Abstract
We created a model conceptualizing sexual risk as a series of discrete event-specific behavioral decisions and tested the hypothesis that marijuana use was associated with increased sexual risk-taking. Three hundred eight marijuana-using women aged 18–24 completed a 90-day time-line-follow-back to assess sexual behaviors and marijuana use. A sequential logit model estimated the effect of marijuana use on the likelihood of being sexually active, partner type when sexually active, and condom nonuse conditional on partner type. Participants had a mean age of 20.4 years, with 67% Caucasian. Marijuana use was associated with an increased likelihood of being sexually active (OR 1.6; 95% CI 1.33, 1.93) and with condom nonuse when sexually active with casual partners (OR 2.58; 95% CI 1.1, 6.09). This behavioral decision model identified where marijuana use affected sexual risk, and suggests where interventions designed to reduce risk may have an impact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HIV and other sexually transmitted infections (STI) continue to present a critical public health challenge. Weinstock et al. [1] estimated that there were 18.9 million new cases of STI in 2000; about 9.1 million of which were among persons aged 15–25. The burden is especially notable among young women. Adolescent females are more likely to contract STIs than adolescent males [2] and are at greater risk of severe health consequences, such as infertility, from common STIs such as chlamydia and gonorrhea [3]. Additionally, more common STIs can increase the risk of acquiring HIV [4]. With respect to HIV, women under the age of 25 have experienced the largest proportionate increase in AIDS cases over the past 15 years [5].
Several studies have linked marijuana, the most frequently used illicit drug in the United States, with increased sexual risk [6–8]. About 51.3% of women aged 18–25 report having ever smoked marijuana and 13.6% report using marijuana monthly or more frequently [9]. Marijuana use has been associated with increased sexual activity [10, 11] and this seems especially true among women [6]. In a longitudinal study [12], Guo et al. reported that monthly use of marijuana in adolescence was a significant predictor of number of sex partners and inconsistent condom use at age 21. Kingree et al. [13] found positive and significant global and situational associations between unprotected sexual intercourse and marijuana use. De Geena et al. [14] found that having STIs was associated significantly with both early age (<15 years) of initiating marijuana use and current marijuana use. Kingree and Phan [15], conducting an event-specific analysis in which they examined the association between marijuana and condom use the first time participants had been sexually active with their current partner, reported that marijuana was associated with condom nonuse among younger, but not older, adolescent detainees. But not all findings have been consistent. Leigh et al. [16] for example, found that condom use was not associated significantly with marijuana use during the most recent sexual encounter. And although Brodbeck et al. [17] found that cannabis users reported more sexual risk behavior over a 12-month period in a sample of young heterosexual adults, they found no association between marijuana and condom use in an event-level analysis.
Sexual risk behavior studies have traditionally relied on participant self-reports to identify predictors of sex-risk and to evaluate the effectiveness of interventions designed to reduce the risk of acquiring or transmitting HIV and other STIs. Prior reports have discussed both the complexity of conceptualizing risky sexual behaviors (most often measuring condom use or nonuse as a surrogate indicator of safer (riskier) behavior) and the pragmatic difficulties of empirically measuring this construct. Different measurement strategies can generate different conclusions. Noar et al. [18] noted the lack of a gold standard in a review article evaluating condom use measurement in 56 studies; they identified 72 measures of condom use in the studies they reviewed.
Based on a review of 116 studies, Schroder et al. [19] discussed methodological and analytical challenges when using self-reported condom use as an indicator of sexual risk behavior; they identified and compared two broad classes of measurement strategies. Count measures give the absolute frequency of unprotected sex and directly assess the number of potential exposures to HIV and other STIs, but do not describe an individual’s overall pattern of sexual activity or condom use [19–22]. A second general strategy assesses the relative frequency or proportion of total sexual activity in which condoms are used. Measures of relative frequency provide useful information about individuals’ propensity to practice safe sex when sexually active but often fail to directly assess actual exposure risk to HIV and other STIs because they confound the frequency of sexual activity and the frequency of condom use. Although both are intended to summarize person level sexual behaviors, Schroder et al. [19] demonstrated that correlations between measures of absolute and relative frequency may be weak or even negative.
