Abstract
Immune checkpoint inhibitors have modified the treatment algorithm in a variety of cancer types, including breast cancer. Nevertheless, optimal selection of ideal candidates to these drugs remains an unmet need. Although PD-L1 expression by immunohistochemistry seems to be the most promising biomarker to date, its predictive ability is far from ideal. Thus, the development of new predictive biomarkers is essential for a better selection of patients. Here, we discuss potential biomarkers beyond PD-L1 that could play an important role in precision cancer immunotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, immune checkpoint inhibitors (ICI) have demonstrated significant clinical activity in more than 15 cancer types [1]. Even though breast cancer has been considered poorly immunogenic, anti-programmed death 1 (PD-1)/programmed death-ligand 1 (PD-L1) drugs have started to make progress in triple-negative breast cancer (TNBC) with promising outcomes both in the early [2, 3] and the metastatic setting [4, 5]. These have led to the food and drug administration (FDA) approval, in 2020, of the anti-PD-1 pembrolizumab in combination with chemotherapy (nab-paclitaxel, paclitaxel, or gemcitabine–carboplatin) for first-line metastatic TNBC [6] and for patients diagnosed with high-risk early-stage TNBC in combination with chemotherapy (anthracyclines plus cyclophosphamide followed by paclitaxel plus carboplatin) as a neoadjuvant treatment and then continued as an adjuvant treatment after surgery. The European Medicine Agency (EMA) approved the anti-PD-L1, atezolizumab, in combination with nab-paclitaxel for first-line metastatic TNBC expressing PD-L1.
Although detection of PD-L1 by immunohistochemistry (IHC) has been validated and widely used as a biomarker for patient’s selection, several issues have hampered the generalization of PD-L1 as the biomarker that guides the use of ICI in oncology. One important issue is the determination of this biomarker, each sponsor implemented a different IHC-based assay for PD-L1 evaluation, implying that different antibodies (28-8 rabbit [Dako], 22.C3 mouse [Dako], 5H1, SP142 rabbit [Roche Ventana], SP263 rabbit [Roche Ventana]) were used and different PD-L1-positive cells populations evaluated (i.e., tumor cells versus immune cells versus both). Moreover, tumor samples are considered PD-L1 positive according to different thresholds, leading to high discrepancies in PD-L1 positivity/negativity [4, 7]. Furthermore, the usage of different IHC assays affect the PD-L1 positivity in the same tumor samples [8]. This huge variability highlights the issues around PD-L1 status determination. One clear example of this controversy is the recent approval of the two anti-PD-L1 treatments: atezolizumab plus nab-paclitaxel for TNBC only in tumors with ≥ 1% PD-L1 expression by IHC using the Ventana assay (SP142) [4], while the benefit from pembrolizumab plus chemotherapy in the KEYNOTE-355 trial was observed in TNBC with a combined positive PD-L1 score (CPS), which determines PD-L1 in tumor cells, lymphocytes, and macrophages using the Dako assay (22C3) [9].
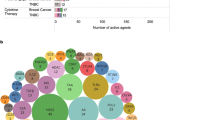
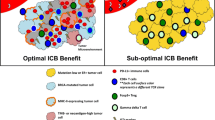
Even though PD-L1 expression is correlated with anti-PD-1/PD-L1 treatment response, response rates vary substantially across patients and most patients do not benefit. Moreover, there are many patients with low to undetectable PD-L1 expression who experience durable clinical benefit to ICI [10, 11], suggesting that other factors related with the tumor or the immune microenvironment may be responsible for the response to different ICI. An example is the benefit of anti-PD-1 treatment in combination with chemotherapy in early-stage TNBC regardless of the PD-L1 expression [2, 12]. Thus, there is a need to identify additional and/or better predictive biomarkers of response to these therapies and to better understand the biology behind their activity. The present literature review discusses biomarkers beyond PD-L1 found within the tumor cells, the tumor microenvironment or the circulation (Fig. 1), all of which are potentially predictive of response and survival to ICI.
Tumor-infiltrating lymphocytes (TILs)
In the last years, TILs have emerged as an attractive biomarker due to its easy and feasible determination [13]. The prevalence of TILs is highly heterogeneous across breast cancer subtypes, with TNBC being the most immune-infiltrated followed by the HER2-postive (HER2+) and the hormone receptor-positive/HER2-negative (HR+/HER2−) breast cancers [14, 15].
Morphologic evaluation of TILs may help select patients with clinically relevant outcomes both in the metastatic and early settings. In the metastatic setting, higher percentage of TILs may suggest a benefit from ICI in monotherapy in TNBC [16, 17]. More recently, a retrospective study performed on the tumor samples from the IMpassion130 phase III trial, where patients were treated with nab-paclitaxel ± atezolizumab, showed a benefit of atezolizumab in terms of progression-free survival (PFS) and overall survival (OS) in patients with PD-L1-positive (PD-L1+) tumors with intermediate/high TILs [18]. In HER2+ breast cancer, patients with PD-L1+ tumors were correlated with higher TILs and tumors with higher TILs had an improved objective response rate (ORR) to pembrolizumab plus trastuzumab compared with patients with low TILs tumor samples who participated in the PANACEA phase Ib-II trial [19]. Finally, the KATE-2 phase II trial suggested that patients with high percentage of TILs may derive a larger benefit from the addition of atezolizumab to trastuzumab-emtansine (T-DM1) than those with low percentage of TILs [20].
In the early-stage setting, TILs have been related to an increased frequency of achieving a pathologic complete response (pCR) in all breast cancer subtypes after neoadjuvant chemotherapy [14, 21,22,23,24] and have predictive and prognostic value in HER2+ breast cancer treated with HER2 blockade and chemotherapy [23, 25,26,27,28,29]. In HR+/HER2− breast cancer, controversial data exist, with studies indicating that increased TILs are related with poor outcomes [14] and other suggesting that high TILs are associated with favorable outcomes in tumors with high Ki-67 [30]. In TNBC, high percentages of TILs are associated with a lower probability of recurrence and death after neoadjuvant chemotherapy [29]. Furthermore, an excellent prognosis has been observed in early-stage TNBC with high TILs without receiving any systemic therapy [31], even in young patients [32]. This observation opens the door to evaluate the value of TILs to help de-escalate the use of systemic chemotherapy in early-stage TNBC. Further studies are needed.
