Abstract
Background
The aim of this study was to investigate the effects of arginine on nutrition, growth and urea cycle function in boys with late-onset ornithine transcarbamylase deficiency (OTCD). Seven Japanese boys with late-onset OTCD enrolled in this study resumed arginine treatment after the cessation of this therapy for a few years. Clinical presentations such as vomiting and unconsciousness, plasma amino acids and urinary orotate excretion were followed chronologically to evaluate urea cycle function and protein synthesis with and without this therapy. In addition to height and body weight, blood levels of proteins, lipids, growth hormone (GH), insulin-like growth factor-I (IGF-I) and IGF-binding protein -3 (IGFBP-3) were monitored.
Results
The frequency of hyperammonemic attacks and urinary orotate excretion decreased significantly following the resumption of arginine treatment. Despite showing no marked change in body weight, height increased gradually. Extremely low plasma arginine increased to normal levels, while plasma glutamine and alanine levels decreased considerably. Except for a slight increase in high-density lipoprotein cholesterol level, blood levels of markers for nutrition did not change. In contrast, low serum IGF-I and IGFBP-3 levels increased to age-matched control levels, and normal urinary GH secretion became greater than the level observed in the controls.
Conclusion
Arginine treatment is able to reduces attacks of hyperammonemia in boys with late-onset OTCD and to increase their growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital urea cycle defects are characterized by hyperammonemia without otherwise profound liver dysfunctions [6, 24]. Encephalopathy caused by hyperammonemia, varying in severity from very mild to extremely severe, has been documented in the literature and the pathophysiology studied extensively [6, 24].
These disorders, with the exception of arginase deficiency, have also been shown to be associated with arginine deficiency [6, 24]. Experiments with animal models have demonstrated that arginine deficiency causes urea cycle dysfunction that can be reversed with arginine treatment [9, 27]. However, the consequences of arginine deficiency in humans have not been fully investigated.
Ammonia-scavenging drugs that remove ammonia via alternative pathways and treatment with arginine (or citrulline) in combination with a low-protein diet have been used to treat patients with these disorders [1, 2, 6, 13, 20–22, 24, 25, 28, 30]. However, it is often difficult to obtain an appropriate balance in the daily diet that will result in normal growth, and precise monitoring of nutritional intake is mandatory [2, 6, 13, 20–22, 24, 30].
Ornithine transcarbamylase deficiency (OTCD; OMIM 311250) is a congenital urea cycle defect and an X-linked dominant trait. It is usually lethal in males with a complete lack of this enzyme [6, 22, 24, 28]. In the past 10 years, we have observed seven boys with OTCD who discontinued arginine treatment and then resumed it several years later.
This report describes the clinical symptoms, growth patterns and nutritional states with and without arginine treatment. The importance of this therapy in the management of late-onset OTCD is discussed.
Subjects and methods
Subjects
Seven boys aged 3–5 years with late-onset OTCD were enrolled in this study (Table 1).
The patients developed the first signs of hyperammonemia at ages ranging from 1 month to 8 months. The diagnoses of OTCD were based on determinations of ornithine transcarbamylase activities in liver biopsy specimens and by gene analyses in addition to clinical manifestations.
After confirmation of the diagnoses, a low-protein diet and pharmacological therapy with sodium benzoate and L-arginine were initiated. Protein intake was restricted to 1.3–2.0 g/kg per day during infancy and thereafter to 0.7–1.1 g/kg per day. Adequate calories corresponding to the requirements of energy for the ages of the patients (1350–1600 kcal), together with adequate minerals and vitamins, were supplied throughout this observation period.
Ammonia-scavenging drugs, such as phenylbutyrate, phenylacetate and sodium benzoate, and arginine or citrulline have been used widely in the pharmacological management of OTCD [1, 2, 6, 13, 20–22, 30]. Recently, a combination of phenylbutyrate and citrulline has been accepted as a standard therapy. Nevertheless, at the time of this study such drugs were not legal in Japan and, consequently, we used sodium benzoate (250 mg/kg per day) and L-arginine (175–220 mg/kg per day) to treat our patients [25, 28].
