papillary thyroid cancer (Washington, United States). Cancer Causes Control 9:341–349. doi:10.1023/A:1008833422577
Sakoda LC, Horn-Ross PL (2002) Reproductive and menstrual history and papillary thyroid cancer risk: the San Francisco Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev 11:51–57
Gaitan E (1990) Goitrogens in food and water. Annu Rev Nutr 10:21–39. doi:10.1146/annurev.nu.10.070190.000321
Nagataki S, Nyström E (2002) Epidemiology and primary prevention of thyroid cancer. Thyroid 12:889–896. doi:10.1089/105072502761016511
Lind P, Langsteger W, Molnar M, Gallowitsch HJ, Mikosch P, Gomez I (1998) Epidemiology of thyroid diseases in iodine sufficiency. Thyroid 8:1179–1183
Franceschi S (1998) Iodine intake and thyroid carcinoma—a potential risk factor. Exp Clin Endocrinol Diab 106(Suppl 3):S38–S44
Delange F, Lecomte P (2000) Iodine supplementation: benefits outweigh risks. Drug Saf 22:89–95. doi:10.2165/00002018-200022020-00001
Weissel M (2003) Legal augmentation of iodine content in table salt from 10 to 20 mg Kl/kg: documented effects a decade later. Exp Clin Endocrinol Diab 111:187–190. doi:10.1055/s-2003-40461
Kolonel LN, Hankin JH, Wilkens LR, Fukunaga FH, Hinds MW (1990) An epidemiologic study of thyroid cancer in Hawaii. Cancer Causes Control 1:223–234. doi:10.1007/BF00117474
Glattre E, Haldorsen T, Berg JP, Stensvold I, Solvoll K (1993) Norwegian case–control study testing the hypothesis that seafood increases the risk of thyroid cancer. Cancer Causes Control 4:11–16. doi:10.1007/BF00051708
Bosetti C, Kolonel L, Negri E et al (2001) A pooled analysis of case–control studies of thyroid cancer. VI. Fish and shellfish consumption. Cancer Causes Control 12:375–382. doi:10.1023/A:1011267123398
Kanno J, Matsouoka C, Furuta K et al (1999) Tumor promoting effect of goitrogens on the rat thyroid. Toxicol Pathol 18:239–246
Bosetti C, Negri E, Kolonel L et al (2002) A pooled analysis of case–control studies of thyroid cancer. VII. Cruciferous and other vegetables (International). Cancer Causes Control 13:765–775. doi:10.1023/A:1020243527152
Yin F, Giuliano AE, Van Herle AJ (1999) Growth inhibitory effects of flavonoids in human thyroid cancer cell lines. Thyroid 9:369–376
Steinmetz K, Potter JD (1996) Vegetables, fruit, and cancer prevention. J Am Diet Assoc 96:1027–1039. doi:10.1016/S0002-8223(96)00273-8
Horn-Ross PL, Hoggatt KJ, Lee MM (2002) Phytoestrogens and thyroid cancer risk: the San Francisco Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev 11:43–49
Berg JP, Glattre E, Haldorsen T et al (1994) Longchain serum fatty acids and risk of thyroid cancer: a population-based case–control study in Norway. Cancer Causes Control 5:433–439. doi:10.1007/BF01694757
Franceschi S, Levi F, Negri E, Fassina A, La Vecchia C (1991) Diet and thyroid cancer: a pooled analysis of four European case–control studies. Int J Cancer 48:395–398. doi:10.1002/ijc.2910480315
Galanti MR, Hansson L, Bergstrom R et al (1997) Diet and the risk of papillary and follicular thyroid carcinoma: a population-based case–control study in Sweden and Norway. Cancer Causes Control 8:205–214. doi:10.1023/A:1018424430711
Markaki I, Linos D, Linos A (2003) The influence of dietary patterns on the development of thyroid cancer. Eur J Cancer 39:1912–1919. doi:10.1016/S0959-8049(03)00432-5