In the early-stage setting, the predictive value of TILs has also been evaluated in patients treated with neoadjuvant ICI in combination with chemotherapy [9]. For example, in the phase II GeparNuevo trial [3], patients with TNBC were randomized to durvalumab or placebo every 4 weeks in addition to an anthracycline/taxane-based neoadjuvant chemotherapy regimen. In both arms, higher TILs were significantly associated with an increased pCR, with a trend for an increase in pCR rates in PD-L1+ disease [3]. Moreover, analysis of the NeoTRIPaPDL1 data demonstrated increased pCR rates in tumors with PD-L1+ and high TILs treated with neoadjuvant atezolizumab plus chemotherapy and indicated that TILs evaluated after 1 cycle of treatment were more informative than TILs at baseline [33]. Of note, the value of TILs in KEYNOTE-522 [2] and IMpassion031 [12] phase III trials is currently unknown. Finally, TILs on residual disease after exposure to neoadjuvant therapy has been linked to improved survival rates in TNBC and HER2+ breast cancer [34, 35].
Futures studies should perform a deep characterization of the immune microenvironment and link these features with patient’s outcomes. For example, CD8-enriched TNBC treated with ICI in combination with chemotherapy has been linked to better outcomes [36]; however, these results have not been validated in the IMpassion130 phase III trial [18]. In HER2+ disease, a correlation was found between CD8+ TILs, measured at baseline, and pCR after anti-HER2 treatment. In addition, the CD8/FOXP3 ratio has been associated with both increased pCR and favorable prognosis following anti-HER2-based neoadjuvant treatment [20, 37, 38]. More studies are needed to better characterize the immune cell compartment and its implications in patient’s outcomes.
Tumor mutational burden
Tumor mutational burden (TMB) is defined as the number of somatic mutations per DNA megabase pair (mut/Mb). A proportion of these mutations give rise to neoantigens, which are processed by the antigen-processing machinery and loaded on to major histocompatibility complex (MHC) molecules for presentation on the cell surface. Some of these neoantigens are immunogenic, which could lead to a major T-cell infiltration and consequently a better response to immunotherapy, especially in cancers with a TMB of 10 mut/Mb or greater (called TMB-high [TMB-H], as defined by the targeted sequencing FoundationOne CDx assay [39]) [40, 41]. Indeed, several studies have shown association of high TMB with immunotherapy response across different tumor types [42, 43]. Recently, a meta-analysis published by Yarchoan and colleagues showed an association between TMB (as a continuous variable) and objective response rate (ORR) across different tumor types to anti-PD-1 and anti PD-L1 therapies [44]. The prospective biomarker analysis of the multicohort, non-randomized, open-label phase II KEYNOTE-158 trial demonstrated a correlation with TMB-H tumors and pembrolizumab response in heavily pre-treated patients across 10 cancer types, with an ORR of 29% (95% confidence interval [CI] 21–39) in TMB-H and 6% ( 95% CI 5–8) in non-TMB-H [45] tumors, which led to the approval of pembrolizumab in TMB-H tumors by the FDA in 2020.
In breast cancer, TMB is generally intermediate [46] and its role in tumor immunogenicity is less clear than in other cancer types. The prevalence of hypermutations in breast cancer is about 5%, using the standard definition of TMB-H as ≥ 10 mut/Mb [39]. However, differences in TMB-H across histological groups and molecular subtypes have been described. TMB-H tumors are more prevalent in metastatic than primary disease, in lobular cancer compared to other histological groups, and in TNBC than in estrogen receptor-positive (ER +) or HER2+ breast cancers, and ORR and durable response rates are observed in TMB-H tumors [47]. Importantly, in TMB-H breast cancers, the most common mutational processes are APOBEC activity (59.2%) and mismatch repair deficiency (dMMR; 36.4%) [47] which will be further discussed below.
Different studies have tried to evaluate TMB as a biomarker of response in metastatic breast cancer. Results from the phase II TAPUR trial, where 28 heavily pre-treated patients with TMB-H (≥ 9 mut/Mb) metastatic breast cancer were treated with pembrolizumab in monotherapy, demonstrated an ORR of 21% (95% CI 8–41) and the median PFS was 10.6 weeks (95% CI 7.7–21.1) with a median OS of 30.6 weeks (95% CI 18.3–103.3). However, TMB did not seem to be related with PFS [48]. In the KEYNOTE-119 phase III trial [17], approximately 42% (253/601) of patients included in the trial had TMB data available (131 patients in the pembrolizumab arm and 121 in the chemotherapy arm) and 10% were TMB-H (≥ 10mut/Mb). However, no statistical differences were observed, probably due to the TMB-H limited sample size, but a tendency could be observed toward benefit in those patients with TMB-H tumors treated with pembrolizumab in terms of ORR, PFS, and OS [49]. TMB has also been explored in the GepardNuevo phase II trial, which evaluated durvalumab and neoadjuvant anthracycline/taxane-based chemotherapy in early TNBC [3], demonstrating a significantly higher TMB in patients achieving pCR regardless of treatment arm. In this study, a predictive value of TMB as a continuous variable for pCR among all patients was observed regardless of treatment arm [50]. Currently, the open-label, single-arm, multicenter, phase II NIMBUS study is evaluating the combination of nivolumab plus ipilimumab in patients with TMB-H HER2-negative metastatic breast cancer [51].
Despite the approval in 2020 of TMB-H by the FDA as a new biomarker of response to ICI, there are some issues to be considered. Firstly, breast cancer was not represented in the KEYNOTE-158 trial [45]; various detection methods have been used to quantify the TMB, whole-exome sequencing (WES) was the initial option, then some studies used targeted gene panels to predict TMB; different thresholds of TMB have been used across cancer types; in addition, TMB varies widely from patient to patient and across tumor types. Finally, a recent analysis across 25 tumors has shown that determination of TMB-H alone might not be enough for response prediction across cancer types [52].
Mismatch repair deficiency/microsatellite instability
DNA mismatch repair (MMR) is an evolutionarily conserved system that removes biosynthetic errors from newly synthesized DNA improving the fidelity of DNA replication [53]. Deficiencies in MMR (dMMR) can cause errors in DNA replication leading to microsatellite instability (MSI) and can be observed in several cancer types [54]. Microsatellites are tandem repeat sequences of 1 to 10 nucleotides [55]. Increased mutational load caused by dMMR/MSI has been shown to predict response to anti-PD-1/PD-L1 treatment in different tumors, especially in colorectal and endometrial cancer [54] leading to the FDA approval of pembrolizumab for any tumor type with dMMR/MSI determined by IHC or molecular tests [56, 57]. More recently, the FDA has approved dostarlimab, an anti-PD-1 treatment, for patients with solid tumors with dMMR that have progressed to different treatments [58].
