Abstract
Ripasudil hydrochloride hydrate (Glanatec® ophthalmic solution 0.4 %; hereafter referred to as ripasudil) is a small-molecule, Rho-associated kinase inhibitor developed by Kowa Company, Ltd. for the treatment of glaucoma and ocular hypertension. This compound, which was originally discovered by D. Western Therapeutics Institute, Inc., reduces intraocular pressure (IOP) by directly acting on the trabecular meshwork, thereby increasing conventional outflow through the Schlemm’s canal. As a result of this mechanism of action, ripasudil may offer additive effects in the treatment of glaucoma and ocular hypertension when used in combination with agents such as prostaglandin analogues (which increase uveoscleral outflow) and β blockers (which reduce aqueous production). The eye drop product has been approved in Japan for the twice-daily treatment of glaucoma and ocular hypertension, when other therapeutic agents are not effective or cannot be administered. Phase II study is underway for the treatment of diabetic retinopathy. This article summarises the milestones in the development of ripasudil leading to the first approval for glaucoma and ocular hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The main goal of glaucoma treatment is to reduce intraocular pressure (IOP), as it is associated with disease progression in patients with glaucoma and ocular hypertension [1, 2]. Current pharmacological treatments for glaucoma are divided into “inflow” drugs (e.g. β blockers, which lower IOP by decreasing aqueous humour production) and “outflow” drugs (e.g. prostaglandin analogues, which lower IOP by stimulation of aqueous humour drainage, largely through the uveoscleral outflow) [2]. Most currently approved antiglaucoma drugs do not target the trabecular meshwork, which is the main site of disease pathology [2].
Features and properties of ripasudil
Alternative names | Glanatec®; K 115; K-115; K115; ripasudil hydrochloride hydrate |
Class | Azepines, fluorine-compounds, isoquinolines, small-molecules, sulphonamides |
Mechanism of action | Rho-associated kinase inhibitor |
Route of Administration | Ophthalmic |
Pharmacodynamics | Highly selective and potent ROCK inhibitor; significantly reduces IOP in a dose-dependent manner in rabbits, monkeys and humans; maximum IOP reduction at 1–2 h; significantly greater reduction than with latanoprost in monkeys; has high intraocular permeability in rabbits |
Pharmacokinetics | |
Maximum plasma concentration (Cmax) | 0.622 ng/mL |
Time to Cmax | 0.083 h |
Area under plasma concentration-time curve | 0.231 ng·h/mL |
Plasma protein binding rate | 55.4–59.8 % |
Renal clearance | 7.112 L/h |
Elimination half-life | 0.455 h |
Most frequent adverse event | Conjunctival hyperaemia |
ATC codes | |
WHO ATC code | S01E (antiglaucoma preparations and miotics), S01L-A (antineovascularisation agents) |
EphMRA ATC code | S1E (miotics and antiglaucoma preparations), S1P (ocular antineovascularisation products) |
Chemical name | 4-fluoro-5-{[(2S)-2-methyl-1,4-diazepan-1-yl]sulfonyl}isoquinoline |
Ripasudil hydrochloride hydrate (Glanatec®; hereafter referred to as ripasudil) is a selective Rho-associated coiled coil-containing protein kinase (ROCK) inhibitor, an “outflow” drug which reduces IOP by stimulating aqueous humour drainage through the trabecular meshwork [3].
Ripasudil 0.4 % ophthalmic solution was approved in Japan in September 2014 for the treatment of glaucoma and ocular hypertension when other therapeutic drugs are not effective or cannot be administered, at a dosage of 1 drop in the eye, twice daily [4]. Kowa Company, Ltd. filed the NDA with Japan’s Ministry of Health, Labour and Welfare in October 2013 [4, 5]. The filing and approval triggered a milestone payment to D. Western Therapeutics Institute [4, 5].
Kowa Company, Ltd. completed phase III clinical development of ripasudil in Japan for the treatment of glaucoma and ocular hypertension in April 2013 [6]. The phase III programme consisted of three 8-week trials [one with ripasudil as monotherapy, one as concomitant therapy with timolol (a β blocker), and one as concomitant therapy with latanoprost (a prostaglandin analogue)] and one 52-week trial (ripasudil was administered as monotherapy or as concomitant therapy with a β blocker, a prostaglandin analogue and/or their combination drugs).
Kowa Company, Ltd. is also investigating the effects of ripasudil on ocular blood flow and macular oedema in patients with diabetic retinopathy associated with diabetic macular oedema in Japan [7].