After the start of therapy, the boys occasionally developed hyperammonemia above the 100 μg/dl of plasma ammonia level in association with vomiting and unconsciousness. The hyperammonemia was resolved by infusions of L-arginine, sodium benzoate and phenylacetate. Within a few years, the boys discontinued arginine treatment because of the unpleasant taste and inadequate understanding by their parents; the frequency of hyperammonemic attacks increased. Following re-education, the boys resumed this therapy.
Study protocol
L-arginine was orally administered at a dose of 55–70 mg/kg three times daily. Height and body weight standard deviation (SD) scores as well as the occurrence of hyperammonemia above 100 mg/dl of plasma ammonia in association with vomiting and unconsciousness were recorded after the start of arginine treatment and before this therapy. Plasma levels of amino acids, including arginine, glutamine, alanine and branched amino acids, were also monitored chronologically. In addition, urinary excretion of orotate, an intermediate of the pyrimidine biosynthetic pathway derived from carbamyl phosphate, was examined.
To assess the nutritional state, serum levels of lipids, including total cholesterol, low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C), together with those of total protein and two rapid turn-over proteins, retinol-binding protein and pre-albumin, were determined at 3 and 0 months before the start of arginine treatment and at 3, 6, 12 and 18 months subsequent to the start of this therapy.
The concentration of growth hormone (GH) in the first urine of the early morning was determined for 5 consecutive days, and the mean GH concentration for each individual calculated [16, 17, 19]. Serum levels of insulin-like growth factor (IGF)-I and IGF binding protein-3 (IGFBP-3) were also determined [8, 15, 17]. For thyroid function, serum levels of free thyroxine (FT4) and thyroid-stimulating hormone (TSH) were determined.
Based on the premise that hypoglycemia induces protein catabolism leading to increased ammonia production, we determined blood sugar after an overnight fasting of 9–9.5 h. Serum levels of total ketone body (TKB) (acetoacetate plus β-hydroxybutyrate) and free fatty acids (FFA) that fluctuate in concert with the fluctuation of blood sugar level were determined simultaneously with those of the blood sugar levels [3, 11].
Age-matched control values were obtained from 17 healthy boys aged 4–6 years. Blood samples from the controls were strictly limited to those after the overnight fasting of 9–9.5 hours; urine samples were also limited to the first urine in the early morning.
This study was approved by an IRB, and parents of all patients and the controls provided written informed consent before the start of this study.
Biochemical assays
Plasma amino acid levels were determined by routine ion-exchange chromatography. The urinary orotate concentration was measured by high performance liquid chromatography according to the method of Brusilow and Hauser and was expressed as micromoles per millimole creatinine [5].
Urinary GH concentration was measured by means of a chemiluminescence enzyme immunoassay using a Hitazyme-CL GH-U kit (Hitachi Chemicals, Tokyo, Japan) and was expressed as picograms per milligram creatinine. Serum levels of IGF-I, IGFBP-3 and TSH were determined by immunoradiometric assays using a Somatomedin C-II kit (Mitsubishi Chemicals, Tokyo, Japan), an IGFBP-3 Eiken kit (Eiken Chemicals, Tokyo, Japan) and an Eiken-TSH- kit (Eiken Chemicals), respectively. The serum FT4 level was determined by a chemiluminescent immunoassay using a Chemilumi-ACS-FT4 kit (Bayer Health Care LLC, New York, N.Y.).
Serum levels of total cholesterol and triglycerides were determined by enzymatic methods using commercial kits (Kyowa Medex, Tokyo, Japan). LDL-C was measured by an enzyme immunoassay using a commercial kit (LDL-C Daiich, Daiichi Pure Chemicals, Tokyo, Japan). High-density lipoprotein cholesterol was determined using 13% polyethylene glycol (PEG 300; Wako Pure Chemical Industries, Osaka, Japan).
