Abstract
Although it is often assumed that drinking alcohol interferes with condom use, most studies on this topic do not meet the conditions required for causal interpretation. We examined the association of drinking to condom use using data from diaries of alcohol use and sexual encounters, collected over 8 weeks from college students and clients of a sexually transmitted disease clinic. This method establishes the temporal relationships between drinking and condom use and controls for individual differences by using a within-subjects analysis. Multilevel models that predicted condom use from alcohol use before the sexual encounter, partner type, and the use of other contraception showed that drinking before sex was unrelated to condom use. These results do not support the persistent notion that alcohol causes people to engage in sexual risk that they would avoid when sober; instead, people tend to follow their usual pattern of condom use, regardless of alcohol use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conventional wisdom has long told of an association of alcohol and sexual activity, based on a widely held belief that drinking makes people do things sexually that they might not otherwise do. In the context of epidemics of HIV and other sexually transmitted diseases (STDs), a potential link between drinking and sex assumes great importance, and it is often assumed that using alcohol in conjunction with sexual activity increases the probability that risky behaviors will occur (U.S. National Institute on Alcohol Abuse and Alcoholism, 1990; U.S. National Institute on Alcohol Abuse and Alcoholism, 2002). The explosion of research on this topic has spurred several literature reviews noting the inconsistency of study findings (Bolton, Vincke, Mak, & Dennehy, 1992; Dingle & Oei, 1997; Donovan & McEwan, 1995; Halpern-Felsher, Millstein, & Ellen, 1996; Leigh & Stall, 1993; Rhodes & Stimson, 1994).
A full understanding of any link between drinking and unsafe sex depends on the use of appropriate methods. Establishing a causal association between drinking and sex requires at least two conditions: alcohol use must precede sexual activity, and confounding variables must be controlled. Most methods for studying the association of alcohol use and high-risk sex do not meet these conditions. Studies that correlate measures of overall substance use and risky sexual behavior do not control for confounding personality variables such as impulsivity or sensation-seeking that may drive both behaviors, nor do they establish that the alcohol use and the risky sex occurred on the same occasion. Some studies ensure this temporal contiguity by using a “critical incident” technique in which respondents are asked about alcohol or drug use and risky sexual activities in these events (Leigh, 2002; Weinhardt & Carey, 2000); however, this method does not eliminate the possibility of confounding personality characteristics (Cooper, Skinner, & George, 1990). Moreover, studying only a single sexual encounter per person might not capture the usual behavioral pattern of individual respondents if the sexual encounter chosen to report on does not represent their usual behavior.
One way to approach meeting these conditions is to collect information about more than one sexual encounter by studying daily events. Diaries or daily logs have been used to gather reports of many health-related behaviors (Sudman & Lannom, 1980; Verbrugge, 1980), including alcohol consumption (see also Leigh, 2000 for review) and sexual behavior (Fortenberry, Orr, Zimet, & Blythe, 1997b; Macaluso, Demand, Artz, & Hook III, 2000). For the purposes of studying the link between alcohol use and sexual activity, such a method has four major features. First, by asking participants to note the time that drinking incidents and sexual encounters began and ended, the temporal relationships of alcohol consumption and sexual behaviors can be determined. Second, sexual encounters with and without substance use can be compared within the same person, using within-subjects or matched-pair analyses, thus holding individual differences constant. Third, because participants record events on the day they occur, a diary method can reduce some of the memory difficulties inherent in retrospective interviews, such as forgetting, “telescoping” (Armstrong, White, & Saracci, 1992; Feinberg & Tanur, 1983), and the tendency to reconstruct events in a manner consistent with current attitudes and knowledge (Bartlett, 1932; Ross, 1989). Finally, if implemented for a sufficiently long period, a diary method can capture variations in drinking and sexual behavior across situations and partners.
