Abstract
Bulimic behaviors are frequently associated with alcohol use disorders. However, extant family and twin study findings have been inconsistent with regard to whether these behaviors share etiologic influences. A sample of 292 young adult, female twins was used to examine genetic and environmental factors underlying the association between binge eating and compensatory behaviors (e.g., vomiting) and alcohol use. Binge eating and compensatory behaviors were assessed using the Minnesota Eating Behavior Survey. Alcohol use was measured using the Alcohol Use Disorders Identification Test. Univariate models indicated that the heritability of binge eating, compensatory behaviors, and alcohol use was 41, 28, and 78%, respectively, with the remaining variance due to nonshared environmental effects. Bivariate models indicated that there was a moderate-to-large degree of overlap (genetic correlation = 0.31–0.61) in additive genetic factors between alcohol use and binge eating and compensatory behaviors, and no overlap in environmental effects. Findings suggest that these phenotypes co-aggregate in families and that similar genes or heritable traits may be contributing to their co-occurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals with eating disorders and substance abuse have the highest risk of premature death of the major mental illnesses (Harris and Barraclough 1998). Within eating disorders, alcohol use disorder severity is one of the most significant predictors of mortality among individuals with anorexia nervosa (AN; Keel et al. 2003), and a history of a substance use disorder is associated with a worse outcome for women with bulimia nervosa (BN; Keel et al. 1999). The co-occurrence of eating disorders and alcohol use disorders is also associated with higher rates of attempted suicide (Duncan et al. 2006) and an increased likelihood of major depressive disorder and drug or tobacco dependence (Duncan et al. 2006). Given the deleterious effects of their co-occurrence, it is important to understand the factors underlying the comorbidity of eating disorders and alcohol use disorders.
Among women with eating disorders, alcohol use disorders are more often comorbid with BN or AN, binge-purge type, than AN, restricting type, (Holderness et al. 1994). Therefore, much of the research focus has been on associations between alcohol use disorders and BN, or more generally, bulimic behaviors (e.g., bingeing and purging). Three family studies that have examined associations between BN and alcohol use disorders have found that these disorders co-occur in families, with higher rates of alcohol disorders in BN probands (Bulik 1987; Kassett et al. 1989; Lilenfeld et al. 1997). However, Lilenfeld et al. (1997) found that only family members of BN probands with comorbid alcohol use disorders had higher rates of alcohol use disorders. This suggests possible independent transmission of the disorders, as alcohol use disorders may be transmitted within families in which alcohol use problems are present, regardless of whether BN is present as well.
Twin studies have begun to examine the issue of etiologic overlap to clarify whether familial aggregation or independent transmission is present, as well as to determine whether relationships are due to common genetic and/or environmental factors. Extant twin data suggests that AN and BN are significantly heritable (>50%), with nonshared environmental factors (i.e., factors unique to co-twins that contribute to their behavioral differences) accounting for the remaining variance in these disorders (Bulik et al. 1998, 2006; Klump et al. 2001; Mazzeo et al. 2010). Genetic and nonshared environmental effects have also been found to influence bulimic behaviors, including binge eating, defined as eating a large amount of food in a short period of time with a feeling of lack of control over the binges, and compensatory behaviors, which are behaviors aimed at weight loss that include self-induced vomiting, laxative use, and diuretic use. Yet, findings for bulimic behaviors are somewhat inconsistent with regard to the magnitude of these factors. With few exceptions (i.e., heritability 8–17%; see Wade et al. 2008), several studies indicated that the heritability of binge eating exceeds 40% (Bulik et al. 1998; Sullivan et al. 1998; Bulik et al. 2003; Reichborn-Kjennerud et al. 2004; Klump et al. 2002) and compensatory behavior ranges from 35 to 70%, depending on whether several compensatory behaviors are examined together (heritability = 50%) or specific types of behaviors are examined separately (e.g., laxative use only; heritability = 43%) are examined (Klump et al. 2000; Mazzeo et al. 2010; Sullivan et al. 1998). Nonetheless, in general, each of these studies indicated that these behaviors are heritable with the remaining variance due to nonshared environmental factors.
For alcohol use disorders, large-scale twin studies indicate heritabilities of over 60% in women (Heath et al. 1997; Whitfield et al. 2004) with nonshared environmental factors accounting for the remaining variance. Alcohol use disorder symptoms, such as symptom counts that tally the number of abuse and/or dependence symptoms, have also been found to be heritable with estimates exceeding 50% (Kendler et al. 1992, 1994; Prescott et al. 1999). Overall, findings across eating disorder and alcohol use disorder studies suggest that if familial aggregation between these phenotypes is present, it may be due to significant genetic and/or nonshared environmental factors.
