Abstract
Rho-associated protein kinase (ROCK), a ubiquitously expressed signaling messenger and downstream effector of Rho, is activated by several bioactive factors in the aqueous humor (AH). Rho-ROCK signaling regulates a wide spectrum of fundamental cellular events, including cell adhesion, motility, proliferation, differentiation, and apoptosis. Previous studies, including our own, found that ROCK inhibitor lowers intraocular pressure (IOP) via a direct effect on the conventional AH outflow pathway, by regulation of contractile properties, fibrotic activity, and permeability of the trabecular meshwork (TM) and Schlemm’s canal (SC) tissues, influencing extracellular matrix (ECM) production. Recently, a novel ROCK inhibitor, ripasudil, has been introduced in Japan. Other ROCK inhibitors are now in clinical trials as new IOP-lowering drugs for glaucoma patients. To date, ripasudil, administered together with other glaucoma medications, has proved safe and efficient in lowering IOP as well as additional effects such as prostaglandin analogs, beta-blockers, and carbonic anhydrase inhibitors, all of which help lower IOP by different mechanisms. In addition, we found that long-term treatment with ripasudil exerted an additional IOP-lowering effect, especially in eyes with high IOP, suggesting that late-onset remodeling of the ECM in glaucomatous eyes may elicit mild and delayed changes in IOP levels. ROCK inhibitors have also shown several additional effects, including increased retinal blood flow, direct protection of neurons against various types of stress, and regulation of wound healing; these benefits may potentially be useful in glaucoma treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glaucoma remains the leading cause of irreversible vision loss worldwide, and 3.9% of people aged 40 years or older are affected in Japan [1]. Taking all subtypes into consideration, the global prevalence of glaucoma in the population 40–80 years old is estimated to increase in the coming years from 76 million in 2020 to 111.8 million in 2040 [2]. Patients with glaucoma suffer from irreversible progressive visual field loss due to deterioration of the optic nerve [3, 4]. Many risk factors are known to be involved, including elevated intraocular pressure (IOP), advanced age, family history, African ancestry, axial myopia, thin central corneal thickness, and low cerebrospinal fluid pressure [4]. Furthermore, glaucoma is known to be a multifactorial disease, with several factors, including retinal vascular autoregulation, oxidative stress and free radical formation, alterations in local cytokines, retinal ganglion cell (RGC) glutamate stimulation, aberrant local immunity, and irregular optic nerve perfusion pressure, having been implicated in its pathogenesis [3, 5]. At present, however, elevated IOP is the major and only clinically modifiable risk factor in glaucoma prevention, and is the sole target of current glaucoma treatment. Elevated IOP in the anterior chamber of the eye damages optic nerve axons and leads to RGC death, which eventually results in impairment of vision in glaucoma patients [6, 7].
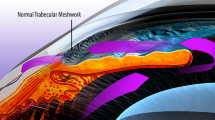
IOP is determined from the balance between aqueous humor (AH) production and outflow. AH is produced by and released from the ciliary body and flows from the posterior to the anterior chamber via a pressure-dependent gradient. It then drains through the conventional pathway via the trabecular meshwork (TM) and uveoscleral pathway through the ciliary body to the suprachoroidal space (Fig. 1) [8, 9]. The major drainage pathway for AH from the anterior chamber is the pressure-dependent conventional outflow pathway, which carries 80% of total AH out of the eye [10]. Under normal physiological conditions, the TM route accounts for up to 90% of aqueous outflow. IOP elevation is hypothesized to be derived from the increased outflow resistance mainly in the conventional pathway. In the most common type of glaucoma, primary open-angle glaucoma (POAG), increased outflow resistance occurs mainly in the juxtacanalicular tissue (JCT), the portion closest to Schlemm’s canal (SC), and in the endothelial-lined SC [11, 12]. A number of medications, such as prostaglandin analogs (PGs), β-blockers, carbonic anhydrase inhibitors (CAIs), and α2-agonists, are used to lower IOP levels in glaucomatous eyes; however, these affect the uveoscleral pathway or AH production as opposed to the conventional pathway.
Schematic drawing showing the two AH outflow pathways. Pathway (1) is the conventional path through the TM and SC to the episcleral vein. Pathway (2) is the uveoscleral pathway, in which AH travels through the iris root and ciliary muscle to the choroidal space. TM, trabecular meshwork; SC, Schlemm’s canal; AH, aqueous humor
Recently a new class of antiglaucoma medications, Rho-associated protein kinase (ROCK) inhibitors, have been shown to reduce IOP in animal and human eyes. ROCK inhibitors directly modulate the target site in AH outflow by decreasing resistance in the conventional outflow by relaxation of TM cells and TM tissue; this changes the behavior of SC endothelial cells and alters the production and contraction of the extracellular matrix (ECM) [13,14,15,16,17,18]. These IOP-lowering mechanisms are different from other antiglaucoma medications that modulate unconventional outflow (PGs and α2-agonists) or inhibit AH formation (β-blockers, CAIs, and α2-agonists).
In the AH of glaucomatous eyes, elevated levels of several bioactive factors, including transforming growth factor-beta (TGF-β), endothelin-1, connective tissue growth factor (CTGF), myocilin, and several other cytokines are proposed as physiological cues to influence TM tissue properties and cellular responses in the context of AH outflow resistance and elevation of IOP via different intracellular signaling pathways, including Rho/ROCK signaling, Wnt, integrins, PKC, BMPs/SMADs, MAP kinases, and others [10, 19,20,21,22,23,24,25,26,27]. Cellular responses in the conventional pathway, such as regulation of contractile properties of TM cells, ECM turnover, adhesive interactions, permeability, and survival of outflow pathway tissues and cells, are reported to be involved in the modulation of outflow resistance [13, 23, 26]. It is also believed that changes in stiffness and metabolic activity of TM tissues due to altered cellular contraction and oxidative damage are associated with increased resistance to AH outflow and elevated IOP [11].
In this review, we focus on describing the Rho/ROCK signaling pathway and its role in TM and SC cellular physiology, regulation of AH outflow, and IOP and the development of ROCK inhibitors as glaucoma medication.
Rho GTPase and Rho kinase (ROCK) signaling pathway
Rho GTPases are a family within the Ras superfamily of monomeric small GTP-binding proteins, including Rho (RhoA, RhoB, RhoC), Rac, and CDC42, which act as molecular switches that cycle between a GTP-bound active and a GDP-bound inactive conformation (Fig. 2). This cycling between bound GDP and GTP is regulated by guanine nucleotide exchange factors (GEFs), GTPase activating proteins (GAPs), and guanine nucleotide dissociation inhibitors (GDIs) [28]. The activities of GEFs and GAPs are regulated via various receptors in the plasma membrane (Fig. 2) [29, 30]. Rho is activated either by stimulation of secreted bioactive molecule receptors (e.g., endothelin-1, thrombin, angiotensin II, lysophosphatidic acid, TGF-β, and cytokines) or via integrin activation after binding with the ECM (Fig. 2). RhoA acts as a direct downstream target for several G protein-coupled receptors that mediate fundamental cellular processes, including receptors for angiotensin II, platelet-derived growth factor and serotonin [31].
Schematic diagram of the role of Rho-ROCK signaling in regulation of actin cytoskeletal organization, and the effects on IOP, filtering blebs, RGCs, and the optic nerve. Agonists, Angioten II, Growth factors, lipid mediator, Thrombin, Endothelin-1 et al.; ROCK, Rho kinase; MYPT1, myosin phosphatase target subunit 1; MLC, myosin light chain; P-MLC, phosphorylation of MLC; LIMK1/2, LIM kinase1/2; P-Cofilin, phosphorylation of cofilin; TM, trabecular meshwork; ECM, extracellular matrix; JCT, juxtacanalicular tissue; TF, tenon fibroblast; IOP, intraocular pressure; RGC, retinal ganglion cell
ROCK is a serine/threonine protein kinase with a molecular weight of ~160 kDa [32], activated by RhoA. When activated by GTP-bound RhoA, ROCK phosphorylates and activates various intracellular molecules, including myosin light chain (MLC) phosphatase, LIM-kinase (LIMK), CPI-17, calponin, and the ERM (ezrin, radixin, and moesin) proteins, which polymerize actin stress fibers, forming focal adhesions (Fig. 2) [31, 33,34,35,36,37]. Through these interactions, Rho-ROCK signaling regulates actin cytoskeletal dynamics, actomyosin contraction, cell adhesion, cell stiffness, cell morphology, and ECM reorganization (Fig. 2). While cellular contraction can be regulated via both calcium-dependent and calcium-independent mechanisms involving myosin light chain kinase (MLCK) and myosin phosphatase, respectively, ROCK regulates cellular contraction in smooth muscle tissues mainly through modulating myosin II activity in a calcium-independent manner [34, 38, 39].
There are two isoforms of Rho kinase, ROCK1 and ROCK2, which are nearly 65% identical in their overall amino acid sequences and 92% of their kinase domains and are reported to share many cellular functions [38, 40]. A study in gene-targeted mouse models indicates several functional differences between ROCK1 and ROCK2 in aspects of cellular physiology [33, 41]. While both isoforms are known to be ubiquitously expressed in tissues throughout the body, it is reported previously that both ROCK1 and ROCK2 were expressed in most eye tissues studied, except the lens [42]. Both ROCK1 and ROCK2 null mice exhibited lower basal IOP, suggesting that they play important roles in IOP regulation [43]. Due to the involvement of ROCK in basic cellular processes and its ubiquitous distribution, it has long been considered a poor therapeutic target due to the potential for numerous off-target effects. In ophthalmology, ROCK inhibitors are applied topically to minimize undesirable off-target adverse effects. In contrast, systemic ROCK inhibitor treatment may result in an excessive vasodepressor response. However, there is also accumulating evidence that the dysregulation of Rho-ROCK signaling is associated with various diseases, including cardiovascular, metabolic, and neurodegenerative diseases as well as cancer. Therefore, ROCK inhibitors are promising therapeutic agents for the treatment of a wide range of diseases [31, 33, 44,45,46,47].