Several published studies have examined the link between drinking and risky sex using a diary method. In two of these studies, repeated measures (within-subjects) analysis of variance revealed that drinking within four hours before sex did not affect the use of coitus-dependent contraceptives among women in stable relationships (Harvey & Beckman, 1986) or condom use among young adults (Leigh, 1993). Two other studies in which data were analyzed with generalized estimating equations (GEE) reported that drinking before sex was unrelated to condom use among college students (de Visser & Smith, 2001a; de Visser & Smith, 2001b) and among female adolescents at an STD clinic (Fortenberry, Orr, Katz, Brizendine, & Blythe, 1997). Using random-effects logistic modeling, studies of adolescents (Bailey, Gao, & Clark, 2006; Morrison et al., 2003) and men who have sex with men (Gillmore et al., 2002) reported no relationship of drinking before sex to condom use.
In the present study,Footnote 1 we used daily reports to examine the association of drinking to condom use in two samples of young adults from a university campus and an STD clinic. Previous reports from our research group summarized findings from two other cohorts of this study: adolescents (Morrison et al., 2003) and men who have sex with men (Gillmore et al., 2002). The study was designed to examine the role of alcohol in conjunction with the type of relationship that the sexual partners share. Alcohol is a symbol of courtship, and as such is more prevalent in sexual encounters with new or casual partners (Cooper, Peirce, & Huselid, 1994; Cooper & Orcutt, 2000; Graves & Leigh, 1995; Temple, Leigh, & Schafer, 1993). Some findings suggest that drinking is related to risky sex for casual sexual partners and not primary partners (Fortenberry et al., 1997; Seage et al., 1998), or that alcohol may affect sexual activity only at certain points in a relationship (Halpern-Felsher et al., 1996). In addition, we investigate gender differences in the association of alcohol and unprotected sex.
Method
Participants
University Sample
Recruitment letters were sent to 6,580 undergraduate students aged 18–23, randomly selected from registration records at a large university in the Pacific Northwest. The letters invited the students to participate in a study of health habits, including alcohol use and sexual activity. The 1125 students who responded to the letter were screened for eligibility (see below for criteria); 191 students met the criteria for study eligibility and agreed to participate; 178 of these entered the study.
Clinic Sample
Recruitment fliers were placed in the restrooms and waiting rooms of several public health clinics treating people with STDs. The posted fliers included tear-off coupons containing local and toll free telephone numbers for potential participants to call. To supplement this passive procedure in the largest clinic, a member of the project staff was located in a private area near the clinic to tell potential participants about the project and be available to answer questions. Interested clients were given the option of calling the project to be screened or giving our staff member her/his name and phone number to be called by one of our interviewers for screening. 193 clinic clients entered the study.
Eligibility Criteria
Potential participants were screened by telephone and considered eligible if they were unmarried, not in a steady monogamous relationship of longer than 6 months duration, had sex on at least four occasions in the last 2 months, had drunk alcohol on at least four occasions in the past 2 months, had sex after drinking alcohol at least once in the last 2 months, and had used a condom at least once in the last year (but did not always use condoms). These conditions were imposed to ensure sufficient within-subject variability in alcohol consumption and condom use for the analyses.
Procedure
Participants were randomly assigned to either a written diary condition or a telephone interview condition. They were told that the study was designed to examine daily patterns of a variety of health-related behaviors. Participants in both conditions were sent initial questionnaires (entry surveys) to complete and return before daily data collection began. Daily data were then collected for 8 weeks (56 consecutive days). In the written diary condition, participants were mailed packets each week that contained 7 days worth of diaries, seven self-addressed stamped envelopes with which to return each day’s completed diaries, and instructions. Participants in this condition were instructed to fill out the diaries at the same time each day, and to mail in the completed diary every day. Interviewers telephoned them weekly to offer encouragement, answer questions, and remind them to mail back each day’s survey. In the telephone condition, trained interviewers telephoned participants daily. Participants were mailed copies of the daily survey form to follow as the interviewer asked the questions. At the conclusion of each interview, an appointment was made for the next day’s call.
