Abstract
Energy restriction from a low-calorie diet and increased energy expenditure induced by physical activity (PA) could promote weight loss/maintenance and be important determinants of breast cancer (BC) prognosis. The aim of this study was to assess participation and adherence of overweight and obese BC survivors to a lifestyle intervention and to demonstrate the capacity of this intervention to induce weight loss and nutritional changes. This single-arm pre–post study, which involved one-hourly weekly diet sessions delivered by a dietician and 75-min bi-weekly PA sessions of moderate-to-high intensity led by PA monitors, was offered to overweight and obese BC survivors shortly after treatment. Before and after the intervention, anthropometry, dietary information, quality of life (QoL) and cardiorespiratory fitness (CRF) were collected. A total of 112 BC survivors were invited to participate: 42 of them started the intervention and 37 completed it. Participants attended more than 90 % of the sessions offered and showed a significant weight loss of 5.6 ± 2.0 kg, as well as significant decreases in body mass index, fat mass and waist circumference. Significant decreases in total energy (−25 %), fat (−35 %), saturated fat (−37 %) and carbohydrate (−21 %) intakes were observed while QoL and CRF showed significant increases. This feasibility study demonstrated the success of a short-term diet and PA intervention to induce weight loss and promote healthful changes in BC survivors. Assessing the long-term effects of these changes, and in particular their possible impact of BC prognosis, and designing interventions reaching a wider number of BC survivors are still issues to be addressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is by far the most common cancer in women worldwide. In Western Europe, its incidence has increased over the past decades to reach an age-standardized incidence rate of 89.7 per 100,000 women in 2008 [1]. Since BC prognosis has significantly improved in developed countries due to earlier diagnosis and treatment improvements [2], there is a growing population of women living with a history of BC. For this reason, improving their survival as well as their daily physical and psychological health is a new goal for cancer epidemiology.
Obesity has been shown to affect survival in women diagnosed with BC. A recent review of 43 prospective studies, assessing the effect of obesity on BC prognosis, showed poorer overall and BC-specific survival among obese compared with non-obese women [3]. Weight gain after BC diagnosis has also been linked to poorer prognosis [4–8];however, previous results have not always been consistent and significant, and some studies also indicated that weight loss could be associated with poorer survival [7]. On the other hand, there is evidence showing that post-diagnosis physical activity (PA) in BC survivors is inversely associated with BC mortality and all causes mortality [9, 10]. The biological mechanisms that could explain these associations are not yet completely identified. Nevertheless, the mechanisms underlying the association between obesity and survival in cancer patients are likely to involve factors such as insulin, insulin-like growth factor 1 (IGF1) and steroid hormones known to be associated with adiposity and to influence tumour initiation and progression [3, 5, 11–13]. On the other hand, the positive association between PA and BC survival still needs to be better described, but previous studies have indicated that exercise might be associated with insulin, leptin and IGF1 and IGF-binding protein 3 levels [14–16] as well as with inflammation [17] and blood immune function markers [18].
Besides being associated with BC survival, PA after diagnosis has also been shown to have positive effects on body composition, cardiorespiratory fitness (CRF) and psychological outcomes such as anxiety or depression and quality of life (QoL) [19–22]. However, previous intervention studies involving PA have very heterogeneous designs, ranging from highly structured training programs involving up to five group sessions per week to very flexible tailored home-based programs. Since the type of intervention will define participation and compliance, designing a pilot study in order to find the most adequate intervention for a specific target population is essential.
Nutritional patterns post-diagnosis are also thought to be associated with BC prognosis; however, the two largest randomized trials run so far have provided controversial results [23, 24]. In the Women’s Intervention Nutrition Study (WINS), the intervention group followed a low-fat diet (<15 % energy from lipids) and experienced a 5-year cumulative incidence of recurrences of 9.8 %, which was significantly lower than the 12.4 % observed in the control group [23]. In contrast, the Women’s Healthy Eating and Living (WHEL) study did not find any significant difference between a diet rich in vegetables, fruit and fibre, and low in fat [24]. Several reasons were put forward to explain these discrepancies; however, the most remarkable difference was the weight loss observed only in WINS. This observation suggests that besides diet, energy balance could play a determinant role in BC prognosis and that interventions involving calorie restriction from diet as well as energy expenditure induced by PA might improve BC prognosis. In order to corroborate this hypothesis, we designed a multicentric randomized trial to assess the effect of an intervention based on weight loss/control through diet and PA on BC outcome. However, before starting this multicentric trial, we set up the present study to assess the feasibility of this intervention in our population.