Because STIs and HIV are common in substance-using populations, researchers must make decisions not only about how best to measure condom use, but also how to interpret the association between substance use and sexual risk-taking. Published “global correlation” studies have generally found that summary measures of individuals’ alcohol use and sexual activity or sexual risk-taking to be positively associated at the person level [23]. However, these studies fail to conclusively demonstrate temporal order, and as Leigh and Stall [24] noted, such global correlations may be the spurious result of unmeasured and uncontrolled individual differences.
Other authors rely on event level reports that focus on the use or non-use of condoms during specific sexual encounters. This might be the first sexual encounter, the most recent sexual encounter, or the first sexual encounter with one’s most recent sexual partner. In a meta-analysis of studies examining condom use in specific sexual episodes, Leigh [25] reported that alcohol use was associated with condom nonuse in first sexual encounters, but not in recent sexual encounters or recent sexual encounters with new partners. An important limitation of this approach is that these analyses are event-specific and may not accurately represent the individual’s typical or usual behaviors.
Alternatively, researchers may use daily diary [26, 27] or time-line-follow-back (TLFB) [28, 29] methods to collect information about all of the sexual encounters individuals experience during a specific period of time. Designs allowing the analysis of multiple event-specific data offer two important advantages. One is that they allow the use of time-varying covariates which are specific to the event. Secondly, these within-person analyses involving time-varying covariates effectively control for individual characteristics that vary between subjects. For example, Leigh et al. [27] examined the effect of alcohol use prior to sexual activity on condom use during sexual encounters and found no association between alcohol and condom use when sexually active. Stein et al. [29] examined differences in the likelihood of being sexually active and sexual risk behaviors on alcohol and non-alcohol use days and reported no significant association between condom use and alcohol use on days when sexually active, however they did find that alcohol increased the overall likelihood of being sexually active, and therefore the overall likelihood of having unprotected sex on days when alcohol was used. We believe such inconsistencies can be better understood by conceptualizing and modeling sexual risk as a behavioral process.
We present a model conceptualizing sexual activity as a process characterized by discrete event-specific behavioral decisions. The behavioral decisions considered here are whether to be sexually active or not, choice of partner type (main or casual), and condom use or nonuse. As a process these serial behavioral decisions create a pathway in which individuals are exposed to varying levels of risk for contracting or transmitting STIs. A potential advantage of this approach is that it will allow investigators to identify the specific points in the behavioral process at which external factors such as substance use may be associated with risk. Such information can be useful in identifying potential targets of intervention. This approach can provide a clearer understanding of how interventions impact behaviors exposing individuals to different levels of risk. Additionally, the model we describe also demonstrates how factors that impact early behavioral decisions (e.g., the propensity to be sexually active) can impact overall sexual risk even when they have no direct effect on behaviors more proximate to infection transmission (i.e., use or non-use of condoms). We illustrate how this model can be operationalized by testing the hypothesis that marijuana use is associated with increased sexual risk-taking.
Procedures
We used baseline data from an ongoing randomized clinical trial testing the effect of a brief, motivationally focused intervention in a cohort of sexually active females aged 18–24. The primary objectives of the trial were to test whether this intervention decreases use of marijuana and risky sexual behaviors. Additionally, the trial was designed to test the hypothesis that reductions in marijuana use would mediate the effect of intervention on sex-risk behaviors.
We recruited 308 females from the community using flyers posted on college campuses and at community agencies, with radio advertisements, and with advertisements posted on public buses. Our flyers and advertisements used the following wording: “Women between 18 and 24, have you used marijuana during the past 3 months? You may be eligible to participate in a research study about the health behaviors of young adults. Participation is completely confidential. Eligible participants receive: compensation for interviews, and free STD testing.” In addition to being a current marijuana user, inclusion criteria were: (1) English speaking, (2) ages 18–24, (3) having had heterosexual intercourse on at least one occasion in the past 3 months, and (4) living within 20 miles of Providence RI and planning to stay in the geographic area for the next 6 months. Women were excluded if they were pregnant, were unable to provide the names of two verifiable contact persons who could assist in locating them for follow-up assessments, were unable to provide a mailing address, or if they met criteria for dependence on substances other than marijuana, alcohol, or nicotine.