After the 8 weeks of daily data collection, participants in both conditions were mailed a brief questionnaire (exit survey) to complete and return. Participants were paid $15 for the entry survey, $2 for each daily report, a $3 bonus for each week with no missing days, and $10 for the exit survey.
Measures
The daily survey (identical in the telephone and written conditions) included questions on smoking, diet, dental care, exercise, seatbelt use, sleeping patterns, drug and alcohol use, and sexual behaviors. On the first day of daily data collection, participants reported on their activities in the past 24 h. Each day thereafter, respondents were asked “Since you filled out this form [talked with us] yesterday, did you ... ”. To reduce demand characteristics, questions on alcohol consumption, drug use, and sexual behavior were separated by other items. Once participants became accustomed to the questions and their flow, it typically took no more than about 5 min to respond to all the questions each day.
Sexual Behavior
Up to three sexual encounters could be reported each day. Participants who reported sexual activity indicated the time that the encounter began, the type of sexual activity (vaginal, oral, or anal), the gender of the sexual partner, whether it was the first sexual experience with this partner, type of partner (steady, casual, paid/paying), whether a condom was used, whether another method was used for disease prevention or birth control (hormonal methods, barrier or spermicide methods, or other), whether the partner was drinking or using drugs before sex, whether the participant was at a party or bar with the partner prior to having sex, whether the encounter was expected, and the initials of the sexual partner. A “casual” partner was defined as “a partner you have had sex with once or only a few times and don’t know very well; someone with whom you have no ongoing relationship.” “Steady” partner was defined as “a partner you have had sex with and with whom you have an ongoing relationship.”
Alcohol Consumption
Up to three drinking occasions could be reported each day. Participants who reported drinking indicated the number of drinks consumed, the time that drinking began and ended, how long the effects of the alcohol were felt, where drinking occurred (bar, party, home, friend’s place, other), and with whom they were drinking (alone, with friends/acquaintances, sexual partner, or other).
Data Analysis
Drinking episodes were matched with sexual encounters if drinking occurred within 4 h before sexual activity started (Harvey & Beckman, 1986; Leigh, 1993). The amount of alcohol consumed in each drinking episode was calculated by converting the amounts of beer, wine, and liquor consumed to standard drinks and summing across beverages (one standard drink = one can or bottle of beer [12 ounces], one glass of wine [4 ounces], or one ounce of spirits).
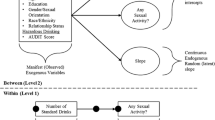
We used multilevel modeling (Affleck, Zautra, Tennen, & Armeli, 1999; Kreft, & DeLeeuw, 1998; Snijders & Bosker, 1999) to construct a random-effects regression model to predict the probability of condom use in sexual encounters from both event-based and person-based variables. Random-effects regression models provide several advantages over alternative techniques for analyzing data in which multiple measurements are collected from each person (Hedeker & Mermelstein, 1996; Schwartz & Stone, 1998). These models do not assume that participants are measured at the same time points or at the same number of time points, can model both time-varying and invariant factors, and adjust for the intraclass correlation that arises when repeated events nested within persons are analyzed. Perhaps most importantly for the purposes of our study, this type of model can estimate subject-specific effects; that is, we can model individual change for each participant (Hu, Goldberg, Hedeker, Flay, & Pentz, 1998).
Results
Three hundred and twelve participants (159 women, 153 men) reported having had intercourse at least one time during the daily diary period; a total of 4,556 events were reported. 165 participants completed all 56 days of reporting, and 80% had fewer than 10 missing days. The mean number of missing days was 8.0 for the STD clinic sample and 6.0 for the university sample (F(1,365)=2.14; ns), and was 7.0 for the written diary condition and 5.0 for the telephone condition (F(1,365)=2.25, ns).