Role of Rho-ROCK signaling in the conventional AH outflow pathway and regulation of IOP
Several studies indicate that cytoskeletal agents that act directly on the cytoskeleton (e.g., cytochalasins, ethacrynic acid (ECA), and latrunculin B) and the contractile properties of the TM influence AH outflow and lower IOP [25, 48,49,50,51,52]. It is also reported that the broad specificity kinase inhibitors, such as staurosporine, ML-7, and H-7, alter the contractile properties of TM and AH outflow [52, 53]. The inhibitor H-7 is believed to target protein kinase C (PKC), MLCK, and ROCK to induce cell relaxation.
These pioneering studies prompted us to investigate the possible IOP-lowering effects of specific ROCK inhibitors. We first reported that topical application and intracameral injection of the specific ROCK inhibitor Y-27632, significantly lowered IOP and induced relaxation of ciliary muscle in rabbit eyes (Fig. 3a) [13]; in that study, we found that Y-27632 modulated cytoskeletal changes in TM cells, increased conventional outflow through the TM, and relaxed ciliary muscle contraction. Rao et al. [54] and Waki et al. [55] also report that Y-27632 increased outflow facility of porcine and rabbit eyes.
IOP-lowering effect of ROCK inhibitors in rabbit eyes and human eyes. (a) Effects of topical Y-27632 on IOP in rabbit eyes. Contralateral eyes were treated with the same volume of vehicle (phosphate-buffered saline). The results are presented as means ± SEM (n = 6). The significance of differences from controls (vehicle alone) was evaluated using Student’s unpaired t tests (*P < 0.05, **P < 0.01, †P < 0.005). (b) Levels of IOP after single instillation of SNJ-1656. Levels of IOP decreased after instillation but were restored by 24 hours after instillation. Values are represented as mean ± SD (SNJ-1656 group, 12 eyes in 6 subjects; placebo group, 30 eyes in 15 subjects). The significance of findings was evaluated by the Dunnett test (2-sided). *P ≤ .05 compared with the placebo group. †P ≤ .01 compared with the placebo group. Figures modified from (a) Honjo et al. [13] and (b) Tanihara et al. [84], respectively
Other ROCK inhibitors, including Y-39983, fasudil (HA-1077), H1152, and SR-367, were subsequently reported to show IOP-lowering effects [56,57,58,59,60].
We first reported that topical application of the IOP-lowering effects of these ROCK inhibitors are mediated by a novel mechanism that is unique and different from other classes of glaucoma drugs, increasing AH outflow, by acting directly on TM cells and SC cells responsible for increased outflow resistance in nearly all types of open-angle glaucoma.
A great deal of work involving many laboratories has gone into exploring the role of Rho-ROCK signaling in the regulation of TM cells, SC cells, and AH outflow, and in trying to determine how ROCK inhibitors lower IOP. These studies indicate that the mechanisms regulating AH outflow and IOP are heavily dependent on physiological changes in the cytoskeleton and ECM, affected by bioactive molecules in the AH.
ROCK inhibition in TM cells was shown to induce dose- and time-dependent reversible changes in cell shape in association with decreased actin stress fibers, focal adhesions, and cell–cell interactions [13]. As Rho-ROCK signaling regulates smooth muscle contractility and actomyosin organization in a calcium-independent manner [34, 38, 39] and the TM cells and tissue are known to possess smooth muscle-like properties and to express α-smooth muscle actin (αSMA) [25, 61], application of ROCK inhibitors caused a reduction in MLC phosphorylation in TM cells and TM tissue. The cellular changes were confirmed to be closely regulated by non-muscle myosin II activity via inhibition of phosphorylation of MLC and myosin phosphatase [55, 62].
The permeability of SC endothelial cells is also suggested to play an important role in the regulation of aqueous outflow [16]. After perfusion with cytoskeletal drugs, breaks have been found in the endothelial lining of the SC and aqueous plexus [63,64,65], and SC endothelial cells had transcellular pores accompanied by giant vacuoles [16, 66]. ROCK inhibition affects the integrity of intercellular junctions, including the adherens and tight junctions, thereby influencing the permeability barrier of the inner wall of the SC; it also affects cell shape, actin cytoskeleton, and cell adhesive interactions, similar to those observed in TM cells [14, 16, 55, 67, 68]. These reactions were confirmed in a series of experiments to assess the effects of ROCK inhibitors on AH outflow both in enucleated eyes and in live animals. A dose-dependent increase in AH outflow primarily through the conventional pathway was observed following treatment with ROCK inhibitors; this response was associated with TM tissue relaxation, increases in giant vacuoles in the SC inner wall, expansion of JCT, widening of SC, and wash-out of the ECM in the conventional pathway [13, 16, 55, 69].
In addition, it is reported that inhibition of ROCK reduces cell tension and stiffness, regulates fibrogenic activity, and decreases ECM synthesis and rigidity in TM, SC, and JCT [70, 71]. Fujimoto et al. report that Y-27632 suppressed dexamethasone-induced cytoskeletal changes and enhanced SC cell permeability, which suggests the possible involvement of Rho-ROCK signaling in steroid-induced glaucoma [15]. The involvement of Rho-ROCK signaling in the modulation of outflow resistance in the conventional pathway was confirmed by several series of experiments using gene transfer, in which the expression of dominant negative ROCK in TM cells decreased actin stress fibers, MLC phosphorylation, and focal adhesions [72,73,74], or expression of constitutively active RhoA GTPase (RhoAV14) in organ-cultured eyes. In an in vivo rat model, it induced an increase in TM contractile activity, a decrease in AH outflow facility, and elevated the IOP and fibrogenic activity of TM [71, 75]. Moreover, we recently reported that in glaucoma patients there were notable increases of aqueous lysophosphatidic acid (LPA) levels [76], and that in conventional outflow pathway specimens from glaucoma patient there was significant expression of autotaxin (ATX) and a generating enzyme of LPA [77]. LPA is known as a strong lipid mediator that induces many kinds of cellular responses including Rho GTPase-regulated cellular interaction. In the study, we demonstrated that the ATX expression was upregulated by dexamethasone treatment in human TM cells, and fibrotic response was also induced in TM cells by dexamethasone possibly by the de novo production of LPA by ATX. The fibrotic response was significantly suppressed by a ROCK inhibitor, Y-27632 (Fig. 4) [77].
The effects of ATX inhibition on dexamethasone or TGF-β2-induced fibrotic responses in human trabecular meshwork cells. The effects of S32826, ATX inhibitor, or Y-27632 in HTM cells treated with 100nM dexamethasone (Dex) or 5 ng/mL TGFβ2. Immunostaining for αSMA (red, upper panels), fibronectin (FN, green), and collagen-1 (Col, red) (lower panels) was performed. Cell nuclei were counterstained with DAPI (blue). Bars, 100 μm and 50 μm for upper and lower panels, respectively. Figure modified from Honjo et al. [77]
As described above, AH derived from glaucoma patients contains elevated levels of various bioactive factors [10, 19,20,21,22,23,24,25,26, 76], and ROCK inhibitors are shown to suppress TGF-β2-, LPA-, CTGF-, and RhoA-induced increases in fibrogenic activity in TM cells and transdifferentiation into myofibroblast-like cells [70, 77]. These observations suggest that Rho-ROCK signaling plays a central role in the pathophysiology underlying the initiation of glaucomatous changes in the conventional pathway by interacting with other key regulatory molecules and cellular pathways.
Pilocarpine is another glaucoma drug that lowers IOP by increasing conventional outflow. Pilocarpine is known to widen the spaces of the TM, thereby decreasing flow resistance and increasing AH outflow by ciliary muscle contraction [78]. Ciliary muscle contraction is mediated mostly in a calcium-dependent manner, but TM contraction is reported to involve both calcium-dependent and calcium-independent pathways [25]. High levels of mRNAs for ROCK and ROCK substrates are reported in the TM in comparison with ciliary muscle [79], and ROCK inhibitors are shown to affect TM cells through a calcium-independent pathway, which is not prominent in ciliary muscle cells. In addition, Inoue et al. report faster and more potent effects of Y-27632 in TM cells than in ciliary muscle cells, suggesting a difference in ROCK pharmacological affinity for TM and ciliary muscle cells [18, 80]. Taken together, these observations indicate that although pilocarpine and ROCK inhibitors both increase conventional outflow, they do it by different mechanisms and with different pharmacological affinity to the target tissue. Still, the interactions between these two classes of drugs should be explored further in future studies.
There are active investigations of the mechanisms and changes in tissues affected by ROCK inhibitors using new techniques, such as anterior high-resolution spectral domain optical coherence tomography (SD-OCT) [81]. A relatively new ROCK inhibitor currently in clinical development, netarsudil (formerly AR-13324), which has been shown to decrease IOP in monkeys by increasing trabecular AH outflow facility [27], has also been shown to decrease episcleral venous pressure in rabbits [82]. Using OCT, Li et al. report that netarsudil treatment widened the TM and significantly increased the SC cross-sectional area [83]. Because netarsudil also exhibits norepinephrine transport inhibitory activity, it is unclear whether the reduction of episcleral venous pressure or widening of the SC is due to inhibition of ROCK [27]; however, an investigation of the modulation of episcleral venous pressure distal to the SC may provide novel possibilities for glaucoma therapy.