Twin studies are able to investigate this possibility by examining the extent to which phenotypic associations between two disorders are due to genetic and/or environmental factors. Using this method, Kendler et al. (1995) only found evidence for a small genetic overlap (i.e., 6%) between BN and “problem drinking” (i.e., “having had or having been considered by others as having a significant drinking problem that is not limited to single isolated incidents”) in a large sample of middle-aged twins (mean age = 30.1 years, SD = 7.6). Indeed, BN was found to predominately load on a separate genetic factor from problem drinking. Common nonshared environmental influences were similarly small for both disorders. However, it must be noted that Kendler et al.’s (1995) study included several psychiatric disorders which were examined together in the same model to see if a common genetic and environmental factor or several independent genetic and environmental factors influenced the phenotypes. Thus, findings from studies that only examined BN and alcohol use disorders may differ somewhat due to different methodologies and information included in the twin models.
Indeed, recent bivariate studies examining associations between BN and alcohol use disorders only have provided stronger support for shared genetic etiologies, where genetic correlations (i.e., the degree of overlap in genetic factors influencing two phenotypes) ranged from 0.53 to 1.0 (Baker et al. 2010; Mitchell et al. 2010) and nonshared environmental correlations were either small (i.e., −0.03; Baker et al. 2010) and/or non-significant (i.e., confidence intervals overlapped with zero; Mitchell et al. 2010). These findings suggest that the association between BN and alcohol use disorders may be primarily due to shared genetic factors. Nonetheless, the above cited studies are few in number (N = 3), and confidence intervals have been rather broad. Additional research therefore is needed to confirm genetic associations and provide additional point estimates of these shared effects.
Consequently, the purpose of the current study was to investigate genetic and environmental influences on associations between bulimic behaviors and problematic alcohol use in adult female twins. We examined symptoms of BN (i.e., binge eating and the use of compensatory behaviors), which are much more prevalent than BN diagnoses (Crowther et al. 2008; Hudson et al. 2007). These symptoms frequently predate the development of BN (Patton et al. 1999) and have been found to be associated with increased levels of depression and anxiety (Fitzgibbon et al. 1998; Johnson et al. 2002; Mond et al. 2006) in adolescents and adults. Similarly, alcohol abuse or problem drinking is much more prevalent in the population than alcohol dependence (Hasin et al. 2007) and is strongly associated with other forms of psychopathology, including depression (Marmorstein 2009). Thus, in addition to increasing statistical power in the study, symptoms of BN and problematic alcohol use are important phenotypes to examine in their own right.
Methods
Participants
Participants were drawn from the Adult Twin Study of Behavioral Adjustment and Development from the Michigan State University Twin Registry (MSUTR; Klump and Burt 2006), a population-based twin registry focused on understanding risk factors for internalizing and externalizing disorders across the lifespan. Although all MSUTR participants are now recruited through birth records, participants in the current study were also recruited from posted flyers and newspaper advertisements. The participants completed in-person assessments privately in individual computer rooms in the laboratory. Regardless of the recruitment methods used, the twins in the current study have been found to be broadly representative of women in Michigan in terms of racial identification (Culbert et al. 2008).
The current study included 292 female twins (164 monozygotic [MZ]; 128 dizygotic [DZ]) between the ages of 18 and 29 years (mean age = 20.92 years; SD = 2.47). Participants identified as Caucasian (83%), African American (11%), Hispanic (2%), Asian American (1%), or “Other” (3%) ethnicity. Socioeconomic status, measured using the four-factor index of social status (Hollingshead 1975), indicated that the majority of twins were in the middle-to-upper socioeconomic classes (i.e., Level 1 = 28.1%, Level 2 = 44.2%, Level 3 = 18.8%, Level 4 = 4.5%, and Level 5 = 2.4%). This breakdown is broadly representative of the socioeconomic status of similar aged adults in the State of Michigan (www.census.gov 2008).
Zygosity determination
Zygosity was determined using a physical similarity questionnaire shown to be over 95% accurate (Plomin et al. 2008). Decisions about indeterminate zygosity were made by the project’s principal investigators (KLK and SAB) who reviewed questionnaire ratings and waist-up photographs of the twins.