Of the 1,690 women screened, 513 met eligibility criteria; 1,015 women were excluded because they had smoked marijuana on fewer than three occasions in the past 90 days, 90 because they had not been sexually active in the last 3 months, 63 because they were unable to provide sufficient information on the screen to determine eligibility, and 9 because they did not meet secondary study eligibility (e.g., pregnant, non-English speaking). One hundred seventy (33.1%) of the 513 eligible participants refused or were unable to enroll in the clinical trial. The study protocol, including the informed consent was approved by the institutional review boards of Butler Hospital, Rhode Island Hospital, and Women & Infants Hospital; 343 women were consented. An additional 35 participants were determined to be ineligible for study participation at the baseline assessment resulting in a sample size of 308 women. Participants were paid $30 for completing the baseline assessment.
Measures
The valid, reliable time line follow-back (TLFB) methodology [30] was used to assess sexual behaviors during the 90-day period prior to baseline. For each day participants reported if they had vaginal or anal sex. For each sexual episode participants were asked about use or nonuse of condoms and partner type. A “main” partner was defined as “someone that you have sex with and you consider this person to be the person that you are serious about.” “Casual” partners were defined as “anyone that you have sex with but you do not consider this person to be a main partner to you. This person can be someone you have had sex with only once, or a few times, or you have sex with them on an on-going, casual basis. The important thing, however, is that this person is not a main partner.” For each day, a participant’s sexual behavior was classified into one of five categories; not sexually active, protected sex with main partner, unprotected sex with main partner, protected sex with casual partner, and unprotected sex with casual partner. Only very rarely did participants report multiple sex risk behaviors on the same day. When this occurred, participants were assigned to the highest risk category ordered as unprotected sex with casual partner > unprotected sex with main > protected sex with casual > protected sex with main.
Marijuana and alcohol use are dichotomous time-varying covariates also assessed using TLFB methods. For each day of the TLFB participants were asked if they used marijuana (1 = yes) and/or alcohol (1 = yes). The quantity of marijuana and alcohol used on each day was not assessed. Other covariates assessed included age in years, race (1 if Caucasian), education (1 if some college or completed college), employment status (1 if full-time or regular part-time), and any cocaine use in the 90-days prior to baseline (1 if yes). Additionally, because personality characteristics such as sensation-seeking and impulsivity have been cited as potentially confounding the association between substance use and sexual risk-taking [27], we included a 5-item impulsivity index [31] as an additional control variable.
Analytical Methods
We report means, counts, and percentages to describe the characteristics of this cohort. To explicate the event-specific process model of sexual risk-taking, we present a figure giving the average daily probability of each behavioral decision observed in this sample. The effects of daily marijuana use, daily alcohol use, and selected covariates on the likelihood of each behavioral decision are estimated with a sequential logit model [32, 33]. This model is closely related to the continuation ratio logit model [34] and the sequential response model [35] and uses a logistic response to simultaneously estimate the effect of the included predictor variables on the probability of each discrete behavioral decision. The model assumes that there is a unique path through which each final outcome can be reached. Furthermore, the model implies that an estimate of the final outcome probabilities can be described as the product of decision probabilities on the path leading to the outcome.
In the current application there are four discrete behavioral decisions, each is represented as a separate prediction equation. The first is the likelihood of being sexually active on any given day, the second is the likelihood of partner type conditional on being sexually active, and the third and fourth decisions involve the likelihood of using a condom conditional on being sexually active with main or casual partners, respectively. The Wald χ2-statistic tests the null hypothesis that the 4 coefficients associated with each predictor variable are simultaneously equal to 0. Rejection of this null hypothesis indicates the corresponding predictor variable has a significant effect on the behavioral process leading to the terminal outcomes. Interpretation of coefficients for each equation directly parallels an ordinary logistic regression model.
Here we report exponentiated coefficients giving the estimated effect of each predictor on the expected odds of each of the four behavioral decisions. Tests of significance and 95% confidence interval estimates are based on robust standard error estimators adjusted for within subject clustering. The model was fit using the seqlogit module [33] in Stata 10.1 [36].
