Abstract
Denosumab increased lumbar spine bone mineral density (BMD) versus placebo in a 2-year, randomized, placebo-controlled, phase 3 study of patients with hormone-receptor-positive, non-metastatic breast cancer and low bone mass who were receiving adjuvant aromatase inhibitor therapy. In subgroup analyses at 12 and 24 months, we evaluated factors (duration and type of aromatase inhibitor, tamoxifen use, age, time since menopause, body mass index, T-score) that might influence BMD at the lumbar spine, total hip, femoral neck, and 1/3 radius. Patients were randomized to receive placebo (n = 125) or 60 mg denosumab (n = 127) subcutaneously every 6 months. In all subgroups, 12 or 24 months’ treatment with denosumab was associated with larger BMD gains than placebo across multiple skeletal sites. Most increases were statistically significant (P < 0.05). Twice-yearly administration of denosumab, regardless of patient subgroup or skeletal site, resulted in consistent increases in BMD versus placebo at 12 and 24 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although tamoxifen has been the standard adjuvant hormone therapy in postmenopausal women with hormone-receptor-positive, early-stage breast cancer, its use has been associated with some uncommon but potentially life-threatening adverse effects including thromboembolic events and endometrial cancer [1, 2]. More recently, adjuvant therapy with aromatase inhibitors (AIs) has demonstrated prolonged disease-free survival and a favourable safety profile compared with tamoxifen [3–6]. Consequently, the American Society of Clinical Oncology has recommended that adjuvant hormonal therapy for postmenopausal women with hormone-receptor-positive, early-stage breast cancer should include an AI [7, 8]. However, AI therapy is associated with bone loss and increased risk of fracture [9–12].
We previously reported the results of a 2-year, randomized, double-blind, placebo-controlled study, which demonstrated that denosumab, a fully human monoclonal antibody to RANKL (receptor activator of nuclear-factor kappa-B ligand), increased bone mineral density (BMD) at the lumbar spine and other skeletal sites, compared with placebo, in patients with hormone-receptor-positive breast cancer who were receiving adjuvant AI therapy and had evidence of low bone mass [13]. It is important to evaluate denosumab in subgroups of the study population to determine the consistency of its skeletal effect and to identify patients for whom denosumab might be of greater or lesser benefit. Patient subgroups were analyzed based on baseline variables that are known risk factors for bone loss, including previous breast cancer treatment (duration and type of AI therapy, prior tamoxifen use) and other patient characteristics (age, time since menopause, baseline body mass index [BMI], and baseline BMD T-score) [14]. Here we present the results of these subgroup analyses of the treatment effect of denosumab at 12 and 24 months on BMD percentage change from baseline at the lumbar spine, total hip, femoral neck, and 1/3 radius.
Patients and methods
Patients
Full inclusion and exclusion criteria have been described previously [13]. Briefly, eligible women were ≥18 years of age with early-stage, histologically or cytologically confirmed, breast cancer that was hormone receptor-positive. All women had completed treatment with surgery and/or radiation and chemotherapy ≥4 weeks before study entry and were undergoing adjuvant AI therapy. At enrollment, all patients were required to have evidence of low bone mass (lumbar spine, total hip [total proximal femur], or femoral neck BMD corresponding to a T-score classification of −1.0 to −2.5). Patients also were required to have serum 25-hydroxyvitamin D levels ≥12 ng/ml. Key exclusion criteria included osteoporosis (T-score < −2.5), prior vertebral fracture, or concurrent anti-neoplastic therapy apart from an aromatase inhibitor.
Study design
This 2-year double-blind, placebo-controlled phase 3 study was conducted at 53 sites in the United States and Canada; a 2-year follow-up period is ongoing. Patients were randomly assigned (1:1) to receive subcutaneous placebo or denosumab 60 mg every 6 months for 4 doses. Randomization, done via interactive voice response system at enrollment, was stratified by duration of prior AI therapy (≤6 months vs. >6 months). All patients were instructed to take calcium (1 g/day) and vitamin D (≥400 IU/day). No change in AI therapy was mandated by study participation, and any change in antineoplastic therapy was at the discretion of the treating physician. The study was conducted according to the Declaration of Helsinki and the International Conference on Harmonisation Tripartite Guideline on Good Clinical Practice. Approvals from appropriate research ethics committees were obtained for each participating study center. All patients provided written informed consent before participating. The primary endpoint was the percentage change from baseline at month 12 in lumbar spine BMD.
BMD assessment
Bone mineral density was measured by dual-energy X-ray absorptiometry (DXA) using Hologic (Hologic Inc., Bedford, MA) or Lunar (General Electric Lunar Corp., Madison, WI) densitometers. Analysis and quality control of all DXA scans were conducted at a central imaging facility (Synarc, Portland, OR), which also calibrated the densitometers across study centers with a set of standard phantoms.