The primary aims of the present study were as follows: (a) to assess the capacity of a diet and PA intervention to induce weight loss in BC survivors who had recently achieved their BC treatment (excluding hormonal therapy and treatment for human epidermal growth factor receptor 2) and (b) to evaluate the participation and compliance rates in this intervention. The secondary objectives of this feasibility study were to assess short-term effects of the intervention on diet-related choices, CRF and QoL.
Patients and methods
Participants and eligibility
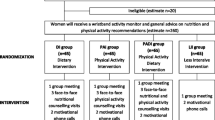
The present feasibility study was a Phase II single-arm trial including only an intervention group. Potentially eligible patients with BC who had completed chemotherapy and/or radiotherapy at the Catalan Institute of Oncology (Spain) during the 6 months preceding recruitment were identified through hospital records and invited by the Head of the BC unit by mail to participate in a study involving a diet and PA intervention. A total of 112 female BC survivors, aged 18–75, with a body mass index (BMI) of 25 kg m−2 or more, received this postal invitation. Exclusion criteria included non-first cancer, tumours of stage IIIB and above, morbid obesity (BMI ≥ 40 kg m−2) and any condition that would not allow patients to follow the diet and PA intervention offered. Ethical approval was obtained from the Clinical Research Ethics Committee (CEIC) of the Bellvitge University Hospital.
After the patients received the postal invitation, they were contacted by phone and the intervention was explained to them in detail before inviting them to come to the hospital for a first visit. During this first visit, the fulfilment of the inclusion and exclusion criteria was checked, the content of the intervention was explained again to the patients, and a consent form was signed by the patients interested in participating in the intervention. A total of 42 patients signed this consent and started the intervention.
Trial intervention
The intervention, planned to last 12 weeks, included a dietary and a PA component, with the combined aim of promoting a weight loss representing at least three per cent of baseline weight. The dietary part of the intervention included a total of 12 weekly one-hour sessions led by a trained dietician. At the beginning of each session, the participants were weighed. The first half of the session was theoretical and focused on food groups, the food pyramid, making healthy choices, preparing and cooking hypo-caloric meals (from 1,200 to 1,500 kcal day−1 on average) and planning weekly menus and shopping lists. The second half of the session was a group discussion focusing on the weight loss goals and achievements of each participant, providing tools and tips to help overcoming weight loss barriers as well as motivational group activities. The PA component of the intervention included 24 bi-weekly sessions of 75 min each led by two trained PA monitors. Each session started with a 10-min warm-up and was then divided into two 25-min sessions of aerobic and muscle-strengthening exercises, respectively. The aerobic exercise part was done using static bicycles aiming at a moderate/high intensity rate corresponding to 70 % of the maximum workload that was re-evaluated every 2 weeks. The muscle-strengthening part was based on group and individual exercises using mats, stability balls and resistance bands. The last 10 min was dedicated to stretching and relaxation. All participants received a pedometer at the beginning of the intervention and were encouraged during the intervention to increase their daily walking to 10,000 steps by the end of the intervention. All diet and PA sessions took place in the hospital, and both morning and evening classes were offered to the participants.
Assessments
Participants were assessed over a 2-week period before and after the intervention. At baseline, a trained technician filled in a lifestyle questionnaire for each participant designed to collect socio-economic status, PA level, tobacco consumption, and medical and reproductive history at time of diagnosis. PA was assessed using the validated questionnaire developed for the European Prospective Investigation into Cancer and Nutrition Cohort study focused on PA in occupational, recreational and household domains [25]. Occupational activity relied on a five-category variable: non-worker, sedentary, standing, manual and heavy manual. Household activities were divided into activities of light (such as cooking, cleaning dishes and ironing) and moderate (such as cleaning windows and bathroom, and playing actively with kids) intensities, while recreational time PA included walking, cycling and sport activities. The weekly duration of recreational and household activities was multiplied by their respective intensity using the Compendium of Physical Activities values [26] to obtain a number of metabolic equivalent (MET)-hours per week. The medical history questionnaire was designed for the study and used to assess the presence of co-morbid conditions at baseline. This information was completed with the medical records used to obtain information related to cancer diagnosis and treatments. At baseline, participants were also asked to fill in a validated self-administered food frequency questionnaire (FFQ) designed to measure habitual food and nutrient intake [27], and eight items related to soy and soy product consumption were added to the FFQ to give a total of 143 food items. The frequency of consumption of the different food items was converted into number of intakes per day and then multiplied by the portion size indicated in the FFQ. Before and after the intervention, three 24-h dietary recalls (24hDR) were conducted by a dietician. Total energy and macronutrient intakes were obtained from the FFQ and 24hDR using the Spanish food composition tables [28, 29]. For anthropometric measurements (taken before and after the intervention), the dietician weighed the participants without shoes and measured their height as well as their waist and hip circumferences. Lean and fat mass were obtained from bioimpedence (tanita BC-418MA). Height and weight were used to calculate BMI.