Measures
Bulimic behaviors
The 7-item binge eating and 6-item compensatory behavior subscales from the Minnesota eating behavior survey (MEBS; von Ranson et al. 2005)Footnote 1 were used to assess binge eating and the use of compensatory behaviors. These subscales assess thoughts about overeating or the tendency to binge eat as well several types of compensatory behaviors such as self-induced vomiting and laxative use for weight loss. Items are endorsed as either true (scored as 1) or false (scored as 0), with a sum score for each subscale. The internal consistency of the binge eating and compensatory behavior scales has been adequate in women in past research (von Ranson et al. 2005) as well as in the current sample (α = 0.75 and 0.65, respectively). Discriminant validity also has been previously established through the ability of these subscales to differentiate between normal control participants and women with eating disorders (von Ranson et al. 2005).
Importantly, the present sample exhibited a range of pathology on these measures. Specifically, binge eating scores ranged from 0 to 7 and compensatory behavior scores ranged from 0 to 6, with mean scores of 1.56 (SD = 1.76) and 0.51 (SD = 0.97), respectively. Corresponding means for these scales among clinical samples with eating disorders are 2.53 for the binge eating scale and 1.53 for the compensatory behavior scale (von Ranson et al. 2005). Notably, 22% (n = 65/290) of women scored a 3 or higher on the binge eating scale, and 31% (n = 89/290) endorsed engaging in one or more compensatory behaviors. This suggests that approximately 1/3 of the sample endorses in these behaviors at or above the average level of endorsement for clinical samples (von Ranson et al. 2005).
Problematic alcohol use
The 10-item alcohol use disorders identification test (AUDIT; Saunders et al. 1993) was used to assess harmful and hazardous amounts of alcohol use. The AUDIT items assess alcohol consumption (i.e., “How often do you have a drink containing alcohol”), drinking behavior (i.e., “How often during the last year have you found that you were not able to stop drinking once you had started”), adverse reactions (i.e., “How often during the last year have you had a feeling of guilt or remorse after drinking”), and problems related to alcohol use (i.e., “Have you or someone else been hurt as a result of your drinking”). Total scores range from 0 (non-hazardous consumption) to 40 (the highest severity of hazardous consumption). A score of 8 or higher indicates a strong likelihood that the person is engaging in harmful alcohol consumption. Twenty-two percent (n = 62) of women in the present sample had scores of 8 or higher on the AUDIT.
In a study of nearly 1,000 male and female undergraduates, the AUDIT displayed internal consistency reliability of 0.80 (Fleming et al. 1991). Discriminant validity was established by comparing male and female non-drinkers to individuals with alcohol dependence, with 0.5% of the non-drinkers and 99% of the individuals with alcohol dependence scoring over 8 on the AUDIT (Saunders et al. 1993). The AUDIT exhibited good internal consistency in this sample (α = 0.82) and scores ranged from 0 to 24 with a mean of 4.48 (SD = 4.73).
Body mass index
Body mass index (BMI; weight [kg]/height2 [m]) was calculated using height and weight measured using a wall-mounted ruler and digital scale, respectively. Participants were asked to remove their shoes and heavy outerwear before the measurements.
Statistical analyses
Data preparation and descriptive statistics
Log transformations (log10 X + 1) were performed for the body mass index, compensatory behavior, and AUDIT scores in order to account for positive skew. Although binge eating was slightly positively skewed, the skewness and kurtosis were within −2 and 2, suggesting that a transformation was not necessary prior to analysis (see Lewis-Beck et al. 2004). BMI was regressed out of binge eating, compensatory behavior, and AUDIT scores prior to analysis in order to determine whether influences underlying associations between bulimic behaviors and problematic alcohol use were independent of BMI.Footnote 2
Genetic and environmental influences on bulimic behaviors and problematic alcohol use
Twin correlations
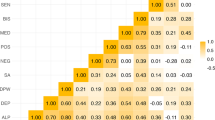
Two types of twin correlations were calculated to provide initial indications of genetic and environmental influences on bulimic behaviors and problematic alcohol use separately, as well as on the association between these phenotypes. Both types of correlations (i.e., twin intraclass and cross-twin, cross trait) were calculated using the double-entry method to remove the variance associated with the ordering of siblings within a pair. Twin intraclass correlations (e.g., Twin 1’s binge eating with Twin 2’s binge eating) were first calculated for binge eating, compensatory behavior, and problematic alcohol use. These correlations were used to provide indications of genetic and environmental factors on each phenotype individually. Cross-twin, cross-trait correlations (e.g., Twin 1’s binge eating with Twin 2’s problematic alcohol use) were then calculated to provide indications of genetic and environmental influences on phenotypic associations between bulimic behaviors and problematic alcohol use. For both types of correlations, greater MZ than DZ twin correlations suggest that additive genetic effects (i.e., the effect of individual genes summed over loci that increase twin similarity relative to the amount of genes shared) influence the trait or phenotypic association in question. By contrast, similar MZ and DZ twin correlations suggest that shared environmental (i.e., the part of the environment common to siblings that acts to make them similar to each other) factors are important. Finally, nonshared environmental (i.e., environmental factors, and measurement error, differentiating twins within a pair) influences are implicated if the MZ twin correlations are less than 1.00.