Subgroup analyses
Analyses of percentage change from baseline in BMD at the lumbar spine, total proximal femur (“hip”), femoral neck, and 1/3 radius at 12 and 24 months were done in the following subgroups of patients in both treatment arms: duration and type of AI therapy (≤6, >6 months; steroidal, non-steroidal), prior tamoxifen use (yes, no), age (<65, ≥65 years), time since menopause (≤5, >5 years), baseline BMI (<25, ≥25 kg/m2), and baseline T-score (≤−1.0, >−1.0). Subgroup analyses for the primary endpoint (lumbar spine BMD change from baseline at month 12) were pre-specified; post-hoc subgroup analyses were conducted for the remaining endpoints. Multiplicity adjustment was not used for these analyses.
Subgroup analyses included all randomized patients who had observations for the relevant endpoint at baseline and at least once at or before the relevant time point; the primary imputation method was last observation carried forward.
As in the primary analyses of the study [13], an analysis of covariance (ANCOVA) [15] model was used for subgroup analyses, adjusting for treatment, stratification variable, baseline BMD value, densitometer type, and baseline BMD value-by-densitometer type interaction.
Results
Patients
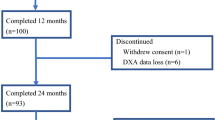
A complete description of patient baseline disease characteristics and disposition has been reported [13]. Overall, baseline characteristics were well balanced between the two treatment groups. The mean age (range) was 59.7 (35–81) years in the placebo arm and 59.2 (38–84) years in the denosumab arm. A total of 252 patients enrolled and received at least one dose of study drug; 125 patients in the placebo group and 127 patients in the denosumab group were included in the subgroup analyses.
Table 1 summarizes the patient baseline characteristics that were examined in the subgroup analyses: duration and type of AI therapy, prior tamoxifen use, age, time since menopause, body mass index, and T-score. The duration of AI therapy was >6 months in 63% of patients in each treatment group. Most patients had received non-steroidal AI therapy (anastrozole or letrozole); only 14 and 11% in the placebo and denosumab groups, respectively, had received steroidal AI therapy (exemestane). Most were <65 years old (67% in placebo, 74% in denosumab) and had been postmenopausal for longer than 5 years (74% in placebo, 72% in denosumab). Other baseline characteristics were reasonably well balanced between treatment groups.
Bone mineral density
As previously reported [13], denosumab treatment was associated with statistically significant gains in lumbar spine BMD, compared with placebo, regardless of duration of AI therapy, the primary stratification variable. Table 2 demonstrates the treatment effect of denosumab (denosumab minus placebo) after 12 months on BMD in other skeletal sites for the seven baseline covariates: duration of AI therapy, type of AI therapy, prior tamoxifen use, age, time since menopause, BMI, and baseline T-score. The observed differences in BMD percentage change from baseline between denosumab and placebo groups were statistically significant (P < 0.05) across all subgroups and skeletal sites, with two exceptions (radial BMD in patients who received prior steroidal AI therapy and femoral neck BMD in patients aged ≥65 years at baseline).
The treatment effect of denosumab on BMD was maintained at 24 months, as shown in Figs. 1 and 2, which display forest plots of the differences in percentage change from baseline between denosumab and placebo in the same subgroups. The observed differences in BMD between denosumab and placebo groups were statistically significant (P < 0.05) across all skeletal sites and subgroups, except for radial BMD in patients who had received steroidal AI therapy.
Forest plots of the treatment effect of denosumab at 24 months in percentage change from baseline (±95% CI) in BMD at the lumbar spine, total hip, femoral neck, and 1/3 radius: by duration of AI therapy (Panel A), type of AI therapy (Panel B), and by prior tamoxifen use (Panel C). Results are presented as least-squares means (ANCOVA models adjusting for treatment, stratification variable, baseline BMD value, machine type, and baseline BMD value-by-machine-type interaction). *P < 0.05 versus placebo
Forest plots of the treatment effect of denosumab at 24 months in percentage change from baseline (±95% CI) in BMD at the lumbar spine, total hip, femoral neck, and 1/3 radius: by age (Panel A), by time since menopause (Panel B), by BMI (Panel C), and by baseline T-score (Panel D). Results are presented as least-squares means (ANCOVA models adjusting for treatment, stratification variable, baseline BMD value, machine type, and baseline BMD value-by-machine-type interaction). *P < 0.05 versus placebo
Safety
The overall safety profile of denosumab compared with placebo has been previously reported [13]. In brief, the incidence of adverse events was similar between treatment groups (91% denosumab, 90% placebo) and most commonly included arthralgia, pain in extremity, back pain, and fatigue. Serious adverse events were reported in 19 denosumab (15%) and 11 placebo (9%) patients. These occurred in 12 system organ classes with no discernible pattern in the type or frequency of event, and none were reported in more than 2 patients.