Quality of life was also assessed at baseline and after the intervention using a questionnaire targeted at cancer patients, the European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire C30 (EORTC QLQ-C30), and a general measure of QoL, the 36-Item Short Form Health Survey (SF-36). The first instrument, a 30-item questionnaire, comprises functioning and symptom scales as well as a scale of global QoL [30]. These scales were transferred to a 0–100 scale using the scoring manual provided by the EORTC [31]. The second instrument, the SF-36, does not target any specific group and is a validated generic measure that yields an 8-scale profile of functional health and well-being scores ranging from 0 to 100 [32, 33].
Before and after the intervention, all the participants were asked to take a CRF test. The first test was used not only to establish baseline CRF level but also to discard any health condition that would prevent participation in the PA intervention. These tests were performed in the physiology laboratory of the University of Barcelona where participants were tested on a precalibrated cycle ergometer (Excalibur, Lode, Groningen, the Netherlands), cycling at 50 rpm. After a 4-min period cycling at 0 W, participants followed a 20 W min−1 ramp protocol up to exhaustion, which was the maximal test. Oxygen uptake and carbon dioxide production were measured by an automatic gas analysis system (Metasys TR-plus, Brainware SA, La Valette, France) equipped with a pneumotach and making use of a two-way mask (Hans Rudolph, Kansas, USA). Before each test, gas and volume calibration took place, according to the manufacturer’s guidelines.
Outcomes
The participants’ participation and compliance to the intervention, as well as weight change between the beginning and the end of the intervention, were the primary outcomes of this feasibility study. Participation was defined by the ratio of the number of women who signed the informed consent form and the number of women who were invited to this study. Compliance was defined by the number of diet and PA sessions attended divided by the number of sessions offered. In terms of weight loss, the objective was a loss equivalent to at least three per cent of the weight measured at baseline. Changes in CRF, QoL and macronutrients consumption pattern were the secondary outcomes of the present study.
Statistical analysis
Shapiro–Wilk’s tests were used to check the normality of the data prior to analysis. The general characteristics of the patients who accepted and did not accept to participate were compared using t-tests and Wilcoxon–Mann–Whitney tests for continuous variables, according to the normality of the distribution within each group. Fisher exact tests were used for categorical variables, as all of them showed some expected values below 5. The effect of the intervention on weight, BMI, CRF, QoL and nutritional pattern was based on the data provided by the participants who completed the intervention. The data obtained before and after the intervention were compared using paired t-tests when the difference was normally distributed and Wilcoxon signed-rank tests for paired samples otherwise. Sensitivity analyses were performed for the main outcome variable (weight change), imputing a weight change of zero to all the participants who did not complete the intervention.
Results
One hundred and twelve BC survivors were eligible to enter the present feasibility study, of which 42 women accepted to participate and signed the informed consent form, 20 women were not interested in participating, 46 women could not participate (the main reasons given were they had grandchildren to look after, they worked or they lived far from the hospital) and four women said they could not without giving a specific reason. Therefore, the present study had a participation rate of 38 %. Table 1 compares the patients who accepted to participate to those who did not. This table does not show any major difference between the two groups. The only statistically significant difference was observed for type of treatment, for which we observed a higher proportion of patients who received surgery and chemotherapy but no radiotherapy in the group who accepted to participate.
The baseline characteristics of the 42 patients who accepted to participate are shown in Table 2. The age of the participants at recruitment ranged from 33 to 70 years, and the participants had a mean BMI of 30.4 ± 3.8 kg m−2. At diagnosis, 60 % of the participants were postmenopausal, 81 % were married or lived with their partner, 40 % were not working and the median level of leisure PA was 22.5 MET-h week−1 (quartile range 21–46). Inclusion criteria did not originally include stage IIIB; however, a patient with a stage IIIB (T4bN0M0) tumour was included on request of one of the oncologists involved in the study.
During the 12 weeks of the intervention, five participants dropped out. Two of them left the study for personal reasons not related with the intervention, two were diagnosed with medical conditions that needed a medical treatment incompatible with the design of the intervention and one was diagnosed with local and distant metastasis. Among the 37 participants who completed the intervention, the attendance to the diet and PA sessions reached 92 and 91 %, respectively (results not shown).
