Abstract
Background
Upper dorsal sympathectomy achieves excellent long-term results in the treatment of primary palmar hyperhidrosis. Compensatory hyperhidrosis (CHH) remains an unexplained sequel of this treatment, attaining in a small percentage of cases disastrous proportions. It has been claimed that lowering the level of sympathectomy (from T2 to T3 and even T4), substituting resection by other means of ablation, and limiting its extend reduce the occurrence of this sequel. This review was designed to evaluate the validity of these claims.
Methods
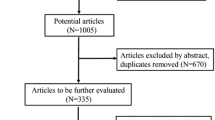
A MEDLINE search was performed for the years 1990–2006 and all publications about thoracoscopic upper dorsal sympathectomy for hyperhidrosis were retrieved.
Results
The search identified 42 techniques of sympathetic ablation. However, pertinent data for the present study were reported for only 23 techniques with multiple publications found only for 10. The only statistically valid results from this review point that T2 resection and R2 transection of the chain (over the second rib) ensue in less CHH than does electrocoagulation of T2. Further comparisons were probably prevented due to the enormous disparity in the reported results, indicating lack of standardization in definitions.
Conclusions
The compiled results published so far in the literature do not support the claims that lowering the level of sympathetic ablation, using a method of ablation other than resection, or restricting the extend of sympathetic ablation for primary palmar hyperhidrosis result in less CHH. In the future, standardization of the methods of retrieving and reporting data are necessary to allow such a comparison of data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperhidrosis is a pathological condition of excessive secretion of the eccrine sweat glands in amounts greater than required for physiological needs [1]. It may develop secondary to a variety of medical disorders [2] or it may be primary of unknown etiology. A multitude of therapeutic modalities have been proposed for the treatment of primary hyperhidrosis (PHH) [3, 4]. However, the only effective procedure to permanently abolish hyperhidrosis is ablation of the upper thoracic sympathetic chain. The several open approaches used in the past [5] are now supplanted by the endoscopic technique. Sympathectomy bears sequels, of which compensatory hyperhidrosis (CHH) is the gravest and most commonly observed [6, 7]. This phenomenon consists of increased perspiration after the operation in a part of the body not affected anatomically by the sympathectomy [8]. An old study [9] suggested that the total body amount of perspiration was unchanged by the sympathetic ablation, therefore, the increase of sweating in one part of the body representing a compensation for the arrest of sweating produced by the sympathetic ablation in another area. Hence the term “compensatory hyperhidrosis” was adopted. However, these results were not confirmed by another recent study [10]. Furthermore, CHH does not develop in all patients [11] and does not necessarily present immediately, but may appear even as late as 6 months postoperatively [12]. The degree of CHH is variable [13], and it may be alleviated or abate spontaneously [9, 14]. Moreover, arrest of sweating in the “compensatory area” by botulinum-toxin A injections did not result in increased sweating in a “new” area [15]. Finally, the opposite effect—decreased sweating in other parts of the body—also has been reported after sympathectomy [13, 14, 16]. Thus, the mechanism of CHH seems to be more complex than simple compensation for thermoregulatory purposes, and remains enigmatic and obscure. To reduce the incidence of this sequel, which is extremely troublesome in a certain percentage of operated patients [6], numerous variations in the type and extent of the technique of sympathetic ablation have been advocated. To evaluate the correlation between the technique and the subsequent degree and occurrence rate of CHH, we reviewed the literature pertinent to the results of thoracoscopic sympathectomy for primary palmar hyperhidrosis.
Materials and methods
Using the PubMed search engine, a quest was made for all publications that involved thoracoscopic sympathectomy for palmar hyperhidrosis listed in MEDLINE and published during the period January 1, 1990 to December 31, 2006. Retrieval was performed by the following key words and phrases: Hyperhidrosis AND Thoracoscopic sympathectomy; Hyperhidrosis AND Endoscopic sympathectomy; Palmar hyperhidrosis; Dorsal OR Thoracic AND Sympathectomy; Compensatory hyperhidrosis OR Compensatory sweating. Additional pertinent articles published before 1990 were obtained from the lists of references in the former publications. Reviews, editorials, letters to the editor, reports on the anatomy of the sympathetic system, and articles on the pathophysiology of its ablation were excluded. All articles describing series of patients who underwent thoracoscopic upper dorsal sympathectomy for palmar hyperhidrosis were identified, collected, and reviewed. Excluded from the collective review were case reports, articles reporting small series (less than 10 patients), articles reporting mixed series (more than one operative method and/or indications for surgery) in which separate data for each method or indication were not supplied, and articles missing follow-up on complications and sequels. The remaining articles were grouped by authors. Some authors periodically publish their data; the patients included in one publication were reviewed with some more cases in a subsequent study. To prevent inclusion of the same patients more than once in the collective review, only the last such publication of each group of authors was included in the present study. In case of double publications of the same series, only one was included in the present review.
The remaining articles were grouped according to the method of sympathetic ablation. The data that were retrieved included the number of patients, the percentage of immediate failures (persistent overperspiration of the hands), the number of patients for which a follow-up was documented, and the occurrence of CHH.
The various methods of sympathetic ablations were grouped as following: resection of parts of the sympathetic chain, electrocauterization of parts of the sympathetic chain, transection of the sympathetic chain at various levels, transection of sympathetic rami communicants (ramicotomies), and sympathetic ablations using clips.
Methods and level of ablations for which only one or two references were found could not be compared statistically. Therefore, comparison was made only for those methods and extent of ablations for which more than two reports were found.
We examined the success of sympathetic ablation by dividing the percentage of CHH by the percentage of obtained dry hands (morbidity/success index). The best possible index is zero, whereas the worst index should be one (or higher if CHH would occur despite failure to abolish PHH).
Statistical analysis was performed by using the Mann–Whitney nonparametric test. p ≤ 0.05 was considered statistically significant.
Results
After elimination of the nonpertinent retrieved articles (reviews, editorials, letters to the editor, etc.), 216 relevant papers were identified. After examining these studies, 87 publications were selected for the present review. The remaining 129 papers were eliminated. The reasons for their elimination are listed in Table 1.
The search identified 42 reported techniques of sympathetic ablation. However, pertinent data for the present study were reported for only 23 techniques. These were grouped and the data are reported in Table 2. The remaining published techniques, which were not included due to insufficiently reported data, are listed in Table 3.
