Abstract
Breast cancer recurrence is a major cause of the disease-specific death. Circulating tumor cells (CTCs) are negatively associated with breast cancer survival. Plakoglobin, a cell adhesion protein, was recently reported as a determinant of CTCs types, single or clustered ones. Here, we aim to summarize the studies on the roles of plakoglobin and evaluate the association of plakoglobin and breast cancer survival. Plakoglobin as a key component in both cell adhesion and the signaling pathways was briefly reviewed first. Then the double-edge functions of plakoglobin in tumors and its association with CTCs and breast cancer metastasis were introduced. Finally, based on an open-access database, the association between plakoglobin and breast cancer survival was investigated using univariate and multivariate survival analyses. Plakoglobin may be a molecule functioning as a double-edge sword. Loss of plakoglobin expression leads to increased motility of epithelial cells, thereby promoting epithelial–mesenchymal transition and further metastasis of cancer. However, studies also show that plakoglobin can function as an oncogene. High expression of plakoglobin results in clustered tumor cells in circulation with high metastatic potential in breast cancer and shortened patient survival. Plakoglobin may be a potential prognostic biomarker that can be exploited to develop as a therapeutic target for breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common and the most deadly cancer worldwide in women. In 2015, it is estimated that additional 231,840 women will be diagnosed with breast cancer, and 40, 290 women will die of the disease in United States [1]. The recurrence of breast cancer is a major cause of the disease-specific death, which often occurs typically within 5 years or even up to 10–20 years after surgery, since the recurrence is usually more aggressive and untreatable [2–4]. Accumulating evidence has shown that cancer stem cells (CSCs) are a culprit of the recurrence, metastasis, and resistance to traditional chemotherapy in human cancer including breast, thereby shortening patient survival [5, 6]. Metastases can occur at the early stage of breast cancer [7, 8]. Disseminated breast CSCs either are in quiescent status living somewhere in the body or grow again and lead to recurrence once they meet favorable niches [9–11].
Circulating tumor cells (CTCs) are those tumor cells detaching from primary tumor tissues and circulating in the bloodstream after intravasation. Accumulating evidence shows that CTCs are linked to metastatic relapse and are regarded as a prognostic marker for human cancer including breast, prostate, lung, and colorectal cancer [12–17]. CTCs also demonstrate the properties of CSCs that can generate the diverse tumor cells in immunodeficient mice [18]. Functional xenograft assays show that primary human luminal breast cancer-derived CTCs contain metastasis-initiating cells (MICs) with the phenotypes of EPCAMlow METhigh CD47high CD44high [19]. The presence of CTCs clusters in the blood of patients with cancer has attracted attention, since CTCs clusters show more metastatic potential than single CTCs [20, 21]. It has been demonstrated that CTCs could aggregate with other types of cells that are present in the circulation, for example, platelets and leukocytes [22–24]. These accompanying components have either protective or cytotoxic effects on CTCs. On the other hand, tumor cells could also detach in clusters with either stromal or tumor cells from primary tumor tissues and enter into the circulation as partners to start their journey; the clustered cells traveling through the bloodstream facilitate the growth of metastatic loci at a distant site [20, 25].
Cell–cell adhesion is a determinant of CTCs in the form of either single or clustered cells, between which significant differences in the expression of junction plakoglobin (JUP, or plakoglobin) have been shown [20]. Plakoglobin is an important component of desmosomes (a junctional complex structure for cell–cell adhesion) and adherence junctions [20, 26]. Studies have shown that plakoglobin plays a key role in controlling the motility of epithelial cells [27–30]. The cells with upregulated levels of plakoglobin show lower motility, while those with low plakoglobin levels display high metastatic potential [27–30]. However, the association between plakoglobin and malignancies still remains controversial [31–33]. In this review, we summarized recent findings on the role of plakoglobin in breast cancer metastasis, as well as evaluated the association between plakoglobin and breast cancer survival using an open-access database of gene expression-based outcome for breast cancer.
Plakoglobin mediates cell adhesion
Junction plakoglobin (JUP or plakoglobin) gene is located on chromosome 17, neighboring breast cancer 1, early onset gene (BRCA1). Plakoglobin encodes an 83-kDa cell adhesion protein of γ-catenin (also known as plakoglobin), a homolog of β-catenin [34, 35]. The plakoglobin stability is associated with the status of threonine 14 in its amino acid sequence; the post-translational glycosylation of threonine 14 increases the stabilization of plakoglobin, which may prevent the access of proteasome for degradation [36]. Localization staining shows that plakoglobin is expressed in both desmosomes and the adherent junction [34]. Like β-catenin, plakoglobin can be a linker between E-cadherin (a calcium-dependent cell surface glycoprotein) and α-catenin in cell–cell adhesion (Fig. 1), stabilizing the localization of E-cadherin in cell surface [35, 37, 38]. Studies have shown that plakoglobin plays an important role in the formation of desmosomes, promoting the binding of desmoplakin proteins to intermediate cytoskeletal filaments, and recruiting plakophilin 3 to the membrane, where cadherin proteins are enriched [39, 40]. The positive associations of plakoglobin with both adherens junction and desmosome cadherin were observed in keratinocytes that overexpress UDP-N-acetylglucosamine-polypeptide β-N-acetylglucosaminyl transferase (O-GlcNAc transferase, OGT), which glycosylates plakoglobin protein [36]. Moreover, there is a dose-dependent correlation between plakoglobin levels and the function of cell adhesion, making cells functional coordination. For instance, JUP −/− mice displayed an embryonic lethal phenotype due to cell dissociation in the heart [41], whereas heterozygous JUP +/−-deficient mice showed increased right ventricular volume with reduced right ventricular function, although the levels of β-catenin and N-cadherin did not change [42, 43]. This intercellular adhesion makes both epithelial and non-epithelial cells endure mechanical stress and maintain organ morphogenesis and cell polarity. Loss of the desmosomal assembly leads to the cytoskeletal reorganization and loss of polarity of epithelial cells, thereby increasing the capacity of cell migration and invasion with acquisition of metastatic seeding and stemness traits of epithelial–mesenchymal transition (EMT) [44–47]. A squamous cell carcinoma SCC9 cell line, which is insufficient in the expression of both plakoglobin and E-cadherin, exhibited a mesenchymal–epithelial transition (MET) upon the enforced plakoglobin expression [48, 49]. Another study demonstrated that ectopically expressed plakoglobin resulted in the decreases in metastatic potential by enhancing intercellular adhesive strength in prostate cancer [50]. A very recent study found that plakoglobin expression was down-regulated by hepatitis C virus protein, which can induce EMT in human hepatocytes [51].