Table 3 describes the 37 participants who completed the intervention and shows anthropometric values, macronutrient intakes, CRF and QoL measured before and after the intervention as well as the percentage changes from baseline assessment and the p values indicating whether the changes observed were statistically significant. Over the 12-week intervention, the participants lost on average 5.6 ± 2.0 kg, which represents 7.8 ± 2.9 % of their baseline weight. Not only this weight difference but also the changes in BMI, waist and hip circumferences, fat percentage and fat mass were statistically significant. Besides these changes in anthropometry, we also observed significant changes in dietary intakes. During the intervention, the participants decreased their total energy intake by 25 %, and the most relevant changes were significant decreases in fat, and in particular saturated fat, and carbohydrates intakes. Before the intervention, participants consumed an average of 1,904 kcal day−1 of which 16 % were from proteins, 42 % from lipids and 43 % from carbohydrates, while after the intervention, patients consumed 1,390 kcal day−1 of which 22 % were from proteins, 34 % from lipids and 44 % from carbohydrates.
At baseline, the participants showed a low peak rate of oxygen consumption (VO2peak) (19.0 ± 2.8 mL kg−1 min−1), which significantly increased by 27 % during the intervention to reach 24.0 ± 4.1 mL kg−1 min−1 at the end of the intervention. A significant improvement was also observed for peak power output with respect to body mass that increased from 1.3 ± 0.3 to 1.7 ± 0.3 W kg−1. No adverse event such as lymphedema was observed during the intervention.
Finally, both questionnaires, the SF-36 and the EORTC QLQ-C30, showed significant increases in QoL over the time of the intervention. At the end of the intervention, the participants perceived that their health in general, and their physical health in particular, had significantly improved, and this was true for which ever tool we used to measure perceived health.
The sensitivity analyses performed for weight change, imputing a weight change of zero to the five participants who did not complete the intervention, showed a significant weight loss of 5.0 ± 2.7 kg corresponding to 6.8 ± 3.7 % of baseline weight (results not shown).
Discussion
The participation rate in this one-arm pre–post feasibility study involving a diet and PA intervention was reasonably low, with only 38 % (42 out of 112) of the eligible women contacted accepting to participate. On the other hand, the compliance with the intervention was very high with 88 % (37 out of 42) of the participants completing the intervention after having attended more than 90 % of the 36 supervised group-based sessions offered over a 12-week period. Among the women who completed the intervention, we observed a significant weight loss of 5.6 kg corresponding to 7.8 % of baseline weight. Apart from weight change, significant decreases in total energy, fat, saturated fat and carbohydrates were also observed as well as significant increases in CRF and QoL.
The participation rate observed in the present study was low; nevertheless, previous intervention studies in BC survivors have shown participation rates of different magnitudes. Indeed, the two largest intervention studies focusing on diet showed participation rates of 45 % for the WINS [23] and 71 % for the WHEL study [24], while two trials involving PA showed participation rates of 42 % for the FRESH START trial [34] and 78 % for the BC and exercise (BREX) study [35]. A study in Sheffield observed a 39 % response rate to the invitation letter sent by the clinicians to eligible patients [36]. On the other hand, the high compliance observed in the present study was somewhat higher than the compliance observed in previous studies involving PA, such as the BREX study that showed a compliance of 62 % [37] or another intervention study carried out in women recovering from early-stage BC that also involved PA and hypocaloric healthy eating that showed that participants completed on average 80 % of the sessions offered to them [38]. While the BREX study was similar to the present study and involved a 12-week intervention, the study published by Scott et al. involved a 6-month intervention. Since one of the aims of this feasibility study was to assess participation and compliance, it is important to mention that these factors are probably defined by the type and timing of the intervention offered and that focussing on these aspects is essential. Flexible trials, involving tailored home-based programs, provided by mail or telephone, are more likely to reach a wider range of participants and offering them a broader selection of activities to choose from that may enhance participation. On the other hand, highly structured training programmes, based on supervised group-based sessions two to five times per week, might be more motivating for the participants who would get more direct contact with intervention monitors and other participants from whom they will get support. So finding the right balance between these two concepts is the challenge for future intervention studies. In a recently published one-arm treatment trial undertaken in rural BC survivors, based on a group-based weight control intervention delivered through conference calls, Befort et al. [39] combined the two approaches and observed a high participation rate of 83 % and a very good average session attendance of 91 % in the women who completed the study (31 out of 34 women).