ROCK inhibitors as glaucoma medications in clinical use
Several clinical trials of ROCK inhibitors are underway with a view toward their approval for clinical use. We first reported that twice-daily use of the topical ROCK inhibitor, Y-39983 (SNJ-1656), markedly lowered IOP in healthy human volunteers (Fig. 3b) [84]. Several ROCK inhibitors have been evaluated for clinical safety and efficacy in human subjects, including ripasudil (K-115), fasudil, AMA0076, AR-12286, and netarsudil (AR-13324), all of which showed ocular hypotensive effects [60, 85,86,87,88,89,90,91]. In 2014, ripasudil was the first clinically available ROCK inhibitor approved for the treatment of ocular hypertension (OHT) and glaucoma in Japan [90,91,92].
It has been over 3 years since the approval of ripasudil, and clinical experience with this drug has been accumulating. Although the number of patients has been small and analyses were performed retrospectively, several groups have used ripasudil as an adjunctive therapy and report significant IOP-lowering effects in POAG and normal tension glaucoma (NTG), even in patients receiving other medical therapy at the maximum tolerated doses [93, 94].
Treating glaucoma subtypes other than POAG, NTG, and OHT, Matsumura et al. report the IOP-lowering effects of ripasudil as a second-line drug in addition to prostaglandin analogs, with a follow-up period of at least 5 months in 27 eyes of 19 exfoliation glaucoma patients [95]. Ripasudil significantly lowered IOP in patients with exfoliation glaucoma, and the effect increased over time within 5 months, the mean average IOP level prior to commencement of ripasudil was 16.2, mmHg, after 1–2 months it was 14.7 mmHg, and after 5–6 months it was and 13.1 mmHg. Sato et al. also report IOP-lowering effects of ripasudil as an additive treatment in secondary glaucoma, exfoliation glaucoma, and developmental glaucoma, as the mean preadministration IOP and %IOP reduction at the last follow-up were 22.8 ± 8.3 mmHg and 19.1% ± 13.5% for secondary glaucoma, 22.5 ± 4.4 mmHg and 2.1% ± 14.5% for exfoliation glaucoma, and 20.2 ± 8.9 mmHg and 11.4% ± 23.1% for developmental glaucoma [96].
These recent clinical reports indicate no cases of severe drug-related systemic or ocular adverse events. As reported in previous clinical studies [90, 91], one of the major ocular adverse reaction of topical administration of 0.4% ripasudil is conjunctival hyperemia, which was consistently reported to peak rapidly to moderate severity after instillation, but subsided relatively quickly [97]. As ROCK inhibitors can increase blood flow by inhibiting calcium sensitization and relaxing vascular smooth muscle [39], vasodilation of conjunctival vessels would manifest as conjunctival hyperemia [84]. This cosmetic side effect has been a concern since long before approval of the drug, as it would likely reduce adherence or satisfaction in glaucoma patients. However, it has not been a major problem. For example, Sato et al. report that although several ocular side effects, i.e., allergic reaction, blepharitis, or a burning sensation, led to discontinuation of ripasudil in some patients, this was unlikely to be related to conjunctival hyperemia. Transient morphological changes in corneal endothelial cells were detected in healthy subjects after ripasudil administration by noncontact specular microscopy; however, these morphological changes were reversible, and corneal endothelial cell morphology returned to normal prior to the next administration [98]. As ROCK inhibitors are completely different from other glaucoma medications and represent a new class of glaucoma treatment, further studies are needed to clarify the long-term safety and adverse events of these drugs.
In a recently published prospective clinical study assessing the IOP-lowering effects and safety of ripasudil in a large cohort with a longer follow-up period, a 52-week administration of 0.4% ripasudil successfully lowered IOP when used as both monotherapy and additive therapy [99]. A multicenter prospective study of 354 patients with POAG or OHT was conducted, in which patients were divided into a ripasudil monotherapy group or a group receiving additive therapy with prostaglandin analogs, beta-blockers, or fixed combination drugs. The mean IOP reductions at trough and peak at the conclusion of the study were −2.5 and −3.7 mmHg for monotherapy and −1.4 and −2.4, −2.2 and −3.0, and −1.7 and −1.7 mmHg for additive therapy with prostaglandin analogs, beta-blockers, and fixed combination drugs, respectively [99]. The frequency of adverse drug reactions was relatively high, affecting 301 of 354 (85.0%) patients, with the most frequent drug-related adverse events being conjunctival hyperemia (74.6%), blepharitis (20.2%), and allergic conjunctivitis (15.0%). Despite the high incidence, the majority of adverse effects were mild and transient, and frequently resolved spontaneously, consistent with other reports.
In previous phase III clinical trials, ripasudil showed additive effects on IOP reduction to latanoprost and timolol after 8 weeks of treatment [100]. This recent clinical study supported and expanded the findings related to the additive effects of ripasudil on IOP reduction to other prostaglandin analogs, beta-blockers, and fixed combination drugs over a longer treatment period. In addition, the study also confirmed the effectiveness of ripasudil for IOP reduction, even in monotherapy, compared with current first-line antiglaucoma drugs [99], adding to previous findings of the IOP-lowering effects of the drug compared to second-line medications, such as CAIs and brimonidine [101, 102].
Despite accumulating knowledge regarding the IOP-lowering effects of ripasudil, the long-term efficacy and safety of ROCK inhibitors have yet to be fully asserted. Therefore, we conducted additional analysis by conducting a clinical study with a 52-week treatment period to better characterize the IOP response of twice-daily topical administration of 0.4% ripasudil.
Additional IOP-lowering effects of ripasudil observed after long-term topical administration: insights from a prospective, open-label, 52-week clinical study.
The study design and main results regarding efficacy and safety are described above [97, 98]. Changes in IOP in the first half (4–28 weeks) and the second half (32–52 weeks) of the study period were calculated as the difference between the least-square means of the two periods based on the mixed effect model.
Of 354 patients with glaucoma and OHT, 109 (31%) discontinued treatment with ripasudil 52-week trial; 36% in the monotherapy group and 26% in the combination therapy with prostaglandin analogs, β-blockers, or fixed combination drugs group also discontinued their treatment. The time course of IOP was comparable for all of the enrolled patients and for the patients that completed the study (data not shown). Therefore, it seems unlikely that the dropouts would bias our results. The most critical limitations were that the study was a post hoc analysis and it was conducted without a placebo control group.
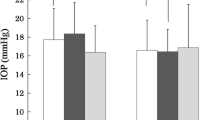
In the monotherapy group (n = 173, 66 men, age 62.5 ± 12.6 years, IOP at 09:00 19.3 ± 2.7 mmHg), the changes in IOP from baseline to the first and second halves of the study period were −2.12 ± 0.15 and −2.61 ± 0.15 mmHg at trough (before instillation) with a difference of −0.49 ± 0.07 mmHg (P < 0.001), and −3.23 ± 0.17 and −3.81 ± 0.17 mmHg at peak (2 h after instillation) with a difference of −0.58 ± 0.08 mmHg (P < 0.001), respectively (Fig. 5a). Subgroup analysis stratified according to the baseline IOP (15 ≤ to < 18, 18 ≤ to < 21, ≥ 21 mmHg); eyes with IOP of 21 mmHg or higher showed the greatest reduction (trough: −0.40 ± 0.12, −0.28 ± 0.11, and −0.91 ± 0.16 mmHg; peak: −0.49 ± 0.12, −0.47 ± 0.11, and −0.84 ± 0.17 mmHg, P < 0.01 respectively) (Fig. 5b and 5c). Differences in IOP were also observed (trough: −0.40 ± 0.07 mmHg, P < 0.001; peak: −0.46 ± 0.07 mmHg, P < 0.001) in the combination therapy group (n = 181, 80 males, age 63.9 ± 11.7 years, IOP at 09:00 17.8 ± 2.1 mmHg) (Fig. 5a).
Changes in IOP by 0.4% ripasudil. Changes in IOP in the first half (4–28 weeks) and the second half (32–52 weeks) of the study period were calculated as the difference between the least-square means of the two periods based on the mixed effect model. Changes in IOP before instillation (trough) or at 2 h after instillation (peak) in monotherapy and combination therapy groups are shown (a). Changes in IOP at trough (b) and at peak (c) in monotherapy were stratified according to the baseline IOP level (●: < 18 mmHg, n = 47; ○: 18 ≤ to < 21 mmHg, n = 74; ■: ≥ 21 mmHg, n = 52). The differences in IOP between the first and second halves of the study period were statistically significant in all groups (P < 0.01). Data are presented as least-square means ± standard error
To our knowledge, this is the first report of additional IOP-lowering effects derived from long-term topical administration of an antiglaucoma medication. In POAG, abnormal outflow resistance occurs mainly in conventional aqueous outflow. ROCK inhibitors modulate this target site, which is a mechanism different from other antiglaucoma medications. The additional IOP-lowering effects of ripasudil may be related to the aberrant status of the TM and/or SC in eyes with POAG and OHT. As Rho-ROCK signaling is in part associated with the production and contraction of ECM via altered TM cellular behaviors [15, 17], late-onset remodeling of the ECM in glaucomatous eyes may elicit mild and delayed changes in IOP levels.
