Abstract
Objective
There is controversy on whether lowering or restricting the level of sympathectomy can reduce compensatory sweating (CS). This study compared the results from sympathectomies performed to treat severe palmar hyperhidrosis using two distinct levels of T2–4 and T3–4.
Methods
One hundred and sixteen patients with primary palmar hyperhidrosis were randomly allocated to undergo either T2–4 sympathectomy treatment (T2–4 group) or T3–4 sympathectomy treatment (T3–4 group). Follow-up data were collected using a telephone questionnaire to assess efficacy, side effects, overall satisfaction, and factors affecting CS and the degree of satisfaction.
Results
There were no significant differences with respect to either CS or severe CS between the two treatment groups at 1, 6, or 12 months of follow-up. The total scores of the quality-of-life questionnaires after surgery were remarkably decreased compared with those before surgery in the two groups. However, no significant differences in quality-of-life scores were found between the two groups before surgery, or at 1, 6, or 12 months of follow-up. Age was predictive of severe CS at 6 months of follow-up (P = 0.045). Severe CS was inversely associated with patient satisfaction at 1, 6, and 12 months of follow-up.
Interpretation
The issue of whether lowering or restricting the level of sympathectomy reduces CS is controversial and needs more supportive evidence. Age may be a predictive factor for severe CS at 6 and 12 months of follow-up. Severe CS is the only known factor that affects patient satisfaction, and family history may also be associated with patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic thoracic sympathectomy (ETS) is known to be an efficient method for treating palmar hyperhidrosis (PH). The success rate of ETS is greater than 95 % in most series [1]. However, the side effect that has the largest effect on quality of life (QOL) is compensatory sweating (CS) [2]. The pathophysiology of CS remains unknown. Many authors believe that lowering or restricting the level of sympathectomy can reduce CS [3–7]. However, a thorough review of 246 articles has shown that the literature from 1999 to 2006 does not support this claim [8]. This controversy is partially because of poor definitions of the terms used for diagnosis of the problem and the surgical therapies applied [8, 9].
This study compared the results of two different levels of denervation, T2–4 versus T3–4, in a prospective randomized manner to evaluate whether lowering or restricting the extent of sympathectomy can reduce CS. We adopted anatomical definitions and standard metrics for symptomatic assessments endorsed by the Society of Thoracic Surgeons’ Expert Consensus for the Surgical Treatment of Hyperhidrosis [9].
Methods
Patients
From June 2008 to October 2010, 116 patients with PH who underwent ETS were prospectively enrolled. The study protocol that was applied to the patients was approved by the Research Ethics Committee of The Third Affiliated Hospital, Sun Yat-sen University. All of the patients gave their informed consent. Randomization was performed on the day before the operation. Recruitment stopped when 116 patients had undergone an operation. Randomization was carried out by an outpatient clinic employee using a closed-envelope method (Fig. 1). The patients were randomized into two groups: 56 patients were randomized to undergo T2–4 sympathectomy and 60 patients were randomized to undergo T3–4 sympathectomy (Table 1). Sex, age, body mass index (BMI), medical history, and family history were not significantly different between the groups. Severe primary PH was the indication for ETS. Exclusion criteria were the presence of bradycardia (heart rate <60 beats/min) [10, 11], having previously undergone thoracic surgery, or pleural or lung disorders.
Consort flowchart. A total of 116 patients with PH who underwent ETS were prospectively enrolled. All of the patients gave informed consent. Fifty-six patients were randomized to undergo T2–4 sympathectomy and 60 patients were randomized to undergo T3–4 sympathectomy. Thirty-seven patients were excluded according to our study design. The patients’ response rate for the telephone questionnaires was 100 % at 1, 6, and 12 months after surgery
Surgical procedure
All of the surgeries were performed by two surgeons, both experts in ETS. In accordance with the protocol, each surgeon had performed at least 100 ETS procedures. All of the patients were placed under general anesthesia with double-lumen endotracheal intubation and were in a semi-seated position. Two 5-mm mini-incisions were made in each hemithorax. The first incision was at the fifth intercostal space on the mid-axillary line. Thoracoscopy was introduced through this incision. The second incision was at the third intercostal space on the anterior line. Electrocautery was performed through this incision.