To illustrate more fully the influence of marijuana use on sexual risk, we also report differences in the predicted probabilities of each behavioral decision on days when marijuana was and was not used. We chose to express the behavioral decision effects in terms of predicted probabilities because they are easily interpretable. While effects expressed as changes in the expected odds of an outcome are constant across the values of all covariates, effects expressed as differences in predicted probabilities are not. That is, the predicted probabilities are direct functions of the estimated model parameters, the effect of any one variable (e.g., marijuana use or nonuse) expressed as a difference in the probability of a dichotomous sexual behavior decision (e.g., sexually active or not sexually active) is contingent on the value of all other variables included in the model. The probabilities we report here were evaluated by fixing other covariates to the following values: age and impulsivity were set to their respective means, while categorical variables were fixed to Caucasian race, no college, not employed, no recent cocaine use, and no alcohol use. This is not to say that participants did not use cocaine or alcohol, or that the model excludes such persons; rather, we fixed these covariates to present a single example. Setting any of the covariates to different values (e.g., cocaine (yes) or alcohol (yes)) would change the values of the specific sexual behavior probabilities we report, but importantly, the logit model is such that particular covariate choices would have no effect on the odds ratios relating marijuana use to each behavioral decision.
Results
Participants averaged 20.4 (SD = 1.74) years of age, 206 (66.9%) were Caucasian, 35 (11.4%) were African-American, 34 (11.0%) were Hispanic, and 33 (10.7%) were of other ethnic origins (Table 1). About two-thirds (67.2%) had some college or more, and 188 (61.0%) were employed full- or part-time. Most participants (96.5%) were never married. The mean age of initiating marijuana use was 14.8 (SD = 2.2, Mdn = 15) years. On average, participants used marijuana on 51.2 (SD = 30.4, Mdn = 50.5) days during the reporting period; alcohol was used less frequently (Mean = 18.7, SD = 16.3, Mdn = 14).
Overall, the 308 participants were observed for a total of 28,198 person days. With respect to final sex-risk outcomes, participants were not sexually active on 20,518 (72.8%) days, they had protected sex with a main partner on 1,481 (5.3%) days, unprotected sex with main partners on 5,647 days, protected sex with casual partners on 363 days, and unprotected sex with casual partners on 189 days. Twenty-two (7.1%) participants reported only protected sex with a main partner, 167 (54.2%) had no casual partners but said they had unprotected sex with a main partner on at least 1 occasion, 65 (21.1%) reported having protected sex with a casual partner, and 54 (17.5%) had unprotected sex with a casual partner one or more times.
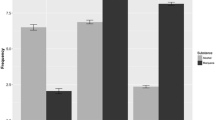
Figure 1 gives the decision probabilities and final outcome probabilities observed in the 308 women. Each decision represents a different behavior and together these represent alternative behavioral paths leading to five final sex-risk outcomes. On any given day (or more generally any given time period) individuals may have protected sex with a main partner, unprotected sex with a main partner, protected sex with a casual partner, unprotected sex with a casual partner, or they may not be sexually active. The initial decision is whether or not individuals are sexually active. In this cohort, the probability of being sexually active on any given day was 0.270. On days when sexually active the observed probabilities of sex with main and casual partners were 0.928 and 0.072, respectively. The final behavioral decisions considered here involve the use or nonuse of condoms in specific events; participants used condoms on 20.8% of the days they were sexually active with main partners, and on 65.6% of days they were sexually active with casual partners.
At each decision the probabilities of alternative behaviors sum to 1.0 and the probabilities of the final outcomes sum to 1.0. Additionally, the final outcome probabilities can be obtained as the product of the probabilities on the behavioral path leading to that outcome. For example, the probability of unprotected sex with a main partner is (0.270 × 0.928 × 0.792) = 0.198. This implies that factors influencing behaviors at early decisions can have profound impacts on final outcomes, even if all subsequent decision probabilities remain constant. Assume that a factor (say marijuana use) increased probability of being sexually active from 0.270 to 0.500 and that this same factor was unrelated to partner type or condom use within partner type. Now the probability of having unprotected sex with casual partners would increase from 0.007 to 0.012 and the probability of having unprotected sex with main partners would increase from 0.198 to 0.367. These differences in probabilities may appear small but they represent 1.72 and 2.35 fold increases in the odds of having unprotected sex with a casual partner and main partners, respectively.