The other primary aim of the present study was to assess whether the intervention offered could induce a weight loss representing at least three per cent of baseline weight. The weight loss of 5.6 kg (7.8 % of baseline weight) that we observed definitely shows that the intervention reached its main objective. Previous intervention studies, carried out in overweight BC survivors, which involved diet and PA and lasted 6 months or less, have also reported significant weight losses; nevertheless, these losses were of inconsistent magnitudes. McTTiernan et al. [40] in 1998 and Scott et al. [38] in 2013 reported a very modest weight loss at the end of their interventions that, respectively, lasted 8 and 24 weeks. Campbell et al. [41] reported a somewhat higher weight difference −3.83 ± 5.0 kg while Befort et al. [39], who offered a 6-month intervention based on conference call technology in rural BC survivors, observed weight changes of 12.5 ± 5.8 kg or 13.9 ± 5.9 % of baseline weight. While part of the differences observed between studies might be explained by baseline weight, BC survivors in Befort et al. weighed at baseline 89.8 ± 13.6 kg while in the other three studies, baseline weight ranged from 77 to 79 kg, this factor cannot explain all the differences observed. Besides showing changes in weight at the end of the intervention, the present study, as well as those of similar characteristics mentioned before, also showed significant decreases in fat mass and waist circumference. These anthropometric changes are of major importance as obesity and adiposity have been found to be associated with increased levels of insulin, free IGF1, free testosterone and free oestradiol (in postmenopausal women only), and these hormones and proteins have been shown to inhibit apoptosis and promote cell proliferation [12, 13].
Dietary changes were among the secondary objectives of the present study, which involved nutrition classes aimed at reducing total energy intake as well as working towards a better distribution of energy intake coming from proteins, fat and saturated fat and carbohydrates. Changes in dietary pattern were clearly observed in the present study where total energy intake decreased by 25 %. More specifically, the amount of calories coming from fat and saturated fat, respectively, represented 42 and 11 % of total calorie intake at baseline and only 34 and 8 % of total calorie intake at the end of the intervention. Baseline values in the present study were higher than those reported by previous studies of similar characteristics, but the magnitude of the changes was in the range of those previously observed [38–41]. The proportion of saturated fat at the end of the intervention was below 10 % as recommended by WHO; however, the total amount of fat was still above the range of 15–30 % recommended by WHO in order to prevent chronic diseases [42]. Although BC patients tend to be younger than cancer patients in general, a lot of them will have comorbid conditions at diagnosis or will acquire them after diagnosis, because of age or because cancer survivors are at higher risk of getting comorbid conditions [43]. Therefore, reaching the population nutrient intake goals needs to be a priority for BC survivors in order to increase survival as well as health and well-being.
The present study showed a significant increase in CRF, and in particular significant increases in VO2peak and peak power output with respect to body mass. These results are in agreement with the results of four clinical trials that previously showed significant increases in VO2peak [38, 41, 44, 45] and peak power output [44, 45] at the end of PA interventions of 8–24 weeks, offered to BC survivors who had completed their adjuvant treatment. Since CRF is related to the ability to carry out day-to-day activities, it is important to underline that the present study showed very poor baseline CRF (VO2peak = 19.0 ± 2.8 mL kg−1 min−1). These low values stress the need to promote interventions able to increase CRF in order to increase the health and well-being of BC survivors.
During the present study, the participants perceived significant changes in their QoL. Significant increases were observed for general and physical health while mental health showed an increase that was of borderline statistical significance. Increases in QoL after a PA intervention have previously been described in several reviews [19–21]. However, summarizing the evidence is difficult as studies tend to differ in many aspects such as population (age, menopausal status, BMI), type of intervention (PA only, PA and diet), intervention duration and timing (during adjuvant treatment, shortly after, a long time after) or tools used to assess QoL. In a study such as the present one, identifying the possible mechanisms that may explain the changes observed is also a challenge as besides the fact that the absence of control group prevents us from attributing these changes to the intervention, several hypotheses can be made and are difficult to disentangle. Since the intervention was based on 3 weekly group sessions, part of the results observed might be explained by the support the participants got from the group. During the intervention, the participants who shared the same new lifestyle goals and previously had the same BC experience formed very cohesive groups that probably helped them to get over some personal issues related to their recent BC diagnosis and to gain mental strength and optimism. On the other hand, since all these women who were overweight and obese at baseline lost important amounts of weight, part of their increase in QoL might be attributable to this weight loss that may have helped them to have a better image of themselves as well as to feel lighter and more dynamic.