Cell adhesion molecule of plakoglobin. Both plakoglobin and β-catenin can be a linker between E-cadherin (a transmembrane glycoprotein) and α-catenin that attaches to actin filaments (cytoskeleton elements), forming cell junction complex. The complex can enhance the endurance against mechanical stress and maintain cell polarity and organ morphogenesis
Plakoglobin is involved in cell signaling
Evidence that plakoglobin regulates the shuttle of different transcription factors to the nucleus suggests that it is also involved in cell signaling besides cell adhesion [52]. In consistence with the hypothesis of plakoglobin as cell signaling molecules, the interaction between plakoglobin and cytoplasmic domain of desmoglein could induce the alteration of downstream molecules, leading to the suppression of dorsalized gastrulation and anterior axis duplication in fertilized Xenopus embryos [53]. Recently, it has been reported that plakoglobin is involved in extracellular matrix (ECM)-Src (SRC proto-oncogene, non-receptor tyrosine kinase) and RhoGTPase-dependent pathways, controlling cell motility by inhibiting Src kinase [27], and keeping ECM protein vitronectin (CN) at a low level [50]. Moreover, evidence has exhibited that plakoglobin also participates in the Wnt signaling pathway [54], and it functions as an antagonist [55]. Further study has shown that the expressions of downstream genes in the Wnt signaling pathway increased in the plakoglobin-deficient zebrafish models, whereas plakoglobin −/−-induced cardiac phenotype could be rescued by the expression of the Wnt inhibitor Dkk1 [55]. In addition, Spindler et al. [56] demonstrated that plakoglobin was involved in the phosphorylation of p38 mitogen-activated protein kinase (p38MAPK). Knockdown of plakoglobin expression with the silencing RNA led to the activation of p38MAPK and reduced cell adhesion [56], thereby activating downstream effectors of mitogen-activated protein kinase-activated protein (MAPKAP) kinase 2 and heat shock protein 27 (HSP27) [57, 58]. Furthermore, plakoglobin can act as a transcription factor, regulating the expression of desmocollins 2 (Dsc2) or Dsc3 [59]. With the help of lymphoid enhancer factor 1 (Lef-1), plakoglobin translocates into cell nucleus and binds to the promoters of Dsc2 and Dsc3. However, this binding can be blocked by T cell factor (TCF)/Lef-1 complex [59, 60]. Similarly in tumor cells, reporter assays exhibited that plakoglobin was a key regulator of several genes, such as pituitary tumor transforming gene (PTTG) [61], special AT-rich sequence binding protein 1 (SATB1), and metastasis suppressor Nm23-H1 (NME1) [62]. Although plakoglobin can bind to the promoters of both SATB1 and NME1, it showed differentiated regulatory roles; ectopic expression of plakoglobin results in decreases in the levels of SATB1, but not NME1 [62].
Interestingly, plakoglobin may also be a regulator in glucose intolerance via the involvement of insulin signaling. In skeletal muscle, it has been shown that plakoglobin could bind to the insulin receptor and PI3K subunit p85, promoting PI3K-Akt-FoxO signaling, and enhancing glucose uptake to maintain glucose homeostasis [63]. The ubiquitin ligase tripartite motif-containing protein 32 (Trim32) could act as a suppressor of plakoglobin activity; overexpression of Trim32 could induce glucose intolerance and cause muscle atrophy, whereas the inhibition of Trim32 expression could release its suppressive role in plakoglobin-mediating insulin signaling pathway, making cells sensitize to insulin [63].
Plakoglobin: an oncogene or a tumor suppressor?
There are controversial reports on whether plakoglobin is an oncogene or tumor suppressor. Some studies indicate that plakoglobin has oncogenic activities. Kolligs et al. reported that enforced over-expression of plakoglobin in rat RK3E epithelial cells, in which considerable amounts of endogenous plakoglobin and β-catenin are expressed, promoted neoplastic transformation; the underlying molecular mechanism was that plakoglobin over-expression led to upregulation of c-Myc and activation of TCF/Lef signaling [31]. Similarly, ectopic over-expression of plakoglobin in HCT116 cells, a cell line carrying both wild-type adenomatous polyposis coli (APC) and p53, could result in the enhanced invasive capacity by decreasing Ecadherin and upregulating c-Myc [61]. Chen et al. showed that Desmoglein 3 (DSG3)/plakoglobin/TCF/Lef pathway facilitated cancer growth and invasion [64]. The authors found that knockdown of DSG3 disrupted its association with plakoglobin and led to the down-regulated expression in the downstream target genes of c-myc, cyclin D1, and MMP-7, thereby inhibiting cell migration and invasion [64].
Plakoglobin also acts as a tumor suppressor, inhibiting tumor growth, migration, and invasion in some in vitro experiments [62]. In the plakoglobin-overexpressing cells, the BrdU incorporation is significantly decreased compared to their parental cells [62]. Loss of plakoglobin resulting from latent membrane protein 1 (LMP1) of Epstein–Barr virus (EBV) may also activate PI3 K/Akt/NF-kB signaling, thereby engaging in EBV-induced metastasis [28]. Restoration of plakoglobin could, however, inhibit LMP1-induced tumor invasion [28]. Moreover, plakoglobin could interact with the sex-determining region Y box 4 (SOX4) in response to the Wnt signaling in breast and prostate cancer cell lines, blocking the SOX4-DNA binding, and suppressing the Wnt-responsive transcription [65]. This blockade may reduce the metastatic potential and improve survival of breast cancer given that SOX4 is positively associated with distant metastases and death of the tumor [66, 67]. In addition, plakoglobin may also act as a tumor suppressor via enhancing the transcriptional activity of p53. It has been shown that plakoglobin could bind to the p53 consensus sequence in the promoter of SFN gene, inducing the expression of 14-3-3σ (also called stratifin, encoded by SFN gene) in MCF-7 cells [68].