Serum levels of FFA and TKB were measured by enzymatic methods using the NEFA-SS kit EIKEN (Eiken Chemicals) and Total Ketone Body kit (Kainos Laboratories, Tokyo, Japan), respectively.
Statistic analysis
Comparisons of values of the age-matched controls with those of patients were performed with Mann-Whitney’s U test, and the significance of changes in patients’ data was assessed by the two-factor ANOVA test. Any p<0.05 was considered significant.
Results
Plasma arginine level before arginine treatment was extremely low in patients with OTCD as compared to those of age-matched controls (p<0.001); subsequent to beginning this therapy, the levels in the patients became higher than those of the controls (p<0.01) (Table 2). Simultaneously, their plasma glutamine and alanine levels fell significantly (p<0.01) but remained higher than those of the controls (p<0.05) (Table 2). In contrast, plasma levels of leucine, isoleucine and valine did not change, with the values remaining lower than the control levels (Table 2).
After the start of this therapy, plasma ammonia level and urinary orotate excretion in the patients also fell significantly (p<0.01) (Table 2).
Arginine treatment reduced the frequency of hyperammonemic attacks. Following 12 months and 18 months of this therapy, the frequency of hyperammonemic attack decreased to one-third of that before the start of this therapy (Fig. 1). Concomitantly, height SD scores increased, although the weight SD scores remained nearly unchanged (Fig. 2).
The two rapid turn-over proteins, retinol-binding protein and prealbumin, remained unchanged throughout the course of treatment, with the levels remaining lower than those in the controls (p<0.01), whereas the total protein levels in the patients were similar to those in the controls (Table 2). The serum HDL-C levels in the patients before the start of this therapy were slightly lower than those in the age-matched controls (p<0.05), while the serum LDL-C levels were similar. At 3 months following the start of the therapy, the HDL-C levels in the patients were similar to those of age-matched controls, whereas the LDL-C levels had remained unchanged (Table 2).
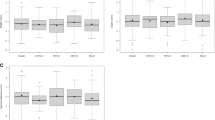
Before the start of the arginine treatment, the serum IGF-I and IGF-BP3 levels in the patients were under the normal ranges obtained from the age-matched healthy controls, while the urinary GH levels in the patients were within the normal range (Fig. 3). At 3 months into the therapy, urinary GH levels had increased significantly (p<0.001), with the levels being over or near the upper limit of the normal range. The serum IGF-I and IGF-BP3 levels in the patients following 3 months of therapy were also higher than those before the start of therapy (p<0.001) and were normal or near the lower limits of the normal ranges. Thereafter, the increased levels of urinary GH and serum IGF-I and IGFBP-3 were observed throughout the course of therapy (Fig. 3). The serum TSH and FT4 levels in the patients remained unchanged, and the values were similar to those in the age-matched controls (data not shown).
Changes in serum levels of insulin-like growth factor (IGF-I) and IGF-binding protein-3 (IGFBP-3) and in urinary growth hormone excretion (U-GH). N Normal ranges. Before the start of arginine treatment, the serum IGF-I and IGF-BP3 levels in the patients were under the normal ranges as determined in 17 healthy boys aged 4–6 years, while their urinary GH levels were within the normal range. At 3 months after the start of therapy, urinary GH levels had increased significantly (p<0.001), and the levels were greater than or near the upper limit of the normal range. Simultaneously, the serum IGF-I and IGF-BP3 levels in the patients were also higher than those before the start of therapy (p<0.001), and the levels were normal or near the lower limits of the normal ranges; thereafter, high levels of IGF-I and IGF-BP3 were observed
The serum TKB and FFA levels in the patients before the start of arginine treatment were lower and higher, respectively, than those in the age-matched controls (p<0.01) (Fig. 4). At 3 months into the therapy, the serum TKB levels had significantly increased (p<0.001) and reached levels close to those found in the controls. In contrast, the FFA levels had decreased significantly by 3 months into the treatment (p<0.001) and were similar to the control levels (Fig. 4). On the other hand, throughout the course of therapy, blood sugar levels in the patients showed no significant changes and remained between 4.2 and 5.2 mmol/l.