Univariate twin models
Univariate twin models were fit to raw data using the maximum likelihood option in Mx (Neale et al. 2003) to examine additive genetic (A), shared environmental (C), and nonshared environmental (E) influences on binge eating, compensatory behaviors, and problematic alcohol use, separately. The raw data option in Mx considers missing data to be missing at random and can lead to less biased estimates than pairwise or list wise deletion (Little and Rubin 1987). When fitting models to raw data, their variances, covariances, and means are first freely estimated to get a baseline index of fit (minus twice the log-likelihood; −2lnL). The −2lnL under this unrestricted baseline model is then subtracted from the −2lnL under more restrictive biometric models. This result is a likelihood-ratio Chi-square test of goodness of fit for the model (χ2), which is then used to calculate the Akaike’s information criterion (Akaike 1987), AIC = χ2 − 2df, the traditional fit index of behavioral genetics research. The AIC measures model fit relative to parsimony. Better fitting models have lower AIC values. In addition to the AIC, the χ2 difference test can also be used as a measure of model fit. The χ2 difference test examines changes in Chi-square values and degrees of freedom between nested models. If the Chi-square difference test is nonsignificant, then the most parsimonious (i.e., reduced) model is preferred. Using this approach, the full ACE model was compared to several submodels (i.e., AE, CE, and E) to ascertain whether a reduced model provided a better fit to the data.
Bivariate models
Bivariate models (see Fig. 1) were then fit to raw data using Mx (Neale et al. 2003) to examine additive genetic, shared environmental, and nonshared environmental influences on associations between bulimic behaviors and problematic alcohol use. These influences were investigated through genetic and environmental correlations that quantify overlap in genetic and environmental factors between the phenotypes. The genetic (ra), shared environmental (rc), and nonshared environmental (re) correlations indicate the degree of overlap in genetic factors, shared environmental factors, and nonshared environmental factors, respectively, influencing each phenotype. Thus, these correlations estimate the extent to which a common set of genes and/or environmental factors contribute to phenotypic associations between two traits/behaviors.
Path diagram of the bivariate model examining bulimic behaviors and alcohol use. Variance estimates are comprised of additive genetic (A), shared environmental (C), and nonshared environmental (E) effects, including: (1) genetic and environmental influences on alcohol use (a11, c11, e11); (2) genetic and environmental influences on bulimic behaviors (a22, c22, e22); (3) genetic (ra), shared environmental (rc), and nonshared (re) environmental correlations that examine the degree of overlap in genetic and environmental factors between bulimic behaviors and alcohol use. Alcohol Use P1 = Alcohol Use as Phenotype 1; BN beh. P2 = Bulimic behaviors as Phenotype 2
Similar to the univariate models, we initially estimated variances, covariances, and means of the bulimic behaviors and problematic alcohol use to determine a baseline fit (−2lnL) of the data. The −2lnL under this unrestricted baseline model was then compared with −2lnL under more restrictive biometric models. This comparison provides a likelihood-ratio Chi-square test of goodness of fit for the model, which is then converted to the AIC. The AIC and changes in χ2 were used to examine model fit. Additional submodels, based on the best-fitting univariate models, were then fit to the data to examine whether constraining the genetic, shared, or nonshared environmental correlations to 0 would provide a better fit to the data. These models tested whether there is statistically significant overlap in genetic/environmental influences on bulimic behaviors and problematic alcohol use.
Results
Univariate models
Twin intraclass correlations suggested significant genetic, but no shared environmental, influences, on binge eating, compensatory behavior, and problematic alcohol use (see Table 1). That is, in all cases, MZ correlations were nearly double the DZ correlations. Additionally, nonshared environmental factors also appeared important for all three phenotypes, as the MZ twin correlations were less than 1.00.
Univariate twin models confirmed these impressions. The best fitting model for binge eating, compensatory behavior, and problematic alcohol use was the AE model (see Table 2). This model had the lowest AIC and did not provide a significantly worse fit to the data than the full ACE model for each phenotype. Genetic factors were the highest for problematic alcohol use, with parameter estimates of 78% for genetic influences and 22% for nonshared environmental effects. Binge eating had the second highest heritability of 41%, with the remaining variance accounted for by nonshared environment. Compensatory behaviors were accounted for, in part, by genetic factors (i.e., 28%) with the remaining variance attributed to nonshared environmental effects (i.e., 72%).