Taken together, these findings suggest that plakoglobin functions as a two-edge sword as either an oncogene or tumor suppressor, depending on the cellular context and the activated downstream signaling pathways it regulates.
Plakoglobin, CTCs, and breast cancer metastasis
In BRCA1-associated breast cancer, loss of heterozygosity of plakoglobin is also common [69]. Plakoglobin mutation increases the risk of breast cancer [70]. Based on the datasets of breast cancer in The Oncomine® Platform (http://www.oncomine.org), plakoglobin was co-expressed in a strong correlation (correlation coefficients were 0.71–0.75) with epithelial cell adhesion molecule (EPCAM) [71, 72], a transmembrane glycoprotein that is involved in cell adhesion and cell signaling [73, 74]. This co-downregulation of plakoglobin and E-cadherin was also observed in other malignant cells [75]. Insufficient expression of plakoglobin could promote EMT, and loss of cell–cell adhesion is thought as the first necessary step for tumor cells to leave primary loci and enter the circulation. Studies have shown that low levels of plakoglobin expression are positively associated with high metastatic potential in breast cancer [76–78]. Axillary lymph node metastases showed a lower percentage of plakoglobin immunostatining than the regional metastases [79]. Plakoglobin silencing in vitro leads to the decrease in cell–cell contact and in vivo results in the increase of breast cancer dissemination [80]. In addition, studies also indicate the presence of an E2-box element in the promoter of plakoglobin gene. This element can be bound by the zinc finger transcription factor SLUG, which is highly expressed in triple-negative breast cancer [81, 82] and is a key regulator in EMT and stem cell phenotypes [83, 84]. Through recruiting co-repressor C-terminal binding protein 1 (CtBP1) and histone deacetylase 1 (HDAC1), SLUG inhibits plakoglobin expression [77, 85, 86].
Tumor metastasis, a major cause of cancer-specific mortality, is a complex process with a series of steps. First, tumor cells leave the primary disease loci, go through the extracellular matrix (ECM) and intravasate into circulation and lymphatic vessels. Then, CTCs survive all kinds of body defense systems, extravasate, and adapt to the new niches. Finally, as seeds, CTCs colonize and proliferate to form new tumor loci in new places [87]. Compared to via the blood systems, tumor spread via lymphatic vessels is still poorly understood [88]. CTCs in blood are present in different forms, single CTCs, clustered CTCs, and cloaked CTCs by platelets or coagulation factors [23, 89]. The diameters of all these types of CTCs are much larger than the bores of distal capillaries. Thus, most of CTCs are trapped and cleared out, resulting in the rare number of CTCs in the circulation [87, 88], which may be the subpopulation of CTCs with extremely small size and/or considerable flexibility to go through capillary beds, or those surviving through bypass tracts of capillary beds. Based on the currently available Chip-capturing detection methods, there were greater than 500 CTCs per 7.5 ml of blood in approximately less than 1.5 % of patients with progressive breast cancer [19]. Clustered CTCs are most likely directly derived from the primary tumors, rather than the proliferation of single CTCs or the aggregation of circulating CTCs [20]. Although the clearance rate of clustered CTCs is higher than that of single CTCs, clustered CTCs have a higher metastatic potential to lung than single CTCs [20]. Clustered CTCs that account for only 2–5 % of all detectable CTCs in the circulation contribute to appropriately 50 % of all metastatic breast cancer loci in orthotopic breast cancer models [20]. Moreover, the clustered CTCs-derived lung metastases are more resistant to apoptosis than single CTCs-derived lung loci, and metastatic tumors expand more rapidly, thereby leading to shorter overall survival in mouse models [20]. In breast cancer patients, those with detectable clustered CTCs across more than three time points had significantly shorter progression-free survival than those with detectable clustered CTCs at less than 3 time points or with single CTCs [20]. The higher metastatic potential was also pronounced, leading to significantly shorter overall survival in prostate cancer patients who had detectable clustered CTCs during at least one time point than those with single CTCs only [20].
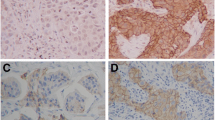
Transcriptome analyses using single-cell resolution next generation sequencing (NGS) showed that clustered CTCs consistently had a higher expression of plakoglobin than single CTCs, although there was no obvious difference at the global gene expression level between the two types, single and clustered CTCs [20]. As an important component of cell adherence complex, the heterogeneity of plakoglobin expression within primary tumors might lead to different types of CTCs, single or clustered. Plakoglobin protein staining was positive in multiple clustered CTCs, while matched single CTCs from the same breast cancer patient showed negative [20]. Interestingly, some mesenchymal markers, e.g., transforming growth factor (TGF)-β pathway components and the forhead box C1 (FOXC1) transcription factor, were also over-expressed in clustered CTCs [22, 23, 90], which may enhance the survival of clustered CTCs and interactions of cell–cell and cell–matrix during cancer spread. In vitro experiments showed that plakoglobin silencing resulted in the dissociation of cell–cell junctions in breast cancer cell lines, but not in non-transformed breast epithelial cells [20]. This finding suggested that cell–cell junctions of breast cancer cells might be more plakoglobin-dependent than normal epithelial cells. Similarly, the potential to form lung metastasis was reduced in in vivo animal models when plakoglobin was silenced in the breast cancer cell lines; orthotopic xenografts results showed that plakoglobin silencing significantly reduced both the number of clustered CTCs and metastatic loci in lung, despite neither the growth rate of xenografted primary tumors nor the number of single CTCs derived from the primary tumor were not affected [20].