An enormous variability in reported results was found for each technique and level of ablation. To illustrate this variability, the reported incidence of CHH is presented for T2–T3 resections (Fig. 1), T2–T3 cauterizations (Fig. 2), and R2–R3 transection of the sympathetic chain (Fig. 3). In Fig. 4, the compilations of the data regarding the occurrence of CHH are reported for each of the techniques of resection, cauterization, and transection of the sympathetic chain for each of which more than three publications were found. The statistical data and statistical comparison of the percent of CHH of these eight procedures are listed in Table 4. For the remaining two methods (ramicotomies and clipping), only one publication was found for each anatomical level, therefore, statistical evaluation and comparison were not possible.
Compilation of results for the occurrence of CHH after the commonest sympathetic procedures. Fifty percent of cases have values within the boxes. The upper point of the bars represents the largest observed value that is not outlier, whereas the lower point of the bars represents the smallest observed value that is not outlier. The horizontal line within the boxes represents the median value
The morbidity/success index for the various techniques is reported in Table 2. Statistical comparison of the indexes for T2–T3 resections, T2–T3 cauterizations, and R2–R3 chain transections is given in Table 5.
Discussion
Disparity of results
Despite the vast number of pertinent publications, more than half of the reported series could not be included in the present study. The reason is the enormous variability in data compilation and report. Even in apparently similar procedures, the wide disparity of the reported occurrence of CHH as illustrated in Figs. 1–3 underlines the lack of standardization in reporting data. It is inconceivable that exactly the same procedure would produce such a disparity of resulting CHH as 0.6% in one series and 100% in another. There are two explanations for this disparity: lack of standardization in definitions and anatomical variations.
Lack of standardization (different definitions of CCH, intensity of questioning, and length of follow-up) is probably the most important one. If only the patients who complained of CHH are listed as having developed this sequel of sympathectomy, the number will be low. If on the other hand, a meticulous inquiry is made concerning increased humidity in other areas of the body irrespective of its quantity, a high percentage of patients would be considered as having CHH. The figure would attain the 100% if specific laboratory measurements (sudometry) of the amount of perspiration are made in the areas prone to CHH before and after the sympathetic ablation [230].
Anatomical variations are another possible cause for disparity of results. The anatomy of the upper sympathetic chain has been studied and described in several studies. Although the second thoracic ganglion is considered to be located in the second intercostal space [231, 232], some other studies have shown a substantial variability. Chung et al. [233] have found in their cadaver anatomical study that only 50% of T2 ganglia were located in the second intercostal space, 9.1% of T2 ganglia were fused with the stellate ganglion, and 6% were located over the third rib. Variability exists not only concerning the level of the T2 ganglion, but also in the location of the chain along the horizontal axes of the rib heads [234]. Another anatomical inconsistency was reported regarding alternate neural pathways [231], the rami communicants [235], and the presence of the nerve of Kuntz (connecting the second intercostal to the ventral ramus of the first thoracic nerve) [236]. Therefore, if decision on the level of sympathetic ablation is made by rib count without observing the exact anatomy of the chain, the sympathetic ablation may be performed at a level different than the intended one.
Another cause for confusion in reported data is the count of the ribs. This is the intraoperative means of locating the appropriate ganglia. However, some authors claim that the first rib cannot be observed during thoracoscopy [237], whereas the majority of surgeons consider the uppermost observed rib to be the first one. In fact, it seems that the first rib is visible in some patients but can be only palpated in others [191]. Failure to achieve sympathicolysis has been attributed to erroneous rib count [238]. To overcome the problem, sympathetic ablation by clipping has been suggested [71]. However, unless intraoperative radiography is performed, clip application will not prevent incorrect estimation of the level as shown by Chou et al. [64], who reported 4.4% of clipping at an incorrect level, assessed only postoperatively.
A further bias in the published results may be due to the almost invariable use of diathermy, not only for thermocoagulation of ganglia or transection of the sympathetic chain, but even for dissection of the chain and resection of ganglia. The heath produced by the diathermy propagates and results in neural damage beyond the intended procedure. This additional injury cannot be measured but may explain such sequels as the occurrence of Horner’s syndrome [239] and brachial plexus injury [240]. The use of the harmonic scalpel instead of diathermy may eliminate collateral (and unpredictable) damage resulting from the heath propagated by the diathermy. The published data in which this instrument was used are too limited to allow any conclusions.
Methods and level of sympathetic ablation
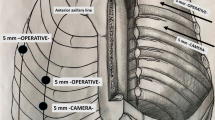
With the advent of endoscopic surgery, two basic changes in the technique of upper limb sympathetic denervation were introduced: 1) instead of resecting ganglia, some surgeons destroyed the ganglia or merely transected the sympathetic chain by electrocautery, and 2) instead of the second ganglion (T2), a lower than T2 ablation of the chain was chosen. In both of these modifications of the classical (T2 resection) approach for treating PHH, if failure occurs, contrary to the difficulty in reoperation after the open approaches, reoperation by endoscopy is relatively easy, both technically and clinically.
The reason for preferring ganglionic thermoablation or thermotransection of the chain is due to the relative simplicity of the latter procedure compared with the more time-consuming and demanding technique of endoscopic resection. Furthermore, although T2 resection achieves dry hands in almost 100% of cases [241], the results of thermoablation are usually not much inferior to those of resection [203]. However, exceptionally high percentages of recurrences of palmar overperspiration have been reported [242]—25.6% for T2 thermoablation—far exceeding the average published results (4.8%) [241].