Notably, the heritability estimate for compensatory behaviors is somewhat lower than what might be suggested by the intraclass twin correlations (see Table 1). We tested whether this was due to our modeling of compensatory behavior on a continuous rather than a categorical scale. When a univariate twin model is conducted using a categorical compensatory behavior variable (i.e., 0–6 with no transformations), the variance due to genetic effects (i.e., 0.23–0.38, depending on the constraints used in the model) fell within the range of the heritability estimate in the continuous univariate model (i.e., 0.28). Given the relative similarity in the magnitude of these effects, and the difficulty of accounting for BMI using a categorical compensatory behavior variable, we retained the continuous compensatory behavior variables in all analyses.
Bivariate models
Within-person, phenotypic associations between BN behaviors and problematic alcohol use were statistically significant and in the small-to-moderate range (see Table 1). Cross-twin, cross trait correlations revealed that these phenotypic associations were likely mediated by common genetic factors. Higher MZ relative to DZ cross-twin, cross-trait correlations were observed between binge eating and problematic alcohol use, as well as between compensatory behavior and problematic alcohol use, suggesting the presence of genetic influences on relationships between these phenotypes.
Results from the bivariate models are presented in Table 3. The AE model with re constrained to 0 provided the best fit to the data for associations between binge eating and problematic alcohol use as well as compensatory behavior and problematic alcohol use. These models evidenced a non-significant Δχ2 (see Table 3) relative to the baseline model, and a lower AIC than the AE model or the AE submodel with ra constrained to 0. Parameter estimates for the best-fitting AE model with re constrained indicated some overlap (ra = 0.31) in additive genetic factors between binge eating and problematic alcohol use, and a larger overlap (ra = 0.61) for compensatory behavior and problematic alcohol use.
Discussion
The current investigation examined etiologic associations between bulimic behaviors (i.e., binge eating and compensatory behaviors) and problematic alcohol use in an effort to clarify past discrepant results regarding shared/independent transmission of these commonly comorbid phenotypes. Each behavior was separately influenced by genetic and nonshared environmental factors. However, associations between bulimic behaviors and problematic alcohol use appeared to be entirely mediated by common genetic rather than nonshared environmental factors. This suggests that the phenotypes do, in fact, aggregate in families, and that similar genes or heritable traits may be contributing to the co-occurrence of these disorders.
At the univariate level, we examined genetic and environmental influences on all three phenotypes, controlling for BMI. Heritabilities were 41, 28, and 78% for binge eating, compensatory behaviors, and problematic alcohol use, respectively, with the remaining variance due to nonshared environmental effects. These estimates are within the ranges found in previous research (Bulik et al. 1998, 2003; Kendler et al. 1992, 1994; Klump et al. 2000; Mazzeo et al. 2010; Prescott et al. 1999; Reichborn-Kjennerud et al. 2004; Sullivan et al. 1998) and suggest that between 1/4 and 3/4 of the variance in individual differences in these phenotypes is due to genetic effects.
Bivariate twin models extended our univariate results by indicating that common genetic factors primarily influence associations between binge eating and problematic alcohol use (ra = 0.31) and compensatory behaviors and problematic alcohol use (ra = 0.61). Findings support those of Baker et al. (2010) and Mitchell et al. (2010) who found that shared genetic factors underlie associations between BN and alcohol use disorders. Our results complement and add to this work by showing that shared genetic factors are present for bulimic behaviors/problematic alcohol use symptoms, and by highlighting the fact that genetic overlap appears to be greater for problematic alcohol use and compensatory behaviors than it is for problematic alcohol use and binge eating. Taken together, these data suggest that etiologic associations between BN and problematic alcohol use disorders may be carried largely by associations with compensatory behaviors. One way to examine this possibility would be to compare genetic overlap between alcohol use disorders and BN to alcohol use disorders and purging disorder (i.e., a diagnosis that is characterized by the use of compensatory behaviors in the absence of binge eating; Keel et al. 2005). Based on findings in our study, we would expect stronger etiologic associations between alcohol use disorders and purging disorder than BN. Notably, in one study, women with purging disorder had higher current and lifetime rates of substance use disorders than women with BN and controls (Keel et al. 2005).