Little is known about the predictive value of dMMR/MSI in breast cancer, probably due to its low prevalence which is approximately 1–2% [54, 59]. Some data have demonstrated that dMMR/MSI can be found across all breast cancer subtypes, especially in high-grade tumors and in tumors with low progesterone receptor expression. dMMR/MSI status could confer poor prognosis in patients with ER+ breast cancer treated with tamoxifen [59, 60].
Importantly, durable responses to ICI have been reported in patients with metastatic breast cancer including a dMMR/MSI TNBC treated with nivolumab [61], a dMMR/MSI luminal treated with pembrolizumab [62], and a TMB-H and dMMR HER2+ treated with pembrolizumab and trastuzumab [63]. Despite of its low prevalence, the determination of ddMR as a biomarker of response to ICI, potentially combined with TMB, could be crucial to better identify candidates for these therapies.
APOBEC signature
The APOBEC family of zinc-coordinating enzymes converts cytosine to uracil in single-strand DNA. The enzymatic activity of this family member is essential for both adaptive and innate immune responses [64]. Dysregulated activity of cytidine deaminases is a major source of mutations in several types of cancers [47]. APOBEC-mediated mutational signatures (signature 2 and 13) have been detected in at least 22 different tumor types and are particularly enriched in bladder, head and neck, cervical, and breast cancer [65]. Among breast cancer, the APOBEC-related signature contributed to higher percent of mutations in metastatic tumors confirming a link between APOBEC-mediated mutagenesis and the acquisition of subclonal mutations, leading to increased TMB and potential neoantigens expression [66]. Importantly, ORR and durable response rates to immunotherapy have been observed in TMB-H breast cancers with dominant APOBEC activity [47], including patients with PD-L1-negative tumors [11, 67].
Differences in the APOBEC signatures across breast cancer subtypes have been described, with HER2+ breast tumors having the highest median levels of APOBEC signature enrichment [68]. At the same time, several studies have now linked APOBEC genetic signatures with metastatic HR+ and HER2− breast cancer [66, 69], high TILs [70], and the PAM50 HER2-enriched molecular subtype [65, 71]. Altogether, little is known about the association of APOBEC signatures with response to ICI, but the indirect and emerging data warrant further studies to validate these signatures as predictive biomarkers of response.
CD274 amplification
CD274, which encodes for PD-L1 protein, is located in the chromosomic region of 9p24.1, and amplification of this gene has recently been evaluated in a pan-cancer cohort of 48,782 tumors, demonstrating a prevalence of 0.7% across tumors, being higher in PD-L1+ than in PD-L1-negative tumors (1.56% vs 0.1%) [72]. Moreover, CD274 have been associated with frequent and durable responses to ICI [73]. In breast cancer, 9p24.1 amplifications have been observed in approximately 1.2% of tumors within the MSK-IMPACT metastatic breast cancer cohort, with significantly higher events for TNBC than non-TNBC (5.1% vs 0.5%) [74]. The predictive value of CD274 amplifications has been evaluated in samples of patients with metastatic breast cancer included in the randomized phase II SAFIR02-IMMUNO study, where patients with TNBC had a higher proportion of CD274 amplifications and showed improvement of OS with durvalumab in CD274-amplified tumors (hazard ratio = 0.17, 95% CI 0.05–0.55) [75]. More prospective studies are needed to validate CD274 amplification as a biomarker of response to ICI.
POLE and POLD1 mutations
Proofreading exonucleases domains of the DNA polymerases POLE and POLD1 are essential for fidelity in DNA replication. Germline or somatic mutations in these genes lead to DNA repair deficiencies and MSI and are observed in hypermutated tumors [76]. The prevalence of POLE and POLD1 mutations was evaluated in a pan-cancer cohort of 47,721 patients and POLE and POLD1 mutational frequencies were 2.8% and 1.4%, respectively, and were associated with benefit from ICI [77]. POLE and POLD1 mutations are particularly promising in predicting ICI efficacy in endometrial cancer [78]. In breast cancer, POLE or POLD1 mutations are observed in approximately 1.5% of tumors [77] and are associated with TMB-H tumors [77, 79]. Therefore, these tumors could be amenable to ICI but the predictive value of POLE and POLD1 mutations beyond TMB remains unknown.
Gene expression-based biomarkers
In the last years, several studies have suggested potential predictive factors of response to immune checkpoint blockade based on gene expression. The most described to date has been the tumor inflammation signature (TIS) or T cell-inflamed gene expression profile, which measures the expression of 18 genes associated with cytotoxic cells, antigen presentation, and interferon gamma (IFNγ) activity and was first associated with response to the anti-PD-1 ICI pembrolizumab across cancer types [80, 81], of the KEYNOTE-001 (melanoma and non-small cell lung cancer), the KEYNOTE-012 (head and neck squamous cell carcinoma, gastric cancer, triple-negative breast cancer, and bladder cancer), and the KEYNOTE-028 (anal canal, biliary, colorectal, esophageal, and ovarian cancer).
In the TCGA breast cancer dataset, the Basal-like and HER2-enriched molecular subtypes have higher TIS scores than the luminal subtypes [82], concordant with the higher infiltration of TILs observed in these subtypes, and therefore could benefit more from ICI. To this end, the SOLTI-1716 TATEN (NCT04251169) phase II trial is currently evaluating the effects of pembrolizumab + paclitaxel in Basal-like and HER2-enriched metastatic HR+/HER2− breast cancer [83].
In metastatic breast cancer, we have recently reported that lung and pleura metastatic sites have the highest expression of genes included in the TIS score, while brain and liver have the lowest [84], which could be of relevance when designing trials with ICI. Finally, a composite biomarker comprising TIS and TMB has demonstrated to better predict response to pembrolizumab in > 300 patient’s advanced tumor samples across 22 tumor types from four KEYNOTE clinical trials, including 12 TNBC and 3 HR+/HER2− breast cancers [85]. However, these results have not been further validated.
Single PD-1 mRNA expression might also be of value. Indeed, we conducted [86] an analysis of 10,078 tumor samples across 34 different cancer types from the TCGA and 773 tumor samples across 17 cancer types from Hospital Clínic of Barcelona. PD-1 mRNA expression was found associated with CD8 T-cell-related genes and signatures, and the proportion of PD-1 mRNA-high tumors across 10 cancer types was found strongly correlated with ORR to anti-PD-1 ICI reported in the literature as well as in our internal pan-cancer dataset. Importantly, we observed that PD-1 mRNA alone better predicts ORR across tumors than other immune signatures, including the TIS score, PD-L1 expression, or TILs. In breast cancer, we identified PD-1 mRNA-high tumors in Basal-like (29%), HER2-enriched (16–31%), and Luminal A and B (8–9%) subtypes, all of which could potentially benefit from ICIs [86]. To validate PD-1 mRNA as a tumor agnostic biomarker of response to ICI, the SOLTI-1904 ACROPOLI phase II trial (NCT04802876) is evaluating the efficacy of the anti-PD-1 spartalizumab monotherapy in PD-1 mRNA-high tumors.