During the period of open surgery, the second thoracic ganglion was considered to be the key to the sympathetic innervation of the upper extremity [144, 243]. Therefore, it was invariably accepted that this is the ganglion that should be resected to obtain dry hands, resection being the standard method of ablation. Recent anatomical studies confirm this anatomical supply to the hand [231], as did a recent sudometric study [230]. However, this accepted neuroanatomical standard has been challenged in recent years. Indeed, performing lower than T2 sympathetic ablations abolish or reduce palmar sweating in a large percentage of cases. In a recent publication, Drs. Lin and Telaranta [244] proposed what they called the Lin-Telaranta classification for the sympathetic innervation of the hand, axilla, and face. They claimed that to obtain sympathetic denervation of the hand while reducing the occurrence of CHH, T4 ganglion ablation only should be performed, thus preserving what they considered the afferent sympathetic fibers to the anterior portion of the hypothalamus, originating according to their hypothesis from the T2 and T3 ganglia. This is an interesting hypothesis, but as far as neuroanatomical pathways are concerned, they can be demonstrated only by appropriate stains, and no such stains have been performed to prove their hypothesis. Furthermore, recurrence rates of almost 23% have been reported for T4 ablations [242]. The main considered reason for recurrence is inadequate ablation of the sympathetic chain and not nerve regeneration [245]. It seems that such a high percentage of recurrences after T4 ablation and lack of stains to show the exact neuroanatomical pathways question the validity of the Lin-Telaranta classification. Regarding the claim that T4 ablations, compared with higher sympathetic procedures, reduce the amount of CHH [135, 226, 242], a compilation of data was not possible. In the first report [226], ablation was achieved by clipping the chain above T4, and in the second report [135] above and below T4 clipping was used. In the third report [242], the sympathetic chain was cauterized over R4 and R5. Thus, on clinical basis as well, the data published so far in the literature are insufficient to confirm the Lin-Telaranta hypothesis. Similarly, from the compiled data in the present review, no conclusion can be drawn for the T3 level of ablation. Only sporadic valid reports for only T3 ablations were found, each using a different technique [149, 173, 207, 222], making statistical comparison impossible. In the remaining studies, T3 and T4 ablations were performed jointly with another adjoining ganglion. However, even for the remaining levels and methods of ablation, due to the enormous discrepancies between reported results, the data compiled in the present review yielded only restricted information on the subject. If the level of ablation is responsible for the subsequent occurrence of CHH, one should expect approximately the same results for T2 resection and T2 thermocauterization, which according to the present review is not the case: T2 resection results in less CHH than T2 thermocauterization, as does transection of the sympathetic chain over the second rib (R2). Schmidt et al. [60] claimed that restricting the extend of resection reduces the subsequent occurrence of CHH, while Lesèche et al. [101] obtained opposite results. From the data of the present review, restricting resection resulted in less CHH only for T2 in comparison to T2–T4 resections. However, these statistical results should be considered with caution because of the enormous disparity of data. All other comparisons of levels, extend, and methods of ablation did not reach statistical significance. Thus, the question of how to reduce CHH after sympathetic ablation for PHH remains unanswered. Future studies, based on standard definition of terms and standardization of the method of follow-up, are required.
Methods of evaluating results
In the past, dry hands were considered the positive result of sympathectomy for PHH, although persisting or recurrent moisture of the hands (similar to normal perspiration) cannot be regarded as failures [246]. Therefore, many authors consider reduction of palmar perspiration as a positive result of surgery. However, there is no quantitative measurement of the amount of reduction. Thus, many authors evaluate their results by the satisfaction of the patients. There is no doubt that sympathetic ablation for PHH—being a procedure for functional and esthetic improvement—should result in the patient’s satisfaction. However, this method possesses two drawbacks: it is not a physiological evaluation of the procedure, and patient satisfaction reflects the totality of results, including failure to obtain dry hands, too dry hands, recurrence of palmar perspiration, and the development of any sequel, including CHH and Horner’s syndrome. Furthermore, to use “patient satisfaction” as a tool of comparing results of various techniques, levels, and extend of sympathectomy, standardization in the method used for evaluating the satisfaction also should be used. Such standardization should include the time lag between the operation and the point at which the data were obtained. No such standard has been established so far. However, if we seek to learn the physiologic outcome of the procedure concerning a specific sequel, an objective method of evaluating results is possible.
Morbidity/success index
In the present study, to evaluate the merit of sympathetic ablations for hyperhidrosis based on the occurrence of CHH, we used an index comparing the occurrence of CHH to the percentage of obtained dry hands (morbidity/success index). We were unable to calculate this index for many types of procedures due to insufficiently published data. For the most commonly published level of sympathetic ablation (T2–T3), the lowest mean index was for resections and the highest for cauterization (Table 5). However, no statistical significance was found while comparing these results. As already mentioned, the bias of this index is in its reflecting only the pathophysiological success of the procedure as far as dry hands and CHH result. It does not necessarily correlate with the satisfaction of the patient from the operation. Furthermore, it does not take into account the severity of preoperative sweating or CHH.
