Abstract
Purpose
To explore the feasibility, adherence, safety and potential efficacy of Every Day Counts; a randomized pilot trial designed for women with metastatic breast cancer (MBC) framed by the American Cancer Society nutrition and physical activity (PA) guidelines
Methods
Women with clinically stable MBC were recruited to complete an interview, dual energy X-ray absorptiometry imaging and phlebotomy at baseline and post-intervention. Multidimensional quality of life, symptom burden, lifestyle behaviors (nutrition and PA) and biomarkers of prognosis were procured and quantified. Women were randomized to the immediate intervention or a waitlist control arm. The 12-week intervention included a curriculum binder, lifestyle coaching (in-person and telephone-based sessions) and intervention support (activity monitor, text messaging, cooking classes.) Women in the waitlist control were provided monthly text messaging.
Results
Forty women were recruited within 9 months (feasibility). Women in the immediate intervention attended 86% of all 12 weekly coaching sessions (adherence) and showed significant improvements in general QOL (p = 0.001), and QOL related to breast cancer (p = 0.001), endocrine symptoms (p = 0.002) and fatigue (p = 0.037), whereas the waitlist control did not (all p values ≥ 0.05) (efficacy). PA significantly increased for women in the intervention compared to control (p < 0.0001), while dietary changes were less evident across groups due to high baseline adherence. No significant changes in biomarkers or lean mass were noted, yet visceral adipose tissue declined (p = 0.001). No intervention-related injuries were reported (safety). Qualitative feedback strongly supports the desire for a longer intervention with additional support.
Conclusions
Lifestyle interventions are of interest, safe and potentially beneficial for women with MBC. A larger trial is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in the treatment and management of early stage breast cancer (BC), ~ 20–30% of the 3 million US patients with BC will develop metastatic disease, signifying BC spread to the bone, liver, lung and other distal locations [1]. Additionally, 6–10% (13,776–22,096) of women with metastatic breast cancer (MBC) present with de novo disease, reflecting distal BC metastases at the time of initial diagnosis. Recent analyses highlight de novo disease is increasing among women aged 25–39, particularly non-Hispanic white and African-Americans (AA) [2]. Due to the integration and expansion of targeted therapies, the median survival for women with recurrent and de novo MBC has increased substantially [3,4,5,6,7,8]. In fact, the number of women living with MBC has doubled in the last decade [7]. Nevertheless, there is an on-going perception that the majority of these women struggle with weight loss, cancer cachexia and frailty, which is often inaccurate for many living with this disease. Although symptom burden is a challenge, numerous women with MBC frequently endorse complaints of weight gain and general physical deconditioning associated with on-going anti-neoplastic treatments [9].
Breast cancer treatment is associated with adverse body composition changes, specifically gains in adipose tissue and reductions in strength and lean mass (LM; also known as skeletal muscle) [10, 11]. No clear consensus exists on the etiology of these changes; however, BC treatment, lifestyle habits and menopausal status, likely in combination, are all implicated [10]. Excess adiposity contributes to inflammation and insulin-resistance, which are theorized to promote tumor progression and loss of LM [12, 13]. Low levels of LM are associated with chemotherapy toxicity, increased symptom burden, and compromised survival in women with MBC [14, 15]. For women with early-stage BC, health behavior changes targeting reductions in adiposity and/or increases in muscle strength and LM lead to improvements in QOL and symptom reports, as well as prognostic changes serum biomarkers [16,17,18,19,20], mitochondrial function [21] and potentially novel microRNA [22]. Thus, interventions promoting favorable body composition changes would likely have numerous benefits for women with MBC, yet this remains largely unexplored. Typically, women with MBC are excluded from nutrition and/or PA intervention trials under the assumptions that: (1) exercise could be unsafe or pose additional burdens, (2) changes in lifestyle habits would have little impact on quality of life (QOL) or disease trajectory, or (3) women with MBC lack interest in such trials. We designed Every Day Counts to challenge and test these assumptions, hypothesizing women would demonstrate trends for improvements in QOL and lean mass.
Methods
Study design
Every Day Counts (EDC) was a 12-week randomized, waitlist controlled trial designed primarily to evaluate the feasibility, adherence and safety of an intervention promoting the American Cancer Society (ACS) nutrition and physical activity (PA) guidelines [23] in women with clinically stable MBC. Our secondary objective was to assess its short-term impact on patient reported outcomes and physical performance. We also explored biomarkers of inflammation, mitochondrial function and conducted a nested study to examine the additive benefits of extending the intervention to 16-weeks. Informed by our developmental work [9], EDC reflected essential adaptations of our previously successful lifestyle interventions [24,25,26,27,28] in a novel population. The ethical review board of the Medical College of Wisconsin (MCW) and other participating institutions reflective of the investigative team approved this study. This trial was registered on clinicaltrials.gov (NCT03824145.)