1.1 Company Agreements
In September 2002, Kowa Company, Ltd. entered a licensing agreement with D. Western Therapeutics Institute, Inc. regarding the worldwide rights to ripasudil [8]. Under the terms of the agreement, D. Western Therapeutics Institute, Inc. is eligible to receive milestone payments. Other terms are undisclosed.
1.2 Patent Information
Kowa Company, Ltd. was issued a US patent (No. 8,193,193, entitled “Agent for prevention or treatment of glaucoma”) on 5 June 2012 for the use of ripasudil in patients with glaucoma [9].
2 Scientific Summary
2.1 Pharmacodynamics
ROCK, a serine/threonine kinase, is an important downstream effector of Rho guanosine triphosphatase, playing a critical, calcium-independent role in the regulation of the contractile tone of smooth muscle tissues [3]. Ripasudil is a highly selective and potent ROCK inhibitor [3]. The 50 % inhibitory concentrations (IC50) of ripasudil for ROCK 1 and ROCK 2 were 0.051 and 0.019 μmol/L, respectively; the IC50 for protein kinase A catalytic α, protein kinase C and calmodulin-dependent protein kinase α were 2.1, 27 and 0.37 μmol/L, respectively.
The IOP in both rabbits and monkeys was significantly (p < 0.05) reduced in a dose-dependent manner by topical instillation of ripasudil, at concentrations of 0.0625–0.5 % (in rabbits) and 0.1–0.4 % (in monkeys) [3]. In monkeys, maximum reduction of IOP versus vehicle was observed at 2 h, and was significantly (p < 0.001) greater with ripasudil 0.4 % than with latanoprost 0.005 %. The maximum reduction effect observed with latanoprost occurred at 4 h. The significant reduction in IOP observed in the monkeys receiving ripasudil 0.4 % continued until 6 h after instillation.

Chemical structure of ripasudil
Ripasudil has high intraocular permeability [3]. Whole-head autoradiography in rabbits showed that the peak radioactivity level was at 15 minutes after instillation of [14C]ripasudil in all eye tissues except for the lens, where the peak occurred at 4 h, and the vitreous body, where radioactivity was barely detected.
In rabbits, the aqueous flow rate did not significantly differ before and after instillation of ripasudil 0.4 % or uveoscleral outflow; however, the outflow facility in eyes treated with ripasudil 0.4 % was 2.2 times higher than in vehicle-treated eyes (p < 0.05) [3].
Some morphological changes in corneal endothelial cells have been noted with ripasudil ophthalmic solution in cynomolgus monkeys; however, these were considered to be of minimal toxicological significance, as they were transient, no enhancement with repeated instillation was found, and no significant structural changes occurred [10].
In healthy human volunteers, single instillations of ripasudil 0.05–0.8 % were associated with reductions from baseline in IOP in a dose-dependent manner, with the maximum reduction reached after 2 h; ripasudil 0.4 and 0.8 % were both associated with steady, significantly (p < 0.05) reduced IOPs compared with those in placebo recipients [11]. Ripasudil 0.05–0.8 % instilled twice daily for 7 days was also associated with significant (p < 0.05) reductions from baseline at 2 h post-dose in healthy volunteers (maximum reduction at 1–2 h); however, no significant difference was found between any ripasudil concentration and placebo with regard to change in IOP.
In-vitro and in-vivo data indicate that ripasudil attenuates retinal neovascularization and reduces the areas of avascular retina; it may thus may have potential in retinal neovascular diseases, such as diabetic retinopathy [12].
In cats, intravitreal ripasudil was associated with increased blood velocity and retinal blood flow [13]. Preliminary, preclinical data indicate that ripasudil may also be of use in neuroprotective treatment for glaucoma [14, 15].
2.2 Pharmacokinetics
After 7 days of twice-daily ripasudil 0.4 % treatment in 8 healthy male volunteers, the maximum plasma concentration of 0.622 ng/mL was reached after 0.083 h, and the area under the plasma concentration-time curve was 0.231 ng·h/mL, in a phase I pharmacokinetic trial [16]. The corresponding main metabolite (M1) pharmacokinetic values were 1.465 ng/mL, 0.500 h and 4.761 ng·h/mL, respectively. The metabolite M2 occurred at negligible levels.
Ripasudil has a plasma protein binding rate of 55.4–59.8 % [16]. Renal clearance was 7.112 L/h for ripasudil and 17.516 L/h for M1, and the elimination half-life was 0.455 and 2.189 h, respectively.