Recently, a recent retrospective RNA sequencing analysis of metastatic TNBC samples from the IMpassion130 phase III trial [87] observed improved PFS with atezolizumab and nab-paclitaxel in PD-L1-positive tumors that were Basal-like and immune-activated (BLIA) or Basal-like immunosuppressed (BLIS) [88]. Increased gene expression of proliferation and DNA repair pathways has also been associated with improved PFS, while potential mechanisms of resistance observed in PD-L1+ tumors were the luminal androgen receptor (LAR) molecular subtype and increased angiogenesis, EMT, hedgehog signaling, estrogen response, and TNF signaling pathways. Regarding OS, a benefit of atezolizumab in the BLIA molecular subtype has been described, while resistance has been observed in the BLIS and LAR molecular subtypes [87].
In early breast cancer, the predictive value of several gene expression signatures has been evaluated in samples from the neoadjuvant NeoTRIPaPDL1 trial of atezolizumab, carboplatin, and nab-paclitaxel in patients with early high-risk and locally advanced TNBC. The 27-gene IO score was predictive of atezolizumab benefit, while angiogenesis and lipid/glutamine metabolism gene signatures were associated with resistance [89]. Finally, a translational study of samples from the GIADA phase II trial of stage II-IIIA HR+/HER2- pre-menopausal breast cancer patients treated with neoadjuvant anthracycline chemotherapy followed by nivolumab and endocrine therapy has identified the PAM50 Basal-like molecular subtype and TILs as potential biomarkers of response [90].
Circulating tumor DNA (ctDNA)
Liquid biopsy includes circulating tumor DNA (ctDNA), circulating tumor cells (CTC), and exosomes; and it is non-invasive, rapid, precise, and provides real-time information regarding the genomic state of a disease [91]. ctDNA analysis might allow the identification of prognostic and predictive biomarkers for ICI therapy. On one side, baseline ctDNA has been reported to correlate with tumor burden and proliferation and it has been proposed as a prognostic factor in patients with metastatic cancer treated with immunotherapy [92]. For instance, in melanoma [93] and in urothelial cancer [94], high baseline ctDNA levels have been associated with lower PFS and OS benefit to ICI. On the other side, liquid biopsies represent an opportunity to detect biomarkers of response in blood such as MSI and TMB, which can be estimated from ctDNA. In pretreatment plasma samples of a pan-cancer cohorts, detection of blood MSI and TMB-H was associated with PFS benefit to ICI [95]. In non-small cell lung cancer, high blood TMB has been associated with benefit from atezolizumab in the POPLAR and OAK clinical trials [96]. The phase III MYSTIC randomized study identified ≥ 20 mut/Mb as an optimal threshold for OS benefit with durvalumab plus tremelimumab [97]. Moreover, monitoring ctDNA during therapy can be a surrogate of response to therapy in breast cancer [91, 93]. Indeed, recent studies have demonstrated that ctDNA clearance during ICI as a biomarker of improved survival both in patients with advanced solid tumors treated with pembrolizumab in the INSPIRE phase II clinical trial, including a TNBC cohort [98] and patients with 16 advanced-stage tumor types from the Study 1108, ATLANTIC and Study 10 phase I/II trials of durvalumab (± the anti-CTLA4 therapy tremelimumab) [99]. Therefore, future clinical trials with ICI should consider including ctDNA dynamics.
Microbiome
The microbiome has been implicated in development and progression of several types of cancer [100]. In breast cancer in particular, a distinct breast microbiome and differences between the breast tissue microbiome in benign and malignant disease have been demonstrated, observing that patients diagnosed with breast cancer had lower basal levels of some bacteria compared with non-cancer patients [101, 102]. Moreover, bacteria or their components may influence the local immune microenvironment [102] which could have therapeutic implications. The composition of gut microbiome could affect immunotherapy response, due to the pro-inflammatory microenvironment created by some bacteria which could lead to a favorable immunotherapy response [103]. Higher diversity of some bacteria has been related with better response and it is suggested that the modification of the microbiome could have an impact on the ICI efficacy [104]. To date, the data available are too unspecific to use the microbiome as a reliable biomarker; more studies will be needed to improve the knowledge and its implications in cancer treatment and prognosis.
Conclusion
Although immunotherapy has been approved for PD-L1+ advanced TNBC, the benefit is modest. Several studies have recently reported responses to ICI in patients with PD-L1-negative tumors. Moreover, discrepancies have been observed regarding the value of PD-L1 expression in predicting benefit in early [2, 12] and metastatic [4] breast cancer, which may be due to different PD-L1 IHC assays or differences in the biology of the early vs metastatic breast cancer. In the early setting, immunotherapy seems to impact the most, regardless the PD-L1 expression.
Here we describe potential biomarkers that could be useful for patient selection (Table 1). However, none has yet been validated in prospective trials. Emerging data show that the combination of different biomarkers may help better identify those patients that will benefit to ICI and warrant further translational studies to improve patient selection [105]. Identifying the suitable time when these biomarkers are determined (before/during treatment) may be critical due to different changes in the TME caused by the ICI treatments. Furthermore, different ICI may require different biomarkers. Taken together, prospective trials are needed to identify biomarkers of response and standardize their determination to do a more accurate selection of the patients who will benefit from immunotherapy.