Plakoglobin expression and breast cancer survival
In a cohort of 1,956 patients with either estrogen receptor (ER)-positive, HER2-positive, or triple-negative breast cancer, Kaplan–Meier survival curves analysis showed that patients with high plakoglobin in the primary tumors had a significantly worse distant metastasis-free survival compared to those with low expression (p = 0.008) [20]; the curves between low and high plakoglobin expression were not separated approximately until 3.5 years. Using a publicly available database on breast cancer (http://co.bmc.lu.se/gobo/) [91, 92], we analyzed the associations of plakoglobin expression and breast cancer 10-year survival using both univariate and multivariate analyses, in which patients were classified into three subgroups based on the tertile distribution of plakoglobin expression: low (−3.570 ≤ plakoglobin <−0.508), medium (−0.508 ≤ plakoglobin <0.208), and high (0.208 ≤ plakoglobin ≤2.726). Kaplan–Meier survival curves showed that patients with low plakoglobin expression had significantly better distant metastasis-free survival (Fig. 2a, p = 0.02182) and overall survival (Fig. 2b, p < 0.00001), and borderline significantly superior relapse-free survival (Fig. 2c, p = 0.05008) compared to those with high one. After adjusting the potential confounding factors (which include estrogen status (ER), lymph node status (NodeStatus), tumor grade (GradeStrat), patient age (AgeStrat), and study (SizeStrat)) using multivariate Cox proportional hazard regression analyses, again, patients with low plakoglobin expression had significantly reduced risks of distant metastasis (p = 0.01), death (p = 1 × 10−5), and relapse (p = 0.001) compared to those with high one (Fig. 3). Patients with low plakoglobin expression had approximately 75 % reduced death risks, followed by 50 % reduced relapse risks and 40 % reduced distant metastatic risks, and that those with the medium one had approximately 50 % reduced death risks (p = 0.006), followed by 30 % reduced relapse risks (p = 0.05), 20 % reduced distant metastasis risks (p = 0.4). These findings suggest that plakoglobin expression is an independent prognostic factor in the patients with breast cancer; particularly for overall survival, those with low plakoglobin expression had superior survival than those with the high one. Plakoglobin may be a potential therapeutic target in the improvement of breast cancer survival and prevention of relapse and distant metastasis.
Kaplan–Meier survival curves stratified by plakoglobin expression in breast cancer. Compared to those with high plakoglobin expression (0.208≤ plakoglobin ≤2.726), patients with low one (−3.570 ≤ plakoglobin <−0.508) had superior distant metastasis-free survival (DMFS) (p = 0.02182) (a), overall survival (OS) (p < 0.00001) (b), and relapse-free survival (RFS) (p = 0.05008) (c), respectively
Associations of plakoglobin expression and breast cancer patient outcome in multivariate Cox proportional hazard regression analyses. After the adjustment of estrogen status (ER), lymph node status (NodeStatus), tumor grade (GradeStrat), patient age (AgeStrat), and study (SizeStrat), patients with low plakoglobin expression (−3.570 ≤ plakoglobin <−0.508) and medium one (−0.508 ≤ plakoglobin <0.208) had reduced distant metastasis risks compared to those with high one (0.208 ≤ plakoglobin ≤ 2.726); the adjusted hazard ratios (HRs) were significant (p = 0.01) for the low, but not statistically significant (p = 0.4) for the medium (a). Patients with low or medium plakoglobin expression had significantly reduced death risks compared to those with high one; the p values for their adjusted HRs were 1 × 10−5 and 0.006, respectively (b). Patients with low or medium one had reduced relapse risks compared to those with the high, the p values for their adjusted HRs were 0.001 and 0.05, respectively (c)
Conclusions
Plakoglobin is not only involved in cell adhesion, but can also be a regulator of signaling pathways. Both microenvironments and the activated signaling pathways determine its functions of plakoglobin as either an oncogene or tumor suppressor. The roles of plakoglobin in the development and progression of breast cancer seem to be phase-dependent. In the progression of breast cancer, plakoglobin expression was negatively associated with prognosis; high plakoglobin expression makes breast cancer cells move in clusters, which are more predisposed to form distant metastasis. In other words, the correlation between high plakoglobin expression and worse survival of breast cancer may have nothing to do with either oncogenic or tumor-suppressive function of plakoglobin. Instead, being an adhesion molecule, high plakoglobin expression enables tumor cells to stick together and move in clusters in the bloodstream, allowing more chances of metastasis, resulting in worse survival of breast cancer (Fig. 4). However, plakoglobin silencing only can reduce the clustered CTCs-associated metastasis, but not single CTCs-associated spread via blood. Thus, it is worthy of further investigations on (1) what factor(s) is involved in the single CTCs-associated metastasis; (2) what other factor(s) may be involved in clustered CTCs-associated metastasis besides plakoglobin; (3) what transcription factor(s) regulates the expression of plakoglobin; (4) what molecules are potentially involved in the aggregation of single CTCs to become clustered CTCs in the circulation; (5) whether or not and how the phenotypes of CTCs can be modified by the uptake of circulating exosomes (extracellular nanovesicles) that are released from other cells.