Long-term treatment with ripasudil revealed an additional IOP-lowering effect in eyes with glaucoma and OHT, suggesting an attractive clinical feature that differentiates this drug from other antiglaucoma medications. Positive findings of recent clinical studies are encouraging, as ripasudil appears to be a highly promising new drug for IOP reduction in patients with POAG and OHT, and possibly in secondary glaucoma.
Additional ocular effects of ROCK inhibitors
In addition to the primary function of ROCK inhibitors, lowering IOP, the inhibition of ROCK is reported to be effective in several pathological conditions and could be a useful drug target. These additional desirable effects discussed below could possibly slow progression of glaucomatous neuropathy, which may stimulate efforts to bring ROCK inhibitors to the clinic.
Increase in ocular blood flow
Impaired blood flow around the optic disc is reported as a risk factor in glaucomatous eyes [103, 104]. As described above, ROCK inhibitors increase blood flow by relaxing vascular smooth muscles [39], and the vasodilating effect of topical instillation of ROCK inhibitors has been documented in the retina and optic nerve [56, 105, 106]. In addition, in-vitro experiments using isolated rabbit ciliary arteries showed that selective ROCK inhibitors (Y-27632, Y-39983, and K115) induced concentration-dependent relaxation of ciliary arteries; the results indicate that the relaxation mechanism may involve a decrease in Ca2+ sensitivity of key intracellular contractile protein(s). Additionally, altered regulation of Rho kinases Y-27632, Y-39983, and K115 (ripasudil) may relax isolated rabbit ciliary arteries via mechanisms independent of changes in intracellular calcium ion concentrations and/or altered regulation of ROCK (Fig. 6) [107, 108]. Decreased perfusion is thought to be a causative factor in loss of vision in glaucoma [109]. ROCK inhibitors may slow progression of glaucomatous optic neuropathy not only by lowering IOP but also by working directly on the optic disc blood vessels.
Effects of ripasudil on optic disc blood flow (ODBF). The mean blur rate (MBR) was determined in the optic disk by use of the LSFG-NAVI. The MBR is a parameter that yields a theoretically exact measurement of the retinal microcirculation. MBR-A was the average MBR over the entire optic disk, MBR-V was the MBR average over the vessel area, and MBR-T was the average of the MBR of the optic disk area minus the vessel area. %MBR values were calculated by dividing the MBR value at each time by the baseline MBR value. In the case of administration of ripasudil without phenylephrine, MBR-V (a), MBR-T (b), and MBR-A (c) did not change significantly (n = 5, P > .05). MBR-V (d) in the control eye (n = 9) instilled with phenylephrine followed by saline was decreased from the baseline value at 120 min (*P < .05). MBR- V (d), MBR-T (e), and MBR-A (f) were increased in the ripasudil-treated eyes (n = 9) when compared with the control eyes at 30 and 120 min (†P < .05). Figure modified from Ohta et al. [108]
Improved RGC survival and RGC axon regeneration
Although the precise role of the Rho-ROCK pathway in the pathology of glaucoma optic neuropathy remains unknown, significantly elevated levels of RhoA in the optic nerve head are reported in glaucomatous eyes in comparison with age-matched healthy control subjects, suggesting the possible involvement of the Rho-ROCK pathway in the pathophysiology of optic nerve damage in glaucoma [110]. Moreover, ROCK inhibitors, including HA1007 (fasudil), Y-39983 (SJN-1656), ripasudil (K-115), and Y-27632 are shown to exhibit neuroprotective effects against various stresses by promoting axonal outgrowth and RGC survival in a number of animal models [106, 111,112,113,114,115,116]. A recent study demonstrates that administration of the ROCK inhibitor, K115 (ripasudil), delayed RGC death in an optic nerve crush model in mice or TNF injection model in rat (Fig. 7) [117, 118]. Although a number of animal and preclinical studies supported the potency of Rho-ROCK signaling as a target for neuroprotection therapy in glaucoma [116], the actual efficacy of these drugs as direct neuroprotective agents has yet to be tested in human patients.
Effects of Ripasudil on TNF-Induced Axon Loss. Rat TNF injection model was carried out by intravitreal injection of 10 ng TNF to the right eye and PBS to the contralateral left eye. Histologic findings 2 weeks following injection of (a) PBS, (b) TNF, (c) TNF + 2 pmol ripasudil, (d) TNF + 20 pmol ripasudil, or (e) TNF + 200 pmol ripasudil in rat eye. Scale bar: 10 μm. (f) Comparison of axon numbers. N = 4–6 per group. #P < 0.005 versus CTL. *P < 0.05 versus TNF. Figure modified from Kitaoka et al. [118]
Regulation of wound healing
Glaucoma filtration surgery, such as trabeculectomy, is the most widely used type of antiglaucoma surgery. The most frequent cause of failure in filtration surgery is postoperative excess scarring in the filtering bleb and ECM deposits, resulting in closure of the route for AH; controlling post-operative scarring is key to improving the outcome of filtering surgery. Subconjunctival scarring of the filtering bleb is mainly mediated by tenon fibroblast proliferation, migration, and contraction [119, 120]. Transdifferentiation of fibroblasts into myofibroblasts is a crucial step in wound healing and scar formation [121], associated with enhanced expression of α-SMA with increased synthesis of ECM proteins, growth factors, and integrins [122]. Our research group, along with several other groups, previously reported that ROCK inhibition may reduce scarring by inhibiting transdifferentiation of fibroblasts into myofibroblasts, collagen matrix contraction, and ECM deposition via suppression of TGF-β signaling or LPA-induced fibrotic reaction (Fig. 8) [17], resulting in improved glaucoma filtration surgery outcome in rabbit models [17, 123, 124]. Ripasudil (K115) is also reported to attenuate activation of human conjunctival fibroblasts in vitro [125], resulting in prolonged bleb survival in an in-vivo model of canine glaucoma filtration surgery [126]. Therefore, ROCK inhibitors have potential as anti-scarring agents after glaucoma filtration surgery.
Effect of Y-27632 on the cytoskeleton and on α-SMA expression. (a) Distribution of F-actin in human tenon fibroblasts (HTFs). Serum-starved HTFs were incubated with 10 μM LPA for 10 minutes and were then incubated without (control, 0 μM) or with 1, 10, or 100 μM Y-27632 for 30 minutes. Experiments repeated three times yielded similar results. (b) Distribution of F-actin and vinculin in HTFs. Serum-starved HTFs were stimulated with 10 μM LPA for 10 minutes and were then incubated with 10 μM Y-27632 for 30 minutes. LPA induced assembly of actin stress fibers (B, white arrows) and redistribution of focal adhesions in the cell periphery (b, white arrowheads), and Y-27632 prevented these effects. Right: merged images. (c) Distribution of F-actin and α-SMA in HTFs. α-SMA expression is a hallmark of myofibroblast generation and the cells’ fibrogenic reaction. The cells were stimulated with LPA in the presence of 10 μM Y-27632. LPA treatment induced assembly of α-SMA-positive stress fibers (c white arrows). Y-27632 prevented LPA-induced expression of α-SMA and its incorporation into actin stress fibers. Right: merged images. Scale bars, 50 μm. Figure modified from Honjo et al. [17]
Potent therapeutic property for corneal disease
Rho-ROCK pathway is known to be involved in many corneal cell functions. In corneal epithelial cells, it is involved in a number of cellular reactions such as differentiation, proliferation, cell adhesion cytoskeleton reorganization and cell-matrix interactions in corneal epithelial cells [127,128,129,130,131]. Both ROCK 1 and ROCK 2 are activated in response to wounding, and ROCK inhibitor Y-27632 accelerates wound healing mainly by modulating cell-ECM and cell–cell adhesion in corneal endothelial cells, whereas Rho inhibitor C3 attenuates wound closure [128, 132]. Meanwhile, the use of ROCK inhibitors for enhancing endothelial wound healing is also garnering attention as a promising approach for corneal endothelial dysfunction. Corneal endothelial dysfunction results in corneal haziness and causes severe vision loss, a primary indication for corneal endothelial transplantation. Y-27632 promoted migration of corneal endothelial cells in different models both in vitro and in vivo (rabbit, monkey and human eyes), [133,134,135,136]. ROCK inhibitor eye drops have been tested for accelerating endothelial healing in a rabbit model and eyes of Fuchs’ endothelial dystrophy and bullous keratopathy patients that all underwent transcorneal freezing, and the topical administration of ROCK inhibitors improved corneal clarity in patients with central corneal edema caused by Fuchs’ dystrophy and in rabbit eyes (Fig. 9) [133, 137, 138]. Furthermore, it is reported that ROCK inhibitors promote the engraftment of injected cultured corneal endothelial cells to the recipient cornea, and the use of ROCK inhibitors as adjunct drugs for cell-based therapeutic treatment of corneal endothelial dysfunction are being proposed [139, 140]. Okumura et al. report the initiating clinical research into cell injection therapy using a ROCK inhibitor as an adjunct drug [141]. Collectively, the use of ROCK inhibitors in corneal disorders may prove to be efficient for treatment of corneal epithelial disease, edematous cornea due to endothelial dysfunction, and as a post-surgical management, not only in patients with corneal disorders but also in glaucoma patients.