Future research should examine the mechanisms that might account for greater phenotypic and genetic associations between problematic alcohol use and compensatory behaviors than problematic alcohol use and binge eating. One potential explanation for this difference is impulsivity. Previous studies have indicated that women exhibiting bulimic pathology tend to score higher on measures of impulsivity compared to women with AN, restricting type, and controls (Cassin and von Ranson 2005). More specifically, however, a recent study of women exhibiting bulimic pathology found that higher levels of novelty seeking (a measure of impulsivity) was predictive of purging, but not binge eating (Wade et al. 2008). Further, extant research has found a significant genetic correlation between impulsivity and the use of compensatory behaviors (ra = −0.23; note that correlation is negative due to low scores on the scale indicating high impulsivity; Klump et al. 2002). Notably, Klump et al. (2002) did not examine genetic associations between impulsivity and binge eating due to a nonsignificant phenotypic correlation between the scales. Emerging data from our lab replicates these findings by showing a higher genetic correlation between impulsivity and compensatory behavior (ra = 0.37) than impulsivity and binge eating (ra = 0.17; Spanos et al. in preparation).
Importantly, impulsivity is associated with alcohol use disorders both cross-sectionally and prospectively (Sher et al. 2000) and predicts early initiation of alcohol (McGue et al. 2001) as well as frequency and quantity of use (Grau and Ortet 1999). Therefore, it may be that stronger phenotypic and genetic associations between problematic alcohol use and compensatory behavior are due to impulsivity as a “third variable” underlying both phenotypes. It is unclear why impulsivity might be more strongly linked phenotypically and genetically to compensatory behavior rather than binge eating. However, given the emerging data, this is an important area of research to pursue along with seeing if the impulsivity link underlies differential associations between problematic alcohol use, compensatory behavior, and binge eating.
Despite the potential importance of these findings for understanding in the comorbidity between bulimic behaviors and problematic alcohol use, some limitations must be noted. First, the sample size was relatively small, which may have decreased the power and precision in detecting genetic effects. However, none of the confidence intervals in the best-fitting models overlapped with zero, suggesting that we had adequate power to detect significant etiologic effects. Nonetheless, additional research with larger samples of female twins is needed to confirm our results.
Second, the internal consistency was only adequate for binge eating and compensatory behavior (α = 0.75 and 0.65, respectively). However, both interview and self-report questionnaires have been found to produce similar heritability estimates in twin studies (see Bulik et al. 1998; Sullivan et al. 1998; Reichborn-Kjennerud et al. 2004; Klump et al. 2002), despite clinical interviews being considered the “gold standard” for diagnosing bulimia nervosa (Fairburn and Beglin 1994). Nonetheless, future research should examine these phenotypes using clinical interviews to determine whether findings can be replicated.
Third, the majority of our twins were not entirely through the period of risk for the development of clinical eating disorders (i.e., through age 25) or alcohol use disorders (i.e., 20s to mid-30s; American Psychiatric Association 2000). Notably, however, the symptoms assessed typically predate the development of clinical eating disorders (Patton et al. 1999) and alcohol dependence (Conigrave et al. 1995) and so would be expected to be present even in “at risk” individuals. Indeed, research suggests that the “peak risk” of onset is 16 years old for binge eating and 18 years old for purging symptoms (Stice et al. 1998). The present sample has an age range of 18–29 years with a mean age of 21; thus, the majority of participants are past the age of “peak risk” for these symptoms. Further, the AUDIT measure was specifically developed to identify individuals with problematic alcohol use before they develop more severe problems, such as alcohol dependence (Saunders et al. 1993). Thus, even though our subjects have not passed the peak period of risk for eating disorders and alcohol use disorders, findings are still informative for the types of symptoms that put individuals at risk for more severe eating and alcohol problems.
Finally, the direction of genetic associations between binge eating and problematic alcohol use, as well as compensatory behavior and problematic alcohol use, cannot be determined in our study, as our data were cross-sectional. Future research should examine prospective associations between these bulimic behaviors and problematic alcohol use in twins in order to further understand the direction and nature of the genetic and environmental associations.
Notes
The Minnesota eating behavior survey (MEBS; previously known as the Minnesota Eating Disorder Inventory (M-EDI)) was adapted and reproduced by special permission of Psychological Assessment Resources, Inc., 16204 North Florida Avenue, Lutz, Florida 33549, from the Eating Disorder Inventory (collectively, EDI and EDI-2) by Garner, Olmstead, Polivy, Copyright 1983 by Psychological Assessment Resources, Inc. Further reproduction of the MEBS is prohibited without prior permission from Psychological Assessment Resources, Inc.
Analyses using raw MEBS subscales and the AUDIT score did not differ from those with BMI regressed out.