The present study has several limitations and strengths that need to be acknowledged. Among the limitations, the most important one is the absence of a control group. Without a control group, it is impossible to attribute the changes observed to the intervention. Nevertheless, these changes and in particular the significant change in weight observed in the present study do not reflect the pattern generally observed in BC survivors outside of any intervention. A recent review on weight change during and after BC treatment by Vance et al. [46] indicates that more than half of the women experience weight gain during treatment and that some women who manage to remain stable during treatment then report weight gain after treatment. This hypothesis is confirmed by the fact that in our study there was no difference in weight at baseline between the women who finished their treatment <3 months before recruitment and those who finished it from three to 6 months before recruitment. For this reason, it is reasonable to think that the change in weight observed was due to the intervention. Also, and as pointed out by Saarto et al. [37], randomization in studies involving willingness to make changes is difficult to implement and control as participants who sign the informed consent form are generally willing to enter the intervention group and change their habits and quite likely to try to make these changes even if they end up in the group that does not benefit from the intervention. This process of contamination of the control group may then mask the real effect of the intervention. On the other hand, not having a control group in the present study may have affected the participation, compliance and results of the intervention. Indeed, signing an informed consent form knowing it means entering an intervention is not the same that signing having only a 50 % chance to be allocated in the intervention group. For this reason, the participation, compliance and major changes observed in the present study will need to be extrapolated cautiously, remembering they might be based on BC survivors who are highly motivated and ready to make changes. However, this acceptation rate is likely to reflect the proportion of women willing and ready to change their diet and increase their PA shortly after treatment in order to increase the prognosis of their disease. These results are in line with those published by Alfano et al. [47] who indicated that 58 % of long-term BC survivors reported having made positive changes in exercise and/or dietary intake since their diagnosis (32 % reporting increases in PA, and 40–45 % reporting changes in fat, fibre, or fruits and vegetables intakes).
Another limitation of the present study is related to the type of intervention. Although classes programmed at different times of the day were offered to eligible participants, having to come to the hospital three times per week at specific times, to participate in predefined activities, without being able to choose them, may have reduced the participation rate into the study or failed to reach the entire target population.
The use of validated questionnaires to assess dietary habits and QoL is one of the strengths of the present study. Nevertheless, the use of a questionnaire designed to assess QoL in cancer patients may not be the best option to assess QoL in survivors, and future intervention studies may benefit more by completing the use of a general questionnaire such as the SF-36 by questionnaires focussed on anxiety and depression, two psychological dimensions that may not have been sufficiently taken into account in the present study. On the other hand, the use of objective and reliable measures of CRF obtained from a cycloergometer test with ECG monitoring performed by exercise physiologists is another strength of this study.
The content of the intervention involved in the present study, which relied on both diet and PA, is also a strength of this study. Indeed, since the biological mechanisms involved in the association between obesity, and more generally energy balance, and BC prognosis are likely to rely on more than one pathway [12], designing and evaluating the effect of interventions likely to affect multiple pathways is essential. Furthermore, adding PA to a diet designed to lose weight is on the one hand likely to increase the probability of success of the intervention and to help the participants to maintain the changes obtained over time, and on the other hand, an opportunity to adopt a new habit known to also reduce the risk of hypertension, coronary heart disease, stroke and diabetes [48].
The present feasibility study, carried out in a Spanish population of BC survivors, produced valuable results that helped the authors to design a multicentric randomized trial aimed to assess the effect of an intervention based on weight loss/control through diet and PA on BC outcome in the very same population. The high adherence to the intervention and the major changes observed at the end of the intervention showed that the intervention offered was well received by the population and able to produce the weight loss and lifestyle changes expected. However, the authors also believe it would be necessary to extend the intervention duration from 12 to 20 weeks to make sure the changes observed are long-lasting changes relying on the adoption of new habits likely to improve the BC prognosis, and health in general, of the participants. In order to help instigate these new habits, and in particular to encourage participants to add exercise to their daily routine, the authors decided to add three home-based sessions of physical exercise per week, on top of the two sessions led by PA monitors already included in the intervention of the feasibility study. On the other hand, the low participation rate observed indicates that special efforts need to be made to reach a larger proportion of the target population. To meet this objective, the authors are planning to prospectively recruit participants instead of retrospectively. Indeed, instead of receiving a postal invitation during the few months following treatments, the patients will hear about the clinical trial before finishing chemotherapy and/or radiotherapy and will be invited to participate by a member of the clinical team treating them. The aim of this change is to help them view the intervention offered as a continuation of their treatment, which could possibly increase participation.
Conclusion
The present feasibility study confirms that BC survivors are willing to make changes and adopt healthier habits and that a short-term lifestyle intervention based on diet and PA can induce weight loss, promote healthful changes in dietary habits and increase CRF and QoL. Further research is needed to define interventions that increase participation rate by reaching a wider number of BC survivors and to determine the long-term effects of this type of intervention and in particular the possible impact of these lifestyle changes on BC prognosis.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, Cancer incidence and mortality worldwide: IARC CancerBase No. 10. International Agency for Research on Cancer. IARC. 22-2-2013. Lyon, France. 22-2-2013. http://globocan.iarc.fr/. Accessed May 2013.
Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F, Capocaccia R. EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentary. Eur J Cancer. 2009;45:931–91.
Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–35.
Bradshaw PT, Ibrahim JG, Stevens J, Cleveland R, Abrahamson PE, Satia JA, et al. Postdiagnosis change in bodyweight and survival after breast cancer diagnosis. Epidemiology. 2012;23:320–7.
Chlebowski RT, Aiello E, McTiernan A. Weight loss in breast cancer patient management. J Clin Oncol. 2002;20:1128–43.
Nichols HB, Trentham-Dietz A, Egan KM, Titus-Ernstoff L, Holmes MD, Bersch AJ, et al. Body mass index before and after breast cancer diagnosis: associations with all-cause, breast cancer, and cardiovascular disease mortality. Cancer Epidemiol Biomarkers Prev. 2009;18:1403–9.
Caan BJ, Kwan ML, Shu XO, Pierce JP, Patterson RE, Nechuta SJ, et al. Weight change and survival after breast cancer in the after breast cancer pooling project. Cancer Epidemiol Biomarkers Prev. 2012;21:1260–71.
Thivat E, Therondel S, Lapirot O, Abrial C, Gimbergues P, Gadea E, et al. Weight change during chemotherapy changes the prognosis in non-metastatic breast cancer for the worse. BMC Cancer. 2010;10:648.
Ibrahim EM, Al Homaidh A. Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Med Oncol. 2011;28:753–65.
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104:815–40.
Demark-Wahnefried W, Platz EA, Ligibel JA, Blair CK, Courneya KS, Meyerhardt JA, et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomarkers Prev. 2012;21:1244–59.
Hursting SD, Digiovanni J, Dannenberg AJ, Azrad M, LeRoith D, Demark-Wahnefried W, et al. Obesity, energy balance, and cancer: new opportunities for prevention. Cancer Prev Res (Phila). 2012;5:1260–72.
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–91.
Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K, et al. Relationship of obesity and physical activity with C-peptide, leptin, and insulin-like growth factors in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2005;14:2881–8.
Irwin ML, Varma K, Alvarez-Reeves M, Cadmus L, Wiley A, Chung GG, et al. Randomized controlled trial of aerobic exercise on insulin and insulin-like growth factors in breast cancer survivors: the Yale Exercise and Survivorship study. Cancer Epidemiol Biomarkers Prev. 2009;18:306–13.
Fairey AS, Courneya KS, Field CJ, Bell GJ, Jones LW, Mackey JR. Effects of exercise training on fasting insulin, insulin resistance, insulin-like growth factors, and insulin-like growth factor binding proteins in postmenopausal breast cancer survivors: a randomized controlled trial. Cancer Epidemiol Biomarkers Prev. 2003;12:721–7.
Pierce BL, Neuhouser ML, Wener MH, Bernstein L, Baumgartner RN, Ballard-Barbash R, et al. Correlates of circulating C-reactive protein and serum amyloid A concentrations in breast cancer survivors. Breast Cancer Res Treat. 2009;114:155–67.
Fairey AS, Courneya KS, Field CJ, Bell GJ, Jones LW, Mackey JR. Randomized controlled trial of exercise and blood immune function in postmenopausal breast cancer survivors. J Appl Physiol. 2005;98:1534–40.
Fong DY, Ho JW, Hui BP, Lee AM, Macfarlane DJ, Leung SS, et al. Physical activity for cancer survivors: meta-analysis of randomised controlled trials. BMJ. 2012;344:e70.
Bicego D, Brown K, Ruddick M, Storey D, Wong C, Harris SR. Effects of exercise on quality of life in women living with breast cancer: a systematic review. Breast J. 2009;15:45–51.
McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS. Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. CMAJ. 2006;175:34–41.
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409–26.
Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, et al. Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women’s Intervention Nutrition Study. J Natl Cancer Inst. 2006;98:1767–76.
Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, et al. Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women’s Healthy Eating and Living (WHEL) randomized trial. JAMA. 2007;298:289–98.
Cust AE, Smith BJ, Chau J, van der Ploeg HP, Friedenreich CM, Armstrong BK, et al. Validity and repeatability of the EPIC physical activity questionnaire: a validation study using accelerometers as an objective measure. Int J Behav Nutr Phys Act. 2008;5:33.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504.
Fernandez-Ballart JD, Pinol JL, Zazpe I, Corella D, Carrasco P, Toledo E, et al. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr. 2010;103:1808–16.