The sympathetic trunk was carefully identified at the costal heads by thoracoscopy. Patients randomized to the T2–4 sympathectomy group underwent sympathetic trunk electrocautery at the top of the second, third, and fourth ribs with an electrical hook. Patients randomized to the T3–4 sympathectomy group underwent sympathetic trunk electrocautery at the top of the third and fourth ribs with an electrical hook. The lung was routinely inflated after the procedure. Any ports were removed after the lung was fully expanded. Chest drains were not necessary. The same procedure was performed on the contralateral sympathetic trunk.
Follow-up and data collection
Patients underwent clinical and QOL assessments in person before surgery, and by means of a telephone questionnaire at 1, 6, and 12 months after the operation. CS was graded as minor, moderate, or embarrassing and severe CS (either disabling or incapacitating) [5, 12]. The patient’s degree of satisfaction was measured using the QOL instrument described by De Campos et al. [13]. The questionnaire had 20 questions with five levels for each answer, and the total score was out of 100 (total score before surgery: 20 = excellent and 100 = very poor/inferior; total score after surgery: 20 = much better and 100 = much worse).
Statistical analysis
Student’s t tests were used to compare continuous descriptive variables. χ 2 tests were used to compare categorical descriptive variables. Logistic regression analysis was used to examine the risk factors for severe CS. Univariate linear regression was used to analyze the factors affecting the satisfaction levels of the patients. Statistical significance was defined as P < 0.05.
Results
All of the patients were discharged within 48 h after their operations. There was no operative mortality. Ten patients (8.6 %) had postoperative pneumothorax, but only three patients with large pneumothoraxes (2.6 %) needed thoracocenteses. Neither Horner’s syndrome nor hemothorax occurred. The patients’ response rate for the telephone questionnaires was 100 % at 1, 6, and 12 months after surgery.
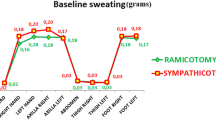
All of the patients’ PH resolved, and there were no recurrences during the 12 months of post-operative follow-up. A total of 50 (89.3 %), 50 (89.3 %), and 53 patients (94.6 %) had CS in the T2–4 group at 1, 6, and 12 months of follow-up, respectively. A total of 49 (81.2 %), 54 (90.0 %), and 53 patients (88.3 %) had CS (including severe CS) in the T3–4 group at 1, 6, and 12 months of follow-up, respectively (Table 2). There was no significant difference in the frequency of CS between the two groups at 1, 6, or 12 months of follow-up (P = 0.246, P = 0.900, and P = 0.226, respectively). There was also no significant difference in the frequency of severe CS between the two groups at 1 or 12 months of follow-up (Table 2).
The total scores of the QOL questionnaires in the two groups are shown in Table 3. There was a remarkable decrease in the total QOL scores after surgery compared with those before surgery in the two groups. However, there was no significant difference in QOL scores between the two groups before surgery, and at 1, 6, and 12 months of follow-up.
The factors affecting severe CS are shown in Table 4. The variables used to predict severe CS after surgery in multivariate logistic regression analysis included age, sex, medical history, family history, BMI, and different levels of sympathectomy. Age and family history were predictive of severe CS at 6 months of follow-up. None of the variables predicted severe CS at 1 and 12 months of follow-up. However, age tended to affect severe CS at 12 months of follow-up (P = 0.079).
Factors that affected the conversion of non-severe CS at 1 month of follow-up to severe CS at 12 months of follow-up are shown in Table 5. In multivariate logistic regression analysis, neither age, sex, medical history, family history, BMI, nor different levels of sympathectomy predicted a change in non-severe CS at 1 month of follow-up to severe CS at 12 months of follow-up.