References
Akaike H (1987) Factor analysis and AIC. Psychometrika 52:317–332.
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn (text revision) American Psychiatric Press, Washington
Baker JH, Mitchell KS, Neale MC, Kendler KS (2010) Eating disorder symptomatology and substance use disorders: Prevalence and shared risk in a population based twin sample. Int J Eat Disord 43:648–658
Bulik CM (1987) Drug and alcohol abuse by bulimic women and their families. Am J Psychiatry 144:1604–1606
Bulik CM, Sullivan PF, Kendler KS (1998) Heritability of binge-eating and broadly defined bulimia nervosa. Biol Psychiatry 44:1210–1218
Bulik CM, Sullivan PF, Kendler KS (2003) Genetic and environmental contributions to obesity and binge eating. Int J Eat Disord 33:293–298
Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL (2006) Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry 63:305–312
Cassin SE, von Ranson KM (2005) Personality and eating disorders: a decade in review. Clin Psychol Rev 25:895–916
Conigrave KM, Saunders JB, Reznik RB (1995) Predictive capacity of the AUDIT questionnaire for alcohol-related harm. Addiction 90:1479–1485
Crowther JH, Armey M, Luce KH, Dalton GR, Leahey T (2008) The point prevalence of bulimic disorders from 1990 to 2004. Int J Eat Disord 41:491–497
Culbert KM, Breedlove SM, Burt SA, Klump KL (2008) Prenatal hormone exposure and risk for eating disorders. Arch Gen Psychiatry 65:329–336
Duncan AE, Neuman RJ, Kramer JR, Kuperman S, Hesselbrock VM, Bucholz KK (2006) Lifetime psychiatric comorbidity of alcohol dependence and bulimia nervosa in women. Drug Alcohol Depend 84:122–132
Fairburn CG, Beglin SJ (1994) Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord 16:363–370
Fitzgibbon ML, Spring B, Avellone ME, Blackman LR, Pingitore R, Stolley MR (1998) Correlates of binge eating in hispanic, black, and white women. Int J Eat Disord 24:43–52
Fleming MF, Barry KL, MacDonald R (1991) The alcohol use disorders identification test (AUDIT) in a college sample. Int J Addict 26:1173–1185
Grau E, Ortet G (1999) Personality traits and alcohol consumption in a sample of non-alcoholic women. Pers Indiv Differ 27:1057–1066
Harris EC, Barraclough B (1998) Excess mortality of mental disorder. Br J Psychiatry 173:11–53
Hasin DS, Stinson FS, Ogburn E, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Arch Gen Psychiatry 64:830–842
Heath AC, Bucholz KK, Madden PAF, Dinwiddie SH, Slutske WS, Bierut LJ et al (1997) Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychol Med 27:1381–1396
Holderness CC, Brooks-Gunn J, Warren MP (1994) Co-morbidity of eating disorders and substance abuse review of the literature. Int J Eat Disord 16:1–34
Hollingshead AB (1975) Four factor index of social status. Yale University Sociology Department, New Haven
Hudson JI, Hiripi E, Pope HG Jr, Kessler RC (2007) The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiatry 61:348–358
Johnson WG, Rohan KJ, Kirk AA (2002) Prevalence and correlates of binge eating in white and African American adolescents. Eat Behav 3:179–189
Kassett JA, Gershon ES, Maxwell ME, Guroff JJ, Kazuba DM, Smith AL et al (1989) Psychiatric disorders in the first-degree relatives of probands with bulimia nervosa. Am J Psychiatry 146:1468–1471
Keel PK, Mitchell JE, Miller KB, Davis TL, Crow SJ (1999) Long-term outcome of bulimia nervosa. Arch Gen Psychiatry 56:63–69
Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DL, Herzog DB (2003) Predictors of mortality in eating disorders. Arch Gen Psychiatry 60:179–183
Keel PK, Haedt A, Edler C (2005) Purging disorder: an ominous variant of bulimia nervosa? Int J Eat Disord 38:191–199
Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ (1992) A population-based twin study of alcoholism in women. J Am Med Assoc 268:1877–1882
Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ (1994) A twin-family study of alcoholism in women. Am J Psychiatry 151:707–715
Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ (1995) The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Phobia, generalized anxiety disorder, panic disorder, bulimia, major depression, and alcoholism. Arch Gen Psychiatry 52:374–383
Klump KL, Burt SA (2006) The Michigan State University Twin Registry (MSUTR): genetic, environmental, and neurobiological influences on behavior across development. Twin Res Hum Genet 9:971–977