Moreiras O, Carbajal A, Cabrera L, Cuadrado C. Tablas de composicion de alimentos (Food Composition Tables). 9th ed. Pirámide; 2005.
Jimenez Cruz A, Cervera Ral P, Bacardi Gascon M. Tabla de composición de alimentos (Food Composition Table). 7th ed. Novartis; 2002.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A. The EORTC QLQ-C30 Scoring Manual. 3rd ed. European Organisation for Research and Treatment of Cancer; 2001.
Ware JE, Snow KK, Kosinski M, Gandek B. SF36 health survey: manual and interpretation guide. Boston: The Health Institute; 1983.
Alonso J, Regidor E, Barrio G, Prieto L, Rodriguez C, de la Fuente L. Population reference values of the Spanish version of the Health Questionnaire SF-36. Med Clin (Barc). 1998;111:410–6.
Demark-Wahnefried W, Clipp EC, Lipkus IM, Lobach D, Snyder DC, Sloane R, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25:2709–18.
Penttinen H, Nikander R, Blomqvist C, Luoto R, Saarto T. Recruitment of breast cancer survivors into a 12-month supervised exercise intervention is feasible. Contemp Clin Trials. 2009;30:457–63.
Daley AJ, Crank H, Mutrie N, Saxton JM, Coleman R. Patient recruitment into a randomised controlled trial of supervised exercise therapy in sedentary women treated for breast cancer. Contemp Clin Trials. 2007;28:603–13.
Saarto T, Penttinen HM, Sievanen H, Kellokumpu-Lehtinen PL, Hakamies-Blomqvist L, Nikander R, et al. Effectiveness of a 12-month exercise program on physical performance and quality of life of breast cancer survivors. Anticancer Res. 2012;32:3875–84.
Scott E, Daley AJ, Doll H, Woodroofe N, Coleman RE, Mutrie N, et al. Effects of an exercise and hypocaloric healthy eating program on biomarkers associated with long-term prognosis after early-stage breast cancer: a randomized controlled trial. Cancer Causes Control. 2013;24:181–91.
Befort CA, Klemp JR, Austin HL, Perri MG, Schmitz KH, Sullivan DK, et al. Outcomes of a weight loss intervention among rural breast cancer survivors. Breast Cancer Res Treat. 2012;132:631–9.
McTiernan A, Ulrich C, Kumai C, Bean D, Schwartz R, Mahloch J, et al. Anthropometric and hormone effects of an eight-week exercise-diet intervention in breast cancer patients: results of a pilot study. Cancer Epidemiol Biomarkers Prev. 1998;7:477–81.
Campbell KL, Van Patten CL, Neil SE, Kirkham AA, Gotay CC, Gelmon KA, et al. Feasibility of a lifestyle intervention on body weight and serum biomarkers in breast cancer survivors with overweight and obesity. J Acad Nutr Diet. 2012;112:559–67.
Nishida C, Uauy R, Kumanyika S, Shetty P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: process, product and policy implications. Public Health Nutr. 2004;7:245–50.
Khan NF, Mant D, Carpenter L, Forman D, Rose PW. Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: a database study. Br J Cancer. 2011;105(Suppl 1):S29–37.
Courneya KS, Mackey JR, Bell GJ, Jones LW, Field CJ, Fairey AS. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003;21:1660–8.
Herrero F, SanJuan AF, Fleck SJ, Balmer J, Perez M, Canete S, et al. Combined aerobic and resistance training in breast cancer survivors: a randomized, controlled pilot trial. Int J Sports Med. 2006;27:573–80.
Vance V, Mourtzakis M, McCargar L, Hanning R. Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev. 2011;12:282–94.
Alfano CM, Day JM, Katz ML, Herndon JE, Bittoni MA, Oliveri JM, et al. Exercise and dietary change after diagnosis and cancer-related symptoms in long-term survivors of breast cancer: CALGB 79804. Psychooncology. 2009;18:128–33.
World Health Organization. Global Strategy on Diet, Physical Activity and Health. WHO. (2006). 1-3-2013. http://www.who.int/dietphysicalactivity/pa/en/index.html. Accessed May 2013.
Acknowledgments
This research was supported by a grant from the Asociación Española Contra el Cancer (AECC) Junta de Barcelona and by ISCIII (RETICC RD06/0020/0091) of the Spanish Ministry of Health.
Conflict of interest
The authors declare that they have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Travier, N., Fonseca-Nunes, A., Javierre, C. et al. Effect of a diet and physical activity intervention on body weight and nutritional patterns in overweight and obese breast cancer survivors. Med Oncol 31, 783 (2014). https://doi.org/10.1007/s12032-013-0783-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0783-5