Changes in serum free fatty acids (FFA) and total ketone body (TKB) levels in a fasting state. The serum TKB and FFA levels in patients before the start of arginine treatment were lower and higher, respectively, than those in age-matched controls (p<0.01). From 3 months onwards following the start of this therapy, the serum TKB and FFA showed levels close to the respective control levels
Discussion
Arginine is an amino acid found in some proteins. It is produced in the liver and plays an essential role in ureogenesis and, as such, it is plausible that arginine deficiency might influence protein synthesis, growth and development. However, clinical manifestations primarily attributable to arginine deficiency or the pathophysiological significance of arginine deficiency have not been fully investigated in humans. Brislow et al. reported that arginine treatment stimulates protein synthesis in patients with congenital urea cycle defects and that it inhibits the accumulation of ammonia in plasma [4]. Several other reports have described growth disturbances in animal models with arginine deficiency [9]. In addition, the association between arginine deficiency and urea cycle function has been studied, but uniform results have not been obtained [7, 9, 27].
In the management of arginosuccinate lyase deficiency, a urea cycle defect, arginine has often been used without ammonia-scavenging drugs and has been found to exert a substantial effect towards preventing hyperammonemia [10, 29]. On the other hand, in the management of OTCD and carbamyl phosphate synthetase deficiency, a combination of low-protein diet, ammonia-scavenging drugs and arginine (citrulline) has commonly been used. It has therefore been difficult to evaluate the efficacy of arginine in each individual with such disorders [1, 2, 6, 13, 20–22, 24, 25, 28, 30].
The results of the present study revealed that a considerable amount of the nitrogen that had accumulated as ammonia, glutamine and alanine in our OTCD patients was directed to protein synthesis with arginine treatment. It is possible to explain the substantial decreases in the frequency of hyperammonemic attacks and urinary orotate excretion by these changes in the nitrogen balance.
Nutrition and appetite are common problems in the long-term management of patients with urea cycle defects. It is sometimes difficult to achieve normal growth because of inadequate or inappropriate nutrition [2, 6, 13, 20–22, 24, 30].
No significant change in the serum markers for nutrition, except for a minimal change in HDL-C level, was observed in our patients throughout the course of treatment. However, height SD scores improved substantially after the start of this therapy, although weight SD scores did not change significantly. Furthermore, significant increases in serum IGF-I and IGFBP-3 levels along with an increase in urinary GH secretion were observed following the commencement of the therapy. It seems likely that such hormonal changes were associated with an increase in height.
It is known that patients with malnutrition or anorexia nervosa show low serum IGF-I and IGFBP-3 levels without impairment in pituitary GH secretion [8, 15, 17]. Our patients were under protein restriction. Their body weight SD scores and serum levels of markers for their respective nutritional states were lower than those of the controls. Accordingly, we speculated that their low serum IGF-I and IGFBP-3 levels before arginine treatment were attributable mainly to their poor nutritional states. Their normal urinary GH secretions supported this speculation, although urinary GH secretion does not necessarily reflect pituitary GH secretion [19]. Nevertheless, it remains unclear why, despite no significant improvement in nutritional condition, the urinary GH secretion did increase with concomitant increases in serum IGF-I and IGFBP-3 levels with arginine treatment. Intravenous administration of high-dose arginine leading to a rapid and intensive rise in plasma arginine level is known to stimulate pituitary GH secretion [14, 18, 23]. On the other hand, it remains unknown whether GH secretion under a normal basal plasma arginine level and that under an extremely low basal plasma arginine level are different. The present study raises the possibility that arginine treatment is associated with such hormonal changes in patients with late-onset OTCD, but the detailed mechanism remains known.