Table 1 presents information on sociodemographic characteristics, sexual experience, and alcohol use for these sample members.
Number of occasions of sexual intercourse reported for the 8 weeks ranged from 1 to 85 per participant (mean = 13.2, SD = 12.0, median = 10). Of all the occasions reported, 40% were condom-protected; 24% were preceded by alcohol use; 83% took place with a steady sexual partner; and 17% took place with a casual partner. Preliminary analyses indicated that although alcohol use was reported on somewhat more days in the interview relative to the diary condition, there were no significant differences between methods of data collection in the number of days on which sex occurred, condom use, the amount of alcohol consumed or the number of days on which drugs were used. Therefore, we combined data from both conditions for the analyses.
Drinking and Condom Use
We calculated the proportion of times that condoms were used for vaginal intercourse (1) when intercourse was preceded by alcohol use and (2) when intercourse was not preceded by alcohol use for each participant who had at least one occasion of intercourse in both situations (n = 224). These proportions are presented in Table 2 by gender and type of partner (steady or casual). (Note that the number of subjects available for the analysis of casual partners in particular was small because it included only those who had sex with casual partners both with and without drinking.) Paired t-tests comparing these proportions within subjects showed no tendency for drinking to reduce condom use. In fact, there was a trend toward more condom use in sexual encounters preceded by drinking in encounters with casual partners.
Figure 1 presents a frequency distribution of drinking-related differences in condom use for the 224 respondents (103 men, 121 women) who reported at least one occasion of sex after drinking and at least one occasion of sex that did not follow drinking. These differences represent the proportion of times condoms were used with sex that occurred after drinking minus the proportion of times that condoms were used with sex that occurred when the respondent had not been drinking. This figure highlights the individual consistency of condom use (or non-use) among this sample, regardless of drinking. Most respondents used condoms equally often on both types of occasions (difference = 0); among respondents whose condom use did vary by alcohol consumption, most had a difference of less than ±.25.
To perform more detailed analysis with both person-level and event-level variables, we constructed a multilevel model to predict the probability of condom use, using a random-effects logit model. In this model, sexual occasions constitute event-level observations, and are nested within individuals. We first analyzed a simple model in which condom use was predicted from drinking before sex (an event-level variable; coded yes/no). The odds of condom use were not significantly different for drinking versus non-drinking events (Odds ratio [OR] = 1.19, 95% confidence interval [CI] .93, 1.54). Estimating this model separately by gender revealed that drinking was not significantly related to condom use for men (OR = 1.35, 95% CI .92, 2.0) or for women (OR = 1.10, 95% CI = .79, 1.52). Similar results were obtained when condom use was predicted from number of drinks consumed (men: OR = 1.05, 95% CI .99, 1.12; women: OR 1.17, 95% CI = 1.08, 1.27).
Finally, we specified a model that included additional individual and situational variables that might affect the association of drinking to condom use. Because drinking is more common with casual sexual partners, and condoms are used more often with casual partners, drinking might be associated with an increase in condom use when partner type and other factors are not controlled. A second multilevel model was estimated that included drinking before sex, partner type (casual or steady), use of other contraceptives, and whether the encounter was the first time the participant had sex with that partner, with age and sample included as control variables. To investigate whether drinking was associated with condom use differently for steady and casual partners, we included an interaction term of Drink X Partner Type. In this model (see Table 3), condom use was more likely with casual and first-time partners, and was less likely when other contraceptive methods were used at the time of intercourse. In women, a significant interaction of drinking and partner type indicated that although drinking was unrelated to condom use with steady partners, women who drank before sex with casual partners were more likely than non-drinking women to use condoms (predicted probabilities of condom use: for steady partners, non-drinkers .22, drinkers .24; for casual partners, non-drinkers .29, drinkers .51).Footnote 2
Discussion
In this study, we investigated the character of the much-discussed association between intoxication and risky sexual behaviors, using a within-person analysis that approximates the causal assumptions that are implicit in much research on this topic. HIV- and STD-prevention promotion campaigns often implicitly assume a causal relationship of drinking and risky sex at the event level: that drinking causes people to behave less cautiously than they do when they are sober. Among the young adults in this study, however, we found no overall association of event-level drinking and condom use. This finding is consistent with those of other event-based, within-subject studies (Fortenberry et al., 1997; Harvey & Beckman, 1986; Leigh, 1993) and supports the suggestion that the links that have been established in other published work may be artifacts of confounding with individual differences.