References
Sharma P, Allison JP (2015) The future of immune checkpoint therapy. Science 348:56–61. https://doi.org/10.1126/SCIENCE.AAA8172
Schmid P, Cortes J, Pusztai L et al (2020) Pembrolizumab for early triple-negative breast cancer. N Engl J Med 382:810–821. https://doi.org/10.1056/nejmoa1910549
Loibl S, Untch M, Burchardi N et al (2019) A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: clinical results and biomarker analysis of GeparNuevo study. Ann Oncol 30:1279–1288. https://doi.org/10.1093/annonc/mdz158
Schmid P, Adams S, Rugo HS et al (2018) Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 379:2108–2121. https://doi.org/10.1056/NEJMoa1809615
Schmid P, Adams S, Rugo HS et al (2019) IMpassion130: updated overall survival (OS) from a global, randomized, double-blind, placebo-controlled, Phase III study of atezolizumab (atezo) + nab- paclitaxel (nP) in previously untreated locally advanced or metastatic triple-negative breast ca. J Clin Oncol 37:1003–1003. https://doi.org/10.1200/JCO.2019.37.15_suppl.1003
Cortes J, Cescon DW, Rugo HS et al (2020) KEYNOTE-355: Randomized, double-blind, phase III study of pembrolizumab + chemotherapy versus placebo + chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer. J Clin Oncol 38:1000–1000. https://doi.org/10.1200/jco.2020.38.15_suppl.1000
Cortes J, Cescon DW, Rugo HS et al (2020) Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 396:1817–1828. https://doi.org/10.1016/S0140-6736(20)32531-9
Rugo HS, Loi S, Adams S et al (2019) Performance of PD-L1 immunohistochemistry (IHC) assays in unresectable locally advanced or metastatic triple-negative breast cancer (mTNBC): post-hoc analysis of IMpassion130. Ann Oncol 30:v858–v859. https://doi.org/10.1093/annonc/mdz394.009
Schmid P, Salgado R, Park YH et al (2020) Pembrolizumab plus chemotherapy as neoadjuvant treatment of high-risk, early-stage triple-negative breast cancer: results from the phase 1b open-label, multicohort KEYNOTE-173 study. Ann Oncol. https://doi.org/10.1016/j.annonc.2020.01.072
Sunshine J, Taube JM (2015) PD-1/PD-L1 inhibitors. Curr Opin Pharmacol 23:32. https://doi.org/10.1016/J.COPH.2015.05.011
Brasó-Maristany F, Sansó M, Chic N et al (2021) Case report: a case study documenting the activity of atezolizumab in a PD-L1-negative triple-negative breast cancer. Front Oncol. https://doi.org/10.3389/FONC.2021.710596
Mittendorf EA, Zhang H, Barrios CH et al (2020) Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. Lancet 396:1090–1100. https://doi.org/10.1016/S0140-6736(20)31953-X
Salgado R, Denkert C, Demaria S et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26:259–271. https://doi.org/10.1093/ANNONC/MDU450
Denkert C, von Minckwitz G, Darb-Esfahani S et al (2018) Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol 19:40–50. https://doi.org/10.1016/S1470-2045(17)30904-X
Stanton SE, Adams S, Disis ML (2016) Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: a systematic review. JAMA Oncol 2:1354–1360. https://doi.org/10.1001/JAMAONCOL.2016.1061
Loi S, Adams S, Schmid P et al (2017) Relationship between tumor infiltrating lymphocyte (TIL) levels and response to pembrolizumab (pembro) in metastatic triple-negative breast cancer (mTNBC): results from KEYNOTE-086. Ann Oncol 28:v608. https://doi.org/10.1093/ANNONC/MDX440.005
Winer EP, Lipatov O, Im SA et al (2021) Pembrolizumab versus investigator-choice chemotherapy for metastatic triple-negative breast cancer (KEYNOTE-119): a randomised, open-label, phase 3 trial. Lancet Oncol 22:499–511. https://doi.org/10.1016/S1470-2045(20)30754-3
Emens LA, Molinero L, Loi S et al (2021) Atezolizumab and nab -paclitaxel in advanced triple-negative breast cancer: biomarker evaluation of the IMpassion130 study. JNCI J Natl Cancer Inst 113:1005–1016. https://doi.org/10.1093/jnci/djab004
Loi S, Giobbie-Hurder A, Gombos A et al (2019) Pembrolizumab plus trastuzumab in trastuzumab-resistant, advanced, HER2-positive breast cancer (PANACEA): a single-arm, multicentre, phase 1b–2 trial. Lancet Oncol 20:371–382. https://doi.org/10.1016/S1470-2045(18)30812-X
Emens LA, Esteva FJ, Beresford M et al (2020) Trastuzumab emtansine plus atezolizumab versus trastuzumab emtansine plus placebo in previously treated, HER2-positive advanced breast cancer (KATE2): a phase 2, multicentre, randomised, double-blind trial. Lancet Oncol 21:1283–1295. https://doi.org/10.1016/S1470-2045(20)30465-4
Salgado R, Denkert C, Campbell C et al (2015) Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol 1:448–455. https://doi.org/10.1001/jamaoncol.2015.0830
Denkert C, von Minckwitz G, Brase JC et al (2015) Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2–positive and triple-negative primary breast cancers. J Clin Oncol 33:983–991. https://doi.org/10.1200/JCO.2014.58.1967
Heppner BI, Untch M, Denkert C et al (2016) Tumor-infiltrating lymphocytes: a predictive and prognostic biomarker in neoadjuvant-treated HER2-positive breast cancer. Clin Cancer Res 22:5747–5754. https://doi.org/10.1158/1078-0432.CCR-15-2338
Issa-Nummer Y, Darb-Esfahani S, Loibl S et al (2013) Prospective validation of immunological infiltrate for prediction of response to neoadjuvant chemotherapy in HER2-negative breast cancer—a substudy of the neoadjuvant geparquinto trial. PLoS ONE 8:e79775. https://doi.org/10.1371/JOURNAL.PONE.0079775
Nuciforo P, Pascual T, Cortés J et al (2018) A predictive model of pathologic response based on tumor cellularity and tumor-infiltrating lymphocytes (CelTIL) in HER2-positive breast cancer treated with chemo-free dual HER2 blockade. Ann Oncol 29:170–177. https://doi.org/10.1093/annonc/mdx647
Chic N, Luen SJ, Nuciforo P et al (2021) Tumor cellularity and infiltrating lymphocytes as a survival surrogate in HER2-positive breast cancer. JNCI J Natl Cancer Inst. https://doi.org/10.1093/JNCI/DJAB057
Kim R, Song N, Gavin P et al (2019) Stromal tumor-infiltrating lymphocytes in NRG oncology/NSABP B-31 adjuvant trial for early-stage HER2-positive breast cancer. J Natl Cancer Inst 111:867–871. https://doi.org/10.1093/JNCI/DJZ032