Patient population and recruitment
To participate, adult (≥ 18 years) females with histologically confirmed MBC had to be deemed clinically stable by their medical oncologist defined as follows: anticipated life expectancy of at least ≥ 12 months, no unintentional weight loss, no new symptoms or change in performance status (ECOG 0–1) for the past 30 days, no clinical (including laboratory) or radiologic evidence of disease progression (past 30 days), no changes in anti-neoplastic therapies (previous or anticipated next 30 days), and no reports of severe pain precluding practical and safe participation (≥ Grade 3 per the NCI CTCAE)] [29]. In addition, women were required to have access to a mobile phone with unlimited text messaging, able to participate in moderate PA and strength training, and non-compliant with the ACS nutrition and PA recommendations (i.e., consuming < 5 fruits and vegetables/day, ≤ 90 min/week moderate exercise (which allows for progress to 150 min/week), and/or < twice/week of resistance exercise training (RET).) Women with < 12 months of life anticipated, receiving appetite stimulants and/or steroids were not approached. Women not medically cleared by their oncologist or already adherent to the ACS lifestyle guidelines were ineligible. Recruitment methods included letters sent to directly to women with MBC describing the program and oncologist/nurse referrals within the cancer center. To support a broader inclusion of women, members of the community advisory board were encouraged to use ‘word of mouth’ recruiting. Further, brochures and/or study advertisements were sent to medical oncologists at local community hospitals and EDC was promoted on targeted social media outlets (non-public Facebook breast cancer support groups) in the greater Milwaukee, WI area.
Randomization
Following the baseline interview and using a random digit generator, women were randomized to the immediate intervention or waitlist control group. Randomization allocation was stored and maintained in a secured password protected server. To ensure blinding, only the biostatistician and project coordinator had access; data collectors (phlebotomy, questionnaire, diet) and investigators did not.
Every Days Counts intervention
EDC was a 12-week behavioral intervention rooted in social cognitive theory (SCT) addressing adoption of the ACS nutrition and PA guidelines for cancer survivors, including: (1) consumption of whole grains and 5+ fruits and vegetables daily, and (2) engagement in a minimum of 150 min of moderate PA and 2 sessions of resistance exercise training (RET)/week. A certified, licensed athletic trainer (LAT, ATC, CES) experienced in lifestyle counseling spearheaded: (1) four supervised aerobic/RET sessions, (2) weekly individual telephone sessions based on the EDC program intervention manual; and (3) intervention support. Attendance at each scheduled (in person or telephone session) was tracked. If the participant failed to show up (in person or telephone session) and did not respond to text or voicemail to reschedule, this was deemed a “no show” and used to assess adherence.
Prior to session 1, the coach created an RET program tailored to the participant’s strength. Using the baseline physical assessment data and guided by normative scores for strength [30, 31], the health coach recommended upper and lower extremity and core exercises based on a predetermined list of activities targeting these areas (e.g. curls, squats, lunges, planks.) At the first supervised intervention session, the health coach delivered the EDC program binder, reviewed program structure, and provided nutrition education and PA/RET guidance tailored to the participant’s perceived level of conditioning. The EDC binder addressed knowledge (e.g., plant-based eating), attitudes (e.g., understanding barriers and facilitators to healthy eating and PA), and behavioral strategies (e.g., self-monitoring) (Table 1). The EDC binder also contained recipes, a plant-based eating and PA self-monitoring form, and other materials to support adherence, reinforcement and review. Telephone sessions began with information on the weekly theme, discussion of previous week’s achievements and challenges, a review of adherence using nutrition and PA tracking, and setting one SMART weekly goal for nutrition and one for PA/RET. The supervised exercise portion included: (1) guiding participant in her choice of appropriate modes of moderate PA to work toward engaging in 30 min most days of the week (e.g., walking, biking), (2) assessing proper type and intensity of RET for safe conditioning, and (3) instructing and observing participants in the correct execution of RET. RET exercise using appropriately prescribe exercise bands were progressed individually by altering load (reps/set) or band (resistance), using a combination of participant feedback (e.g., “feels too easy,” “not challenging”), consistency of program adherence via verbal feedback and data from the tracking device. Guidance was also provided on endurance activities (e.g., increasing step goals or time spent walking.)
In support of self-monitoring and intervention adherence, participants received a Fitbit™ activity tracker (Charge or Charge HR), exercise bands, cooking utensils and twice weekly text messages (weeks 1–12) focused on self-efficacy, outcomes expectations, social support and/or resources or self-monitoring tools. These strategies were successfully applied in our previous lifestyle interventions [32, 33]. Women were also provided the opportunity to attend three interactive cooking classes focused on simple plant-based meals (1 salad, 1 side dish, 1 main course). These group classes, held at a community location, served to: increase skills and comfort with preparing plant-based meals and promote dietary adherence [34].
Every Day Counts waitlist control
Participants in the waitlist control group received a monthly text message thanking them for their participation in the study and reminding them of their intervention start. Following the 12-week waitlist control period, women in this group were offered the intervention and all supportive materials. This design was selected based on critical feedback from a community advisory board, who strongly believed all women should have access to the intervention.