Conclusions
The pathophysiology of CHH remains obscure. The claim that lowering or restricting the level of sympathetic ablation reduces the occurrence of CHH is not supported by the data currently published in the literature, nor can a decision be made, based on these data, which method of sympathetic ablation is preferable. To obtain this vital information from future publications, definition of terms and standardization of the method of follow-up are required. Use of a quantitative method for determining CHH (sudometry) will prevent the enormous disparity in published results. The International Society of Sympathetic Surgery has produced a standard questionnaire for compilation of data and follow-up. It can be retrieved from the website of the Society: www.isss.net (enter: “About ISSS” and then “Recommendations”). We urge all surgeons with a special interest in sympathetic surgery to use this questionnaire prospectively and allow future compilation of standardized data so that the two paramount questions of sympathetic ablation, namely lowering the occurrence of CHH and the best method of sympathetic ablation, be elucidated.
References
Sato K, Kang WH, Saga K et al (1989) Biology of sweat glands and their disorders. II. Disorders of sweat gland function. J Am Acad Dermatol 20:713–726
Sato K (1991) Hyperhidrosis. JAMA 265:651
Hashmonai M, Kopelman D, Assalia A (2000) The treatment of primary palmar hyperhidrosis: a review. Surg Today 30:211–218
Connolly M, de Berker D (2003) Management of primary hyperhidrosis. A summary of the different treatment modalities. Am J Clin Dermatol 4:681–697
Hashmonai M, Schein M (1994) Upper thoracic sympathectomy–open approaches. In: Paterson-Brown S, Garden J (eds) Principles and practice of surgical laparoscopy. WB Saunders, London, pp 587–603
Lai Y-T, Yang L-H, Chio C-C et al (1997) Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery 41:110–115
Schick CH, Horbach T (2003) Sequelae of endoscopic sympathetic block. Clin Auton Res 13(Suppl 1):I/36–I/39
Shelley WB, Florence R (1960) Compensatory hyperhidrosis after sympathectomy. N Engl J Med 263:1056–1058
Shoenfeld Y, Shapiro Y, Machtiger A et al (1976) Sweat studies in hyperhidrosis palmaris and plantaris. Dermatologica 152:257–262
Kopelman D, Assalia A, Ehrenreich M et al (2000) The effect of upper dorsal thoracoscopic sympathectomy on the total amount of body perspiration. Surg Today 30:1089–1092
Plas EG, Függer R, Herbst F et al (1995) Complications of endoscopic thoracic sympathectomy. Surgery 118:493–495
Gjerris F, Olesen HP (1975) Palmar hyperhidrosis: long-term results following high thoracic sympathectomy. Acta Neurol Scand 51:167–172
Kopelman D, Hashmonai M, Ehrenreich M et al (1996) Upper dorsal thoracoscopic sympathectomy for palmar hyperhidrosis: improved intermediate-term results. J Vasc Surg 24:194–199
Cloward RB (1969) Hyperhidrosis. J Neurosurg 30:545–551
Heckmann M (1998) Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery 42:1403–1404
Shih C-J, Lin M-T (1979) Thermoregulatory sweating in palmar hyperhidrosis before and after upper thoracic sympathectomy. J Neurosurg 50:88–94
Weale FE (1980) Upper thoracic sympathectomy by transthoracic electrocoagulation. Br J Surg 67:71–72
Malone PS, Cameron AE, Rennie JA (1986) Endoscopic thoracic sympathectomy in the treatment of upper limb hyperhidrosis. Ann R Coll Surg Engl 68:93–94
Malone PS, Cameron AEP, Rennie JA (1986) The surgical treatment of upper limb hyperhidrosis. Br J Dermatol 115:81–84
Austin JJ, Doobay B, Schatz SW (1992) Transaxillary endoscopic laser sympathectomy. Can J Surg 35:414–416
Pace RF, Brown PM, Gutelius JR (1992) Thoracoscopic transthoracic dorsal sympathectomy. Can J Surg 35:509–511
Appleby TC, Edwards WH Jr (1992) Thorascopic dorsal sympathectomy for hyperhidrosis: a new approach. J Vasc Surg 16:121–123
Krasna MJ, Flowers J, Morvick R (1993) Thoracoscopic sympathectomy. Surg Laparosc Endosc 3:391–394
Millar AJW, Steiner Z, Rode H et al (1994) Trans-axillary transpleural sympathectomy for palmar hyperhidrosis in children: a 3 to 7 year follow-up of 9 cases. Eur J Pediatr Surg 4:3–6
Orteu CH, McGregor JM, Almeyda JR et al (1995) Recurrence of hyperhidrosis after endoscopic transthoracic sympathectomy: case report and review of the literature. Clin Exp Dermatol 20:230–233
Bonjer HJ, Hamming JF, du Bois NAJJ et al (1996) Advantages of limited thoracoscopic sympathectomy. Surg Endosc 10:721–723
Rashid HI, Osman HS, McIrvine AJ (1998) Thoracoscopic (upper thoracic) sympathectomy for primary palmar hyperhidrosis in children. Int J Clin Pract 52:537–538
Sugiyama S, Ikeya T, Hara H et al (1998) Dorsal sympathectomy for palmar hyperhidrosis by the thin thoracoscope. Kyobu Geka 51:1087–1089
Kesler KA, Brooks-Brunn JA, Campbell RL et al (2000) Thoracoscopic sympathectomy for hyperhidrosis palmaris: a periareolar approach. Ann Thorac Surg 70:314–317
Lau WT, Lee JD, Dang CR et al (2001) Improvement in quality of life after bilateral transthoracic endoscopic sympathectomy for palmar hyperhidrosis. Hawaii Med J 60:122,129,135
Gooi BH, Manjit S, Premnath N (2002) Thoracoscopic sympathectomy for primary palmar hyperhidrosis: the Penang Hospital experience. Med J Malaysia 57:66–69
Moon SW, Yoon JS, Jo KH et al (2005) Thoracoscopic sympathetic clamping in a patient with an azygos fissure. Surg Laparosc Endosc Percutan Tech 15:110–111
Guérin JC, Demolombe S, Brudon JR (1990) Thoracic sympathectomy by thoracoscopy. Rev Mal Resp 7:327–330
Flora G (1994) Thoracoscopic sympathectomy. Chirurg 65:677–679
Davies AL (1997) The current role of video-assisted thoracic surgery (VATS) in the overall practice of thoracic surgery. A review of 207 cases. Int Surg 82:229–231
Krasna MJ, Demmy TL, McKenna RJ et al (1998) Thoracoscopic sympathectomy: the US experience. Eur J Surg Suppl 580:19–21