Krop IE, Paulson J, Campbell C et al (2019) Genomic correlates of response to adjuvant trastuzumab (H) and pertuzumab (P) in HER2+ breast cancer (BC): biomarker analysis of the APHINITY trial. J Clin Oncol 37:1012–1012. https://doi.org/10.1200/JCO.2019.37.15_SUPPL.1012
Loi S, Michiels S, Salgado R et al (2014) Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 25:1544–1550. https://doi.org/10.1093/ANNONC/MDU112
Criscitiello C, Vingiani A, Maisonneuve P et al (2020) Tumor-infiltrating lymphocytes (TILs) in ER+/HER2− breast cancer. Breast Cancer Res Treat 183:347–354. https://doi.org/10.1007/s10549-020-05771-7
Park JH, Jonas SF, Bataillon G et al (2019) Prognostic value of tumor-infiltrating lymphocytes in patients with early-stage triple-negative breast cancers (TNBC) who did not receive adjuvant chemotherapy. Ann Oncol 30:1941–1949. https://doi.org/10.1093/ANNONC/MDZ395
De Jong VMT, Wang Y, Opdam M et al (2020) 159O Prognostic value of tumour infiltrating lymphocytes in young triple negative breast cancer patients who did not receive adjuvant systemic treatment; by the PARADIGM study group. Ann Oncol 31:S303. https://doi.org/10.1016/J.ANNONC.2020.08.281
Bianchini G, Huang C-S, Egle D et al (2020) LBA13 tumour infiltrating lymphocytes (TILs), PD-L1 expression and their dynamics in the NeoTRIPaPDL1 trial. Ann Oncol 31:S1145–S1146. https://doi.org/10.1016/J.ANNONC.2020.08.2241
Loi S, Dushyanthen S, Beavis PA et al (2016) RAS/MAPK activation is associated with reduced tumor-infiltrating lymphocytes in triple-negative breast cancer: therapeutic cooperation between MEK and PD-1/PD-L1 immune checkpoint inhibitors. Clin Cancer Res 22:1499–1509. https://doi.org/10.1158/1078-0432.CCR-15-1125
Dieci MV, Radosevic-Robin N, Fineberg S et al (2018) Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: a report of the International immuno-oncology biomarker working group on breast cancer. Semin Cancer Biol 52:16–25
Adams S, Diamond JR, Hamilton E et al (2019) Atezolizumab plus nab-paclitaxel in the treatment of metastatic triple-negative breast cancer with 2-year survival follow-up: a phase 1b clinical trial. JAMA Oncol 5:334–342. https://doi.org/10.1001/JAMAONCOL.2018.5152
Asano Y, Kashiwagi S, Goto W et al (2016) Tumour-infiltrating CD8 to FOXP3 lymphocyte ratio in predicting treatment responses to neoadjuvant chemotherapy of aggressive breast cancer. Br J Surg. https://doi.org/10.1002/bjs.10127
De AC, Nagi C, Hoyt CC et al (2020) Evaluation of the predictive role of tumor immune infiltrate in patients with HER2-positive breast cancer treated with neoadjuvant anti-HER2 therapy without chemotherapy. Clin Cancer Res 26:738–745. https://doi.org/10.1158/1078-0432.CCR-19-1402
Merino DM, McShane L, Butler M et al (2019) TMB standardization by alignment to reference standards: phase II of the friends of cancer research TMB harmonization project. J Clin Oncol 37:2624–2624. https://doi.org/10.1200/jco.2019.37.15_suppl.2624
Chan TA, Yarchoan M, Jaffee E et al (2019) Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol 30:44–56. https://doi.org/10.1093/ANNONC/MDY495
Havel JJ, Chowell D, Chan TA (2019) The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat Rev Cancer 19:133–150
Van Allen EM, Miao D, Schilling B et al (2015) Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science 350:207–211. https://doi.org/10.1126/science.aad0095
Rizvi NA, Hellmann MD, Snyder A et al (2015) Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348:124–128. https://doi.org/10.1126/science.aaa1348
Yarchoan M, Hopkins A, Jaffee EM (2017) Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med 377:2500–2501. https://doi.org/10.1056/NEJMc1713444
Marabelle A, Fakih M, Lopez J et al (2020) Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol 21:1353–1365. https://doi.org/10.1016/S1470-2045(20)30445-9
O’Meara TA, Tolaney SM (2021) Tumor mutational burden as a predictor of immunotherapy response in breast cancer. Oncotarget 12:394–400
Barroso-Sousa R, Jain E, Cohen O et al (2020) Prevalence and mutational determinants of high tumor mutation burden in breast cancer. Ann Oncol 31:387–394. https://doi.org/10.1016/j.annonc.2019.11.010
Alva AS, Mangat PK, Garrett-Mayer E et al (2021) Pembrolizumab in patients with metastatic breast cancer with high tumor mutational burden: results from the targeted agent and profiling utilization registry (TAPUR) study. J Clin Oncol 39:2443–2451. https://doi.org/10.1200/JCO.20.02923
Winer EP, Lipatov O, Im S-A et al (2020) Association of tumor mutational burden (TMB) and clinical outcomes with pembrolizumab (pembro) versus chemotherapy (chemo) in patients with metastatic triple-negative breast cancer (mTNBC) from KEYNOTE-119. J Clin Oncol 38:1013–1013. https://doi.org/10.1200/jco.2020.38.15_suppl.1013
Karn T, Denkert C, Weber KE et al (2020) Tumor mutational burden and immune infiltration as independent predictors of response to neoadjuvant immune checkpoint inhibition in early TNBC in GeparNuevo. Ann Oncol 31:1216–1222. https://doi.org/10.1016/j.annonc.2020.05.015
Barroso-Sousa R, Trippa L, Lange P et al (2019) Nimbus: a phase II study of nivolumab plus ipilimumab in metastatic hypermutated HER2-negative breast cancer. J Clin Oncol 37:TPS1115–TPS1115. https://doi.org/10.1200/JCO.2019.37.15_SUPPL.TPS1115
McGrail DJ, Pilié PG, Rashid NU et al (2021) High tumor mutation burden fails to predict immune checkpoint blockade response across all cancer types. Ann Oncol 32:661–672. https://doi.org/10.1016/j.annonc.2021.02.006
Jiricny J (2006) (2006) The multifaceted mismatch-repair system. Nat Rev Mol Cell Biol 75(7):335–346. https://doi.org/10.1038/NRM1907
Bonneville R, Krook MA, Kautto EA et al (2017) Landscape of microsatellite instability across 39 cancer types. JCO Precis Oncol. https://doi.org/10.1200/po.17.00073
Vieira MLC, Santini L, Diniz AL, de Munhoz CF (2016) Microsatellite markers: what they mean and why they are so useful. Genet Mol Biol 39:312. https://doi.org/10.1590/1678-4685-GMB-2016-0027