Data collection
At baseline (prior to randomization) and post-intervention (12-weeks) two 60-min assessments were completed, involving: (1) an interview and (2) physical measurements (dual energy X-ray absorptiometry [DXA], strength, anthropometrics) and phlebotomy. During the interview, women completed questionnaires quantifying QOL (Functional Assessment of Cancer Therapy—Breast [FACT-B] [35]), symptom burden (fatigue [36], pain [37, 38], sleep [39], mood [40]) and lifestyle factors (Godin leisure time exercise [41], stress [42], self-efficacy [43], social support [35]). Physical measures included standardized measures of weight and height to calculate BMI (weight [kg]/height [m]2.) Body composition (adipose and lean mass) were measured by DXA (GE Lunar Medical Systems, enCORE software version 14.10.022.) Whole body scans were performed and analyzed by a trained technician blind to study group or outcomes, following calibration with the manufacturer’s phantom. Visceral fat mass was estimated from the android region; a region of interest automatically defined using the methods of Kaul et al. [44] Three 24-h diet recalls (24DR) were completed in person and/or via telephone by the MCW CTSI Registered Dietitian using the 5-pass methodology within the week of interview [45]. Dietary data were collected and entered into Nutrition Data System for Research to detect changes in target dietary intake patterns (i.e., F/V, red meat, alcohol.) [46]. Handgrip dynamometry (Jamar Plus handgrip) was completed for all participants following standard study procedures [47]. Other physical performance measures were completed in a subset of participants (e.g., sit to stand, bicep curls, calf raises, planks.) Blood biospecimens were acquired after an overnight fast to profile inflammatory biomarkers implicated in carcinogenesis (e.g., C-reactive protein (CRP), interleukin-6, tumor necrosis factor). Samples were sent immediately to assess mitochondrial function (Seahorse XF Analyzer, Agilent, CA) or processed and stored at − 80 °C until the time of batch analyses (Eve Technologies, Calgary, AB. Canada). For purposes of this project, spare respiratory capacity (a measurement of mitochondrial integrity and energetics) was considered a representative parameter of overall mitochondrial health.
Statistical analyses
Descriptive statistics were reported for all outcomes of interest at baseline and 12 weeks, including QOL, symptoms, body composition and lifestyle behaviors by group. We defined feasibility as meeting 100% of our recruitment goal, adherence as attending at least 75% of telephone coaching sessions and 2/3 exercise training sessions, and efficacy as evidenced by trends in improvements QOL for women in the intervention vs. the control groups. To assess safety, adverse events (i.e., intervention-related injuries) were monitored throughout the study period. Linear mixed models with an interaction term to account for differences in trend over time between groups and a random effect to account for correlation of repeated measures within each woman were used to assess each outcome. Compound symmetry covariance structures were assumed for the correlation from the same woman across time. Statistical significance of the difference between outcomes for the immediate and waitlist control groups were from the interaction term and the within group comparisons used the corresponding contrasts terms. No formal power calculations were conducted a priori; 40 women were recruited taking into consideration the duration of the parent study and to demonstrate feasibility. A significance level of 0.05 was used and statistical analysis was performed using SAS v9.4 (SAS Institute, Cary, NC).
Results
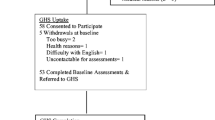
A total of 78 women were screened and 40 women were consented in 9 months (January–September, 2018.) Written letters or referrals from oncologists provided the greatest participant yields (n = 34/40), followed by our community engagement efforts (n = 6/40). Thirty-five women completed the 12-week study contributing evaluable data. (Fig. 1) On average, participants were: 55 years of age (± 12), white (91%), employed full-time (32%), retired or on disability (68%), had bone (63%), liver (26%) or lung metastases (26%), and were 3.6 (± 3.2) years after MBC diagnoses. Overall attendance was 86% during the 12-week intervention: 93% for in-person sessions and 84% for telephone sessions. No adverse events (injuries related to the intervention) occurred; however, three of the women (2 Intervention, 1 Waitlist control) developed new symptoms/disease progression during the study, something expected given the unpredictable nature of MBC.
In line with our secondary objective, we evaluated patient reported outcomes, with an intentional focus on QOL (Table 2). Using the FACT-General, significant increases in QOL were reported between groups (p = 0.003) and for women in the intervention group (p = 0.001), which were largely driven by improvements in physical (p = 0.003), emotional (p = 0.01) and functional well-being (p = 0.06). When we examined symptoms unique to BC and endocrine treatment, only women in the intervention arm reported significant within group improvements for BC (p = 0.001) and Endocrine symptoms (p = 0.002), whereas. women in the waitlist control did not (p = 0.356 and p = 0.450, respectively.) Fatigue improved for women in the intervention group (p = 0.037), but not between groups (p = 0.107). Findings related to mood were mixed. Significant declines in depression were noted between groups (p = 0.03) and for women in the intervention (p = 0.010), yet anxiety and perceived stress significantly declined for all women, regardless of group (all p values < 0.05).
By design, this was not a weight-loss study; thus, declines in body weight or BMI were not observed. Trends in energy intake declined for women in the intervention and increased for those in the waitlist control, yet these differences were not statistically different within or between groups (Table 3). Although improvements in body composition were targeted, no significant changes between or within groups were noted for fat or lean mass. Visceral fat mass decreased between and within all groups (all p values < 0.05), however. Using applicable DXA cut points, 20% (n = 7) and 14% (n = 5) of women were classified as sarcopenic pre vs. post-intervention, respectively (p = 0.938); none of these women had obesity. Considering sarcopenia is ideally defined as compromises in lean mass and strength [48], the significant increases in handgrip strength for women in the intervention (p = 0.002) vs. waitlist control (p = 0.163) were deemed clinically meaningful. The Godin results support women in the intervention spent significantly more time engaged in PA pre vs. post-intervention (p < 0.001), which was significantly different compared to those in the waitlist control (p < 0.001).