A putative model for plakoglobin, types of circulating tumor cells (CTCs), and their metastasis capacities. Tumor cells with high plakoglobin expression escape from primary tumor masses, enter and circulate in clusters in the bloodstream. Such clusters promote their metastases to secondary sites, leading to worse survival of breast cancer patients
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics. CA Cancer J Clin 65(1):5–29. doi:10.3322/caac.21254
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347(16):1227–1232. doi:10.1056/NEJMoa020989
Blichert-Toft M, Nielsen M, During M, Moller S, Rank F, Overgaard M, Mouridsen HT (2008) Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol 47(4):672–681. doi:10.1080/02841860801971439
Nielsen HM, Overgaard M, Grau C, Jensen AR, Overgaard J (2006) Loco-regional recurrence after mastectomy in high-risk breast cancer–risk and prognosis. An analysis of patients from the DBCG 82 b&c randomization trials. Radiother Oncol 79(2):147–155. doi:10.1016/j.radonc.2006.04.006
Visvader JE, Lindeman GJ (2012) Cancer stem cells: current status and evolving complexities. Cell Stem Cell 10(6):717–728. doi:10.1016/j.stem.2012.05.007
El Helou R, Wicinski J, Guille A, Adelaide J, Finetti P, Bertucci F, Chaffanet M, Birnbaum D, Charafe-Jauffret E, Ginestier C (2014) Brief reports: a distinct DNA methylation signature defines breast cancer stem cells and predicts cancer outcome. Stem Cells 32(11):3031–3036. doi:10.1002/stem.1792
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353(8):793–802. doi:10.1056/NEJMoa050434
Berman AT, Thukral AD, Hwang WT, Solin LJ, Vapiwala N (2013) Incidence and patterns of distant metastases for patients with early-stage breast cancer after breast conservation treatment. Clin Breast Cancer 13(2):88–94. doi:10.1016/j.clbc.2012.11.001
Balic M, Lin H, Young L, Hawes D, Giuliano A, McNamara G, Datar RH, Cote RJ (2006) Most early disseminated cancer cells detected in bone marrow of breast cancer patients have a putative breast cancer stem cell phenotype. Clin Cancer Res 12(19):5615–5621. doi:10.1158/1078-0432.CCR-06-0169
Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, Bell GW, Richardson AL, Polyak K, Tubo R, Weinberg RA (2007) Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 449(7162):557–563. doi:10.1038/nature06188
Kasai T, Chen L, Mizutani A, Kudoh T, Murakami H, Fu L, Seno M (2014) Cancer stem cells converted from pluripotent stem cells and the cancerous niche. J Stem Cells Regen Med 10(1):2–7
Aggarwal C, Meropol NJ, Punt CJ, Iannotti N, Saidman BH, Sabbath KD, Gabrail NY, Picus J, Morse MA, Mitchell E, Miller MC, Cohen SJ (2013) Relationship among circulating tumor cells, CEA and overall survival in patients with metastatic colorectal cancer. Ann Oncol 24(2):420–428. doi:10.1093/annonc/mds336
Deneve E, Riethdorf S, Ramos J, Nocca D, Coffy A, Daures JP, Maudelonde T, Fabre JM, Pantel K, Alix-Panabieres C (2013) Capture of viable circulating tumor cells in the liver of colorectal cancer patients. Clin Chem 59(9):1384–1392. doi:10.1373/clinchem.2013.202846
Hou JM, Krebs MG, Lancashire L, Sloane R, Backen A, Swain RK, Priest LJ, Greystoke A, Zhou C, Morris K, Ward T, Blackhall FH, Dive C (2012) Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J Clin Oncol 30(5):525–532. doi:10.1200/JCO.2010.33.3716
Krebs MG, Sloane R, Priest L, Lancashire L, Hou JM, Greystoke A, Ward TH, Ferraldeschi R, Hughes A, Clack G, Ranson M, Dive C, Blackhall FH (2011) Evaluation and prognostic significance of circulating tumor cells in patients with non-small-cell lung cancer. J Clin Oncol 29(12):1556–1563. doi:10.1200/JCO.2010.28.7045
Scher HI, Jia X, de Bono JS, Fleisher M, Pienta KJ, Raghavan D, Heller G (2009) Circulating tumour cells as prognostic markers in progressive, castration-resistant prostate cancer: a reanalysis of IMMC38 trial data. Lancet Oncol 10(3):233–239. doi:10.1016/S1470-2045(08)70340-1
Zhang L, Riethdorf S, Wu G, Wang T, Yang K, Peng G, Liu J, Pantel K (2012) Meta-analysis of the prognostic value of circulating tumor cells in breast cancer. Clin Cancer Res 18(20):5701–5710. doi:10.1158/1078-0432.CCR-12-1587
Alix-Panabieres C, Pantel K (2014) Challenges in circulating tumour cell research. Nat Rev Cancer 14(9):623–631. doi:10.1038/nrc3820
Baccelli I, Schneeweiss A, Riethdorf S, Stenzinger A, Schillert A, Vogel V, Klein C, Saini M, Bauerle T, Wallwiener M, Holland-Letz T, Hofner T, Sprick M, Scharpff M, Marme F, Sinn HP, Pantel K, Weichert W, Trumpp A (2013) Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat Biotechnol 31(6):539–544. doi:10.1038/nbt.2576
Aceto N, Bardia A, Miyamoto DT, Donaldson MC, Wittner BS, Spencer JA, Yu M, Pely A, Engstrom A, Zhu H, Brannigan BW, Kapur R, Stott SL, Shioda T, Ramaswamy S, Ting DT, Lin CP, Toner M, Haber DA, Maheswaran S (2014) Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell 158(5):1110–1122. doi:10.1016/j.cell.2014.07.013
Krebs MG, Metcalf RL, Carter L, Brady G, Blackhall FH, Dive C (2014) Molecular analysis of circulating tumour cells-biology and biomarkers. Nat Rev Clin Oncol 11(3):129–144. doi:10.1038/nrclinonc.2013.253
Labelle M, Begum S, Hynes RO (2011) Direct signaling between platelets and cancer cells induces an epithelial–mesenchymal-like transition and promotes metastasis. Cancer Cell 20(5):576–590. doi:10.1016/j.ccr.2011.09.009