The participants in this study were mostly consistent in their sexual behavior; that is, they either used condoms or they didn’t, regardless of alcohol use. To illustrate, consider the transitions across sexual encounters: for each event, 90% of those who did not use a condom in an event also did not use a condom in the next event, and 84% of those who used a condom in an event also used a condom in the next event. This pattern echoes Fortenberry’s (Fortenberry et al., 1997) suggestion that general patterns of sexual behavior are followed in most sexual encounters, whether drinking or not.
Our finding that drinking was associated with increased condom use with casual partners among women echoes a tendency found in a similar diary study (Leigh, 1993). This pattern may have resulted from residual confounding of drinking with partner type. That is, because drinking is more common with casual partners (Cooper & Orcutt, 2000; Temple et al., 1993; Temple & Leigh, 1992) and condoms are used more often with casual partners (Baker, Morrison, Gillmore, & Schock, 1995; Civic, 1999; de Visser, Smith, Rissel, Richters, & Grulich, 2003), drinking is associated with increased condom use. Although we distinguished casual partners from steady partners in the analysis, casual partners might vary in their casualness, from one-night stands to not-quite-steady partners. Therefore, the high levels of condom use among drinkers with casual partners might represent encounters with partners at the most casual end of the spectrum. The appearance of this pattern only among women may have resulted from women’s tendency to label a sexual partner as “steady” earlier in a relationship; women’s “casual” partners would then tend to be the most casual partners, with whom both drinking and condom use would be more likely to occur.
Our analysis revealed two characteristics that strongly predicted condom use: partner type and the use of other birth control methods. As in other studies that examined the role of partner type (Baker et al., 1995; Civic, 1999; de Visser et al., 2003), condoms were used more often with casual partners than with regular sexual partners. This population may have heeded public health warnings to use caution with partners they don’t know well, or may find it more awkward or insulting to suggest condom use with steady partners, given the intimacy concerns of a committed relationship (Morrison, Baker, & Gillmore, 1998; Morrison, Gillmore, & Baker, 1995).
Alternatively, condoms may be used more with casual partners simply because oral contraceptives, which accounted for almost all instances of contraceptive protection in this study, are more likely to be used by women with regular or romantic sexual partners (Ford, Sohn, & Lepkowski, 2001; Morrison, 1985). Women may feel that hormonal methods are less appropriate if they are having sex only occasionally or they may not have planned ahead for a casual encounter. Participants may use condoms with casual partners not because they perceive increased risk of disease transmission but, at least in part, to prevent pregnancy on occasions when they are not protected by other methods. Note that the negative association between contraceptive use and condom use in our findings suggests that condoms were used primarily for contraception rather than for disease prevention, despite the high visibility of campaigns promoting condom use for STD prevention (Civic, 2000).
The limitations of this study include the focus on the effects of a single drug (alcohol) and on drinking by only one of the sexual partners. Illicit substances were used by too few of the participants to enable any analysis, and drinking by the sexual partners was so highly correlated that it was impossible to disentangle the participant’s drinking from the partner’s drinking in the analyses. Our screening criteria excluded people who never or always drank when they had sex, since there was no way to evaluate the effect of intoxication on their condom use with within-subject analyses. We also excluded people who always or never used condoms, for the same reason. However, members of the sample, who have sex with drinking and have sex with casual partners, are representative of the people who are the targets of the “high = high risk” condom promotion campaigns, and are therefore an appropriate group in which to study a putative link between drinking and risky sex.