Results from the sequential logit model are reported in Table 2. Age (Wald χ2 = 12.20, df = 4, P = 0.016), educational attainment (Wald χ2 = 19.55, df = 4, P = 0.0001), use of alcohol (Wald χ2 = 43.15, df = 4, P < 0.001), and use of marijuana (Wald χ2 = 22.49, df = 4, P < 0.0001) had statistically significant overall impacts on the process of sexual risk-taking. Adjusting for other covariates included in the prediction model, the expected odds of being sexually active is about 1.60 (z = 4.94, P < 0.001) times higher on days when marijuana was used. Use of marijuana was not associated significantly with partner type on days when sexually active (OR = 1.18, z = 0.60, P = 0.551), nor was it associated significantly with the likelihood of having unprotected sex when sexually active with main partners (OR = 0.88, z = −0.63, P = 0.527). However, on days when participants were sexually active with casual partners, the expected odds of having unprotected sex was 2.58 times higher (a = 2.17, P = 0.03) on days when marijuana was used.
Use of alcohol was also positively and significantly associated with the likelihood of being sexually active; adjusting for marijuana use and other covariates the odds of being sexually active was estimated to be 1.46 times higher (z = 4.45, P < 0.001) on days when alcohol was used. Alcohol use was also associated significantly with partner type (z = 2.35, P = 0.019); participants were about 1.61 times more likely to have a casual partner on alcohol use days. Alcohol use was not associated significantly with condom nonuse with either main (OR = 1.15, z = 0.86, P = 0.387) or casual (OR = 0.079, z = −0.82, P = 0.412) sex partners. The marijuana by alcohol use interaction effect was not significant (Wald χ2 = 7.15, df = 4, P = 0.128).
Age was not associated significantly with the likelihood of being sexually active (OR = 1.04, z = 1.02, P = 0.306) or with the partner type (OR = 0.92, z = −0.83, P = 0.409). However, on days when sexually active with main partners the expected likelihood of condom nonuse increased by a factor of 1.29 (z = 3.45, P = 0.001) for each year of age. The likelihood of being sexually active was also associated significantly with educational attainment. Compared to women with no college education, the expected odds of being sexually active was 0.57 times lower among women with at least some college education (z = −3.91, P < 0.001). Wald χ2-tests indicated that race (Wald χ2 = 8.50, df = 4, P = 0.075), employment status (Wald χ2 = 2.57, df = 4, P = 0.633), impulsivity (Wald χ2 = 5.13, df = 4, P = 0.274), and recent cocaine use (Wald χ2 = 2.73, df = 4, P = 0.605) were not associated significantly with the overall sexual-risk-taking process.
The sequential logit model presented in Table 2 implies differences in the predicted probability of each behavioral decision and in the probability of each final outcome. Figure 2 gives the predicted probability of each decision, and the predicted probability of the five terminal outcomes, on days when marijuana was and was not used. As noted earlier, to calculate these probabilities the values of other predictors in the model were set to the following values: Race (Caucasian), college (no) employed (no) recent cocaine use (no) years age (20.4), impulsivity (10.99), and alcohol use (no). Figure 2 illustrates that marijuana use was associated with the decision probabilities at two points. The probability of being sexually active was about 0.285 on days when marijuana was used compared with 0.200 on non-use days (this corresponds to an odds ratio of 1.6 as reported for the first equation in Table 2). On days when sexually active, the expected probability of being sexually active with main and casual partners were similar on days when marijuana was and was not used. We also note that on days when participants were sexually active with main partners the expected probabilities of having unprotected sex was similar regardless of marijuana use. But on days when participants were sexually active with casual partners the probability of having unprotected sex was considerably higher when marijuana was used (0.587) than on days when marijuana was not used (0.355) (this corresponds to an odds ratio of about 2.58 as reported in the last equation of Table 2).
Figure 2 also shows that the increased probability of sexual activity on marijuana use days impacts the probabilities of the terminal risk outcomes. On marijuana use days the expected probability of having unprotected sex with a casual partner was 0.011 compared with 0.004 on days when marijuana was not used. This difference represents a 2.77 fold increase in the expected odds of having unprotected sex with casual partners. Although the association between marijuana and condom use was small and not statistically significant on days when participants were sexually active with main partners, the increased likelihood of being sexually active on marijuana use days results in a somewhat higher expected probability of having unprotected sex with main partners (0.193 versus 0.141); this corresponds to a 1.46 fold increased in the expected odds of having unprotected sex with main partners.