2.3 Therapeutic Trials
Ripasudil was associated with a significant, dosage-dependent reduction in IOP (primary endpoint) in a randomized, double-masked, placebo-controlled, multicentre, exploratory, phase II study (JapicCTI-101015) [17]. A total of 87 patients with primary open-angle glaucoma and 123 patients with ocular hypertension, and an untreated IOP of 21–35 mmHg, were randomized to 8 weeks of twice daily treatment with ripasudil 0.1, 0.2 or 0.4 % or placebo eye drops (n = 53, 54, 49 and 54, respectively). Before the final instillation, the mean change in IOP from baseline was −3.4, −3.2 and −3.5 versus −2.2 mmHg in ripasudil 0.1, 0.2 and 0.4 % versus placebo recipients (p < 0.05 for ripasudil 0.1 and 0.4 % vs. placebo); at 2 h after the final instillation the corresponding changes were −3.7, −4.2 and −4.5 versus −2.5 mmHg (p < 0.05 for all three ripasudil dosages vs. placebo), and at 8 h after instillation they were −3.2, −2.7 and−3.1 versus −1.9 mmHg (p < 0.05 for ripasudil 0.1 and 0.4 % vs. placebo) [17]. Baseline values were 23.4, 23.2, 23.2 and 23.0 mmHg, respectively. On the basis of the results from this study, ripasudil 0.4 % was selected as the optimal dosage.
Results from a randomized, open-label, placebo-controlled, crossover, multicentre, phase II study (JapicCTI-090708) showed that IOP could be controlled over a 24-h period with twice daily dosing [18]. A total of 28 patients with primary open-angle glaucoma or ocular hypertension were randomized to a 24-h period of treatment with twice daily ripasudil 0.2 %, ripasudil 0.4 % and placebo, in turn. The greatest change from baseline was observed at 2 h after instillation. From baseline IOPs of 20.3–20.9 mmHg, the mean IOP reduction was −6.4 and −4.3 mmHg at 2 h after the first instillation and at the time of the second instillation, respectively, in ripasudil 0.4 % recipients; corresponding changes in ripasudil 0.2 % recipients were −5.3 and −4.2 mmHg.
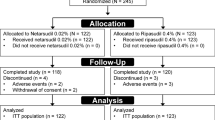
In a phase III randomized, double-masked, placebo-controlled trial in 107 patients with primary open-angle glaucoma or ocular hypertension and a baseline IOP ≥21 mmHg (JapicCTI-111564), twice-daily ripasudil 0.4 % was associated with a significantly greater change from baseline in mean IOP than placebo at 4, 6 and 8 weeks (mean across all time points) before the instillation (−2.9 vs. −1.8 mmHg), at 2 h after instillation (−4.0 vs. −1.7 mmHg), and as an average of both before and after the instillation (−3.4 vs. −1.8 mmHg) (all p < 0.001; mean baseline values were 22.7–23.1 mmHg) [19].
Twice-daily ripasudil 0.4 % plus twice-daily timolol was associated with a significantly greater change in mean IOP than placebo plus timolol in a randomized, double-masked, phase III study in 208 patients with primary open-angle glaucoma or ocular hypertension and a baseline IOP of ≥18 mmHg after monotherapy with timolol (JapicCTI-111701) [20]. At 4, 6 and 8 weeks (mean across all time points), the mean IOP reduction was −2.4 versus −1.5 mmHg before the instillation, −2.9 versus −1.3 mmHg at 2 h after instillation, and −2.6 and −1.4 mmHg as an average of both before and after the instillation (all p < 0.001). Mean baseline values were between 19.6 and 20.1 mmHg for this and the similar study (JapicCTI-111700) outlined below.
Twice-daily ripasudil 0.4 % plus once-daily latanoprost was generally associated with a significantly greater change in mean IOP than placebo plus latanoprost in a randomized, double-masked, phase III study in 205 patients with primary open-angle glaucoma or ocular hypertension and a baseline IOP of ≥18 mmHg after monotherapy with latanoprost (JapicCTI-111700) [20]. At 4, 6 and 8 weeks (mean across all time points), the mean IOP reduction was −2.2 versus −1.8 mmHg before the instillation (p = 0.06), −3.1 versus −1.8 mmHg at 2 h after instillation (p < 0.001), and −2.7 and −1.8 mmHg as an average of both before and after the instillation (p < 0.001).
Key clinical trials of ripasudil (Kowa Company, Ltd.)