Galán Gil G, Tarrazona Hervás V, Morcillo Aixelá A et al (1999) Indications and results of video-assisted thoracoscopic surgery. Reflections on 152 procedures. Arch Bronconeumol 35:477–482
Freund HR, Zamir O, Haskel Y et al (1999) Thoracoscopic surgery in a general surgical service. Surg Laparosc Endosc 9:39–41
Ghisletta N, Habicht J, Stulz P (1999) Video-assisted thoracoscopic sympathectomy: spectrum of indications and our own results (1995–1997). Schweitz Med Wochenschr 129:985–992
Johnson JP, Obasi C, Hahn MS et al (1999) Endoscopic thoracic sympathectomy. J Neurosurg (Spine 1) 91:90–97
Hoshina K, Amemiya R, Asato Y et al (2000) Ineffective and recurrent cases of thoracoscopic sympathectomy for hyperhidrosis and intractable pain. Kyobu Geka 53:136–140
Trignano M, Boatto R, Mastino GP et al (2000) Video-thoracoscopic sympathectomy in the treatment of Raynaud’s disease and palmar hyperhidrosis. Minerva Chir 55:17–23
Stadler P, Sebesta P (2001) Thoracoscopic thoracic sympathectomy - personal experience. Rozhl Chir 80:107–109
Duarte JBV, Kux P (2001) Efficacy of endoscopic thoracic sympathicotomy along with severing the Kuntz nerve in the treatment of chronic non-infectious rhinitis. Ann Chir Gynaecol 90:189–192
Roviaro GC, Varoli F, Vergani C et al (2002) State of the art in thoracoscopic surgery. A personal experience of 2000 videothoracoscopic procedures and an overview of the literature. Surg Endosc 16:881–892
Rivas de Andrés JJ, Freixinet Gilart J, Rodríguez de Castro F et al (2002) Spanish multicenter study of video-assisted thoracoscopy surgery. Arch Bronconeumol 38:60–63
Fuzi A, Szilagyi K, Rozsos I et al (2003) Experiences with endoscopic thoracic sympathectomy. Orv Hetil 144:621–624
Ayed AK, Al-Shawaf E (2004) A survey of 150 video-assisted thoracoscopic procedures in Kuwait. Med Princ Pract 13:159–163
Molins L, Fibla JJ, Pérez J et al (2006) Outpatient thoracic surgical programme in 300 patients: clinical results and economic impact. Eur J Cardiothorac Surg 29:271–275
Malone PS, Duignan JP, Hederman WP (1982) Transthoracic electrocoagulation (TEEC): a new and simple approach to upper limb sympathectomy. Ir Med J 75:20–21
Kao M-C, Chen Y-L, Lin J-Y et al (1996) Endoscopic sympathectomy treatment for craniofacial hyperhidrosis. Arch Surg 131:1091–1094
Drott C, Claes G, Olsson-Rex L et al (1998) Successful treatment of facial blushing by endoscopic transthoracic sympathicotomy. Br J Dermatol 138:639–643
Hsu C-P, Shia S-E, Hsia J-Y et al (2001) Experiences in thoracoscopic sympathectomy for axillary hyperhidrosis and osmidrosis. Focusing on the extent of sympathectomy. Arch Surg 136:1115–1117
Lin T-S (2001) Endoscopic clipping in video-assisted thoracoscopic sympathetic blockade for axillary hyperhidrosis. An analysis of 26 cases. Surg Endosc 15:126–128
Lin TS, Chou MC (2002) Needlescopic thoracic sympathetic block by clipping for craniofacial hyperhidrosis. Surg Endosc 16:1055–1058
Kim DH, Paik HC, Lee DY (2004) Comparative analysis of T2 selective division of rami-communicantes (ramicotomy) with T2 sympathetic clipping in the treatment of craniofacial hyperhidrosis. Eur J Cardiothorac Surg 26:396–400
Callejas MA, Rubio M, Iglesias M et al (2004) Video-assisted thoracoscopic sympathectomy for the treatment of facial blushing: ultrasonic scalpel versus diathermy. Arch Bronconeumol 40:17–19
Licht PB, Jørgensen OD, Ladegaard L et al (2005) Thoracoscopic sympathectomy for axillary hyperhidrosis: the influence of T4. Ann Thorac Surg 80:455–460
Adair A, George ML, Camprodon R et al (2005) Endoscopic sympathectomy in the treatment of facial blushing. Ann Roy Coll Surg Engl 87:358–360
Schmidt J, Bechara FG, Altmeyer P et al (2006) Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact on restrictive denervation on compensatory sweating. Ann Thorac Surg 81:1048–1055
Murphy MO, Ghosh J, Khwaja N et al (2006) Upper dorsal endoscopic thoracic sympathectomy: a comparison of one- and two-port ablation techniques. Eur J Cardiothorac Surg 30:223–227
Reisfeld R (2006) Sympathectomy for hyperhidrosis: should we place the clamps at T2–T3 or T3–T4? Clin Auton Res 16:384–389
Chou S-H, Kao E-L, Lin C-C et al (2006) The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc 20:1749–1753
Chou S-H, Kao E-L, Lin C-C et al (2006) The outcome of ganglion clipping in hyperhidrosis and blushing. Clin Auton Res 16:240–242
Galbis-Caravajal JM, Sales-Badia JG, Cuenca-Torres M et al (2006) Thoracic sympathectomy in primary hyperhidrosis: patient satisfaction. Cir Esp 79:299–304
Edmondson RA, Banerjee AK, Rennie JA (1992) Endoscopic transthoracic sympathectomy in the treatment of hyperhidrosis. Ann Surg 215:289–293
Masters A, Rennie JA (1992) Endoscopic transthoracic sympathectomy for idiopathic upper limb hyperhidrosis. Clin Auton Res 2:349–352
Ahn SS, Machleder HI, Concepcion B et al (1994) Thoracoscopic cervicodorsal sympathectomy: preliminary results. J Vasc Surg 20:511–519
Pillay PK, Kumar K, Tang KK (1997) Video-endoscopic and mini-endoscopic sympathectomy for hyperhidrosis. Stereotact Funct Neurosurg 69:274–277
Lewis DR, Irvine CD, Smith FCT et al (1998) Sympathetic skin response and patient satisfaction on long-term follow-up after thoracoscopic sympathectomy for hyperhidrosis. Eur J Vasc Endovasc Surg 15:239–243
Lin C-C, Mo L-R, Lee L-S et al (1998) Thoracoscopic T2-sympathetic block by clipping—a better and reversible operation for treatment of hyperhidrosis palmaris: experience with 326 cases. Eur J Surg Suppl 580:13–16
Reardon PR, Preciado A, Scarborough T et al (1999) Outpatient endoscopic thoracic sympathectomy using 2-mm instruments. Surg Endosc 13:1139–1142
Lee DY, Hong YJ, Shin HK (1999) Thoracoscopic sympathetic surgery for hyperhidrosis. Yonsei Med J 40:589–595
Lee DY, Yoon YH, Shin HK et al (2000) Needle thoracic sympathectomy for essential hyperhidrosis: intermediate-term follow-up. Ann Thorac Surg 69:251–253
Sung SW, Kim YT, Kim JH (2000) Ultra-thin needle thoracoscopic surgery for hyperhidrosis with excellent cosmetic effects. Eur J Cardiothorac Surg 17:691–696
Swan MC, Paes T (2001) Quality of life evaluation following endoscopic transthoracic sympathectomy for upper limb and facial hyperhidrosis. Ann Chir Gynaecol 90:157–159