Discussion
We present a simple model conceptualizing sexual risk-taking as a series of discrete event-specific behavioral decisions. Further, we demonstrate how this model can be operationalized by estimating the extent to which marijuana use is associated with increased sexual risk-taking among young adult women.
Our findings indicate that women in this cohort have a higher probability of unprotected sexual intercourse on days when marijuana was used. Although based on an event level analysis, our findings are generally consistent with earlier reports that marijuana users have higher levels of sexual activity and/or higher levels of unprotected sexual intercourse [7, 10–12, 17]. In this cohort the likelihood of having anal or vaginal intercourse was about 1.6 times higher on days when marijuana was used. We found that partner type was largely independent of marijuana use on days when participants were sexually active. We also found that the association between condom and marijuana use behaviors was contingent on partner type. On days when sexually active with main partners, the association between condom use and marijuana use was substantively small and not significant statistically. Nonetheless, because of the increased likelihood of being sexually active we found the probability of having unprotected sex with a main partner was elevated on days when marijuana was used. Marijuana use was strongly associated with condom nonuse on days participants had sex with casual partners. This finding is inconsistent with findings reported by Leigh et al. [16] who found that marijuana use was not associated with condom use at the most recent sexual episode with a casual partner. Brodbeck et al. [17] also reported that marijuana and condom use were unrelated in an event level analysis. Other event level analyses, however, have found condom nonuse associated with use of marijuana [8, 13, 15, 37]. More research is needed to explicate the conditions and populations in which marijuana and condom non-use are associated.
Several theories have been proposed to account for the relationship between sexual risk-taking behaviors and substance use in general and marijuana use in particular. A pharmacological model suggests that marijuana directly affects the central nervous system and promotes high-risk behaviors by impairing judgment and reducing inhibitions [38, 39]. Associations between substance use and sexual risk-taking behaviors may also reflect underlying individual characteristics such as impulsivity, sensation seeking, or low self-control that predispose individuals to engage in a range of high-risk behaviors. Though such an explanation is less plausible when applied to event-specific analyses than analyses which rely on global associations, we included a measure of impulsivity as a statistical control and found no evidence that it explains away the association between marijuana use and the likelihood of sexual activity or the increased likelihood of condom non-use with casual partners.
Participants in this cohort were significantly more likely to be sexually active, and significantly more likely to be sexually active with casual sex partners, on days when alcohol was used. But we found alcohol was not a factor in the use or nonuse of condoms on days when sexually active with either main or casual partners. Does this mean alcohol is not associated with increased exposure to STIs as a result of unprotected intercourse? No. Our analysis shows that the increased probability of being sexually active on alcohol use days manifested itself in a higher probability of having unprotected sexual intercourse with both main and casual partners. Conceptualizing and operationalizing sexual activity as an event-specific process characterized by discrete behavioral decisions may also help explicate the role alcohol may play in sexual risk. One advantage of this type of model is that it may help resolve the seeming inconsistency between global association studies that have found higher levels of sexual risk-taking behaviors among individuals who use alcohol more heavily and event-specific analyses [27, 29, 40] that have generally found that alcohol was not associated with condom nonuse when analysis focused on specific sexual episodes.
A second potential advantage of this model is that conceptualizing sexual risk-taking as a series of discrete behavioral decisions can enhance our understanding of how interventions and educational programs work, or fail to work. Individual differences, participants’ social and physical environments, and substance use may influence sex risk by perturbing the process at different decision points. Our findings suggest that marijuana affects both likelihood of sexual activity and condom use with casual partners. Therefore, we would expect a marijuana use reduction intervention, applied to a similar population, would reduce both sexual activity and condom use with casual partners, but would not affect partner choice or condom use with main partners. Alternatively, investigators might consider an intervention designed to increase condom use. Hypothetically, such an intervention could potentially impact the risk process in contradictory ways. It might increase the likelihood of condom use when sexually active, but it could also have the unintended consequence of increasing sexual activity (people feel safer). The result might be that there is no net change in the probability of unprotected sexual intercourse. In this case, count measures giving the absolute frequency of unprotected sex may mask behavioral changes that are occurring at different points in the behavioral process.