Effect of ripasudil eye drops on corneal endothelial proliferation in a rabbit corneal freezing model. (a) A stainless-steel 7-mm-diameter probe was immersed in liquid nitrogen for 3 minutes and then placed onto the rabbit cornea for 15 seconds with the animal under general anesthesia. Then, one 0.4% ripasudil (four times daily) or 0.8% ripasudil (two times daily) eye drop was topically instilled, whereas vehicle was instilled in the fellow eye of each rabbit as a control (n = 6). Slit-lamp microscopy showed that control eyes exhibited hazy corneas after 48 hours, but eyes treated with 0.4% or 0.8% ripasudil eye drops exhibit less hazy corneas. No other adverse effects, such as the delay of corneal epithelial wound healing, severe conjunctival injection, and corneal opacity were observed. (Bb) The wound area of the corneal endothelium was evaluated by Alizarin red staining after 48 hours of treatment. Alizarin red staining images showed that the wound area tended to be smaller in eyes treated with 0.4% or 0.8% ripasudil eye drops than in control eyes. Scale bar: 1 mm. (C, D) Ki67+ cells located at the leading edge (3.5 mm distant from the center of the cornea), middle area (4.5 mm distant from the center of the cornea), and periphery (5.5 mm distant from the center of the cornea) were evaluated. Ki67 staining confirmed that 0.4% or 0.8% ripasudil eye drops promoted cell proliferation throughout the wound edge to the peripheral area. Administration of 0.8% ripasudil (two times per day) enhanced Ki67 expression to a higher level than was observed with 0.4% ripasudil eye drops (four times daily). Morphology was evaluated using actin staining performed with Alexa Fluor 594–conjugated phalloidin. Nuclei were stained with DAPI. Representative images of pupil centers are shown. Scale bar: 50 μm. Figure modified from Okumura et al. [138]
Anti-inflammatory properties
ROCK inhibitors can inhibit cell migration, invasion, and cytokinesis [142,143,144], all of which play roles in inflammation. Yamada et al. report that the topical administration of ripasudil significantly decreased the aqueous flare values and IOP in patients with anterior uveitis with glaucoma [145]. We recently reported that the systemic administration of ripasudil significantly reduced infiltrating cells and protein exudation in the aqueous humor, as well as the number of infiltrating cells in the iris-ciliary body (ICB) and adherent leukocytes in retinal vessels in endotoxin-induced uveitis (EIU) [146]. In the study, we revealed that the mRNA levels of IL-1β, IL-6, TNF-α, MCP-1, and intercellular adhesion molecule-1 in the ICB and retina were suppressed by ripasudil (Fig. 10) [146]. The other ROCK inhibitors, AMA0428 and AMA0526, are also reported to show anti-inflammatory effects in experimental diabetic retinopathy and corneal wound healing models, suggesting that Rho-ROCK signaling may play critical roles in ocular inflammation [147, 148].
The effect of ripasudil on mRNA levels of proinflammatory mediators in the ICB and the retina. The effects of ripasudil on LPS-induced mRNA levels of IL-1β, IL-6, TNF-α, MCP-1, and ICAM-1 in the ICB and the retina were evaluated by quantitative real-time PCR. *P < 0.05; **P < 0.01. Data are representative of at least three independent experiments. Figure modified from Uchida et al. [146]
Conclusions
Rho-ROCK signaling has been identified as a key pathway in the conventional outflow pathway, which integrates input from various bioactive factors in the AH; subsequent output results in cellular behavior that modulates AH outflow resistance.
Ripasudil is the first ROCK inhibitor approved for treatment of patients with glaucoma in Japan. It has been shown to reduce IOP in glaucoma patients, with additive efficacy even when used synergistically with other classes of glaucoma medications. Due to the multi-target nature of ROCK inhibitors, there has been concern regarding tolerance and unwanted side effects. To date, however, ripasudil has been shown to be safe, with only transient cosmetic conjunctival hyperemia and blepharitis side effects. Long-term treatment with ripasudil showed an additional IOP-lowering effect in eyes with glaucoma and OHT, suggesting that the late-onset remodeling of the ECM in glaucomatous eyes may elicit mild and delayed changes in IOP levels. The approval of a clinically available ROCK inhibitor has greatly enhanced our understanding of glaucoma pathology. However, despite our increased knowledge regarding the pathophysiology of glaucoma, the biological basis of disease progression/initiation, giving rise to IOP elevation despite open angles, remains elusive. As glaucoma is a multifactorial disease, it is difficult to explain its progression based only on IOP elevation. However, identification of a biological marker related to IOP elevation would constitute a novel yet fundamental therapeutic target for the treatment of glaucoma. Therefore, it is imperative to identify the cellular and molecular mechanisms that drive the increased resistance to AH outflow. Further studies are required to understand how Rho-ROCK signaling is regulated by bioactive factors in the AH outflow pathway, as well as to identify the mechanisms underlying dysregulation of this pathway in glaucomatous eyes.
In addition to lowering of IOP, ROCK inhibitors may provide other benefits for the treatment of glaucoma. The antifibrotic activity of ROCK inhibitors may attenuate the fibrotic-glaucomatous changes in the conventional pathway, which may represent the mechanism underlying initiation of IOP elevation in glaucoma patients. The neuroprotective effects of ROCK inhibitors may enhance RGC survival in patients with glaucoma.
A therapeutic strategy based on the use of ROCK inhibitors has a great deal of potential, as accumulating evidence indicates that glaucoma is a disease with multifaceted etiology and targets for pharmacological manipulation.
References
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi study. Ophthalmology. 2004;111:1641–8.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Caprioli J, Coleman AL. Blood pressure, perfusion pressure, and glaucoma. Am J Ophthalmol. 2010;149:704–12.
Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma. N Engl J Med. 2009;360:1113–24.
Quigley HA. Glaucoma. Lancet. 2011;377:1367–77.
Quigley HA. Open-angle glaucoma. N Engl J Med. 1993;328:1097–106.
Sommer A. Intraocular pressure and glaucoma. Am J Ophthalmol. 1989;107:186–8.
Gabelt BAT, Kaufman PL. Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res. 2005;24:612–37.
Stamer WD, Acott TS. Current understanding of conventional outflow dysfunction in glaucoma. Curr Opin Ophthalmol. 2012;23:135–43.
Mäepea O, Bill A. Pressures in the juxtacanalicular tissue and Schlemm’s canal in monkeys. Exp Eye Res. 1992;54:879–83.
Honjo M, Tanihara H, Inatani M, Kido N, Sawamura T, Yue BY, et al. Effects of Rho-associated protein kinase inhibitor Y-27632 on intraocular pressure and outflow facility. Invest Ophthalmol Vis Sci. 2001;42:137–44.
Kaneko Y, Ohta M, Inoue T, Mizuno K, Isobe T, Tanabe S, et al. Effects of K-115 (Ripasudil), a novel ROCK inhibitor, on trabecular meshwork and Schlemm’s canal endothelial cells. Sci Rep. 2016;6:19640.
Fujimoto T, Inoue T, Kameda T, Kasaoka N, Inoue-Mochita M, Tsuboi N, et al. Involvement of RhoA/Rho-associated kinase signal transduction pathway in dexamethasone-induced alterations in aqueous outflow. Invest Ophthalmol Vis Sci. 2012;53:7097–108.
Kameda T, Inoue T, Inatani M, Fujimoto T, Honjo M, Kasaoka N, et al. The effect of Rho-associated protein kinase inhibitor on monkey Schlemm’s canal endothelial cells. Invest Ophthalmol Vis Sci. 2012;53:3092–103.
Honjo M, Tanihara H, Kameda T, Kawaji T, Yoshimura N, Araie M. Potential role of Rho-associated protein kinase inhibitor Y-27632 in glaucoma filtration surgery. Invest Ophthalmol Vis Sci. 2007;48:5549–57.
Inoue T, Tanihara H. Rho-associated kinase inhibitors: a novel glaucoma therapy. Prog Retin Eye Res. 2013;37:1–12.
Clark AF, Wordinger RJ. The role of steroids in outflow resistance. Exp Eye Res. 2009;88:752–9.
Acott TS, Kelley MJ. Extracellular matrix in the trabecular meshwork. Exp Eye Res. 2008;86:543–61.
Stamer WD, Read AT, Sumida GM, Ethier CR. Sphingosine-1-phosphate effects on the inner wall of Schlemm’s canal and outflow facility in perfused human eyes. Exp Eye Res. 2009;89:980–8.
Shepard AR, Millar JC, Pang IH, Jacobson N, Wang WH, Clark AF. Adenoviral gene transfer of active human transforming growth factor-{beta}2 elevates intraocular pressure and reduces outflow facility in rodent eyes. Invest Ophthalmol Vis Sci. 2010;51:2067–76.
Keller KE, Aga M, Bradley JM, Kelley MJ, Acott TS. Extracellular matrix turnover and outflow resistance. Exp Eye Res. 2009;88:676–82.
Gottanka J, Chan D, Eichhorn M, Lutjen-Drecoll E, Ethier CR. Effects of TGF-beta2 in perfused human eyes. Invest Ophthalmol Vis Sci. 2004;45:153–8.
Wiederholt M, Thieme H, Stumpff F. The regulation of trabecular meshwork and ciliary muscle contractility. Prog Retin Eye Res. 2000;19:271–95.
Iyer P, Lalane R 3rd, Morris C, Challa P, Vann R, Rao PV. Autotaxin-lysophosphatidic acid axis is a novel molecular target for lowering intraocular pressure. PLoS One. 2012;7:e42627.
Wang RF, Williamson JE, Kopczynski C, Serle JB. Effect of 0.04% AR-13324, a ROCK, and norepinephrine transporter inhibitor, on aqueous humor dynamics in normotensive monkey eyes. J Glaucoma. 2015;24:51–4.
Burridge K, Wennerberg K. Rho and Rac take center stage. Cell. 2004;116:167–79.
Garcia-Mata R, Burridge K. Catching a GEF by its tail. Trends Cell Biol. 2007;17:36–43.