Ueyama T, Matsumoto Y, Abe Y et al (2001) Endoscopic thoracic sympathectomy in Japan. Ann Chir Gynaecol 90:200–202
de Campos JRM, Kauffman P, Werebe E de C et al (2003) Quality of life, before and after thoracic sympathectomy: report on 378 operated patients. Ann Thorac Surg 76:886–891
Ueyama T, Ueyama K, Ueyama K et al (2004) Thoracoscopic sympathetic surgery for hand sweating. Ann Thorac Cardiovasc Surg 10:4–8
Kwong KF, Cooper LB, Bennett LA et al (2005) Clinical experience in 357 consecutive thoracoscopic sympathectomies. Ann Thorac Surg 80:1063–1066
Moya J, Ramos R, Vives N et al (2004) Compensatory sweating after upper thoracic sympathectomy: prospective study of 123 cases. Arch Bronconeumol 40:360–363
Wilson MJ, Magee TR, Galland RB et al (2005) Results of thoracoscopic sympathectomy for the treatment of axillary and palmar hyperhidrosis with respect to compensatory hyperhidrosis and dry hands. Surg Endosc 19:254–256
Dewey TM, Herbert MA, Hill SL et al (2006) One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg 81:1227–1233
Panhofer P, Zacherl J, Jakesz R et al (2006) Improved quality of life after sympathetic block for upper limb hyperhidrosis. Br J Surg 93:582–586
Moya J, Ramos R, Morera R et al (2006) Results of high bilateral endoscopic thoracic sympathectomy and sympatholysis in the treatment of primary hyperhidrosis: a study of 1016 procedures. Arch Bronconeumol 42:230–234
Moya J, Ramos R, Morera R et al (2006) Thoracic sympathicolysis for primary hyperhidrosis: a review of 918 procedures. Surg Endosc 20:598–602
Cinà CS, Robertson SGW, Young EJM et al (2006) Effect of endoscopic sympathectomy for hyperhidrosis on quality of life using the illness intrusiveness rating scale. Minerva Chir 61:231–239
Nüesch B, Ammann J, Hess P et al (1996) Thoracic sympathectomy for palmar hyperhidrosis. Swiss Surg 2:112–115
Friedel G, Linder A, Toomes H (1993) Selective video-assisted thoracoscopic sympathectomy. Thorac Cardiovasc Surg 41:245–248
Pillay PK, Thomas J, Mack P (1994) Thoracoscopic ganglionectomy for hyperhidrosis. Stereotact Funct Neurosurg 63:198–202
Svartholm E, Asking B (1994) Thoracoscopic surgery of palmar hyperhidrosis. Eur J Surg Suppl 572:21
Kao MC, Lin JY, Chen YL et al (1996) Minimally invasive surgery: video endoscopic thoracic sympathectomy for palmar hyperhidrosis. Ann Acad Med Singapore 25:673–678
Yilmaz EN, Dur AHM, Cuesta MA et al (1996) Endoscopic versus transaxillary thoracic sympathectomy for primary axillary and palmar hyperhidrosis and/or facial blushing: 5-year-experience. Eur J Cardiothorac Surg 10:168–172
Tan V, Nam H (1998) Results of thoracoscopic sympathectomy for 96 cases of palmar hyperhidrosis. Ann Thorac Cardiovasc Surg 4:244–246
Uchino T, Ishimaru S, Makimura S et al (1999) Current appraisal of endoscopic thoracic sympathectomy: results of the national questionnaire surgery. Kyobu Geka 52:204–209
Yim APC, Liu HP, Lee TW et al (2000) “Needlescopic” video-assisted thoracic surgery for palmar hyperhidrosis. Eur J Cardiothorac Surg 17:697–701
Krasna MJ, Jiao X, Sonett J et al (2000) Thoracoscopic sympathectomy. Surg Laparosc Endosc Percutan Tech 10:314–318
Reisfeld R, Nguyen R, Pnini A (2002) Endoscopic thoracic sympathectomy for hyperhidrosis: experience with both cauterization and clamping methods. Surg Laparosc Endosc Percut Tech 12:255–267
Gómez Sebastián G, Fibla JJ (2002) Video-assisted thoracoscopic sympathectomy: the experience of a Spanish cooperative group. Arch Bronconeumol 38:64–66
Gossot D, Galetta D, Pascal A et al (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079
Lesèche G, Castier Y, Thabut G et al (2003) Endoscopic transthoracic sympathectomy for upper limb hyperhidrosis: limited sympathectomy does not reduce postoperative compensatory sweating. J Vasc Surg 37:124–128
Byrne J, Walsh TN, Hederman WP (1993) Thoracoscopic sympathectomy. Endosc Surg Allied Technol 1:261–265
Lévy I, Ariche A, Sebbag G et al (1995) Thoracoscopic upper thoracic sympathectomy: a method of choice for the treatment of palmar hyperhidrosis. Ann Chir 49:858–862
Lin C-C, Mo L-R (1996) Experience in thoracoscopic sympathectomy for hyperhidrosis with concomitant pleural adhesion. Surg Laparosc Endosc 4:258–261
Chen H-J, Liang C-L, Lu K (2001) Associated change in plantar temperature and sweating after transthoracic endoscopic T2-3 sympathectomy for palmar hyperhidrosis. J Neurosurg (Spine 1) 95:58–63
Naruse H, Moriyasu K, Yokokawa H et al (2001) Endoscopic transthoracic sympathectomy (ETS) with a fine 2-mm thoracoscope in palmar hyperhidrosis. Kyobu Geka 54:555–559
Helmy MA, Ahmed HA, Allam MF (2001) Thoracoscopic sympathectomy for treatment of hyperhidrosis: surgical experience and results of 30 cases. J Egypt Soc Parasitol 31:835–842
Lin C-C, Wu H-H (2001) Endoscopic T4-sympathetic block by clamping (ESB4) in treatment of hyperhidrosis palmaris et axillaris: experiences of 165 cases. Ann Chir Gynaecol 90:167–169
Singh B, Moodley J, Ramdial PK et al (2001) Pitfalls in thoracoscopic sympathectomy: mechanisms for failure. Surg Laparosc Endosc Percutan Tech 6:364–367
Duarte JBV, Kux P, Castro CHV et al (2003) Fast track endoscopic thoracic sympathicotomy. Clin Auton Res 13(Suppl 1):I/63–I/65
Castier Y, Besnard M, Lesèche G (2004) Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limbs. J Chir 141:31–35
Kao M-C (1992) Video endoscopic sympathectomy using a fiberoptic CO2 laser to treat palmar hyperhidrosis. Neurosurgery 30:131–135
Kao M-C (1992) Laser endoscopic sympathectomy for palmar hyperhidrosis. Lasers Surg Med 12:308–312
Kao M-C, Lee W-Y, Yip K-M et al (1994) Palmar hyperhidrosis in children: treatment with video endoscopic laser sympathectomy. J Pediatr Surg 29:387–391
Claes G, Drott C, Göthberg G (1993) Endoscopic electrocautery of the thoracic sympathetic chain: a minimally invasive way to treat palmar hyperhidrosis. Scand J Plast Reconstr Hand Surg 27:29–33
Claes G, Drott C, Göthberg G (1993) Thoracoscopy for autonomic disorders. Ann Thorac Surg 56:715–716
Göthberg G, Drott C, Claes G (1994) Thoracoscopic sympathicotomy for hyperhidrosis – surgical technique, complications and side effects. Eur J Surg Suppl 572:51–53