We leveraged this pilot study to address concerns related to the length of the EDC intervention and to explore potentially important serum and cellular changes in a novel population. Specifically, we extended the EDC intervention to 16 weeks for women in the waitlist control who were interested (n = 14) to see if they derived additional benefit compared to women who completed the 12-week intervention. QOL results were similar; however, women in the 16-week program displayed more favorable, non-significant trends for lean mass gain, fat mass loss, and biomarker changes and significantly greater increases in strength (sit to stands, planks, bicep curls.) Due to unforeseen challenges regarding the analyses of blood biospecimens, we did not have complete data on all participants pre vs. post-intervention. We also encountered issues with the timely transport of blood biospecimens and reliable machinery, and thus, we were only able to explore mitochondrial function at in a subset of women (n = 12). Spare respiratory capacity increased by a mean 69.7% (± 165.6, p = 0.24), signifying important cellular changes in muscle functioning associated with intervention participation.
Discussion
Every Day Counts was implemented following our developmental work in a small group of women with MBC who provided novel insights on the unmet needs of this population [9]. Our present pilot study results support: (1) feasibility as evidenced by participant interest (78 women contacted and screened) and 100% of our enrollment goal (n = 40 in 9 months vs. our projected 15 months); (2) adherence as evidenced by 86% of women completing all 12 coaching sessions (84% of telephone and 93% in-person sessions) and documentation of improved exercise and dietary behaviors; and (3) potential efficacy as evidenced by significant improvements in QOL. These pilot findings also reinforce the safety of a dietary and PA intervention in this population. Given the common prevalence of bone metastases in women with MBC, the lack of intervention-related injuries is clinically important. Further, our preliminary findings reinforce the impact of lifestyle behaviors on QOL and symptom burden; key somatic reports with potential to complement and support treatment tolerance.
A variety of methods are available to quantify changes in QOL; however, we specifically chose the FACT tools because they afforded us the opportunity to directly compare our findings to a similar patient population. In doing so, we discovered our participants’ baseline scores for physical, social, emotional and functional well-being were higher compared to a larger, more heterogeneous sample of women with MBC [49], but below those for physical, social and functional well-being when compared to a normative sample compromised largely of women with early stage BC [50]. Considering our participants were required to be clinically stable and not near the end of life, these findings are not surprising. Interestingly, intervention participants reported significant improvements in physical well-being post-intervention achieving scores on par with those in the normative sample (22.7 vs. 22.1, respectively.) [50]. We suspect these increases were partially driven by clinically significant improvements in fatigue (> 3 points) [51]. Studies in women with early-stage BC support the positive and sustained impact of lifestyle (nutrition and/or PA) interventions on QOL and other BC-specific outcomes [20, 52,53,54,55,56]. Only a few studies focus on women with MBC. In an early study by Headly et al., these investigators demonstrated that a seated exercise intervention in women with MBC initiating chemotherapy significantly reduced fatigue and slowed decline in total and physical well-being scores [57]. More recently, Jones [58] and Yee [59] showed that women with MBC have reduced cardiopulmonary functioning and lower aerobic fitness, reduced muscular strength and less daily PA compared to healthy controls. Combining 20 patients with bone metastases from prostate and BC, Cormie et al. showed improvements in functional ability, lean mass and QOL at 3- and 6-months following a supervised resistance exercise trial [60]. However, two recent studies conducted exclusively in women with MBC reported high dropout rates and no significant differences in QOL for interventions focused solely on aerobic exercise [61, 62]. Our data support women in the Every Day Counts intervention exhibited statistically and clinically meaningful increases in overall (FACT-G; 3–7 points) [63] and disease-specific (FACT-Breast; 2–3 points) [63] QOL. They also increased their PA levels from ‘insufficiently active’ to ‘active,’ whereas women in the waitlist control remained ‘moderately active,’ albeit on the lower end of this interpretive scale [64]. Together, these data highlight the complexities of this population and emphasize the need for carefully structured programs to achieve positive outcomes.
Body composition is gaining increasing recognition as an important tissue biomarker predictive of prognosis and treatment tolerance in women with early [65] and late stage BC [14, 15, 66]. Using archived abdominal computed tomography (CT) images conducted for clinical purposes, Prado [14] and Shachar [15] quantified body composition in women with MBC. Results support women with MBC who are classified as sarcopenic more often experience shorter time to tumor progression and treatment toxicities [14], hospitalization, dose-reductions and dose delays [15], compared to women without sarcopenia. Within EDC, the prevalence of sarcopenia was 20% (n = 7/35) at baseline without new incident cases post-intervention (using DXA.) We anticipated that increases in PA with twice weekly RET would result in decreased DXA-detected sarcopenia. However, while increases in strength were observed, we also observed overall decreases in lean mass in the intervention and waitlist control groups. These findings are in stark contrast to Cormie et al. who had a similar intervention window (3 months), twice weekly RET and reported significant gains in LM, albeit in a mixed population of metastatic breast (n = 3) and prostate cancer (n = 17) survivors [60]. During the initial design of EDC, we contemplated the potential impact of a 12- vs. 16-week intervention on body composition. Based on the work of Cormie [60], Capozzi [67] and Lonbro et al. [68], 12 weeks of RET seemed a sufficient window to observe lean mass gains. Because these studies did not target women with MBC, we conducted a nested study within this EDC pilot to extend the 12-week intervention by 4 weeks for waitlist control participants. The nested study findings support more favorable changes in body composition, physical performance and biomarker trends. Accompanied by the qualitative feedback from our participants, we advocate a 16-week lifestyle intervention to better meet the quantitative endpoints and desires of this population.