Cherfils J, Zeghouf M. Regulation of small GTPases by GEFs, GAPs, and GDIs. Physiol Rev. 2013;93:269–309.
Shimokawa H, Sunamura S, Satoh K. RhoA/rho-kinase in the cardiovascular system. Circ Res. 2016;118:352–66.
Ishizaki T, Maekawa M, Fujisawa K, Okawa K, Iwamatsu A, Fujita A, et al. The small GTP-binding protein Rho binds to and activates a 160 kDa Ser/Thr protein kinase homologous to myotonic dystrophy kinase. EMBO J. 1996;15:1885–93.
Thumkeo D, Watanabe S, Narumiya S. Physiological roles of Rho and Rho effectors in mammals. Eur J Cell Biol. 2013;92:303–15.
Somlyo AP, Somlyo AV. Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev. 2003;83:1325–58.
Maekawa M, Ishizaki T, Boku S, Watanabe N, Fujita A, Iwamatsu A, et al. Signaling from Rho to the actin cytoskeleton through protein kinases ROCK and LIM-kinase. Science. 1999;285:895–8.
Amano M, Kaneko T, Maeda A, Nakayama M, Ito M, Yamauchi T, et al. Identification of Tau and MAP2 as novel substrates of Rho-kinase and myosin phosphatase. J Neurochem. 2003;87:780–90.
Amano M, Nakayama M, Kaibuchi K. Rho-kinase/ROCK: a key regulator of the cytoskeleton and cell polarity. Cytoskeleton. 2010;67:545–54.
Fukata Y, Amano M, Kaibuchi K. Rho–Rho-kinase pathway in smooth muscle contraction and cytoskeletal reorganization of non-muscle cells. Trends Pharmacol Sci. 2001;22:32–9.
Uehata M, Ishizaki T, Satoh H, Ono T, Kawahara T, Morishita T, et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature. 1997;389:990–4.
Nakagawa O, Fujisawa K, Ishizaki T, Saito Y, Nakao K, Narumiya S. ROCK-I and ROCK-II, two isoforms of Rho-associated coiled-coil forming protein serine/threonine kinase in mice. FEBS Lett. 1996;392:189–93.
Julian L, Olson MF. Rho-associated coiled-coil containing kinases (ROCK): structure, regulation, and functions. Small GTPases. 2014;5:e29846.
Fukiage C, Mizutani K, Kawamoto Y, Azuma M, Shearer TR. Involvement of phosphorylation of myosin phosphatase by ROCK in trabecular meshwork and ciliary muscle contraction. Biochem Biophys Res Commun. 2001;288:296–300.
Whitlock NA, Harrison B, Mixon T, Yu XQ, Wilson A, Gerhardt B, et al. Decreased intraocular pressure in mice following either pharmacological or genetic inhibition of ROCK. J Ocul Pharmacol Ther. 2009;25:187–94.
Amin E, Dubey BN, Zhang SC, Gremer L, Dvorsky R, Moll JM, et al. Rho-kinase: regulation, (dys)function, and inhibition. Biol Chem. 2013;394:1399–410.
Knipe RS, Tager AM, Liao JK. The Rho kinases: critical mediators of multiple profibrotic processes and rational targets for new therapies for pulmonary fibrosis. Pharmacol Rev. 2015;67:103–17.
Loirand G. Rho Kinases in Health and Disease: From Basic Science to Translational Research. Pharmacol Rev. 2015;67:1074–95.
Lai AY, McLaurin J. Rho-associated protein kinases as therapeutic targets for both vascular and parenchymal pathologies in Alzheimer’s disease. J Neurochem. 2017. https://doi.org/10.1111/jnc.14130.
Epstein DL, Rowlette LL, Roberts BC. Acto-myosin drug effects and aqueous outflow function. Invest Ophthalmol Vis Sci. 1999;40:74–81.
Erickson-Lamy K, Schroeder A, Epstein DL. Ethacrynic acid induces reversible shape and cytoskeletal changes in cultured cells. Invest Ophthalmol Vis Sci. 1992;33:2631–40.
Kaufman PL, Barany EH. Cytochalasin B reversibly increases outflow facility in the eye of the cynomolgus monkey. Invest Ophthalmol Vis Sci. 1977;16:47–53.
Peterson JA, Tian B, Bershadsky AD, Volberg T, Gangnon RE, Spector I, et al. Latrunculin-A increases outflow facility in the monkey. Invest Ophthalmol Vis Sci. 1999;40:931–41.
Tian B, Geiger B, Epstein DL, Kaufman PL. Cytoskeletal involvement in the regulation of aqueous humor outflow. Invest Ophthalmol Vis Sci. 2000;41:619–23.
Tian B, Kaufman PL, Volberg T, Gabelt BT, Geiger B. H-7 disrupts the actin cytoskeleton and increases outflow facility. Arch Ophthalmol. 1998;116:633–43.
Waki M, Yoshida Y, Oka T, Azuma M. Reduction of intraocular pressure by topical administration of an inhibitor of the Rho-associated protein kinase. Curr Eye Res. 2001;22:470–4.
Rao PV, Deng PF, Kumar J, Epstein DL. Modulation of aqueous humor outflow facility by the Rho kinase-specific inhibitor Y-27632. Invest Ophthalmol Vis Sci. 2001;42:1029–37.
Tokushige H, Waki M, Takayama Y, Tanihara H. Effects of Y-39983, a selective Rho-associated protein kinase inhibitor, on blood flow in optic nerve head in rabbits and axonal regeneration of retinal ganglion cells in rats. Curr Eye Res. 2011;36:964–70.
Honjo M, Inatani M, Kido N, Sawamura T, Yue BYJT, Honda Y, et al. A myosin light chain kinase inhibitor, ML-9, lowers the intraocular pressure in rabbit eyes. Exp Eye Res. 2002;75:135–42.
Nishio M, Fukunaga T, Sugimoto M, Ikesugi K, Sumi K, Hidaka H, et al. The effect of the H-1152P, a potent Rho-associated coiled coil-formed protein kinase inhibitor, in rabbit normal and ocular hypertensive eyes. Curr Eye Res. 2009;34:282–6.
Feng Y, Yin Y, Weiser A, Griffin E, Cameron MD, Lin L, et al. Discovery of substituted 4-(pyrazol-4-yl)-phenylbenzodioxane-2-carboxamides as potent and highly selective Rho kinase (ROCK-II) inhibitors. J Med Chem. 2008;51:6642–5.
Pakravan M, Beni AN, Ghahari E, Varshochian R, Yazdani S, Esfandiari H, et al. The ocular hypotensive efficacy of topical fasudil, a Rho-associated protein kinase inhibitor, in patients with end-stage glaucoma. Am J Ther. 2017;24:e676–80.
de Kater AW, Shahsafaei A, Epstein DL. Localization of smooth muscle and nonmuscle actin isoforms in the human aqueous outflow pathway. Invest Ophthalmol Vis Sci. 1992;33:424–9.
Rao PV, Deng P, Sasaki Y, Epstein DL. Regulation of myosin light chain phosphorylation in the trabecular meshwork: role in aqueous humour outflow facility. Exp Eye Res. 2005;80:197–206.
Epstein DL, Freddo TF, Bassett-Chu S, Chung M, Karageuzian L. Influence of ethacrynic acid on outflow facility in the monkey and calf eye. Invest Ophthalmol Vis Sci. 1987;28:2067–75.
Ethier CR, Read AT, Chan DW. Effects of latrunculin-B on outflow facility and trabecular meshwork structure in human eyes. Invest Ophthalmol Vis Sci. 2006;47:1991–8.
Inoue T, Pattabiraman PP, Epstein DL, Vasantha Rao P. Effects of chemical inhibition of N-WASP, a critical regulator of actin polymerization on aqueous humor outflow through the conventional pathway. Exp Eye Res. 2010;90:360–7.
Bill A, Svedbergh B. Scanning electron microscopic studies of the trabecular meshwork and the canal of Schlemm—an attempt to localize the main resistance to outflow of aqueous humor in man. Acta Ophthalmol. 1972;50:295–320.
Stamer WD, Braakman ST, Zhou EH, Ethier CR, Fredberg JJ, Overby DR, et al. Biomechanics of Schlemm’s canal endothelium and intraocular pressure reduction. Prog Retin Eye Res. 2015;44:86–98.
Kumar J, Epstein DL. Rho GTPase-mediated cytoskeletal organization in Schlemm’s canal cells play a critical role in the regulation of aqueous humor outflow facility. J Cell Biochem. 2011;112:600–6.
Gong H, Jin X. Potts model partition functions on two families of fractal lattices. Physica A. 2014;414:143–53.
Pattabiraman PP, Maddala R, Rao PV. Regulation of plasticity and fibrogenic activity of trabecular meshwork cells by Rho GTPase signaling. J Cell Physiol. 2014;229:927–42.
Zhang M, Maddala R, Rao PV. Novel molecular insights into RhoA GTPase-induced resistance to aqueous humor outflow through the trabecular meshwork. Am J Physiol. 2008;295:C1057–70.
Vittitow JL, Garg R, Rowlette LL, Epstein DL, O’Brien ET, Borras T. Gene transfer of dominant-negative RhoA increases outflow facility in perfused human anterior segment cultures. Mol Vis. 2002;8:32–44.
Rao PV, Deng P, Maddala R, Epstein DL, Li CY, Shimokawa H. Expression of dominant negative Rho-binding domain of Rho-kinase in organ cultured human eye anterior segments increases aqueous humor outflow. Mol Vis. 2005;11:288–97.