Mack WJ, Preston-Martin S, Dal Maso L et al (2003) A pooled analysis of case–control studies of thyroid cancer: cigarette smoking and consumption of alcohol, coffee, and tea. Cancer Causes Control 14:773–785. doi:10.1023/A:1026349702909
Glattre E, Thomassen Y, Thoresen SØ, Lund-Larsen PG, Theodorsen L, Aaseth J (1989) Prediagnostic serum selenium in a case–control study of thyroid cancer. Int J Epidemiol 18:45–49. doi:10.1093/ije/18.1.45
D’Avanzo B, Ron E, La Vecchia C, Franceschi S, Negri E, Ziegler R (1997) Selected micronutrient intake and thyroid carcinoma risk. Cancer 79:2186–2192. doi :10.1002/(SICI)1097-0142(19970601)79:11<2186::AID-CNCR17>3.0.CO;2-S
Fioretti F, Tavani A, Gallus S, Franceschi S, Negri E, La Vecchia C (1999) Case–control study of thyroid cancer in northern Italy: attributable risk. Int J Epidemiol 28:626–630. doi:10.1093/ije/28.4.626
Haselkorn T, Stewart SL, Horn-Ross PL (2003) Why are thyroid cancer rates so high in Southeast Asian women living in the United States? The Bay area Thyroid cancer study. Cancer Epidemiol Biomarkers Prev 12:1444–1450
Ron E, Kleinerman RA, Boice JD Jr, LiVolsi VA, Flannery JT, Fraumeni JR Jr (1987) A population-based case–control study of thyroid cancer. J Natl Cancer Inst 79:1–12
Mack W, Preston-Martin S, Bernstein L, Qian D (2002) Lifestyle and other risk factors for thyroid cancer in Los Angeles County females. Ann Epidemiol 12:395–401. doi:10.1016/S1047-2797(01)00281-2
Dal Maso L, La Vecchia C, Franceschi S et al (2000) A pooled analysis of thyroid cancer studies. V. Anthropometric factors. Cancer Causes Control 11:137–144. doi:10.1023/A:1008938520101
Negri E, Ron E, Franceschi S et al (2002) Risk factors for medullary thyroid carcinoma: a pooled analysis. Cancer Causes Control 13:365–372. doi:10.1023/A:1015263718760
Vella V, Sciacca L, Pandini G et al (2001) The IGF system in thyroid cancer: new concepts. J Clin Pathol Mol Pathol 54:121–125
Thissein J-P, Ketelslegers J-M, Underwood LE (1994) Nutritional regulation of the insulin-like growth factors. Endocr Rev 15:80–101. doi:10.1210/er.15.1.80
Wingren G, Hatschek T, Axelson O (1993) Determinants of papillary cancer of the thyroid. Am J Epidemiol 138:482–491
Rossing MA, Remler R, Voigt LF, Wicklund KG, Daling JR (2001) Recreational physical activity and risk of papillary thyroid cancer (United States). Cancer Causes Control 12:881–885. doi:10.1023/A:1013757030600
World Cancer Research Fund, American Institute for Cancer Research (2007) Food nutrition, physical activity and the prevention of cancer: a global perspective. American Institute for Cancer Research, Washington, DC
Willett WC (2006) Diet and nutrition. In: Schottenfeld S, Fraumeni JR Jr (eds) Cancer epidemiology and prevention, 3rd edn. Oxford University Press, Oxford, pp 405–421
Acknowledgment
The author wishes to thank Dr C. Braga for her helpful comments and Mrs L. Mei for editorial assistance.
Financial support
This work was conducted with the contribution of the Italian Association for Cancer Research. The work of this paper was undertaken while CLV was a Senior Fellow at the International Agency for Research on Cancer.
Conflicts of interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dal Maso, L., Bosetti, C., La Vecchia, C. et al. Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors. Cancer Causes Control 20, 75–86 (2009). https://doi.org/10.1007/s10552-008-9219-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9219-5