A second limitation lies in the nature of self-report: although daily diaries are assumed to be more accurate than alternative retrospective measures, they may still be subject to errors, biases, and falsification, as are all methods involving self-reports. Reviews of measurement of HIV-relevant sexual behavior conclude that behavioral reports of sensitive sexual behaviors can be valid when proper procedures are followed (Fishbein & Pequegnat, 2000). Reporting on such behaviors on the same day they occur leads to more reliable measurement than longer retrospective periods (Stone, Kessler, & Haythornthwaite, 1991).
In summary, when analyzing event-level data with within-subjects methods, we found no evidence that drinking before sex decreases condom use. The consistency of our findings with those of similar studies in different populations (Bailey et al., 2006; de Visser & Smith, 2001a; de Visser & Smith, 2001b; Fortenberry et al., 1997; Harvey & Beckman, 1986; Leigh, 1993) gives us more confidence that our results are not unique to our samples of young adults. These results do not support the persistent notion that alcohol causes people to engage in sexual risk that they would avoid when sober; instead, people tend to follow their usual pattern of condom use, regardless of alcohol use (Fortenberry, 1998).
Notes
Data collected between 1995 and 1999.
Note that when the logistic equation includes an interaction between two variables A and B, the coefficient for A represents the effect for A when B = 0. Thus, the OR of 1.0 for partner type among women does not represent the lack of a significant main effect of partner type; it signifies that partner type was not associated with condom use when alcohol was not consumed. Odds ratios for drinking and partner type main effects (without the interaction included) among women were 1.08 (95% CI = .77, 1.50) and 1.84 (95% CI = 1.16, 2.90), respectively.
References
Affleck, G., Zautra, A., Tennen, H., & Armeli, S. (1999). Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology, 67(5), 746–754.
Armstrong, B. K., White, E., & Saracci, R. (1992). Principles of exposure measurement in epidemiology. New York: Oxford University Press.
Bailey, S. L., Gao, W., & Clark, D. B. (2006). Diary study of substance use and unsafe sex among adolescents with substance use disorders. Journal of Adolescent Health, 38(3), 297.e13–297.e20.
Baker, S. A., Morrison, D. M., Gillmore, M. R., & Schock, M. D. (1995). Sexual behaviors, substance use, and condom use in a sexually transmitted disease clinic sample. Journal of Sex Research, 32, 37–44.
Bartlett, F. C. (1932). Remembering: A study in experimental psychology. Cambridge, UK: Cambridge University Press.
Bolton, R., Vincke, J., Mak, R., & Dennehy, E. (1992). Alcohol and risky sex: In search of an elusive connection. Medical Anthropology, 14, 323–363.
Civic, D. (1999). The association between characteristics of dating relationships and condom use among heterosexual young adults. AIDS Education and Prevention, 11(4), 343–352.
Civic, D. (2000). College students’ reasons for nonuse of condoms within dating relationships. Journal of Sex and Marital Therapy, 26, 95–105.
Cooper, M. L., Peirce, R. S., & Huselid, R. F. (1994). Substance use and sexual risk taking among black and white adolescents. Health Psychology, 13, 251–262.
Cooper, M. L., & Orcutt, H. K. (2000). Alcohol use, condom use and partner type among heterosexual adolescents and young adults. Journal of Studies on Alcohol, 61(3), 413–419.