Borras T, Buie LK, Spiga MG, Carabana J. Prevention of nocturnal elevation of intraocular pressure by gene transfer of dominant-negative RhoA in rats. JAMA Ophthalmol. 2015;133:182–90.
Pattabiraman PP, Rinkoski T, Poeschla E, Proia A, Challa P, Rao PV. RhoA GTPase-induced ocular hypertension in a rodent model is associated with increased fibrogenic activity in the trabecular meshwork. Am J Pathol. 2015;185:496–512.
Honjo M, Igarahi N, Kurano M, Yatomi Y, Igarashi K, Kano K, et al. Autotaxin-lysophosphatidic acid pathway in intraocular pressure regulation and glaucoma subtypes. Invest Ophthalmol Vis Sci. 2018;59:693–701. https://doi.org/10.1167/iovs.17-23218.
Honjo M, Igarahi N, Nishida J, Kurano M, Yatomi Y, Igarashi K, et al. Role of the autotaxin-LPA pathway in dexamethasone-induced fibrotic responses and extracellular matrix production in human trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2018;59(1):21–30. https://doi.org/10.1167/iovs.17-22807.
Kaufman PL, Barany EH. Loss of acute pilocarpine effect on outflow facility following surgical disinsertion and retrodisplacement of the ciliary muscle from the scleral spur in the cynomolgus monkey. Invest Ophthalmol. 1976;15:793–807.
Nakajima E, Nakajima T, Minagawa Y, Shearer TR, Azuma M. Contribution of ROCK in contraction of trabecular meshwork: proposed mechanism for regulating aqueous outflow in monkey and human eyes. J Pharma Sci. 2005;94:701–8.
Inoue T, Pecen P, Maddala R, Skiba NP, Pattabiraman PP, Epstein DL, et al. Characterization of cytoskeleton-enriched protein fraction of the trabecular meshwork and ciliary muscle cells. Invest Ophthalmol Vis Sci. 2010;51:6461–71.
Xin C, Wang RK, Song S, Shen T, Wen J, Martin E, et al. Aqueous outflow regulation: Optical coherence tomography implicates pressure-dependent tissue motion. Exp Eye Res. 2017;158:171–86.
Kiel JW, Kopczynski CC. Effect of AR-13324 on episcleral venous pressure in Dutch belted rabbits. J Ocul Pharmacol Ther. 2015;31:146–51.
Li G, Mukherjee D, Navarro I, Ashpole NE, Sherwood JM, Chang J, et al. Visualization of conventional outflow tissue responses to netarsudil in living mouse eyes. Eur J Pharmacol. 2016;787:20–31.
Tanihara H, Inatani M, Honjo M, Tokushige H, Azuma J, Araie M. Intraocular pressure-lowering effects and safety of topical administration of a selective ROCK inhibitor, SNJ-1656, in healthy volunteers. Arch Ophthalmol. 2008;126:309–15.
Skaat A, Jasien JV, Ritch R. Efficacy of topically administered Rho-kinase inhibitor AR-12286 in patients with exfoliation syndrome and ocular hypertension or glaucoma. J Glaucoma. 2016;25:e807–14.
Williams RD, Novack GD, van Haarlem T, Kopczynski C. Ocular hypotensive effect of the Rho kinase inhibitor AR-12286 in patients with glaucoma and ocular hypertension. Am J Ophthalmol. 2011;152(834–41):e1.
Lewis RA, Levy B, Ramirez N, Kopczynski CC, Usner DW, Novack GD. Correction: fixed-dose combination of AR-13324 and latanoprost: a double-masked, 28-day, randomised, controlled study in patients with open-angle glaucoma or ocular hypertension. Br J Ophthalmol. 2016;100:1016.
Bacharach J, Dubiner HB, Levy B, Kopczynski CC, Novack GD. Double-masked, randomized, dose-response study of AR-13324 versus latanoprost in patients with elevated intraocular pressure. Ophthalmology. 2015;122:302–7.
Lewis RA, Levy B, Ramirez N, Kopczynski CC, Usner DW, Novack GD. Fixed-dose combination of AR-13324 and latanoprost: a double-masked, 28-day, randomised, controlled study in patients with open-angle glaucoma or ocular hypertension. Br J Ophthalmol. 2016;100:339–44.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M. Phase 2 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol. 2013;156:731–6.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Suganami H, et al. Additive intraocular pressure-lowering effects of the Rho kinase inhibitor ripasudil (K-115) combined with timolol or latanoprost: a report of 2 randomized clinical trials. JAMA Ophthalmol. 2015;133:755–61.
Garnock-Jones KP. Ripasudil: first global approval. Drugs. 2014;74:2211–5.
Inazaki H, Kobayashi S, Anzai Y, Satoh H, Sato S, Inoue M, et al. Efficacy of the additional use of ripasudil, a Rho-kinase inhibitor, in patients with glaucoma inadequately controlled under maximum medical therapy. J Glaucoma. 2017;26:96–100.
Inazaki H, Kobayashi S, Anzai Y, Satoh H, Sato S, Inoue M, et al. One-year efficacy of adjunctive use of Ripasudil, a Rho-kinase inhibitor, in patients with glaucoma inadequately controlled with maximum medical therapy. Graefes Arch Clin Exp Ophthalmol. 2017;255:2009–15.
Matsumura R, Inoue T, Matsumura A, Tanihara H. Efficacy of ripasudil as a second-line medication in addition to a prostaglandin analog in patients with exfoliation glaucoma: a pilot study. Clin Drug Invest. 2017;37:535–9.
Sato S, Hirooka K, Nitta E, Ukegawa K, Tsujikawa A. Additive intraocular pressure lowering effects of the Rho kinase inhibitor, ripasudil in glaucoma patients not able to obtain adequate control after other maximal tolerated medical therapy. Adv Ther. 2016;33:1628–34.
Terao E, Nakakura S, Fujisawa Y, Fujio Y, Matsuya K, Kobayashi Y, et al. Time course of conjunctival hyperemia induced by a Rho-kinase inhibitor anti-glaucoma eye drop: ripasudil 0.4. Curr Eye Res. 2017;42:738–42.
Nakagawa H, Koizumi N, Okumura N, Suganami H, Kinoshita S. Morphological changes of human corneal endothelial cells after Rho-associated kinase inhibitor eye drop (ripasudil) administration: a prospective open-label clinical study. PLoS One. 2015;10:e0136802.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Fukushima A, et al. One-year clinical evaluation of 0.4% ripasudil (K-115) in patients with open-angle glaucoma and ocular hypertension. Acta Ophthalmol. 2016;94:e26–34.
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Suganami H, et al. Intra-ocular pressure-lowering effects of a Rho kinase inhibitor, ripasudil (K-115), over 24 hours in primary open-angle glaucoma and ocular hypertension: a randomized, open-label, crossover study. Acta Ophthalmol. 2015;93:e254–60.
Tanna AP, Rademaker AW, Stewart WC, Feldman RM. Meta-analysis of the efficacy and safety of alpha2-adrenergic agonists, beta-adrenergic antagonists, and topical carbonic anhydrase inhibitors with prostaglandin analogs. Arch Ophthalmol. 2010;128:825–33.
Kitazawa Y, Araie M. Double-masked, phase III comparative study of the combination ophthalmic solution of the 1% dorzolamide hydrochloride/0.5% timolol maleate (MK-0507A) in patients with glaucoma and ocular hypertension. Nippon Ganka Gakkai Zasshi. 2011;115:495–507 (in Japanese).
Harris A, Sergott RC, Spaeth GL, Katz JL, Shoemaker JA, Martin BJ. Color Doppler analysis of ocular vessel blood velocity in normal-tension glaucoma. Am J Ophthalmol. 1994;118:642–9.
Rankin SJ. Color Doppler imaging of the retrobulbar circulation in glaucoma. Surv Ophthalmol. 1999;43(Suppl 1):S176–82.
Nakabayashi S, Kawai M, Yoshioka T, Song YS, Tani T, Yoshida A, et al. Effect of intravitreal Rho kinase inhibitor ripasudil (K-115) on feline retinal microcirculation. Exp Eye Res. 2015;139:132–5.
Sugiyama T, Shibata M, Kajiura S, Okuno T, Tonari M, Oku H, et al. Effects of fasudil, a Rho-associated protein kinase inhibitor, on optic nerve head blood flow in rabbits. Invest Ophthalmol Vis Sci. 2011;52:64–9.
Watabe H, Abe S, Yoshitomi T. Effects of Rho-associated protein kinase inhibitors Y-27632 and Y-39983 on isolated rabbit ciliary arteries. Jpn J Ophthalmol. 2011;55:411–7.
Ohta Y, Takaseki S, Yoshitomi T. Effects of ripasudil hydrochloride hydrate (K-115), a Rho-kinase inhibitor, on ocular blood flow and ciliary artery smooth muscle contraction in rabbits. Jpn J Ophthalmol. 2017;5:423–32.
Flammer J, Orgul S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Goldhagen B, Proia AD, Epstein DL, Rao PV. Elevated levels of RhoA in the optic nerve head of human eyes with glaucoma. J Glaucoma. 2012;21:530–8.
Tura A, Schuettauf F, Monnier PP, Bartz-Schmidt KU, Henke-Fahle S. Efficacy of Rho-kinase inhibition in promoting cell survival and reducing reactive gliosis in the rodent retina. Invest Ophthalmol Vis Sci. 2009;50:452–61.
Hirata A, Inatani M, Inomata Y, Yonemura N, Kawaji T, Honjo M, et al. Y-27632, a Rho-associated protein kinase inhibitor, attenuates neuronal cell death after transient retinal ischemia. Graefes Arch Clin Exp Ophthalmol. 2008;246:51–9.