Drugs(s) | Indication | Phase | Status | Location | Identifier |
|---|---|---|---|---|---|
Ripasudil | Primary open-angle glaucoma or ocular hypertension | II | Completed | Japan | JapicCTI-101015 |
Ripasudil | Primary open-angle glaucoma or ocular hypertension | II | Completed | Japan | JapicCTI-090708 |
Ripasudil | Primary open-angle glaucoma or ocular hypertension | III | Completed | Japan | JapicCTI-111564 |
Ripasudil + latanoprost | Primary open-angle glaucoma or ocular hypertension | III | Completed | Japan | JapicCTI-132286 |
Ripasudil + latanoprost | Primary open-angle glaucoma or ocular hypertension | III | Completed | Japan | JapicCTI-111700 |
Ripasudil + timolol | Primary open-angle glaucoma or ocular hypertension | III | Completed | Japan | JapicCTI-111701 |
Ripasudil (long-term) | Primary open-angle glaucoma, exfoliative glaucoma, pigmentary glaucoma or ocular hypertension | III | Completed | Japan | JapicCTI-111565 |
Ripasudil | Healthy volunteers | III | Completed | Japan | JapicCTI-121924 |
Ripasudil | Diabetic retinopathy and diabetic macular oedema | II | Recruiting | Japan | JapicCTI-142456 |
2.4 Adverse Events
The available data from clinical trials indicate that ripasudil is generally well tolerated in patients with primary open-angle glaucoma or ocular hypertension [17–20]. The most common adverse event in phase III trials was mild conjunctival hyperaemia, which ceased spontaneously within hours, and was not associated with patient withdrawal from treatment [19, 20]. The incidence of conjunctival hyperaemia was 73.6 % of ripasudil 0.4 and 1.9 % of placebo recipients in JapicCTI-111564 [19], 65.4 % of ripasudil 0.4 % plus timolol and 5.8 % of placebo plus timolol recipients in JapicCTI-111701 [20], and 55.9 % of ripasudil 0.4 % plus latanoprost and 8.7 % of placebo plus latanoprost recipients in JapicCTI-111700 [20].
In the phase II JapicCTI-101015 trial, the most common adverse event was also conjunctival hyperaemia (43.4, 57.4 and 65.3 vs. 13.0 % of ripasudil 0.1, 0.2 and 0.4 % vs. placebo recipients) [17]. Most conjunctival hyperaemia events were considered to be treatment related; however, all cases were of mild to moderate severity and most resolved spontaneously within several hours. Conjunctival hyperaemia is the most likely reason that there was a significant dosage dependency in the incidence of adverse events.
Other adverse events occurring in ≥3 patients in any ripasudil treatment group in JapicCTI-101015 were conjunctival haemorrhage [5.7, 1.9 and 0 vs. 0 % of ripasudil 0.1, 0.2 and 0.4 % vs. placebo recipients, respectively (one case in the ripasudil 0.1 % group was considered treatment-related)], ocular irritation (3.8, 1.9 and 12.2 vs. 9.3 %) and abnormal sensation in the eye [17].
Treatment withdrawal as a result of adverse events in JapicCTI-101015 occurred in a total of 6 patients: 5.7, 1.9 and 0 versus 3.7 % of ripasudil 0.1, 0.2 and 0.4 % versus placebo recipients [17]. Those adverse events leading to treatment withdrawal that were considered to be treatment related were photophobia, concomitant eye discomfort, asthma and conjunctival hyperaemia. No clinically significant changes in life signs or laboratory measures occurred.
2.5 Ongoing Clinical Trials
In February 2014, Kowa Company, Ltd. initiated an open-label, phase II trial to investigate the effects of ripasudil on ocular blood flow and macular oedema in patients with diabetic retinopathy associated with diabetic macular oedema (JapicCTI-142456); this trial is currently recruiting patients in Japan [7].
3 Current Status
Ripasudil received its first global approval on 26 September 2014 for glaucoma and ocular hypertension in Japan [4].
References
Novack GD. RHO kinase inhibitors for the treatment of glaucoma. Drugs Future. 2013;38(2):107–13.
Bucolo C, Salomone S, Drago F, et al. Pharmacological management of ocular hypertension: current approaches and future prospective. Curr Opin Pharmacol. 2013;13(1):50–5.
Isobe T, Mizuno K, Kaneko Y, et al. Effects of K-115, a rho-kinase inhibitor, on aqueous humor dynamics in rabbits. Curr Eye Res. 2014;39(8):813–22.
D. Western Therapeutics Institute. DWTI announces the acquisition of marketing approval in japan for a drug for treating glaucoma and ocular hypertension, K-115 [media release]. 26 Sept 2014. http://www.dwti.co.jp.