Le DT, Uram JN, Wang H et al (2015) PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 372:2509–2520. https://doi.org/10.1056/nejmoa1500596
Prasad V, Kaestner V, Mailankody S (2018) Cancer drugs approved based on biomarkers and not tumor type—FDA approval of pembrolizumab for mismatch repair-deficient solid cancers. JAMA Oncol 4:157–158. https://doi.org/10.1001/JAMAONCOL.2017.4182
Andre T, Berton D, Curigliano G et al (2021) Safety and efficacy of anti–PD-1 antibody dostarlimab in patients (pts) with mismatch repair-deficient (dMMR) solid cancers: Results from GARNET study. J Clin Oncol 39:9–9. https://doi.org/10.1200/JCO.2021.39.3_SUPPL.9
Cheng AS, Leung SCY, Gao D et al (2020) Mismatch repair protein loss in breast cancer: clinicopathological associations in a large British Columbia cohort. Breast Cancer Res Treat 179:3–10. https://doi.org/10.1007/s10549-019-05438-y
Haricharan S, Bainbridge MN, Scheet P, Brown PH (2014) Somatic mutation load of estrogen receptor-positive breast tumors predicts overall survival: an analysis of genome sequence data. Breast Cancer Res Treat 146:211–220. https://doi.org/10.1007/s10549-014-2991-x
Kok M, Horlings HM, Snaebjornsson P et al (2017) Profound immunotherapy response in mismatch repair-deficient breast cancer. JCO Precis Oncol. https://doi.org/10.1200/po.17.00052
Fremd C, Hlevnjak M, Zapatka M et al (2019) Mismatch repair deficiency drives durable complete remission by targeting programmed death receptor 1 in a metastatic luminal breast cancer patient. Breast Care 14:53–59. https://doi.org/10.1159/000492580
Li A, Goodyear S, Fuss C, Mitri Z (2021) Exceptional response to pembrolizumab and trastuzumab in a heavily pretreated patient with HER2-positive TMB-H and MSI-H metastatic breast cancer. JCO Precis Oncol 5:904–909. https://doi.org/10.1200/PO.20.00361
Wang S, Jia M, He Z, Liu XS (2018) APOBEC3B and APOBEC mutational signature as potential predictive markers for immunotherapy response in non-small cell lung cancer. Oncogene 37:3924–3936. https://doi.org/10.1038/s41388-018-0245-9
Roberts SA, Lawrence MS, Klimczak LJ et al (2013) An APOBEC cytidine deaminase mutagenesis pattern is widespread in human cancers. Nat Genet 45:970–976. https://doi.org/10.1038/ng.2702
Lefebvre C, Bachelot T, Filleron T et al (2016) Mutational profile of metastatic breast cancers: a retrospective analysis. PLOS Med 13:e1002201. https://doi.org/10.1371/journal.pmed.1002201
Chumsri S, Sokol ES, Soyano-Muller AE et al (2020) Durable complete response with immune checkpoint inhibitor in breast cancer with high tumor mutational burden and APOBEC signature. JNCCN J Natl Compr Cancer Netw 18:517–521. https://doi.org/10.6004/jnccn.2020.7543
Dimarco AV, Qin X, Van Alsten S et al (2021) APOBEC mutagenesis inhibits breast cancer growth through induction of a T cell-mediated antitumor immune response. bioRxiv. https://doi.org/10.1101/2021.02.13.431068
Bertucci F, Ng CKY, Patsouris A et al (2019) Genomic characterization of metastatic breast cancers. Nature 569:560–564. https://doi.org/10.1038/s41586-019-1056-z
Mao Y, Lv M, Zhang Y et al (2020) APOBEC3B expression and its prognostic potential in breast cancer. Oncol Lett 19:3205–3214. https://doi.org/10.3892/ol.2020.11433
Kanu N, Cerone MA, Goh G et al (2016) DNA replication stress mediates APOBEC3 family mutagenesis in breast cancer. Genome Biol. https://doi.org/10.1186/s13059-016-1042-9
Huang RSP, Haberberger J, Severson E et al (2020) A pan-cancer analysis of PD-L1 immunohistochemistry and gene amplification, tumor mutation burden and microsatellite instability in 48,782 cases. Mod Pathol 342(34):252–263. https://doi.org/10.1038/s41379-020-00664-y
Goodman AM, Piccioni D, Kato S et al (2018) Prevalence of PDL1 amplification and preliminary response to immune checkpoint blockade in solid tumors. JAMA Oncol 4:1237–1244. https://doi.org/10.1001/JAMAONCOL.2018.1701
Gupta S, Vanderbilt CM, Cotzia P et al (2019) Next-generation sequencing-based assessment of JAK2, PD-L1, and PD-L2 copy number alterations at 9p24.1 in breast cancer: potential implications for clinical management. J Mol Diagn 21:307–317. https://doi.org/10.1016/J.JMOLDX.2018.10.006
Bachelot T, Filleron T, Dalenc F et al (2020) 128O PDL1/CD274 gain/amplification as a predictive marker of checkpoint blockade inhibitor efficacy in metastatic breast cancer: Exploratory analysis of the SAFIR02-IMMUNO randomized phase II trial. Ann Oncol 31:S58–S59. https://doi.org/10.1016/J.ANNONC.2020.03.231
Rayner E, van Gool IC, Palles C et al (2016) A panoply of errors: polymerase proofreading domain mutations in cancer. Nat Rev Cancer 162(16):71–81. https://doi.org/10.1038/nrc.2015.12
Wang F, Zhao Q, Wang Y-N et al (2019) Evaluation of POLE and POLD1 mutations as biomarkers for immunotherapy outcomes across multiple cancer types. JAMA Oncol 5:1504–1506. https://doi.org/10.1001/JAMAONCOL.2019.2963
Mittica G, Ghisoni E, Giannone G et al (2017) Checkpoint inhibitors in endometrial cancer: preclinical rationale and clinical activity. Oncotarget 8:90532–90544. https://doi.org/10.18632/ONCOTARGET.20042
Voutsadakis IA (2019) High tumor mutation burden and other immunotherapy response predictors in breast cancers: associations and therapeutic opportunities. Target Oncol 151(15):127–138. https://doi.org/10.1007/S11523-019-00689-7
Ayers M, Lunceford J, Nebozhyn M et al (2017) IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest 127:2930–2940. https://doi.org/10.1172/JCI91190
Damotte D, Warren S, Arrondeau J et al (2019) The tumor inflammation signature (TIS) is associated with anti-PD-1 treatment benefit in the CERTIM pan-cancer cohort. J Transl Med 17:357. https://doi.org/10.1186/s12967-019-2100-3
Danaher P, Warren S, Lu R et al (2018) Pan-cancer adaptive immune resistance as defined by the tumor inflammation signature (TIS): results from the cancer genome atlas (TCGA). J Immunother Cancer. https://doi.org/10.1186/s40425-018-0367-1