Yu M, Bardia A, Wittner BS, Stott SL, Smas ME, Ting DT, Isakoff SJ, Ciciliano JC, Wells MN, Shah AM, Concannon KF, Donaldson MC, Sequist LV, Brachtel E, Sgroi D, Baselga J, Ramaswamy S, Toner M, Haber DA, Maheswaran S (2013) Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science 339(6119):580–584. doi:10.1126/science.1228522
Wels J, Kaplan RN, Rafii S, Lyden D (2008) Migratory neighbors and distant invaders: tumor-associated niche cells. Genes Dev 22(5):559–574. doi:10.1101/gad.1636908
Psaila B, Lyden D (2009) The metastatic niche: adapting the foreign soil. Nat Rev Cancer 9(4):285–293. doi:10.1038/nrc2621
Aktary Z, Pasdar M (2012) Plakoglobin: role in tumorigenesis and metastasis. Int J Cell Biol 2012:189521. doi:10.1155/2012/189521
Todorovic V, Desai BV, Patterson MJ, Amargo EV, Dubash AD, Yin T, Jones JC, Green KJ (2010) Plakoglobin regulates cell motility through Rho- and fibronectin-dependent Src signaling. J Cell Sci 123(Pt 20):3576–3586. doi:10.1242/jcs.070391
Shair KH, Schnegg CI, Raab-Traub N (2008) EBV latent membrane protein 1 effects on plakoglobin, cell growth, and migration. Cancer Res 68(17):6997–7005. doi:10.1158/0008-5472.CAN-08-1178
Rieger-Christ KM, Ng L, Hanley RS, Durrani O, Ma H, Yee AS, Libertino JA, Summerhayes IC (2005) Restoration of plakoglobin expression in bladder carcinoma cell lines suppresses cell migration and tumorigenic potential. Br J Cancer 92(12):2153–2159. doi:10.1038/sj.bjc.6602651
Yin T, Getsios S, Caldelari R, Kowalczyk AP, Muller EJ, Jones JC, Green KJ (2005) Plakoglobin suppresses keratinocyte motility through both cell-cell adhesion-dependent and -independent mechanisms. Proc Natl Acad Sci USA 102(15):5420–5425. doi:10.1073/pnas.0501676102
Kolligs FT, Kolligs B, Hajra KM, Hu G, Tani M, Cho KR, Fearon ER (2000) Gamma-catenin is regulated by the APC tumor suppressor and its oncogenic activity is distinct from that of beta-catenin. Genes Dev 14(11):1319–1331
Hakimelahi S, Parker HR, Gilchrist AJ, Barry M, Li Z, Bleackley RC, Pasdar M (2000) Plakoglobin regulates the expression of the anti-apoptotic protein BCL-2. J Biol Chem 275(15):10905–10911
Shiina H, Breault JE, Basset WW, Enokida H, Urakami S, Li LC, Okino ST, Deguchi M, Kaneuchi M, Terashima M, Yoneda T, Shigeno K, Carroll PR, Igawa M, Dahiya R (2005) Functional loss of the gamma-catenin gene through epigenetic and genetic pathways in human prostate cancer. Cancer Res 65(6):2130–2138. doi:10.1158/0008-5472.CAN-04-3398
Cowin P, Kapprell HP, Franke WW, Tamkun J, Hynes RO (1986) Plakoglobin: a protein common to different kinds of intercellular adhering junctions. Cell 46(7):1063–1073
Knudsen KA, Wheelock MJ (1992) Plakoglobin, or an 83-kD homologue distinct from beta-catenin, interacts with E-cadherin and N-cadherin. J Cell Biol 118(3):671–679
Hu P, Berkowitz P, Madden VJ, Rubenstein DS (2006) Stabilization of plakoglobin and enhanced keratinocyte cell–cell adhesion by intracellular O-glycosylation. J Biol Chem 281(18):12786–12791. doi:10.1074/jbc.M511702200
Fukunaga Y, Liu H, Shimizu M, Komiya S, Kawasuji M, Nagafuchi A (2005) Defining the roles of beta-catenin and plakoglobin in cell–cell adhesion: isolation of beta-catenin/plakoglobin-deficient F9 cells. Cell Struct Funct 30(2):25–34
Lewalle JM, Bajou K, Desreux J, Mareel M, Dejana E, Noel A, Foidart JM (1997) Alteration of interendothelial adherens junctions following tumor cell–endothelial cell interaction in vitro. Exp Cell Res 237(2):347–356. doi:10.1006/excr.1997.3799
Acehan D, Petzold C, Gumper I, Sabatini DD, Muller EJ, Cowin P, Stokes DL (2008) Plakoglobin is required for effective intermediate filament anchorage to desmosomes. J Invest Dermatol 128(11):2665–2675. doi:10.1038/jid.2008.141
Palka HL, Green KJ (1997) Roles of plakoglobin end domains in desmosome assembly. J Cell Sci 110(Pt 19):2359–2371
Ruiz P, Brinkmann V, Ledermann B, Behrend M, Grund C, Thalhammer C, Vogel F, Birchmeier C, Gunthert U, Franke WW, Birchmeier W (1996) Targeted mutation of plakoglobin in mice reveals essential functions of desmosomes in the embryonic heart. J Cell Biol 135(1):215–225
Kirchhof P, Fabritz L, Zwiener M, Witt H, Schafers M, Zellerhoff S, Paul M, Athai T, Hiller KH, Baba HA, Breithardt G, Ruiz P, Wichter T, Levkau B (2006) Age- and training-dependent development of arrhythmogenic right ventricular cardiomyopathy in heterozygous plakoglobin-deficient mice. Circulation 114(17):1799–1806. doi:10.1161/CIRCULATIONAHA.106.624502
Fabritz L, Hoogendijk MG, Scicluna BP, van Amersfoorth SC, Fortmueller L, Wolf S, Laakmann S, Kreienkamp N, Piccini I, Breithardt G, Noppinger PR, Witt H, Ebnet K, Wichter T, Levkau B, Franke WW, Pieperhoff S, de Bakker JM, Coronel R, Kirchhof P (2011) Load-reducing therapy prevents development of arrhythmogenic right ventricular cardiomyopathy in plakoglobin-deficient mice. J Am Coll Cardiol 57(6):740–750. doi:10.1016/j.jacc.2010.09.046
Behrens J, Mareel MM, Van Roy FM, Birchmeier W (1989) Dissecting tumor cell invasion: epithelial cells acquire invasive properties after the loss of uvomorulin-mediated cell–cell adhesion. J Cell Biol 108(6):2435–2447
Vleminckx K, Vakaet L Jr, Mareel M, Fiers W, van Roy F (1991) Genetic manipulation of E-cadherin expression by epithelial tumor cells reveals an invasion suppressor role. Cell 66(1):107–119