Klump KL, McGue M, Iacono WG (2000) Age differences in genetic and environmental influences on eating attitudes and behaviors in preadolescent and adolescent female twins. J Abnorm Psychol 109:239–251
Klump KL, Miller KB, Keel PK, McGue M, Iacono WG (2001) Genetic and environmental influences on anorexia nervosa syndromes in a population-based twin sample. Psychol Med 31:737–740
Klump KL, McGue M, Iacono WG (2002) Genetic relationships between personality and eating attitudes and behaviors. J Abnorm Psychol 111:380–389
Lewis-Beck MS, Bryman A, Liao TF (2004) The SAGE encyclopedia of social science research methods, 5th vol. SAGE publications, Thousand Oaks
Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C et al (1997) Psychiatric disorders in women with bulimia nervosa and their first-degree relatives: effects of comorbid substance dependence. Int J Eat Disord 22:253–264
Little RJA, Rubin DB (1987) Statistical analysis with missing data. Wiley, New York
Marmorstein NR (2009) Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol Clin Exp Res 33:49–59
Mazzeo SE, Mitchell KS, Bulik CM, Aggen SH, Kendler KS, Neale MC (2010) A twin study of specific bulimia nervosa symptoms. Psychol Med 40:1203–1213
McGue M, Iacono WG, Legrand LN, Malone S, Elkins IJ (2001) Origins and consequences of age at first drink. I. Associations with substance-use disorders, disinhibitory behavior, psychopathology, and P3 amplitude. Alcohol Clin Exp Res 25:1156–1165
Mitchell KS, Neale MC, Bulik CM, Aggen SH, Kendler KS, Mazzeo SE (2010) A twin model investigation of the comorbidity of bulimia nervosa and alcohol use disorders. Eating Disorders Research Society Annual Meeting, Cambridge
Mond J, Hay P, Rodgers B, Owen C, Crosby R, Mitchell J (2006) Use of extreme weight control behaviors with and without binge eating in a community sample: Implications for the classification of bulimic-type eating disorders. Int J Eat Disord 39:294–302
Neale MC, Boker SM, Xie G, Maes HH (2003) Mx: statistical modeling, 6th edn. Department of Psychiatry, Virginia Commonwealth University, Richmond
Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R (1999) Onset of adolescent eating disorders: population based cohort study over 3 years. Br Med J 318:765–768
Plomin R, DeFries JC, McClearn GE, McGuffin P (2008) Behavioral genetics, 5th edn. Worth Publishers, New York
Prescott CA, Aggen SH, Kendler KS (1999) Sex differences in the sources of genetic liability to alcohol abuse and dependence in a population-based sample of U.S. twins. Alcohol Clin Exp Res 23:1136–1144
Reichborn-Kjennerud T, Bulik CM, Tambs K, Harris JR (2004) Genetic and environmental influences on binge eating in the absence of compensatory behaviors: a population-based twin study. Int J Eat Disord 36:307–314
Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M (1993) Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction 88:791–804
Sher KJ, Bartholow BD, Wood MD (2000) Personality and substance use disorders: a prospective study. J Consult Clin Psychol 68:818–829
Spanos A, Klump KL, Burt SA, McGue, M, Iacono WG Same beast or different animals? Examining differential etiologic associations between impulsivity and binge eating and compensatory behavior (in preparation)
Stice E, Killen JD, Hayward C, Taylor CB (1998) Age of onset for binge eating and purging during late adolescence: A 4-year survival analysis. J Abnorm Psychol 107:671–675
Sullivan PF, Bulik CM, Kendler KS (1998) Genetic epidemiology of binging and vomiting. Br J Psychiatry 173:75–79
United States Census Bureau (2008) Michigan median household income. Retrieved from www.census.gov
von Ranson KM, Klump KL, Iacono WG, McGue M (2005) The Minnesota eating behavior survey: a brief measure of disordered eating attitudes and behaviors. Eat Behav 6:373–392
Wade TD, Treloar S, Martin NG (2008) Shared and unique risk factors between lifetime purging and objective binge eating: a twin study. Psychol Med 38:1455–1464
Whitfield JB, Zhu G, Madden PAF, Neale MC, Heath A, Martin NG (2004) The genetics of alcohol intake and of alcohol dependence. Genetics and molecular biology. Alcohol Clin Exp Res 28:1153–1160
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by Yoon-Mi Hur.
Rights and permissions
About this article
Cite this article
Slane, J.D., Burt, S.A. & Klump, K.L. Bulimic Behaviors and Alcohol Use: Shared Genetic Influences. Behav Genet 42, 603–613 (2012). https://doi.org/10.1007/s10519-012-9525-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10519-012-9525-2