Ciruelos E, Pascual T, Chic N, et al (2021) Abstract OT-13-04: Solti-1716. Targeting non-luminal disease by PAM50 with pembrolizumab + paclitaxel in hormone receptor-positive/HER2-negative advanced/metastatic breast cancer patients who have progressed on or after CDK 4/6 inhibitor treatment (TATEN). In: Cancer Research. American Association for Cancer Research (AACR), p OT-13-04-OT-13-04
Brasó-Maristany F, Paré L, Chic N et al (2021) Gene expression profiles of breast cancer metastasis according to organ site. Mol Oncol 1878–0261:13021. https://doi.org/10.1002/1878-0261.13021
Cristescu R, Mogg R, Ayers M et al (2018) Pan-tumor genomic biomarkers for PD-1 checkpoint blockade–based immunotherapy. Science 362:3593. https://doi.org/10.1126/SCIENCE.AAR3593
Paré L, Pascual T, Seguí E et al (2018) Association between PD1 mRNA and response to anti-PD1 monotherapy across multiple cancer types. Ann Oncol 29:2121–2128. https://doi.org/10.1093/annonc/mdy335
Emens LA, Goldstein LD, Schmid P et al (2021) The tumor microenvironment (TME) and atezolizumab + nab-paclitaxel (A+nP) activity in metastatic triple-negative breast cancer (mTNBC): IMpassion130. J Clin Oncol 39:1006–1006. https://doi.org/10.1200/JCO.2021.39.15_SUPPL.1006
Burstein MD, Tsimelzon A, Poage GM et al (2015) Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clin Cancer Res 21:1688. https://doi.org/10.1158/1078-0432.CCR-14-0432
Bianchini G, Dugo M, Huang C-S et al (2021) LBA12 predictive value of gene-expression profiles (GEPs) and their dynamics during therapy in the NeoTRIPaPDL1 trial. Ann Oncol 32:S1283–S1284. https://doi.org/10.1016/J.ANNONC.2021.08.2084
Dieci MV, Griguolo G, Bisagni G et al (2021) 129P Integration of gene expression and tumor-infiltrating lymphocytes (TILs) to predict pCR after neoadjuvant chemotherapy and nivolumab for patients with luminal B-like breast cancer in the phase II GIADA trial. Ann Oncol 32:S414. https://doi.org/10.1016/J.ANNONC.2021.08.410
Wan JCM, Massie C, Garcia-Corbacho J et al (2017) Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer 17:223–238. https://doi.org/10.1038/nrc.2017.7
Cabel L, Proudhon C, Romano E et al (2018) Clinical potential of circulating tumour DNA in patients receiving anticancer immunotherapy. Nat Rev Clin Oncol 1510(15):639–650. https://doi.org/10.1038/S41571-018-0074-3
Lee JH, Long GV, Boyd S et al (2017) Circulating tumour DNA predicts response to anti-PD1 antibodies in metastatic melanoma. Ann Oncol 28:1130–1136. https://doi.org/10.1093/annonc/mdx026
Powles T, Assaf ZJ, Davarpanah N et al (2021) ctDNA guiding adjuvant immunotherapy in urothelial carcinoma. Nature 5957867(595):432–437. https://doi.org/10.1038/S41586-021-03642-9
Georgiadis A, Durham JN, Keefer LA et al (2019) Noninvasive detection of microsatellite instability and high tumor mutation burden in cancer patients treated with PD-1 blockade. Clin Cancer Res 25:7024–7034. https://doi.org/10.1158/1078-0432.CCR-19-1372
Gandara DR, Kowanetz M, Mok TSK, et al (2017) Blood-based biomarkers for cancer immunotherapy: tumor mutational burden in blood (bTMB) is associated with improved atezolizumab (atezo) efficacy in 2L1 NSCLC (POPLAR and OAK). Abstr B 42nd ESMO Congr (ESMO 2017) 8–12 Sept 2017, Madrid, Spain 28:v460. https://doi.org/10.1093/annonc/mdx380
Rizvi NA, Cho BC, Reinmuth N et al (2020) Durvalumab with or without tremelimumab vs standard chemotherapy in first-line treatment of metastatic non-small cell lung cancer: the MYSTIC phase 3 randomized clinical trial. JAMA Oncol 6:661–674. https://doi.org/10.1001/jamaoncol.2020.0237
Bratman SV, Yang SYC, Iafolla MAJ et al (2020) Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nat Cancer 1:873–881. https://doi.org/10.1038/s43018-020-0096-5
Zhang Q, Luo J, Wu S et al (2020) Prognostic and predictive impact of circulating tumor DNA in patients with advanced cancers treated with immune checkpoint blockade. Cancer Discov. https://doi.org/10.1158/2159-8290.cd-20-0047
Hieken T, ChenJ HT et al (2016) The microbiome of aseptically collected human breast tissue in benign and malignant disease. Sci Rep. https://doi.org/10.1038/SREP30751
Wang H, Altemus J, Niazi F et al (2017) Breast tissue, oral and urinary microbiomes in breast cancer. Oncotarget 8:88122–88138. https://doi.org/10.18632/ONCOTARGET.21490
Xuan C, Shamonki J, Chung A et al (2014) Microbial dysbiosis is associated with human breast cancer. PLoS ONE. https://doi.org/10.1371/JOURNAL.PONE.0083744
Gopalakrishnan V, Spencer CN, Nezi L et al (2018) Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359:97–103. https://doi.org/10.1126/SCIENCE.AAN4236
Sivan A, Corrales L, Hubert N et al (2015) Commensal bifidobacterium promotes antitumor immunity and facilitates anti–PD-L1 efficacy. Science 350:1084. https://doi.org/10.1126/SCIENCE.AAC4255
Blank CU, Haanen JB, Ribas A, Schumacher TN (2016) The “cancer immunogram.” Science 352:658–660. https://doi.org/10.1126/SCIENCE.AAF2834
Acknowledgements
This study has received funding from Generalitat de Catalunya Peris PhD4MD 2019 SLT008/18/00122 (to N.C.), Fundación Científica Asociación Española Contra el Cáncer AECC_Postdoctoral17-1062 (to F.B-M.).
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.P. reports advisory and consulting fees from Roche, Pfizer, Novartis, Amgen, BMS, Puma, Oncolytics Biotech, MSD, Guardant Health, Peptomyc and Lilly, lecture fees from Roche, Pfizer, Novartis, Amgen, BMS, Nanostring Technologies and Daiichi Sankyo, institutional financial interests from Boehringer, Novartis, Roche, Nanostring, Sysmex Europa GmbH, Medica Scientia inno. Research, SL, Celgene, Astellas and Pfizer; a leadership role in Reveal Genomics, SL; and a patent PCT/EP2016/080056.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chic, N., Brasó-Maristany, F. & Prat, A. Biomarkers of immunotherapy response in breast cancer beyond PD-L1. Breast Cancer Res Treat 191, 39–49 (2022). https://doi.org/10.1007/s10549-021-06421-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06421-2