The basic approach we present can readily be extended to capture more fully the rich complexity of sexual risk-taking behavior. We recognize that the discrete behavioral decision model presented herein reflects the simplicity of the available daily data used to reach alternative sex-risk outcomes. Although they represent varying degrees of STI transmission risk, we did not distinguish between vaginal and anal sex, and did not ask about oral sex in the TLFB. We only distinguished between main and casual partners and did not include detailed information regarding partner characteristics. For instance, partners’ use of alcohol or drugs may have influenced participants’ propensity for condom use [41]. Clearly, partners’ sexual behaviors and current STI status represent very different levels of the actual infection risk to which these participants were exposed. We have no measures assessing the integrity with which condoms were used in episodes of protected sex. With sufficient data such extensions can more realistically represent the processes contributing to sexual risk-taking. We believe the approach presented here provides a dynamic though incomplete framework that can be extended in numerous directions in future research.
An additional limitation of the current study was its reliance on self-reports of marijuana, alcohol, and sexual behaviors. Though reliance on self-reports is widely used to assess sexual-risk-taking and substance use, it should be noted that such measures may be subject to recall error and social desirability bias. A third study limitation was that for each day assessed by the TLFB, participants were asked about their use of marijuana, alcohol, and sexual behaviors. The TLFB requires respondents to recall a 90 day period and heavy alcohol or marijuana use may impair the ability to report accurately. Participants were not explicitly asked if marijuana or alcohol use occurred prior to, during, or after sexual activity. Thus the design did not unambiguously establish the temporal order between substance use and sexual intercourse. Fourth, we recruited a non-treatment seeking convenience sample of sexually active young adult women reporting recent marijuana use. While representing a population at relatively high risk for STIs, generalizations to other populations must await confirmation by additional empirical research. Finally, our model uses the term “behavioral decision” by which we mean that individuals can engage in alternative behaviors. We recognize that these behaviors may not always be volitional. For instance, women may put themselves at risk for violence by suggesting condom use to their partners, or feel coerced to not use condoms with specific partners.
In conclusion, we found that use of marijuana and alcohol independently contributed to STI risk as indicated by a higher daily probability of having unprotected sexual intercourse. The event-specific behavioral decision model presented herein helps explicate the processes through which substance use may impact STI risk. Our findings demonstrate how marijuana use that impacts overall sexual activity can, all else being equal, impact exposure to sexual risk even when substance use may have no direct impact on behaviors such as condom use which are more proximate to risk. We encourage future researchers to extend the approach by including more detailed data regarding sex-risk behaviors. We believe that viewing sexual risk-taking behaviors as a dynamic process can help reconcile many extant empirical inconsistencies and further an understanding of the way in which factors may influence STI risk. Such modeling can help better evaluate the effectiveness of behavioral interventions and educational programs intended to reduce the risk of STI transmission.
References
Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36(1):6–10.
CDC. Trends in reportable sexually transmitted diseases in the United States, 2004. Atlanta, GA: U.S. Department of Health and Human Services; 2005.
CDC. Trends in reportable sexually transmitted diseases in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services; 2009.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17.
Centers for Disease Control and Prevention. HIV and AIDS—United States, 1981–2000. MMWR. 2001;50:430–4.
Turner C, Russell A, Brown W. Prevalence of illicit drug use in young Australian women, patterns of use and associated risk factors. Addiction. 2003;98(10):1419–26.
Poulin C, Graham L. The association between substance use, unplanned sexual intercourse and other sexual behaviors among adolescent students. Addiction. 2001;96(4):607–21.
Kingree JB, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug Alcohol Depend. 2003;72(2):197–203.
Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-34, DHHS Publication No. SMA 08-4343): Rockville, MD; 2008.
Lowry R, Holtzman D, Truman BI, Kann L, Collins JL, Kolbe LJ. Substance use and HIV-related sexual behaviors among US high school students: are they related? Am J Public Health. 1994;84(7):1116–20.
Shrier LA, Emans SJ, Woods ER, DuRant RH. The association of sexual risk behaviors and problem drug behaviors in high school students. J Adolesc Health. 1997;20(5):377–83.
Guo J, Chung I-J, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health. 2002;31(4):354–62.