Although this study was methodologically rigorous in design and tailored to meet the perceived needs of this population, it is not without limitations. First, we lacked sufficient measures to comprehensively evaluate changes in physical performance. Due to its ease and acceptability, we collected handgrip strength for all participants; however, we failed to consider other field measures to capture changes in other muscle groups until later in the study providing us with results for only a subset of participants. Additionally, we did not include validated methods to evaluate exercise intensity or cardiorespiratory fitness. Second, our study sample is not representative of all women with MBC. By design, we targeted women capable of healthy eating and PA; thus, our sample may be ‘healthier’ and reflects an inherent selection bias in studies of this nature. Further, although we met 100% of our recruitment goal, we did not adequately engage minority participants. Additional community engagement efforts are needed. Third, our attempts to explore biomarkers of inflammation failed to demonstrate meaningful change. Given our small sample size, we suspect some of this may be due to a Type II error. Finally, feedback from our participants highlighted the need for more information on dietary change strategies and safety guidelines for RET with bone metastases. Interestingly, our exploratory analyses reveal moderate to high adherence to several of the dietary components of the ACS guidelines at baseline for all participants (data not shown); thus, it would be difficult to show significant improvements. Regardless, targeted messaging regarding increasing whole grains and reducing alcohol consumption, along with cooking resources (video links, more plant-based recipes) provide opportunities for further benefit. In addition, reassurance that RET is a safe and recommended treatment modality for treated and medically stable bone metastasis [60, 69] should have been shared earlier in the intervention to help support the need for more frequent and higher load RET to see LM gains.
Conclusions
The design and implementation of Every Day Counts was informed by women with MBC; a growing group of cancer survivors for whom we have limited evidence to guide their lifestyle choices. Results from this pilot highlight the interests, capabilities and importantly, the safety of a nutrition and PA intervention in women with clinically stable MBC, providing strong evidence to support favorable improvements in QOL and symptom burden. A larger trial targeting a more diverse group of women (racial/ethnic, rural, community) and adequately powered to explore the mechanistic pathways between QOL and lifestyle behaviors is warranted.
References
O’Shaughnessy J (2005) Extending survival with chemotherapy in metastatic breast cancer. Oncologist 10(Suppl 3):20–29. https://doi.org/10.1634/theoncologist.10-90003-20
Johnson RH, Chien FL, Bleyer A (2013) Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. JAMA J Am Med Assoc 309(8):800–805. https://doi.org/10.1001/jama.2013.776
Stebbing J, Copson E, O’Reilly S (2000) Herceptin (trastuzamab) in advanced breast cancer. Cancer Treat Rev 26(4):287–290. https://doi.org/10.1053/ctrv.2000.0182
Hortobagyi GN (2001) Overview of treatment results with trastuzumab (Herceptin) in metastatic breast cancer. Semin Oncol 28(6 Suppl 18):43–47
Alexander W (2014) American association for cancer research and American psychiatric association. P T 39(6):448–452
Swain SM, Kim SB, Cortes J, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Knott A, Clark E, Ross G, Benyunes MC, Baselga J (2013) Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol 14(6):461–471. https://doi.org/10.1016/S1470-2045(13)70130-X
Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M (2017) Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol Biomarkers Prev 26(6):809–815. https://doi.org/10.1158/1055-9965.EPI-16-0889
Caswell-Jin JL, Plevritis SK, Tian L, Cadham CJ, Xu C, Stout NK, Sledge GW, Mandelblatt JS, Kurian AW (2018) Change in survival in metastatic breast cancer with treatment advances: meta-analysis and systematic review. JNCI Cancer Spectr 2(4):pky062. https://doi.org/10.1093/jncics/pky062
Sheean P, Kabir C, Rao R, Hoskins K, Stolley M (2015) Exploring diet, physical activity, and quality of life in females with metastatic breast cancer: a pilot study to support future intervention. J Acad Nutr Diet 115(10):1690–1698. https://doi.org/10.1016/j.jand.2015.03.017
Sheean PM, Hoskins K, Stolley M (2012) Body composition changes in females treated for breast cancer: a review of the evidence. Breast Cancer Res Treat 135(3):663–680. https://doi.org/10.1007/s10549-012-2200-8
Christensen JF, Jones LW, Andersen JL, Daugaard G, Rorth M, Hojman P (2014) Muscle dysfunction in cancer patients. Ann Oncol 25(5):947–958. https://doi.org/10.1093/annonc/mdt551