Discussion
Loss of bone mass is of special concern in patients treated with AIs. Since these agents deplete oestrogen levels and thereby accelerate the loss of bone, women receiving adjuvant AI therapy experience significantly more fractures than those receiving tamoxifen [16]. The prevention of AI-induced bone loss has been the subject of discussions at the American Society of Clinical Oncology, the National Osteoporosis Foundation, and the American Association of Clinical Endocrinologists, all of which have published guidelines and recommendations [7, 8, 14, 17].
The primary analysis of this study showed that denosumab was an effective agent for the management of such bone loss, with an adverse event profile that was similar to that of placebo [13]. It was important next to determine whether the overall benefit of denosumab treatment was influenced by baseline variables that are known risk factors for bone loss. Although the results at any individual skeletal site for any individual variable should be interpreted with caution because of the small subgroup population sizes, the overall findings are consistent. The results of these secondary analyses indicate that the beneficial effect of denosumab was consistent across all the clinical subgroups and skeletal sites evaluated. These findings are similar to those in another study of denosumab in postmenopausal women with low bone mass, in which denosumab significantly increased lumbar spine BMD compared with placebo at 24 months, and in which the effects of denosumab were consistent regardless of time since onset of menopause [18]. Moreover, recent data from a head-to-head study of denosumab and the oral bisphosphonate, alendronate, in postmenopausal women with low bone mass showed significantly greater BMD gains across the skeleton after 1 year of treatment with denosumab, compared with alendronate [19]. The treatment difference observed with denosumab in this study may be due, at least in part, to selective inhibition of RANKL, the primary mediator of osteoclast formation, resorptive function, and survival.
To date, no agent has been approved specifically for the prevention of AI-induced bone loss. The efficacy of bisphosphonates in this setting is being investigated. Several studies have reported that intravenous zoledronic acid, given at an investigational dosing regimen of 4 mg twice-yearly, is effective at increasing BMD in women receiving adjuvant AIs [20–22]. Emerging data from studies with oral bisphosphonates have also shown improvements in BMD [23–25].
In summary, twice-yearly treatment with denosumab was associated with consistently greater gains in BMD than treatment with placebo among women receiving adjuvant AI therapy, regardless of patient subgroup or skeletal site. Two large, phase 3 trials investigating the anti-fracture efficacy and safety of denosumab have recently been completed: one in women with postmenopausal osteoporosis [26] and the other in men with androgen deprivation-induced bone loss. Additional studies of denosumab in the prevention and treatment of cancer-related bone metastases are in progress.
References
Kaufmann M, Jonat W, Hilfrich J et al (2007) Improved overall survival in postmenopausal women with early breast cancer after anastrozole initiated after treatment with tamoxifen compared with continued tamoxifen: the ARNO 95 Study. J Clin Oncol 25:2664–2670. doi:10.1200/JCO.2006.08.8054
Land SR, Wickerham DL, Costantino JP et al (2006) Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP study of tamoxifen and raloxifene (STAR) P-2 trial. JAMA 295:2742–2751. doi:10.1001/jama.295.23.joc60075
Thurlimann B, Keshaviah A, Coates AS et al (2005) A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747–2757. doi:10.1056/NEJMoa052258
Howell A, Cuzick J, Baum M et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62. doi:10.1016/S0140-6736(05)74803-0
Group TAT (2006) Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol 7:633–643. doi:10.1016/S1470-2045(06)70767-7
Coombes RC, Hall E, Gibson LJ et al (2004) A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081–1092. doi:10.1056/NEJMoa040331
Winer EP, Hudis C, Burstein HJ et al (2005) American Society of Clinical Oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J Clin Oncol 23:619–629. doi:10.1200/JCO.2005.09.121
Hillner BE, Ingle JN, Chlebowski RT et al (2003) American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21:4042–4057. doi:10.1200/JCO.2003.08.017
Coates AS, Keshaviah A, Thurlimann B et al (2007) Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1–98. J Clin Oncol 25:486–492. doi:10.1200/JCO.2006.08.8617