A significant increase in serum ketone body level, together with a significant decrease in serum FFA level, was also observed following the initiation of therapy. Ketone bodies are generated by fatty acid oxidation, chiefly in mitochondria. Therefore, such changes may be the result of stimulated fatty acid oxidation in mitochondria [3, 11, 26]. A concomitant change in the serum level of carnitine, which is involved in mitochondrial β oxidation, was also observed, thereby supporting this speculation of stimulated fatty acid oxidation in mitochondria (data not shown) [12]. To date, our report is the first to infer stimulated fatty acid oxidation in patients with a urea-cycle defect.
This study has demonstrated that arginine replacement exerts beneficial effects on growth and metabolism in boys with late-onset OTCD.
Abbreviations
- FFA:
-
Free fatty acids
- GH:
-
Growth hormone
- IGF-I:
-
Insulin-like growth factor-I
- IGFBP-3:
-
Insulin-like growth factor binding protein-3
- OTCD:
-
Ornithine transcarbamylase deficiency
- TKB:
-
Total ketone body
- TP:
-
Total protein
References
Batshaw ML, MacArthur RB, Tuchman M (2001) Alternative pathway therapy for urea cycle disorders: twenty years later. J Pediatr 138[Suppl 1]:S46–54, discussion S54–S55
Berry GT, Steiner RD (2001) Long-term management of patients with urea cycle disorders. J Pediatr 138[Suppl]:S56–S60, discussion S60–S61
Bonnefont JP, Specola NB, Vassault A, Lombes A, Ogier H, de Klerk JB, Munnich A, Coude M, Paturneau-Jouas M, Saudubray JM (1990) The fasting test in paediatrics: application to the diagnosis of pathological hypo-and hyperketotic states. Eur J Pediatr 150:80–85
Brusilow SW (1984) Arginine, an indispensable amino acid for patients with inborn errors of metabolism. J Clin Invest 117:2144–2148
Brusilow SW, Hauser E (1989) Simple method of measurement of orotate and orotidine in urine. J Chromatogr 493:388–391
Brusilow SW, Horwich AL (2001) Urea cycle enzymes. In: Scriver CR, Baudet AL, Valle D, Sly WS. The metabolic and molecular bases of inherited disease, 8th edn. McGraw-Hill, New-York, pp 1909–1964
Carey GP, Kime Z, Rogers QR, Morris JG, Hargrove D, Buffington CA, Brusilow SW (1987) An arginine-deficient diet in humans does not evoke hyperammonemia or orotic aciduria. J Nutr 117:1734–1739
Counts DR, Gwirtsman H, Carlsson LM, Lesem M, Cutler GB Jr (1992) The effect of anorexia nervosa and refeeding on growth hormone-binding proteins, the insulin-like growth factors (IGFs), and the IGF-binding proteins. J Clin Endocrinol Metab 75:762–767
Czarnecki GL, Baker DH (1984) Urea cycle function in the dog with emphasis on the role of arginine. J Nutr 114:581–590
Donn SM, Thoene JG (1985) Prospective prevention of neonatal hyperammonemia in arginosuccinic aciduria by arginine therapy. J Inherit Metab Dis 8:18–20
Duran M, Wadman SK (1987) Chemical diagnosis of inherited defects of fatty acid metabolism and ketogenesis (a review). Enzyme 38:115–123
Fingerhut R, Roschinger W, Muntau AC, Dame T, Kreischer J, Arnecke R, Superti-Furga A, Troxler H, Liebl B, Olgemoller B, Roscher AA (2001) Hepatic carnitine palmitoyltransferase I deficiency: acylcarnitine profiles in blood spots are highly specific. Clin Chem 47:1763–1768
Finkelstein JE, Hauser ER, Leonard CO, Brusilow SW (1990) Late-onset ornithine transcarbamylase deficiency in male patients. J Pediatr 117:897–902