Kundu ST, Gosavi P, Khapare N, Patel R, Hosing AS, Maru GB, Ingle A, Decaprio JA, Dalal SN (2008) Plakophilin3 downregulation leads to a decrease in cell adhesion and promotes metastasis. Int J Cancer 123(10):2303–2314. doi:10.1002/ijc.23797
Gosavi P, Kundu ST, Khapare N, Sehgal L, Karkhanis MS, Dalal SN (2011) E-cadherin and plakoglobin recruit plakophilin3 to the cell border to initiate desmosome assembly. Cell Mol Life Sci 68(8):1439–1454. doi:10.1007/s00018-010-0531-3
Parker HR, Li Z, Sheinin H, Lauzon G, Pasdar M (1998) Plakoglobin induces desmosome formation and epidermoid phenotype in N-cadherin-expressing squamous carcinoma cells deficient in plakoglobin and E-cadherin. Cell Motil Cytoskeleton 40(1):87–100. doi:10.1002/(SICI)1097-0169(1998)40:1<87:AID-CM8>3.0.CO;2-C
Li Z, Gallin WJ, Lauzon G, Pasdar M (1998) L-CAM expression induces fibroblast-epidermoid transition in squamous carcinoma cells and down-regulates the endogenous N-cadherin. J Cell Sci 111(Pt 7):1005–1019
Franzen CA, Todorovic V, Desai BV, Mirzoeva S, Yang XJ, Green KJ, Pelling JC (2012) The desmosomal armadillo protein plakoglobin regulates prostate cancer cell adhesion and motility through vitronectin-dependent Src signaling. PLoS ONE 7(7):e42132. doi:10.1371/journal.pone.0042132
Tiwari I, Yoon MH, Park BJ, Jang KL (2015) Hepatitis C virus core induces epithelial–mesenchymal transition in human hepatocytes by upregulating E12/E47 levels. Cancer Lett. doi:10.1016/j.canlet.2015.03.032
Zhurinsky J, Shtutman M, Ben-Ze’ev A (2000) Plakoglobin and beta-catenin: protein interactions, regulation and biological roles. J Cell Sci 113(Pt 18):3127–3139
Karnovsky A, Klymkowsky MW (1995) Anterior axis duplication in Xenopus induced by the over-expression of the cadherin-binding protein plakoglobin. Proc Natl Acad Sci USA 92(10):4522–4526
Bradley RS, Cowin P, Brown AM (1993) Expression of Wnt-1 in PC12 cells results in modulation of plakoglobin and E-cadherin and increased cellular adhesion. J Cell Biol 123(6 Pt 2):1857–1865
Martin ED, Moriarty MA, Byrnes L, Grealy M (2009) Plakoglobin has both structural and signalling roles in zebrafish development. Dev Biol 327(1):83–96. doi:10.1016/j.ydbio.2008.11.036
Spindler V, Dehner C, Hubner S, Waschke J (2014) Plakoglobin but not desmoplakin regulates keratinocyte cohesion via modulation of p38MAPK signaling. J Invest Dermatol 134(6):1655–1664. doi:10.1038/jid.2014.21
Mao X, Li H, Sano Y, Gaestel M, Mo Park J, Payne AS (2014) MAPKAP kinase 2 (MK2)-dependent and -independent models of blister formation in pemphigus vulgaris. J Invest Dermatol 134(1):68–76. doi:10.1038/jid.2013.224
Berkowitz P, Hu P, Liu Z, Diaz LA, Enghild JJ, Chua MP, Rubenstein DS (2005) Desmosome signaling. Inhibition of p38MAPK prevents pemphigus vulgaris IgG-induced cytoskeleton reorganization. J Biol Chem 280(25):23778–23784. doi:10.1074/jbc.M501365200
Tokonzaba E, Chen J, Cheng X, Den Z, Ganeshan R, Muller EJ, Koch PJ (2013) Plakoglobin as a regulator of desmocollin gene expression. J Invest Dermatol 133(12):2732–2740. doi:10.1038/jid.2013.220
Hoverter NP, Waterman ML (2008) A Wnt-fall for gene regulation: repression. Sci Signal 1(39):pe43. doi:10.1126/scisignal.139pe43
Pan H, Gao F, Papageorgis P, Abdolmaleky HM, Faller DV, Thiagalingam S (2007) Aberrant activation of gamma-catenin promotes genomic instability and oncogenic effects during tumor progression. Cancer Biol Ther 6(10):1638–1643
Aktary Z, Pasdar M (2013) Plakoglobin represses SATB1 expression and decreases in vitro proliferation, migration and invasion. PLoS ONE 8(11):e78388. doi:10.1371/journal.pone.0078388
Cohen S, Lee D, Zhai B, Gygi SP, Goldberg AL (2014) Trim32 reduces PI3K-Akt-FoxO signaling in muscle atrophy by promoting plakoglobin-PI3K dissociation. J Cell Biol 204(5):747–758. doi:10.1083/jcb.201304167
Chen YJ, Lee LY, Chao YK, Chang JT, Lu YC, Li HF, Chiu CC, Li YC, Li YL, Chiou JF, Cheng AJ (2013) DSG3 facilitates cancer cell growth and invasion through the DSG3-plakoglobin-TCF/LEF-Myc/cyclin D1/MMP signaling pathway. PLoS ONE 8(5):e64088. doi:10.1371/journal.pone.0064088
Lai YH, Cheng J, Cheng D, Feasel ME, Beste KD, Peng J, Nusrat A, Moreno CS (2011) SOX4 interacts with plakoglobin in a Wnt3a-dependent manner in prostate cancer cells. BMC Cell Biol 12:50. doi:10.1186/1471-2121-12-50
Mathenge EG, Dean CA, Clements D, Vaghar-Kashani A, Photopoulos S, Coyle KM, Giacomantonio M, Malueth B, Nunokawa A, Jordan J, Lewis JD, Gujar SA, Marcato P, Lee PW, Giacomantonio CA (2014) Core needle biopsy of breast cancer tumors increases distant metastases in a mouse model. Neoplasia 16(11):950–960. doi:10.1016/j.neo.2014.09.004
Song GD, Sun Y, Shen H, Li W (2015) SOX4 overexpression is a novel biomarker of malignant status and poor prognosis in breast cancer patients. Tumour Biol. doi:10.1007/s13277-015-3051-9
Aktary Z, Kulak S, Mackey J, Jahroudi N, Pasdar M (2013) Plakoglobin interacts with the transcription factor p53 and regulates the expression of 14-3-3sigma. J Cell Sci 126(Pt 14):3031–3042. doi:10.1242/jcs.120642
Aberle H, Bierkamp C, Torchard D, Serova O, Wagner T, Natt E, Wirsching J, Heidkamper C, Montagna M, Lynch HT et al (1995) The human plakoglobin gene localizes on chromosome 17q21 and is subjected to loss of heterozygosity in breast and ovarian cancers. Proc Natl Acad Sci USA 92(14):6384–6388