Cooper , M. L., Skinner, J. B., & George, W. H. (1990). Alcohol use and sexual risk-taking among adolescents: Methodological approaches for assessing causal issues. In D. Seminara, A. Pawlowski, & R. Watson (Eds.), Alcohol, Immunomodulation, and AIDS (pp. 11–19). New York: Alan R. Liss.
de Visser, R. O., & Smith, A. M. A. (2001a). Inconsistent users of condoms: A challenge to traditional models of health behaviour. Psychology, Health and Medicine, 6(1), 41–46.
de Visser, R., & Smith, A. (2001b). Relationship between sexual partners influences rates and correlates of condom use. AIDS Education and Prevention, 13(5), 413–427.
de Visser, R. O., Smith, A. M., Rissel, C. E., Richters, J., & Grulich, A. E. (2003). Sex in Australia: safer sex and condom use among a representative sample of adults. Australia and New Zealand Journal of Public Health, 27(2), 223–229.
Dingle, G. A., & Oei, T. P. S. (1997). Is alcohol a cofactor of HIV and AIDS? Evidence from immunological and behavioral studies. Psychological Bulletin, 122(1), 56–71.
Donovan, C., & McEwan, R. (1995). A review of the literature examining the relationship between alcohol use and HIV-related sexual risk-taking in young people. Addiction, 90, 319–328.
Feinberg, S. E., & Tanur, J. M. (1983). Large-scale social surveys: Perspectives, problems, and prospects. Behavioral Science, 28, 135–153.
Fishbein, M., & Pequegnat, W. (2000). Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sexually Transmitted Diseases, 27(2), 101–110.
Ford, K., Sohn, W., & Lepkowski, J. (2001). Characteristics of adolescents’ sexual partners and their association with use of condoms and other contraceptive methods. Family Planning Perspectives, 33(3), 100–105, 132.
Fortenberry, J. D., Orr, D. P., Katz, B. P., Brizendine, E. J., & Blythe, M. J. (1997). Sex under the influence. A diary self-report study of substance use and sexual behavior among adolescent women. Sexually Transmitted Diseases, 24, 313–319.
Fortenberry, J. D., Orr, D. P., Zimet, G. D., & Blythe, M. J. (1997b). Weekly and seasonal variation in sexual behaviors among adolescent women with sexually transmitted diseases. Journal of Adolescent Health, 20(6), 420–425.
Fortenberry, J. D. (1998). Alcohol, drugs, and STD/HIV risk among adolescents. AIDS Patient Care and STDs, 12, 783–786.
Gillmore, M. R., Morrison, D.M., Leigh, B. C., Hoppe, M. J. Gaylord, J., & Rainey, D. T. (2002). Does “high = high risk”? An event-based analysis of the relationship between substance use and unprotected anal sex among gay and bisexual men. AIDS and Behavior, 6(4), 361–370.
Graves, K. L., & Leigh, B. C. (1995). The relationship of substance use to sexual activity among young adults in the United States. Family Planning Perspectives, 27(1), 18–22, 33.
Halpern-Felsher, B. L., Millstein, S. G., & Ellen, J. M. (1996). Relationship of alcohol use and risky sexual behavior: A review and analysis of findings. Journal of Adolescent Health, 19, 331–336.
Harvey, S. M., & Beckman, L. J. (1986). Alcohol consumption, female sexual behavior and contraceptive use. Journal of Studies on Alcohol, 47, 327–332.
Hedeker, D., & Mermelstein, R. J. (1996). Application of random-effects regression models in relapse research. Addiction, 91 Suppl, S211–S229.
Hu, F. B., Goldberg, J., Hedeker, D., Flay, B. R., & Pentz, M. A. (1998). Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. American Journal of Epidemiology, 147(7), 694–703.
Kreft, I., & DeLeeuw, J. (1998). Introducing multilevel modeling. London: Sage Publications.
Leigh, B. C. (1993). Alcohol consumption and sexual activity as reported with a diary technique. Journal of Abnormal Psychology, 102, 490–493.
Leigh, B. C. (2002). Alcohol and condom use: a meta-analysis of event-level studies. Sexually Transmitted Diseases, 29(8), 476–482.
Leigh, B. C. (2000). Using daily reports to measure drinking and drinking patterns. Journal of Substance Abuse, 12(1–2), 51–65.