Coleman RE, Banks LM, Girgis SI et al (2007) Skeletal effects of exemestane on bone-mineral density, bone biomarkers, and fracture incidence in postmenopausal women with early breast cancer participating in the Intergroup Exemestane Study (IES): a randomised controlled study. Lancet Oncol 8:119–127. doi:10.1016/S1470-2045(07)70003-7
Eastell R, Adams JE, Coleman RE et al (2008) Effect of anastrozole on bone mineral density: 5-year results from the anastrozole, tamoxifen, alone or in combination trial 18233230. J Clin Oncol 26:1051–1057. doi:10.1200/JCO.2007.11.0726
Eastell R, Hannon R (2005) Long-term effects of aromatase inhibitors on bone. Steroid Biochem Mol Biol 95:151–154. doi:10.1016/j.jsbmb.2005.04.009
Ellis GK, Bone HG, Chlebowski R et al (2008) Randomized trial of denosumab in patients receiving adjuvant aromatase inhibitors for non-metastatic breast cancer. J Clin Oncol 26:2874–2882
National Osteoporosis Foundation (2008) Clinician’s guide to prevention and treatment of osteoporosis. Available at http://www.nof.org/professionals/Clinicians_Guide.htm. Accessed 15 January 2009
Longford NT (1993) Random coefficient models. Oxford University Press, Inc., New York
Hadji P, Body JJ, Aapro MS et al (2008) Practical guidance for the management of aromatase inhibitor-associated bone loss. Ann Oncol 19:1407–1416. doi:10.1093/annonc/mdn164
Hodgson SF, Watts NB, Bilezikian JP et al (2003) American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition, with selected updates for 2003. Endocr Pract 9:544–564
Bone HG, Bolognese MA, Yuen CK et al (2008) Effects of denosumab on bone mineral density and bone turnover in postmenopausal women. J Clin Endocrinol Metab 93:2149–2157. doi:10.1210/jc.2007-2814
Brown JP, Prince RL, Deal C et al (2009) Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. J Bone Miner Res 24:153–161. doi:10.1359/jbmr.0809010
Brufsky A, Harker WG, Beck JT et al (2007) Zoledronic acid inhibits adjuvant letrozole-induced bone loss in postmenopausal women with early breast cancer. J Clin Oncol 25:829–836. doi:10.1200/JCO.2005.05.3744
Bundred NJ, Campbell ID, Davidson N et al (2008) Effective inhibition of aromatase inhibitor-associated bone loss by zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: ZO-FAST study results. Cancer 112:1001–1010. doi:10.1002/cncr.23259
Gnant MF, Mlineritsch B, Luschin-Ebengreuth G et al (2007) Zoledronic acid prevents cancer treatment-induced bone loss in premenopausal women receiving adjuvant endocrine therapy for hormone-responsive breast cancer: a report from the Austrian Breast and Colorectal Cancer Study Group. J Clin Oncol 25:820–828. doi:10.1200/JCO.2005.02.7102
Greenspan SL, Brufsky A, Lembersky BC et al (2008) Risedronate prevents bone loss in breast cancer survivors: a 2-year, randomized, double-blind, placebo-controlled clinical trial. J Clin Oncol 26:2644–2652. doi:10.1200/JCO.2007.15.2967
Lester J, Dodwell D, Purohit O et al (2008) Use of monthly oral ibandronate to prevent anastrozole-induced bone loss during adjuvant treatment for breast cancer: two-year results from the ARIBON study [abstract 554]. J Clin Oncol 26:S554
Van Poznak C, Hannon R, Clack G (2007) The SABRE (Study of Anastrozole with the Bisphosphonate RisedronatE) study: 12 month analysis. Breast Cancer Res and Treat 106(suppl 1):S37 abs 502
Cummings SR, McClung MR, Christiansen C et al (2008) A phase III study of the effects of denosumab on vertebral, nonvertebral, and hip fracture in women with osteoporosis: results from the FREEDOM trial [abstract 1286]. J Bone Miner Res 23:S80
Acknowledgments
This study was funded by Amgen Inc., Thousand Oaks, CA. This study is registered with ClinicalTrials.gov with the identifier NCT00089661. GK Ellis is an investigator in this study and has received research grants from Amgen, Abraxis, and Roche, and has been a speaker for Novartis. HG Bone is an investigator for Amgen, Merck, Zelos, Eli Lilly, Novartis, and Nordic Bioscience, and has been a consultant for Amgen, Osteologix, Nordic Bioscience, Merck, Zelos, Pfizer, Novartis, and GlaxoSmithKline; he has received speaker’s honoraria from Novartis. R. Chlebowski has been a consultant for AstraZeneca, Novartis, Genentech, Pfizer, Lilly, and Wyeth; he has received speaker’s honoraria from AstraZeneca, Abraxis, and Novartis. D. Paul and S. Spadafora have no conflicts of interest to disclose. M. Fan and D. Kim are employees of Amgen Inc. We thank Christine Gatchalian, PhD, of Amgen Inc., and Linda Melvin, BA, for writing assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ellis, G.K., Bone, H.G., Chlebowski, R. et al. Effect of denosumab on bone mineral density in women receiving adjuvant aromatase inhibitors for non-metastatic breast cancer: subgroup analyses of a phase 3 study. Breast Cancer Res Treat 118, 81–87 (2009). https://doi.org/10.1007/s10549-009-0352-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0352-y