Gianotti L, Maccario M, Lanfranco F, Ramunni J, Di Vito L, Grottoli S, Muller EE, Chigo E, Arvat E (2000) Arginine counteracts the inhibitory effect of recombinant human insulin-like growth factor I on the somatotroph responsiveness to growth hormone-releasing hormone in humans. J Clin Endocrinol Metab 85:3604–3608
Gianotti L, Pincelli AI, Scacchi M, Rolla M, Bellitti D, Arvat E, Lanfranco F, Torsello A, Ghigo E, Cavagnini F, Muller EE (2000) Effects of recombinant human insulin-like growth factor I administration on spontaneous and growth hormone (GH)-releasing hormone-stimulated GH secretion in anorexia nervosa. J Clin Endocrinol Metab 85:2805–2809
Girard J, Fischer-Wasels T (1990) Measurement of urinary growth hormone. A noninvasive method to assess the growth hormone status. Horm Res 33[Suppl 4]:12–18
Grottoli S, Gasco V, Ragazzoni F, Ghigo E (2003) Hormonal diagnosis of GH hypersecretory states. J Endocrinol Invest 26:27–35
Hanew K, Utsumi A (2002) The role of endogenous GHRH in arginine-, insulin-, clonidine- and l-dopa-induced GH release in normal subjects. Eur J Endocrinol 146:197–202
Hourd P, Edwards R (1994) Current methods for the measurement of growth hormone in urine (a review). Clin Endocrinol (Oxford) 40:155–170
Leonard JV (2001) The nutritional management of urea cycle disorders. J Pediatr 138[Suppl 1]:S40–S44, discussion S44–S45
Maestri NE, Brusilow SW, Clissold DB, Bassett SS (1996) Long-term treatment of girls with ornithine transcarbamylase deficiency. N Engl J Med 335:855–859
Maestri NE, Clissold DB, Brusilow SW (1999) Neonatal onset ornithine transcarbamylase deficiency: a retrospective analysis. J Pediatr 134:268–272
Merimee TJ, Rabinowtitz D, Fineberg SE (1969) Arginine-initiated release of human growth hormone. Factors modifying the response in normal man. N Eng J Med 280:1434–1438
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits ED (1984) Neurological outcome in children with inborn errors of urea synthesis: outcome of urea-cycle enzymopathies. N Engl J Med 310:1500–1505
Nagasaka H, Komatsu H, Ohura T, Sogo T, Inui A, Yorifuji T, Kei Murayama, Masaki Takayanagi, Hideaki Kikuta, Kunihiko Kobayashi (2004) Nitric oxide synthesis in ornithine transcarbamylase deficiency: possible involvement of low NO synthesis in clinical manifestations of urea cycle defect. J Pediatr 145:259–262
Olpin SE (2004) Implications of impaired ketogenesis in fatty acid oxidation disorders (a review). Prostaglandins Leukot Essent Fatty Acids 70:293–308
Sonoda T, Tatibana M (1983) Purification of N-acetyl-L-glutamate synthetase from rat liver mitochondria and substrate and activator specificity of the enzyme. J Biol Chem 258:9839–9844
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inherit Metab Dis 21[Suppl 1]:151–159
Widhalm K, Koch S, Scheibenreiter S, Knoll E, Colombo JP, Bachmann C, Thalhammer O (1992) Long-term follow-up of 12 patients with the late-onset variant of arginisuccinic acid lyase deficiency: no impairment of intellectual and psychomotor development during therapy. Pediatrics 89:1182–1184
Wilcken B (2004) Problems in the management of urea cycle disorders. Mol Genet Metab 81[Suppl 1]:S86–S91
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagasaka, H., Yorifuji, T., Murayama, K. et al. Effects of arginine treatment on nutrition, growth and urea cycle function in seven Japanese boys with late-onset ornithine transcarbamylase deficiency. Eur J Pediatr 165, 618–624 (2006). https://doi.org/10.1007/s00431-006-0143-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-006-0143-y