Kingree JB, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. J Adolesc Health. 2000;27(3):179–85.
De Genna NM, Cornelius MD, Cook RL. Marijuana use and sexually transmitted infections in young women who were teenage mothers. Womens Health Issues. 2007;17(5):300–9.
Kingree JB, Phan D. Marijuana use and unprotected sexual intercourse among adolescent detainees: an even analysis. Crim Justice Behav. 2002;29(6):705–17.
Leigh BC, Ames SL, Stacy AW. Alcohol, drugs, and condom use among drug offenders: an event-based analysis. Drug Alcohol Depend. 2008;93(1–2):38–42.
Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS Behav. 2006;10(5):599–605.
Noar SM, Cole C, Carlyle K. Condom use measurement in 56 studies of sexual risk behavior: review and recommendations. Arch Sex Behav. 2006;35(3):327–45.
Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: I. Item content, scaling, and data analytical options. Ann Behav Med. 2003;26(2):76–103.
Jemmott JB 3rd, Jemmott LS. HIV risk reduction behavioral interventions with heterosexual adolescents. AIDS. 2000;14(Suppl 2):S40–52.
Jaccard J, McDonald R, Wan CK, Dittus PJ, Quinlan S. The accuracy of self-reports of condom use and sexual behavior. J Appl Soc Psychol. 2002;32(9):1863–905.
Fishbein M, Pequegnat W. Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sex Transm Dis. 2000;27(2):101–10.
Halpern-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health. 1996;19(5):331–6.
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–45.
Leigh BC. Alcohol and condom use: a meta-analysis of event level studies. Sex Transm Dis. 2002;29(8):476–82.
Fortenberry JD, Costa FM, Jessor R, Donovan JE. Contraceptive behavior and adolescent lifestyles: a structural modeling approach. J Res Adolesc. 1997;7(3):307–29.
Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: results from an event-based daily diary. AIDS Behav. 2008;12(1):104–12.
Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behavior with the timeline followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. Int J STD AIDS. 2001;12(6):365–75.
Stein MD, Anderson BJ, Caviness CM, et al. Relationship of alcohol use and sexual risk-taking among hazardously drinking incarcerated women: an event-level analysis. J Stud Alcohol Drugs. 2009;70(4):508–15.
Sobell L, Sobell M. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Allen LA, editor. Measuring alcohol consumption. New York: The Humana Press; 1992.
Cherpitel CJ. Substance use, injury, and risk-taking dispositions in the general population. Alcohol Clin Exp Res. 1999;23(1):121–6.
Mare RD. Change and stability in educational stratification. Am Sociol Review. 1981;46(1):72–87.
Buis ML. SEQLOGIT: Stata module to fit a sequential logit model. 2007. http://ideas.repec.org/c/boc/bocode/s456843.html.
Agresti A. Categorical data analysis. 2nd ed. Hoboken, NJ: Wiley-Interscience; 2002.
Maddala GS. Limited dependent and qualitative variables in econometrics. Cambridge: Cambridge University Press; 1983.
Stata Statistical Software: Release 10 [computer program]. College Station, TX: StatCorp LP; 2007.
Clutterbuck DJ, Gorman D, McMillan A, Lewis R, Macintyre CCA. Substance use and unsafe sex among men in Edinburgh. AIDS Care. 2001;13(4):527–35.
Heishman SJ, Arasteh K, Stitzer ML. Comparative effects of alcohol and marijuana on mood, memory, and performance. Pharmacol Biochem Behav. 1997;58(1):93–101.
Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101–6.
Vélez-Blasini CJ. Evidence against alcohol as a proximal cause of sexual risk taking among college students. J Sex Res. 2008;45(2):118–28.
Staras SA, Cook RL, Clark DB. Sexual partner characteristics and sexually transmitted diseases among adolescents and young adults. Sex Transm Dis. 2009;36:232–8.
Acknowledgements
This study was supported by NIDA grant R01DA018954. Dr. Stein is a recipient of a NIDA Mid-Career Award K24-DA000512-08.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, B.J., Stein, M.D. A Behavioral Decision Model Testing the Association of Marijuana Use and Sexual Risk in Young Adult Women. AIDS Behav 15, 875–884 (2011). https://doi.org/10.1007/s10461-010-9694-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-010-9694-z