Factors affecting patient satisfaction are shown in Table 6. In univariate analysis, severe CS was inversely associated with patient satisfaction at 1, 6, and 12 months of follow-up. Family history was associated with patient satisfaction at 1 month of follow-up, but not at 6 or 12 months of follow-up. Age, sex, medical history, BMI, and different levels of sympathectomy were not related to patient satisfaction at 1, 6, or 12 months of follow-up.
Discussion
In 1990, Kao and colleagues [14] first developed the minimally invasive technique of video endoscopic sympathectomy to treat PH. Currently, the procedure is accepted as a standard treatment technique for PH. However, there are still controversial opinions on the best level and extent of sympathectomy. The main reason for debate is the presence of CS after the operation. The reported rates of CS vary from 3 % [15] to 98 % [16]. Our study showed that CS occurred in more than 80 % of patients in both groups at 12 months post-operatively. This finding may be partially attributed to the fact that most of the patients came from Guangdong Province, which has a humid subtropical climate.
Currently, there is no standard strategy to reduce CS. One sympathectomy technique is to divide only the rami communicantes, while keeping the sympathetic trunk intact. Although this type of sympathectomy reduces the rate of CS, the PH recurrence rate is also high [17]. Currently, few surgeons use this technique.
In Li and colleagues’ [18] prospective, randomized trial, the incidence of severe CS was significantly lower in the T3 group than that in the T2–4 group (3 versus 10 %), and no recurrences were observed in either group. However, Lesèche et al. [19] reported that the incidence and severity of CS were not associated with the extent of sympathectomy. Katara and colleagues [20] noted that the procedure in the T2 group was as effective as that in the T2–3 group in terms of the recurrence rate, compensatory hyperhidrosis, and patient satisfaction in a randomized control trial.
In our study, the incidence of CS and severe CS was not different between the T2–4 and T3–4 groups at 1, 6, and 12 months of follow-up. There was also no difference between the total scores of the QOL questionnaires between the two groups. However, notably, the frequency of severe CS in both groups markedly increased from 1 month of follow-up to 12 months of follow-up (T2–4, 8.93–25.00 %; T3–4, 6.67–21.67 %). The reason for this finding could be because patients felt better and ignored severe CS once they were relieved of PH after surgery. However, after a time, they began to feel the discomfort of severe CS when they had become accustomed to living without PH.
The mechanism of CS after ETS is still unclear. Some researchers consider that ETS blocks the afferent projection of negative feedback to the hypothalamus, and would favor the appearance of CS at the periphery because of continuous efferent projections from the hypothalamus [3, 4]. Negative feedback of the sympathetic nervous system has a time-lag before a corrective mechanism is activated, but this mechanism is unstable. Time is required for the autonomic nervous system to build a stable negative feedback function. The exact mechanism of this process needs to be determined by further studies.
The T2 ganglion is considered important for sympathetic supply of the upper extremities. Some investigators have suggested that the preservation of the T2 ganglion may decrease the severity of CS [3, 21]. Based on feedback mechanisms, Chou and colleagues believe that T2 sympathectomy stops the main negative feedback sympathetic signals, and therefore, T2 sympathectomy causes more severe CS than T3 or T4 [3]. However, nerve fibers may travel superiorly and inferiorly in the sympathetic trunk, and the distribution of the sympathetic nerves may overlap. In our study, the incidence of CS and severe CS after preserving the T2 ganglion in the T3–4 group was not significantly different from that in the T2–4 group.