Berrino F, Villarini A, Traina A, Bonanni B, Panico S, Mano MP, Mercandino A, Galasso R, Barbero M, Simeoni M, Bassi MC, Consolaro E, Johansson H, Zarcone M, Bruno E, Gargano G, Venturelli E, Pasanisi P (2014) Metabolic syndrome and breast cancer prognosis. Breast Cancer Res Treat 147(1):159–165. https://doi.org/10.1007/s10549-014-3076-6
Battaglini CL, Hackney AC, Goodwin ML (2012) Cancer cachexia: muscle physiology and exercise training. Cancers (Basel) 4(4):1247–1251. https://doi.org/10.3390/cancers4041247
Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, Mackey JR, Koski S, Pituskin E, Sawyer MB (2009) Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res 15(8):2920–2926. https://doi.org/10.1158/1078-0432.CCR-08-2242
Shachar SS, Deal AM, Weinberg M, Nyrop KA, Williams GR, Nishijima TF, Benbow JM, Muss HB (2017) Skeletal muscle measures as predictors of toxicity, hospitalization, and survival in patients with metastatic breast cancer receiving taxane-based chemotherapy. Clin Cancer Res 23(3):658–665. https://doi.org/10.1158/1078-0432.CCR-16-0940
Courneya KS, Segal RJ, Mackey JR, Gelmon K, Reid RD, Friedenreich CM, Ladha AB, Proulx C, Vallance JK, Lane K, Yasui Y, McKenzie DC (2007) Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol 25(28):4396–4404. https://doi.org/10.1200/JCO.2006.08.2024
Demark-Wahnefried W, Kenyon AJ, Eberle P, Skye A, Kraus WE (2002) Preventing sarcopenic obesity among breast cancer patients who receive adjuvant chemotherapy: results of a feasibility study. Clin Exerc Physiol 4(1):44–49
Mefferd K, Nichols JF, Pakiz B, Rock CL (2007) A cognitive behavioral therapy intervention to promote weight loss improves body composition and blood lipid profiles among overweight breast cancer survivors. Breast Cancer Res Treat 104(2):145–152. https://doi.org/10.1007/s10549-006-9410-x
Schmitz KH, Ahmed RL, Hannan PJ, Yee D (2005) Safety and efficacy of weight training in recent breast cancer survivors to alter body composition, insulin, and insulin-like growth factor axis proteins. Cancer Epidemiol Biomark Prev 14(7):1672–1680. https://doi.org/10.1158/1055-9965.EPI-04-0736
Zick SM, Colacino J, Cornellier M, Khabir T, Surnow K, Djuric Z (2017) Fatigue reduction diet in breast cancer survivors: a pilot randomized clinical trial. Breast Cancer Res Treat 161(2):299–310. https://doi.org/10.1007/s10549-016-4070-y
Mijwel S, Cardinale DA, Norrbom J, Chapman M, Ivarsson N, Wengstrom Y, Sundberg CJ, Rundqvist H (2018) Exercise training during chemotherapy preserves skeletal muscle fiber area, capillarization, and mitochondrial content in patients with breast cancer. FASEB J 32(10):5495–5505. https://doi.org/10.1096/fj.201700968R
Adams BD, Arem H, Hubal MJ, Cartmel B, Li F, Harrigan M, Sanft T, Cheng CJ, Pusztai L, Irwin ML (2018) Exercise and weight loss interventions and miRNA expression in women with breast cancer. Breast Cancer Res Treat 170(1):55–67. https://doi.org/10.1007/s10549-018-4738-6
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):243–274. https://doi.org/10.3322/caac.21142
Stolley M, Sheean P, Gerber B, Arroyo C, Schiffer L, Banerjee A, Visotcky A, Fantuzzi G, Strahan D, Matthews L, Dakers R, Carridine-Andrews C, Seligman K, Springfield S, Odoms-Young A, Hong S, Hoskins K, Kaklamani V, Sharp L (2017) Efficacy of a weight loss intervention for African American breast cancer survivors. J Clin Oncol 35(24):2820–2828. https://doi.org/10.1200/JCO.2016.71.9856
Stolley MR, Sharp LK, Fantuzzi G, Arroyo C, Sheean P, Schiffer L, Campbell R, Gerber B (2015) Study design and protocol for moving forward: a weight loss intervention trial for African-American breast cancer survivors. BMC Cancer 15(1):1018. https://doi.org/10.1186/s12885-015-2004-4
Sheean P, Liang H, Schiffer L, Arroyo C, Stolley M (2017) Examining the prevalence of metabolic syndrome among overweight/obese African-American breast cancer survivors vs. matched non-cancer controls. J Cancer Surviv 11(1):102–110. https://doi.org/10.1007/s11764-016-0566-z
Sheean P, Liang H, Schiffer L, Arroyo C, Troy K, Stolley M (2015) Assessing the prevalence of compromised bone health among overweight and obese African-American breast cancer survivors: a case-control study. J Cancer Surviv. https://doi.org/10.1007/s11764-015-0448-9
Springfield S, Odoms-Young A, Tussing-Humphreys LM, Freels S, Stolley MR (2019) A step toward understanding diet quality in urban African-American breast cancer survivors: a cross-sectional analysis of baseline data from the moving forward study. Nutr Cancer 71(1):61–76. https://doi.org/10.1080/01635581.2018.1557217
Institute NC (2017) Common terminology criteria for adverse events. Version 5.0
Applebaum EV, Breton D, Feng ZW, Ta AT, Walsh K, Chassé K, Robbins SM (2017) Modified 30-second Sit to Stand test predicts falls in a cohort of institutionalized older veterans. PLoS One 12(5):e0176946. https://doi.org/10.1371/journal.pone.0176946
Rikli RE, Jones CJ (2013) Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 53(2):255–267. https://doi.org/10.1093/geront/gns071
Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML (2009) Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informat J 15(1):17–25. https://doi.org/10.1177/1460458208099865
Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, Van Horn L, Dyer A (2009) Obesity Reduction Black Intervention Trial (ORBIT): six-month results. Obesity 17(1):100–106
Greenlee H, Gaffney AO, Aycinena AC, Koch P, Contento I, Karmally W, Richardson JM, Lim E, Tsai WY, Crew K, Maurer M, Kalinsky K, Hershman DL (2015) Inverted exclamation markCocinar Para Su Salud!: randomized controlled trial of a culturally based dietary intervention among Hispanic breast cancer survivors. J Acad Nutr Diet 115(5 Suppl):S42–S56 e3. https://doi.org/10.1016/j.jand.2015.02.027
Sherbourne CD, Stewart AL (1991) The MOS social support survey. Soc Sci Med 32(6):705–714
Cella D, Lai JS, Chang CH, Peterman A, Slavin M (2002) Fatigue in cancer patients compared with fatigue in the general United States population. Cancer 94(2):528–538. https://doi.org/10.1002/cncr.10245
Amtmann D, Cook KF, Jensen MP et al (2010) Development of a PROMIS item bank to measure pain interference. Pain 150(1):173–182
Revicki DA, Cook KF, Amtmann D, Harnam N, Chen WH, Keefe FJ (2014) Exploratory and confirmatory factor analysis of the PROMIS pain quality item bank. Qual Life Res 23(1):245–255
Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 45(1):5–13
Herrmann C (1997) International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical results. J Psychosom Res 42(1):17–41
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10(3):141–146
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396
Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR (1987) The development of scales to measure social support for diet and exercise behaviors. Prev Med 16(6):825–836
Kaul S, Rothney MP, Peters DM, Wacker WK, Davis CE, Shapiro MD, Ergun DL (2012) Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity (Silver Spring) 20(6):1313–1318. https://doi.org/10.1038/oby.2011.393
Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ (2003) Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr 77(5):1171–1178
NIH National Cancer Institute Dietary Assessment Primer. National Cancer Institute (2019). https://dietassessmentprimer.cancer.gov/approach/table.html#intake
Toolbox N (2012) Performing hand grip strength measures. NIH. http://www.nihtoolbox.org/WhatAndWhy/Motor/Strength/NIH%20Toolbox%20Grip%20Strength%20Test/Pages/default.aspx. Accessed 16 March 2016
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinkova E, Vandewoude M, Zamboni M (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing 39(4):412–423. https://doi.org/10.1093/ageing/afq034
Reed E, Simmonds P, Haviland J, Corner J (2012) Quality of life and experience of care in women with metastatic breast cancer: a cross-sectional survey. J Pain Symptom Manag 43(4):747–758. https://doi.org/10.1016/j.jpainsymman.2011.05.005
Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, Deasy S, Cobleigh M, Shiomoto G (1997) Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 15(3):974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Cella D, Eton DT, Lai JS, Peterman AH, Merkel DE (2002) Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manag 24(6):547–561. https://doi.org/10.1016/s0885-3924(02)00529-8
Mandelblatt JS, Luta G, Kwan ML, Makgoeng SB, Ergas IJ, Roh JM, Sternfeld B, Adams-Campbell LL, Kushi LH (2011) Associations of physical activity with quality of life and functional ability in breast cancer patients during active adjuvant treatment: the Pathways Study. Breast Cancer Res Treat 129(2):521–529. https://doi.org/10.1007/s10549-011-1483-5
Swisher AK, Abraham J, Bonner D, Gilleland D, Hobbs G, Kurian S, Yanosik MA, Vona-Davis L (2015) Exercise and dietary advice intervention for survivors of triple-negative breast cancer: effects on body fat, physical function, quality of life, and adipokine profile. Support Care Cancer. https://doi.org/10.1007/s00520-015-2667-z
Goodwin PJ, Segal RJ, Vallis M, Ligibel JA, Pond GR, Robidoux A, Blackburn GL, Findlay B, Gralow JR, Mukherjee S, Levine M, Pritchard KI (2014) Randomized trial of a telephone-based weight loss intervention in postmenopausal women with breast cancer receiving letrozole: the LISA trial. J Clin Oncol 32(21):2231–2239. https://doi.org/10.1200/JCO.2013.53.1517
Travier N, Fonseca-Nunes A, Javierre C, Guillamo E, Arribas L, Peiro I, Buckland G, Moreno F, Urruticoechea A, Oviedo GR, Roca A, Hurtos L, Ortega V, Munoz M, Garrigos L, Cirauqui B, Del Barco S, Arcusa A, Segui MA, Borras JM, Gonzalez CA, Agudo A (2014) Effect of a diet and physical activity intervention on body weight and nutritional patterns in overweight and obese breast cancer survivors. Med Oncol (Northwood, London, England) 31(1):783. https://doi.org/10.1007/s12032-013-0783-5