McPherson K, Steel CM, Dixon JM (2000) ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ 321(7261):624–628
Boersma BJ, Reimers M, Yi M, Ludwig JA, Luke BT, Stephens RM, Yfantis HG, Lee DH, Weinstein JN, Ambs S (2008) A stromal gene signature associated with inflammatory breast cancer. Int J Cancer 122(6):1324–1332. doi:10.1002/ijc.23237
Korde LA, Lusa L, McShane L, Lebowitz PF, Lukes L, Camphausen K, Parker JS, Swain SM, Hunter K, Zujewski JA (2010) Gene expression pathway analysis to predict response to neoadjuvant docetaxel and capecitabine for breast cancer. Breast Cancer Res Treat 119(3):685–699. doi:10.1007/s10549-009-0651-3
Litvinov SV, Velders MP, Bakker HA, Fleuren GJ, Warnaar SO (1994) Ep-CAM: a human epithelial antigen is a homophilic cell-cell adhesion molecule. J Cell Biol 125(2):437–446
Maetzel D, Denzel S, Mack B, Canis M, Went P, Benk M, Kieu C, Papior P, Baeuerle PA, Munz M, Gires O (2009) Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol 11(2):162–171. doi:10.1038/ncb1824
Galoian K, Qureshi A, Wideroff G, Temple HT (2015) Restoration of desmosomal junction protein expression and inhibition of H3K9-specific histone demethylase activity by cytostatic proline-rich polypeptide-1 leads to suppression of tumorigenic potential in human chondrosarcoma cells. Mol Clin Oncol 3(1):171–178. doi:10.3892/mco.2014.445
Woelfle U, Cloos J, Sauter G, Riethdorf L, Janicke F, van Diest P, Brakenhoff R, Pantel K (2003) Molecular signature associated with bone marrow micrometastasis in human breast cancer. Cancer Res 63(18):5679–5684
Bailey CK, Mittal MK, Misra S, Chaudhuri G (2012) High motility of triple-negative breast cancer cells is due to repression of plakoglobin gene by metastasis modulator protein SLUG. J Biol Chem 287(23):19472–19486. doi:10.1074/jbc.M112.345728
Shafiei F, Rahnama F, Pawella L, Mitchell MD, Gluckman PD, Lobie PE (2008) DNMT3A and DNMT3B mediate autocrine hGH repression of plakoglobin gene transcription and consequent phenotypic conversion of mammary carcinoma cells. Oncogene 27(18):2602–2612. doi:10.1038/sj.onc.1210917
Stajduhar E, Sedic M, Lenicek T, Radulovic P, Kerenji A, Kruslin B, Pavelic K, Kraljevic Pavelic S (2014) Expression of growth hormone receptor, plakoglobin and NEDD9 protein in association with tumour progression and metastasis in human breast cancer. Tumour Biol 35(7):6425–6434. doi:10.1007/s13277-014-1827-y
Holen I, Whitworth J, Nutter F, Evans A, Brown HK, Lefley DV, Barbaric I, Jones M, Ottewell PD (2012) Loss of plakoglobin promotes decreased cell-cell contact, increased invasion, and breast cancer cell dissemination in vivo. Breast Cancer Res 14(3):R86. doi:10.1186/bcr3201
Storci G, Sansone P, Trere D, Tavolari S, Taffurelli M, Ceccarelli C, Guarnieri T, Paterini P, Pariali M, Montanaro L, Santini D, Chieco P, Bonafe M (2008) The basal-like breast carcinoma phenotype is regulated by SLUG gene expression. J Pathol 214(1):25–37. doi:10.1002/path.2254
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, Pietenpol JA (2011) Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121(7):2750–2767. doi:10.1172/JCI45014
Alves CC, Carneiro F, Hoefler H, Becker KF (2009) Role of the epithelial–mesenchymal transition regulator Slug in primary human cancers. Front Biosci (Landmark Ed) 14:3035–3050
Shirley SH, Hudson LG, He J, Kusewitt DF (2010) The skinny on Slug. Mol Carcinog 49(10):851–861. doi:10.1002/mc.20674
Mittal MK, Myers JN, Misra S, Bailey CK, Chaudhuri G (2008) In vivo binding to and functional repression of the VDR gene promoter by SLUG in human breast cells. Biochem Biophys Res Commun 372(1):30–34. doi:10.1016/j.bbrc.2008.04.187
Mittal MK, Singh K, Misra S, Chaudhuri G (2011) SLUG-induced elevation of D1 cyclin in breast cancer cells through the inhibition of its ubiquitination. J Biol Chem 286(1):469–479. doi:10.1074/jbc.M110.164384
Chaffer CL, Weinberg RA (2011) A perspective on cancer cell metastasis. Science 331(6024):1559–1564. doi:10.1126/science.1203543
Chambers AF, Groom AC, MacDonald IC (2002) Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer 2(8):563–572. doi:10.1038/nrc865
Plaks V, Koopman CD, Werb Z (2013) Cancer. Circulating tumor cells. Science 341(6151):1186–1188. doi:10.1126/science.1235226
Labelle M, Begum S, Hynes RO (2014) Platelets guide the formation of early metastatic niches. Proc Natl Acad Sci USA 111(30):E3053–E3061. doi:10.1073/pnas.1411082111
Ringner M, Fredlund E, Hakkinen J, Borg A, Staaf J (2011) GOBO: gene expression-based outcome for breast cancer online. PLoS ONE 6(3):e17911. doi:10.1371/journal.pone.0017911
Fredlund E, Staaf J, Rantala JK, Kallioniemi O, Borg A, Ringner M (2012) The gene expression landscape of breast cancer is shaped by tumor protein p53 status and epithelial–mesenchymal transition. Breast Cancer Res 14(4):R113. doi:10.1186/bcr3236
Acknowledgments
The authors thank the research groups who provide online tool GOBO with the datasets to allow the analyses of gene expression and survival.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lu, L., Zeng, H., Gu, X. et al. Circulating tumor cell clusters-associated gene plakoglobin and breast cancer survival. Breast Cancer Res Treat 151, 491–500 (2015). https://doi.org/10.1007/s10549-015-3416-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3416-1