Kitaoka Y, Kitaoka Y, Kumai T, Lam TT, Kuribayashi K, Isenoumi K, et al. Involvement of RhoA and possible neuroprotective effect of fasudil, a Rho kinase inhibitor, in NMDA-induced neurotoxicity in the rat retina. Brain Res. 2004;1018:111–8.
Bermel C, Tönges L, Planchamp V, Gillardon F, Weishaupt JH, Dietz GPH, et al. Combined inhibition of Cdk5 and ROCK additively increase cell survival, but not the regenerative response in regenerating retinal ganglion cells. Mol and Cell Neurosci. 2009;42:427–37.
Sagawa H, Terasaki H, Nakamura M, Ichikawa M, Yata T, Tokita Y, et al. A novel ROCK inhibitor, Y-39983, promotes regeneration of crushed axons of retinal ganglion cells into the optic nerve of adult cats. Exp Neurol. 2007;205:230–40.
Van de Velde S, De Groef L, Stalmans I, Moons L, Van Hove I. Toward axonal regeneration and neuroprotection in glaucoma: Rho kinase inhibitors as promising therapeutics. Prog Neurobiol. 2015;131:105–19.
Yamamoto K, Maruyama K, Himori N, Omodaka K, Yokoyama Y, Shiga Y, et al. The novel Rho kinase (ROCK) inhibitor K-115: a new candidate drug for neuroprotective treatment in glaucoma. Invest Ophthalmol Vis Sci. 2014;55:7126–36.
Kitaoka Y, Sase K, Tsukahara C, Kojima K, Shiono A, Kogo J, et al. Axonal Protection by ripasudil, a Rho kinase inhibitor, via modulating autophagy in TNF-induced optic nerve degeneration. Invest Ophthalmol Vis Sci. 2017;58:5056–64.
Occleston NL, Daniels JT, Tarnuzzer RW, Sethi KK, Alexander RA, Bhattacharya SS, et al. Single exposures to antiproliferatives: long-term effects on ocular fibroblast wound-healing behavior. Invest Ophthalmol Vis Sci. 1997;38:1998–2007.
Khaw PT, Occleston NL, Schultz G, Grierson I, Sherwood MB, Larkin G. Activation and suppression of fibroblast function. Eye. 1994;8:188–95.
Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3:349–63.
Hinz B, Mastrangelo D, Iselin CE, Chaponnier C, Gabbiani G. Mechanical tension controls granulation tissue contractile activity and myofibroblast differentiation. Am J Pathol. 2001;159:1009–20.
Meyer-ter-Vehn T, Sieprath S, Katzenberger B, Gebhardt S, Grehn F, Schlunck G. Contractility as a prerequisite for TGF-beta-induced myofibroblast transdifferentiation in human tenon fibroblasts. Invest Ophthalmol Vis Sci. 2006;47:4895–904.
Van de Velde S, Van Bergen T, Vandewalle E, Kindt N, Castermans K, Moons L, et al. Rho kinase inhibitor AMA0526 improves surgical outcome in a rabbit model of glaucoma filtration surgery. Prog Brain Res. 2015;220:283–97.
Futakuchi A, Inoue T, Fujimoto T, Inoue-Mochita M, Kawai M, Tanihara H. The effects of ripasudil (K-115), a Rho kinase inhibitor, on activation of human conjunctival fibroblasts. Exp Eye Res. 2016;149:107–15.
Kojima S, Sugiyama T, Takai S, Jin D, Ueki M, Oku H, et al. Effects of ripasudil, a Rho-associated protein kinase inhibitor, on conjunctival scarring in a canine filtration surgery model. Curr Top Pharmacol. 2015;19:67–73.
SundarRaj N, Kinchington PR, Wessel H, Goldblatt B, Hassell J, Vergnes JP, et al. A Rho-associated protein kinase: differentially distributed in limbal and corneal epithelia. Invest Ophthalmol Vis Sci. 1998;39:1266–72.
Yin J, Lu J, Yu FS. Role of small GTPase Rho in regulating corneal epithelial wound healing. Invest Ophthalmol Vis Sci. 2008;49:900–9.
Anderson SC, Stone C, Tkach L, SundarRaj N. Rho and Rho-kinase (ROCK) signaling in adherens and gap junction assembly in corneal epithelium. Invest Ophthalmol Vis Sci. 2002;43:978–86.
Kim A, Petroll WM. Microtubule regulation of corneal fibroblast morphology and mechanical activity in 3-D culture. Exp Eye Res. 2007;85:546–56.
Kim A, Lakshman N, Petroll WM. Quantitative assessment of local collagen matrix remodeling in 3-D culture: the role of Rho kinase. Exp Cell Res. 2006;312:3683–92.
Yin J, Yu FS. Rho kinases regulate corneal epithelial wound healing. Am J Physiol Cell Physiol. 2008;295:378–87.
Okumura N, Koizumi N, Ueno M, Sakamoto Y, Takahashi H, Hirata K, et al. Enhancement of corneal endothelium wound healing by Rho-associated kinase (ROCK) inhibitor eye drops. Br J Ophthalmol. 2011;95:1006–9.
Okumura N, Koizumi N, Kay EP, Ueno M, Sakamoto Y, Nakamura S, et al. The ROCK inhibitor eye drop accelerates corneal endothelium wound healing. Invest Ophthalmol Vis Sci. 2013;54:2493–502.
Pipparelli A, Arsenijevic Y, Thuret G, Gain P, Nicolas M, Majo F. ROCK inhibitor enhances adhesion and wound healing of human corneal endothelial cells. PLoS One. 2013;8:e62095.
Okumura N, Inoue R, Okazaki Y, Nakano S, Nakagawa H, Kinoshita S, et al. Effect of the Rho Kinase Inhibitor Y-27632 on Corneal Endothelial Wound Healing. Invest Ophthalmol Vis Sci. 2015;56:6067–74.
Koizumi N, Okumura N, Ueno M, Kinoshita S. New therapeutic modality for corneal endothelial disease using Rho-associated kinase inhibitor eye drops. Cornea. 2014;33 Suppl 11:S25–31. https://doi.org/10.1097/ICO.0000000000000240.
Okumura N, Okazaki Y, Inoue R, Kakutani K, Nakano S, Kinoshita S, et al. Effect of the Rho-associated kinase inhibitor eye drop (ripasudil) on corneal endothelial wound healing. Invest Ophthalmol Vis Sci. 2016;57(3):1284–92. https://doi.org/10.1167/iovs.15-18586.
Okumura N, Kakutani K, Inoue R, Matsumoto D, Shimada T, Nakahara M, et al. Generation and feasibility assessment of a new vehicle for cell-based therapy for treating corneal endothelial dysfunction. PLoS One. 2016;11:e0158427.
Okumura N, Kinoshita S, Koizumi N. Cell-based approach for treatment of corneal endothelial dysfunction. Cornea. 2014;33 Suppl 11:S37–41. https://doi.org/10.1097/ICO.0000000000000229.
Okumura N, Kinoshita S, Koizumi N. The Role of Rho Kinase Inhibitors in Corneal Endothelial Dysfunction. Curr Pharm Des. 2017;23(4):660–6. https://doi.org/10.2174/1381612822666161205110027.
Itoh K, Yoshioka K, Akedo H, Uehata M, Ishizaki T, Narumiya S. An essential part for Rho-associated kinase in the transcellular invasion of tumor cells. Nat Med. 1999;5:221–5.
Yoshizaki H, Ohba Y, Parrini MC, Dulyaninova NG, Bresnick AR, Mochizuki N, et al. Cell type-specific regulation of RhoA activity during cytokinesis. J Biol Chem. 2004;279:44756–62.
Harvey SA, Anderson SC, SundarRaj N. Downstream effects of ROCK signaling in cultured human corneal stromal cells: microarray analysis of gene expression. Invest Ophthalmol Vis Sci. 2004;45:2168–76.
Yamada H, Yoneda M, Inaguma S, Gosho M, Murasawa Y, Isogai Z, et al. A Rho-associated kinase inhibitor protects permeability in a cell culture model of ocular disease, and reduces aqueous flare in anterior uveitis. J Ocul Pharmacol Ther. 2017;33:176–85.
Uchida T, Honjo M, Yamagishi R, Aihara M. The anti-inflammatory effect of ripasudil (K-115), a rho kinase (ROCK) inhibitor, on endotoxin-induced uveitis in rats. Invest Ophthalmol Vis Sci. 2017;58:5584–93.
Hollanders K, Hove IV, Sergeys J, Bergen TV, Lefevere E, Kindt N, et al. AMA0428, a potent rock inhibitor, attenuates early and late experimental diabetic retinopathy. Curr Eye Res. 2017;42:260–72.
Sijnave D, Van Bergen T, Castermans K, Kindt N, Vandewalle E, Stassen JM, et al. Inhibition of Rho-associated kinase prevents pathological wound healing and neovascularization after corneal trauma. Cornea. 2015;34:1120–9.
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science (JSPS) Grant Number 15K10854 (MH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Honjo, Analysis Support (Kowa); H. Tanihara, Analysis Support (Kowa).
Additional information
Section Organizer: Makoto Aihara, MD, PhD.
About this article
Cite this article
Honjo, M., Tanihara, H. Impact of the clinical use of ROCK inhibitor on the pathogenesis and treatment of glaucoma. Jpn J Ophthalmol 62, 109–126 (2018). https://doi.org/10.1007/s10384-018-0566-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0566-9