Previous studies have examined the predictive factors related to the severity of CS and the degree of satisfaction with sympathectomy procedures. In Chang and colleagues’ retrospective review, the extent of CS was correlated with BMI, but was independent of age, sex, family history, and the level of sympathectomy in univariate and multivariate analyses [5]. In their univariate analysis, patient satisfaction was correlated with age but was inversely correlated with the severity of CS, and was independent of sex, BMI, and family history. In their multivariate analysis, patient satisfaction was inversely correlated with the severity of CS and was independent of age, sex, BMI, and family history. BMI has been reported to be related to severe CS but not to the degree of satisfaction [22]. Another study reported that increased age is associated with severe CS [23]. Patients with CS are older (median age of 31 versus 23 years, P = 0.037) and have a BMI greater than 28 (P = 0.048) [24].
In our study, age was related to severe CS at 6 months of follow-up. Notably, age tended to affect severe CS at 12 months of follow-up. This finding suggests that our study will suffer from a high incidence of type-2 error, if we conclude that age is not predictive of severe CS.
In our study, BMI did not significantly affect severe CS at 6 and 12 months of follow-up. The reason for this finding may be related to the tendency of Asian young people to be less overweight than older people. In our study, severe CS was inversely associated with patient satisfaction at 1, 6, and 12 months of follow-up. Family history was associated with patient satisfaction at 1 month of follow-up. Family history may also have been associated with patient satisfaction at 6 and 12 months of follow-up because this reached borderline statistical significance. Family history has seldom been associated with patient satisfaction in other published studies, and the reason for this is still unknown.
In our study, notably, the rates of severe CS were as high as 25.0 % in the T2–4 group and 21.7 % in the T3–4 group at 12 months of follow-up. These results agree with other published values. Patients with PH should carefully consider the side effects of severe CS before surgery, especially elderly patients. Patients with a family history should also carefully consider their options before surgery because there may be a lower level of patient satisfaction after surgery.
The main reason that it is difficult to select the best level for sympathectomy to reduce CS is that the pathophysiology of PH is still unclear. The cause of PH appears to be an abnormal central response to emotional stress [9]. Many authors have suggested that a negative feedback mechanism may play an important role in the occurrence of CS after surgery. In our study, the transected regions of the sympathetic trunks between the T2–4 and T3–4 groups were both minor compared with the whole sympathetic trunk. Therefore, the differences in the transected regions were negligible, and the sympathetic trunk under the level of the sympathectomy was not remarkably different between the two groups. This similarity may be one of the reasons that there was no significant difference in the frequency of either CS or severe CS between the two treatment groups at 12 months of follow-up, once stable negative feedback of the autonomic nervous system had been achieved.
In summary, T2–4 and T3–4 sympathectomies are safe and effective therapies for severe PH. There are no significant differences in the frequency of CS or the degree of patient satisfaction with either T2–4 or T3–4 sympathectomies at 12 months of follow-up. Previous authors’ claims that lowering or restricting the level of sympathectomy can reduce CS are doubtful, and more positive evidence is needed. Age may be a predictive factor for severe CS at 6 and 12 months of follow-up. Severe CS is a factor that affects patient satisfaction, and family history may also be associated with patient satisfaction.