D. Western Therapeutics Institute Inc. Notice of NDA application in Japan for a glaucoma treatment drug “K-115 (nonproprietary name: Ripasudil hydrochloride hydrate” by Kowa Company Limited [media release]. 10 Oct 2013. http://www.dwti.co.jp.
D. Western Therapeutics Institute Inc. Notice of completion of late phase III clinical study of glaucoma treatment drug “K-115” in Japan [media release]. 10 Apr 2013. http://www.dwti.co.jp.
Kowa Company Ltd. K-115 Clinical pharmacology study [JAPIC identifier JapicCTI-142456]. 2014. http://clinicaltrials.jp. Accessed 22 Oct 2014.
D. Western Therapeutics Institute. Anti-glaucoma K-115 (Glanatec® ophthalmic solution 0.4 %). 2014. http://dwti.co.jp/english/business-outline/product-pipeline/anti-glaucoma-k-115. Accessed 23 Oct 2014.
Mizuno K, Matsumoto J. United States Patent No. US 8,193,193 B2: agent for prevention or treatment of glaucoma. 2012. http://patft.uspto.gov/. Accessed 23 Oct 2014.
Wato E, Omichi K, Yoneyama S, et al. Safety evaluation of morphological changes in corneal endothelial cells induced by K-115 in cynomolgus monkeys. Fundam Toxicol Sci. 2014;1(2):39–47.
Tanihara HMD, Inoue TMD, Yamamoto TMD, et al. Phase 1 clinical trials of a selective Rho kinase inhibitor, K-115. JAMA Ophthalmol. 2013;131(10):1288–95.
Nakao S, Arita R, Isobe T, et al. Therapeutic potential of topical ROCK inhibitor K-115 in retinal neovascularization [abstract no. FP-SA-51-4]. In: World Ophthalmology Congress. Tokyo; 2014.
Yoshioka T, Nakabayashi S, Nagaoka T, et al. Effect of intravitreal Rho kinase inhibitors on retinal microcirculation in cats [abstract no. 6855-D1185]. In: Association for research in vision and ophthalmology annual meeting. Fort Lauderdale; 2012.
Yamamoto K, Maruyama K, Himori N, et al. The novel Rho kinase (ROCK) inhibitor K-115: a new candidate drug for neuroprotective treatment in glaucoma. Invest Ophthalmol Vis Sci. 2014. doi:10.1167/iovs.13-13842.
Mizuno K, Koide T, Fujieda J, et al. Ocular hypotensive and neuroprotective effects on K-115, a novel Rho-kinase inhibitor [abstract no. 4805-B998]. Invest Ophthalmol Vis Sci. 2007;48.
Japanese Pharmaceuticals and Medical Devices Agency. Glanatec® (ripasudil hydrochloride hydrate ophthalmic solution 0.4 %): Japanese prescribing information. 2014. http://www.info.pmda.go.jp/. Accessed 22 Oct 2014.
Tanihara H, Inoue T, Yamamoto T, et al. Phase 2 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol. 2013;156(4):731–6.
Yamamoto T, Abe H, Kuwayama Y, et al. Efficacy and safety of the Rho kinase inhibitor, K-115, over 24 h in patients with primary open-angle glaucoma and ocular hypertension [abstract no. 216/A512]. In: Association for research in vision and ophthalmology annual meeting. Orlando; 2011.
Yamamoto T, Tanihara H, Kuwayama Y, et al. Phase 3 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension [abstract no. FP-TH-12-6]. In: World Ophthalmology Congress. Tokyo; 2014.
Tanihara H, Yamamoto T, Kuwayama Y, et al. Phase 3 randomized clinical studies of a Rho kinase inhibitor, K-115, in combination with timolol or latanoprost in primary open-angle glaucoma and ocular hypertension [abstract no. FP-TH-12-7]. In: World Ophthalmology Congress. Tokyo; 2014.
Disclosure
The preparation of this report was not supported by any external funding. During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. K.P. Garnock-Jones is a salaried employee of Adis, Springer SBM.
Author information
Authors and Affiliations
Corresponding author
Additional information
This profile has been extracted and modified from the Adis R&D Insight drug pipeline database. Adis R&D Insight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies, to market launch.
Rights and permissions
About this article
Cite this article
Garnock-Jones, K.P. Ripasudil: First Global Approval. Drugs 74, 2211–2215 (2014). https://doi.org/10.1007/s40265-014-0333-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0333-2