Harrigan M, Cartmel B, Loftfield E, Sanft T, Chagpar AB, Zhou Y, Playdon M, Li F, Irwin ML (2016) Randomized trial comparing telephone versus in-person weight loss counseling on body composition and circulating biomarkers in women treated for breast cancer: the Lifestyle, Exercise, and Nutrition (LEAN) study. J Clin Oncol 34(7):669–676. https://doi.org/10.1200/JCO.2015.61.6375
Headley JA, Ownby KK, John LD (2004) The effect of seated exercise on fatigue and quality of life in women with advanced breast cancer. Oncol Nurs Forum 31(5):977–983. https://doi.org/10.1188/04.ONF.977-983
Jones LW, Courneya KS, Mackey JR, Muss HB, Pituskin EN, Scott JM, Hornsby WE, Coan AD, Herndon JE 2nd, Douglas PS, Haykowsky M (2012) Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J Clin Oncol Off J Am Soc Clin Oncol 30(20):2530–2537. https://doi.org/10.1200/JCO.2011.39.9014
Yee J, Davis GM, Beith JM, Wilcken N, Currow D, Emery J, Phillips J, Martin A, Hui R, Harrison M, Segelov E, Kilbreath SL (2014) Physical activity and fitness in women with metastatic breast cancer. J Cancer Surviv 8(4):647–656. https://doi.org/10.1007/s11764-014-0378-y
Cormie P, Galvao DA, Spry N, Joseph D, Taaffe DR, Newton RU (2014) Functional benefits are sustained after a program of supervised resistance exercise in cancer patients with bone metastases: longitudinal results of a pilot study. Support Care Cancer 22(6):1537–1548. https://doi.org/10.1007/s00520-013-2103-1
Ligibel JA, Giobbie-Hurder A, Shockro L, Campbell N, Partridge AH, Tolaney SM, Lin NU, Winer EP (2016) Randomized trial of a physical activity intervention in women with metastatic breast cancer. Cancer 122(8):1169–1177. https://doi.org/10.1002/cncr.29899
Scott JM, Iyengar NM, Nilsen TS, Michalski M, Thomas SM, Herndon J 2nd, Sasso J, Yu A, Chandarlapaty S, Dang CT, Comen EA, Dickler MN, Peppercorn JM, Jones LW (2018) Feasibility, safety, and efficacy of aerobic training in pretreated patients with metastatic breast cancer: a randomized controlled trial. Cancer 124(12):2552–2560. https://doi.org/10.1002/cncr.31368
Webster K, Cella D, Yost K (2003) The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes 1:79. https://doi.org/10.1186/1477-7525-1-79
Oncology Nursing Society. https://www.ons.org/make-a-difference/quality-improvement/get-up-get-moving. Accessed 11 Sept 2020
Caan BJ, Cespedes Feliciano EM, Prado CM, Alexeeff S, Kroenke CH, Bradshaw P, Quesenberry CP, Weltzien EK, Castillo AL, Olobatuyi TA, Chen WY (2018) Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol 4(6):798–804. https://doi.org/10.1001/jamaoncol.2018.0137
Rier HN, Jager A, Sleijfer S, van Rosmalen J, Kock M, Levin MD (2018) Changes in body composition and muscle attenuation during taxane-based chemotherapy in patients with metastatic breast cancer. Breast Cancer Res Treat 168(1):95–105. https://doi.org/10.1007/s10549-017-4574-0
Capozzi LC, McNeely ML, Lau HY, Reimer RA, Giese-Davis J, Fung TS, Culos-Reed SN (2016) Patient-reported outcomes, body composition, and nutrition status in patients with head and neck cancer: results from an exploratory randomized controlled exercise trial. Cancer 122(8):1185–1200. https://doi.org/10.1002/cncr.29863
Lonbro S, Dalgas U, Primdahl H, Johansen J, Nielsen JL, Aagaard P, Hermann AP, Overgaard J, Overgaard K (2013) Progressive resistance training rebuilds lean body mass in head and neck cancer patients after radiotherapy—results from the randomized DAHANCA 25B trial. Radiother Oncol 108(2):314–319. https://doi.org/10.1016/j.radonc.2013.07.002
Rief H, Akbar M, Keller M, Omlor G, Welzel T, Bruckner T, Rieken S, Häfner MF, Schlampp I, Gioules A, Debus J (2014) Quality of life and fatigue of patients with spinal bone metastases under combined treatment with resistance training and radiation therapy—a randomized pilot trial. Radiat Oncol 9:151. https://doi.org/10.1186/1748-717x-9-151
Acknowledgements
We acknowledge the efforts, enthusiasm and feedback of the ladies who participated in our EDC study, and the assistance of the Clinical and Translational Science Institute of Southeastern Wisconsin through the NIH Clinical and Translational Science Award (UL1TR001436.) Additionally, we want to thank Dr. Zora Djuric for generously sharing her dietary assessment tools and trackers.
Funding
This study was funded by the National Cancer Institute R21CA218888.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P Sheean has no conflict of interest. L Williams has no conflict of interest. A Visotcky has no conflict of interest. A Banerjee has no conflict of interest. A Moosreiner has no conflict of interest. K Kelley owns and operates the Kelley Kinetics. C Chitambar has no conflict of interest. P Papanek has no conflict of interest. M Stolley has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sheean, P., Matthews, L., Visotcky, A. et al. Every Day Counts: a randomized pilot lifestyle intervention for women with metastatic breast cancer. Breast Cancer Res Treat 187, 729–741 (2021). https://doi.org/10.1007/s10549-021-06163-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06163-1