Drott C, Göthberg G, Claes G (1995) Endoscopic transthoracic sympathectomy: an efficient and safe method for the treatment of hyperhidrosis. J Am Acad Dermatol 33:78–81
Rex LO, Drott C, Claes G et al (1998) The Borås experience of endoscopic thoracic sympathicotomy for palmar, axillary, facial hyperhidrosis and facial blushing. Eur J Surg Suppl 580:23–26
Lin T-S (1999) Transthoracic endoscopic sympathectomy for palmar hyperhidrosis in children and adolescents: analysis of 350 cases. J Laparoendosc Adv Surg Tech A 9:331–334
Lin T-S (1999) Transthoracic endoscopic sympathectomy for palmar and axillary hyperhidrosis in children and adolescents. Pediatr Surg Int 15:475–478
Lin T-S, Fang H-Y (1999) Transthoracic endoscopic sympathectomy in the treatment of palmar hyperhidrosis–with emphasis on perioperative management (1,360 case analyses). Surg Neurol 52:453–457
Lin T-S, Fang H-Y, Wu C-Y (2000) Repeat transthoracic endoscopic sympathectomy for palmar and axillary hyperhidrosis. Surg Endosc 14:134–136
Lin T-S, Wang N-P, Huang L-C (2001) Pitfalls and complication avoidance associated with transthoracic endoscopic sympathectomy for primary hyperhidrosis (analysis of 2200 cases). Int J Surg Investig 2:377–385
Lin T-S, Huang L-C, Wang N-P et al (2001) Video-assisted thoracoscopic T2 sympathetic block by clipping for palmar hyperhidrosis: analysis of 52 cases. J Laparoendosc Adv Surg Tech A 11:59–62
Lin TS (2001) Video-assisted thoracoscopic “resympathicotomy” for palmar hyperhidrosis: analysis of 42 cases. Ann Thorac Surg 72:895–898
Gossot D (1995) Selective endoscopic sympathectomy for palmar hyperhidrosis. Presse Med 24:1739–1742
Gossot D, Toledo L, Fritsch S et al (1997) Thoracoscopic sympathectomy for upper limb hyperhidrosis: looking for the right operation. Ann Thorac Surg 64:975–978
Gossot D, Debrosse D, Grunenwald D (2000) Endoscopic thoracic sympathectomy for isolated axillary hyperhidrosis. Ann Dermatol Venereol 127:1065–1067
Herbst F, Plas EG, Függer R et al (1994) Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limbs. A critical analysis and long-term results of 480 operations. Ann Surg 220:86–90
Zacherl J, Imhof M, Plas EG et al (1997) Hyperhidrosis of the upper extremity: long-term outcome of endoscopic thoracic sympathicotomy. Langenbecks Arch Chir Suppl Kongressbd 114:1287–1289
Zacherl J, Huber ER, Imhof M et al (1998) Long-term results of 630 thoracoscopic sympathicotomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl 580:43–46
Imhof M, Zacherl J, Plas EG et al (1999) Long-term results of 45 thoracoscopic sympathicotomies for primary hyperhidrosis in children. J Pediatr Surg 34:1839–1842
Zacherl J, Imhof M, Huber ER et al (1999) Video assistance reduces complication rate of thoracoscopic sympathicotomy for hyperhidrosis. Ann Thorac Surg 68:1177–1181
Neumayer C, Zacherl J, Holak G et al (2004) Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb. Reduction of compensatory sweating by clipping T4. Surg Endosc 18:152–156
Cohen Z, Shinar D, Levi I et al (1995) Thoracoscopic upper thoracic sympathectomy for palmar hyperhidrosis in children and adolescents. J Pediatr Surg 30:471–473
Cohen Z, Shinhar D, Kurzbart E et al (1997) Laproscopic and thoracoscopic surgery in children and adolescents: a 3-year experience. Pediatr Surg Int 12:356–359
Lee DY, Kim DY, Paik HC (2004) Selective transection of T3 Rami communicantes (T3 ramicotomy) in the treatment of palmar hyperhidrosis. Ann Thorac Surg 78:1052–1055
Han PP, Kenny K, Dickman CA (2002) Thoracoscopic approaches to the thoracic spine: experience with 241 surgical procedures. Neurosurgery 51(Suppl 2):88–95
Noppen M, Vincken W, Dhaese J et al (1996) Thoracoscopic sympathicolysis for essential hyperhidrosis: immediate and one year follow-up results in 35 patients and review of the literature. Acta Clin Belg 51:244–253
Lin C-C (1990) A new method of thoracoscopic sympathectomy in hyperhidrosis palmaris. Surg Endosc 4:224–226
Kim DH, Paik HC, Lee DY (2005) Video assisted thoracoscopic re-sympathetic surgery in the treatment or re-sweating hyperhidrosis. Eur J Cardiothorac Surg 27:741–744
Chen S-C, Lin C-Y, Chou M-C et al (2005) Endoscopic thoracic sympathetic block by clipping for recurrent palmar hyperhidrosis. Int Surg 90:284–288
Singh B, Haffejee AA, Moodley J et al (1996) Endoscopic transthoracoscopic sympathectomy–the Durban experience. S Afr J Surg 34:11–16
Singh B, Shaik AS, Moodley J et al (2002) Limited thoracoscopic ganglionectomy for primary hyperhidrosis. S Afr J Surg 40:50–53
Lee KH, Hwang PYK (1996) Video endoscopic sympathectomy for palmar hyperhidrosis. J Neurosurg 84:484–486
Hehir DJ, Brady MP (1993) Long-term results of limited thoracic sympathectomy for palmar hyperhidrosis. J Pediatr Surg 28:909–911
Yano M, Kiriyama M, Fukai I et al (2005) Endoscopic thoracic sympathectomy for palmar hyperhidrosis: efficacy of T2 and T3 ganglion resection. Surgery 138:40–45
Doolabh N, Horswell S, Williams M et al (2004) Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg 77:410–414
Fukushima H, Makimura S, Takae H et al (2001) Endoscopic thoracic sympathectomy for palmar, axillary and plantar hyperhidrosis: intermediate-term results. Kyobu Geka 54:379–383
Robertson DP, Simpson RK, Rose JE et al (1993) Video-assisted endoscopic thoracic ganglionectomy. J Neurosurg 79:238–240
Little AG (2004) Video-assisted thoracic surgery sympathectomy for hyperhidrosis. Arch Surg 139:586–589
Loscertales J, Arroyo Tristán A, Congregado Loscertales M et al (2004) Thoracoscopic sympathectomy for palmar hyperhidrosis: immediate results and postoperative quality of life. Arch Bronconeumol 40:67–71
Lefaucheur J-P, Fitoussi M, Becquemin J-P (1996) Abolition of sympathetic skin responses following endoscopic sympathectomy. Muscle Nerve 19:581–586
Fischel R, Cooper M, Kramer D (2003) Microinvasive resectional sympathectomy using the harmonic scalpel. Clin Auton Res 13(Suppl 1):I/66–I/70
Lin C-C (1992) Extended thoracoscopic T2-sympathectomy in treatment of hyperhidrosis: experience with 130 consecutive cases. J Laparoendosc Surg 2:1–6