Leigh, B. C., & Stall, R. (1993). Substance use and risky sexual behavior for exposure to HIV: Issues in methodology, interpretation, and prevention. American Psychologist, 48, 1035–1045.
Macaluso, M., Demand, M. J., Artz, L. M., & Hook III, E. W. (2000). Partner type and condom use. AIDS, 14(5), 537–546.
Morrison, D. M., Baker, S. A., & Gillmore, M. R. (1998). Condom use among high-risk heterosexual teens: A longitudinal analysis using the theory of reasoned action. Psychology & Health, 13, 207–222.
Morrison, D. M., Gillmore, M. R., & Baker, S. A. (1995). Determinants of condom use among high-risk heterosexual adults: A test of the theory of reasoned action. Journal of Applied Social Psychology, 25, 651–676.
Morrison, D. M. (1985). Adolescent contraceptive behavior: A review. Psychological Bulletin, 98, 538–568.
Morrison, D. M., Gillmore, M. R., Hoppe, M. J., Gaylord, J., Leigh, B. C., & Rainey, D. T. (2003). Adolescent drinking and sex: Findings from a daily diary study. Perspectives on Sexual and Reproductive Health, 35(4), 162–168.
Rhodes, T. & Stimson, G. (1994). What is the relationship between drug taking and sexual risk? Social relations and social research. Sociology of Health and Illness, 16, 209–228.
Ross, M. (1989). Relation of implicit theories to the construction of personal histories. Psychological Review, 96(2), 341–357.
Schwartz, J. E., & Stone, A. A. (1998). Strategies for analyzing ecological momentary assessment data. Health Psychology, 17(1), 6–16.
Seage, G. R. 3rd, Mayer, K. H., Wold, C., Lenderking, W. R., Goldstein, R., Cai, B., Gross, M., Heeren, T., & Hingson, R. (1998). The social context of drinking, drug use, and unsafe sex in the Boston Young Men Study. Journal of Acquired Immune Deficiency Syndromes, 17, 368–375.
Snijders, T., & Bosker, R. (1999). Multilevel analysis: An introduction to basic and advanced multilevel modeling. London: Sage Publications.
Stone, A. A., Kessler, R. C., & Haythornthwaite, J. A. (1991). Measuring daily events and experiences: Decisions for the researcher. Special Issue: Personality and daily experience. Journal of Personality, 59(3), 575–607.
Sudman, S., & Lannom, L. B. (1980). Health care surveys using diaries. DHHS Publication No. PHS 80–3279. Washington D.C.: Department of Health and Human Services.
Temple, M. T., Leigh, B. C., & Schafer, J. (1993). Unsafe sexual behavior and alcohol use at the event level: Results of a national survey. Journal of Acquired Immune Deficiency Syndromes, 6, 393–401.
Temple, M. T., & Leigh, B. C. (1992). Alcohol consumption and unsafe sexual behavior in discrete events. Journal of Sex Research, 29(2), 207–219.
U.S. National Institute on Alcohol Abuse and Alcoholism. (1990). Alcohol and Health: Seventh Special Report to the U.S. Congress. Washington, D.C.: U.S. Department of Health and Human Services.
U.S. National Institute on Alcohol Abuse and Alcoholism. (2002). Alcohol and HIV/AIDS. Alcohol Alert No. 57.
Verbrugge, L. M. (1980). Health diaries. Medical Care, 18(1), 73–95.
Weinhardt, L. S., & Carey, M. P. (2000). Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research, 11, 125–157.
Acknowledgments
This work was Supported by Grants AA09701, K02 AA0183, and AA013688 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leigh, B.C., Vanslyke, J.G., Hoppe, M.J. et al. Drinking and Condom use: Results from an Event-Based Daily Diary. AIDS Behav 12, 104–112 (2008). https://doi.org/10.1007/s10461-007-9216-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9216-9