References
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern JB, Grunenwald D (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079
Chang YT, Li HP, Lee JY, Lin PJ, Lin CC, Kao EL, Chou SH, Huang MF (2007) Treatment of palmar hyperhidrosis: T(4) level compared with T(3) and T(2). Ann Surg 246:330–336
Chou SH, Kao EL, Lin CC, Chang YT, Huang MF (2006) The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc 20:1749–1753
Lin CC, Telaranta T (2001) Lin–Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol 90:161–166
Licht PB, Pilegaard HK (2004) Severity of compensatory sweating after thoracoscopic sympathectomy. Ann Thorac Surg 78:427–431
Kwong KF, Cooper LB, Bennett LA, Burrows W, Gamliel Z, Krasna MJ (2005) Clinical experience in 397 consecutive thoracoscopic sympathectomies. Ann Thorac Surg 80:1063–1066
Yazbek G, Wolosker N, de Campos JR, Kauffman P, Ishy A, Puech-Leao P (2005) Palmar hyperhidrosis—which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg 42:281–285
Kopelman D, Hashmonai M (2008) The correlation between the method of sympathetic ablation for palmar hyperhidrosis and the occurrence of compensatory hyperhidrosis: a review. World J Surg 32:2343–2356
Cerfolio RJ, De Campos JR, Bryant AS, Connery CP, Miller DL, DeCamp MM, McKenna RJ, Krasna MJ (2011) The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 91:1642–1648
Cl Lai, Chen WJ, Liu YB, Lee YT (2001) Bradycardia and permanent pacing after bilateral thoracoscopic T2-sympathectomy for primary hyperhidrosis. Pacing Clin Electrophysiol 24:524–525
O’Connor K, Molin F, Poirier P, Vaillancourt R (2009) Cardiac arrest as a major complication of bilateral cervico-dorsal sympathectomy. Interact Cardiovasc Thorac Surg 8(2):238–239
Liu Y, Yang J, Liu J, Yang F, Jiang G, Li J, Huang Y, Wang J (2009) Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg 35:398–402
De Campos JR, Kauffman P, Werebe EC, Andrade FL, Kusniek S, Wolosker N, Jatene FB (2003) Quality of life, before and after thoracic sympathectomy: report on 378 operated patients. Ann Thorac Surg 76:886–891
Katara AN, Domino JP, Cheah WK, So JB, Ning C, Lomanto D (2007) Comparing T2 and T2–T3 ablation in thoracoscopic sympathectomy for palmar hyperhidrosis: a randomized control trial. Surg Endosc 21:1768–1771
Kao MC, Chern SH, Cheng LC, Hsiao YY, Lee YS, Tsai JC (1994) Video thoracoscopic laser sympathectomy for palmar hyperhidrosis. Ann Acad Med Singapore 23:38–42
Sugimura H, Spratt EH, Compeau CG, Kattail D, Shargall Y (2009) Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg 137:1370–1376
Lai YT, Yang LH, Chio CC, Chen HH (1997) Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery 41(110–113):113–115
Gossot D, Toledo L, Fritsch S, Celerier M (1997) Thoracoscopic sympathectomy for upper limb hyperhidrosis: looking for the right operation. Ann Thorac Surg 64:975–978
Li X, Tu YR, Lin M, Lai FC, Chen JF, Dai ZJ (2008) Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2–4 ablation. Ann Thorac Surg 85:1747–1751
Leseche G, Castier Y, Thabut G, Petit MD, Combes M, Cerceau O, Besnard M (2003) Endoscopic transthoracic sympathectomy for upper limb hyperhidrosis: limited sympathectomy does not reduce postoperative compensatory sweating. J Vasc Surg 37:124–128
Schmidt J, Bechara FG, Altmeyer P, Zirngibl H (2006) Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact of restrictive denervation on compensatory sweating. Ann Thorac Surg 81:1048–1055
de Campos JR, Wolosker N, Takeda FR, Kauffman P, Kuzniec S, Jatene FB, de Oliveira SA (2005) The body mass index and level of resection: predictive factors for compensatory sweating after sympathectomy. Clin Auton Res 15:116–120
Baumgartner FJ, Reyes M, Sarkisyan GG, Iglesias A, Reyes E (2011) Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg 92:2015–2019
Miller DL, Bryant AS, Force SD, Miller JJ (2009) Effect of sympathectomy level on the incidence of compensatory hyperhidrosis after sympathectomy for palmar hyperhidrosis. J Thorac Cardiovasc Surg 138:581–585
Acknowledgments
This study was granted by the “985” project of Sun Yat-sen University (No. 82000-3321301) to Dr. Junhang Zhang.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, S., Huang, S., An, J. et al. Effect of lowering or restricting sympathectomy levels on compensatory sweating. Clin Auton Res 24, 143–149 (2014). https://doi.org/10.1007/s10286-014-0242-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-014-0242-1