Kopelman D, Hashmonai M, Ehrenreich M et al (1998) Thoracoscopic sympathectomy for hyperhidrosis: is there a learning curve? Surg Laparosc Endosc 8:370–375
Elia S, Guggino G, Mineo D et al (2005) Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 28:312–317
Chou S-H, Lee S-H, Kao E-L (1993) Thoracic endoscopic T2–T3 sympathectomy in palmar hyperhidrosis: experience of 112 cases. Surg Today 23:105–107
de Haan J, Mackaay AJC, Cuesta MA et al (2001) Posterior approach for the simultaneous, bilateral thoracoscopic sympathectomy. J Am Coll Surg 192:418–420
Matthews BD, Bui HT, Harold KL et al (2003) Thoracoscopic sympathectomy for palmaris hyperhidrosis. South Med J 96:254–258
Heuberger J, Furrer M, Habicht J et al (2000) Indications and results of videothorascopic sympathectomy. Dtsch Med Wschr 125:817–821
Alric P, Branchereau P, Berthet J-P et al (2002) Video-assisted thoracoscopic sympathectomy for palmar hyperhidrosis: results in 102 cases. Ann Vasc Surg 16:708–713
Dumont P, Denoyer A, Robin P (2004) Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 78:1801–1807
Gossot D, Kabiri H, Caliandro R et al (2001) Early complications of thoracic endoscopic sympathectomy: a prospective study of 940 procedures. Ann Thorac Surg 71:1116–1119
Nicolas C, Grosdidier G, Granel F et al (2000) Endoscopic sympathectomy for palmar and plantar hyperhidrosis: results in 107 patients. Ann Dermatol Venereol 127:1057–1063
Dumont P, Hamm A, Skrobala D et al (1997) Bilateral thoracoscopy for sympathectomy in the treatment of hyperhidrosis. Eur J Cardiothorac Surg 11:774–775
Chu D, Shi PK, Wu CM (1997) Transthoracic endoscopic sympathectomy for treatment of hyperhidrosis palmaris. Kaohsiung J Med Sci 13:162–168
Chiou TS-M, Chen S-C (1999) Intermediate-term results of endoscopic transaxillary T2 sympathectomy for primary palmar hyperhidrosis. Br J Surg 86:45–47
Chen H-J, Shih D-Y, Fung S-T (1994) Transthoracic endoscopic sympathectomy in the treatment of palmar hyperhidrosis. Arch Surg 129:630–633
Reisfeld R, Nguyen R, Pnini A (2000) Endoscopic thoracic sympathectomy for treatment of essential hyperhidrosis syndrome: experience with 650 patients. Surg Laparosc Endosc Percutan Tech 10:5–10
Yamamoto H, Okada M, Kanehira A et al (1999) Clinical experience with video-assisted thoracic sympathectomy through the restrosternal pulmonary junction. Ann Thorac Surg 68:2361–2363
Yoon DH, Ha Y, Park YG et al (2003) Thoracoscopic limited T3 sympathicotomy for primary hyperhidrosis: prevention for compensatory hyperhidrosis. J Neurosurg 99(Spine 1):39–43
Grabham JA, Raitt D, Barrie WW (1998) Early experience with day-case transthoracic endoscopic sympathectomy. Br J Surg 85:1266
Sayers RD, Jenner RE, Barrie WW (1994) Transthoracic endoscopic sympathectomy for hyperhidrosis and Raynaud’s phenomenon. Eur J Vasc Surg 8:627–631
Adams DCR, Wood SJ, Tulloh BR et al (1992) Endoscopic transthoracic sympathectomy: experience in the south west of England. Eur J Vasc Surg 6:558–562
Cartier B, Cartier P (1999) Thoracoscopic cervicodorsal sympathectomy with diathermy. Ann Vasc Surg 13:582–585
Ng I, Yeo T-T (2003) Palmar hyperhidrosis: intraoperative monitoring with laser Doppler blood flow as a guide for success after endoscopic thoracic sympathectomy. Neurosurgery 52:127–131
Johnson JP, Patel NP (2002) Uniportal and biportal endoscopic thoracic sympathectomy. Neurosurgery 51(Suppl 2):S2/79–S2/83
Moya Amorós J, Prat Ortells J, Morera Abad R et al (2003) Sympathetic dermatomes corresponding to T2 and T3 ganglia. A prospective study of 100 superior thoracic sympathicolytic procedures. Arch Bronconeumol 39:19–22
Chao C, Tsai C-T, Hsiao H-C et al (1993) Transaxillary endoscopic sympathectomy–a report of experience in 150 patients with palmar hyperhidrosis. Surg Laparosc Endosc 3:365–369
Chen H-J, Lu K, Liang C-L (2001) Transthoracic endoscopic T2, 3 sympathectomy for facial hyperhidrosis. Auton Neurosci 93:91–94
Lin C-L, Yen C-P, Howng S-L (1999) The long-term results of upper dorsal sympathetic ganglionectomy and endoscopic thoracic sympathectomy for palmar hyperhidrosis. Surg Today 29:209–213
Fredman B, Zohar E, Shahor D et al (2000) Video-assisted transthoracic sympathectomy in the treatment of primary hyperhidrosis: friend or foe? Surg Laparosc Endosc Percutan Tech 10:226–229
Cohen Z, Levi I, Pinsk I et al (1998) Thoracoscopic upper thoracic sympathectomy for primary palmar hyperhidrosis: the combined paediatric, adolescents and adult experience. Eur J Surg Suppl 580:5–8
Andrews BT, Rennie JA (1997) Predicting changes in the distribution of sweating following thoracoscopic sympathectomy. Br J Surg 84:1702–1704
Drott C, Claes G (1996) Hyperhidrosis treated by thoracoscopic sympathicotomy. Cardiovasc Surg 4:788–790
Kao MC, Chern SH, Cheng LCJ et al (1994) Video thoracoscopic laser sympathectomy for palmar hyperhidrosis. Ann Acad Med Singapore 23:38–42
Kumagai K, Kawase H, Kawanishi M (2005) Health-related quality of life after thoracoscopic sympathectomy for palmar hyperhidrosis. Ann Thorac Surg 80:461–466
de Campos JRM, Wolosker N, Takeda FR et al (2005) The body mass index and level of resection: predictive factors for compensatory sweating after sympathectomy. Clin Auton Res 15:116–120
Wong C-W (1997) Transthoracic video endoscopic electrocautery of sympathetic ganglia for hyperhidrosis palmaris: special reference to localization of the first and second ribs. Surg Neurol 47:224–230
Graham ANJ, Owens WA, McGuigan JA (1996) Assessment of outcome after thoracoscopic sympathectomy for hyperhidrosis in a special unit. J R Coll Surg Edinb 41:160–163
Vanaclocha V, Sáiz-Sapena N, Panta F (2000) Uniportal endoscopic superior thoracic sympathectomy. Neurosurgery 46:924–928
Rajesh YS, Pratap CP, Woodyer AB (2002) Thoracoscopic sympathectomy for palmar hyperhidrosis and Raynaud’s phenomenon of the upper limb and excessive facial blushing: a five year experience. Postgrad Med J 78:682–684
Guijarro Jorge R, Arnau Obrer A, Fernández Centeno A et al (2002) Our experience in the treatment of hyperhidrosis of the upper limbs by video-assisted thoracoscopy: an analysis of our first 100 procedures. Arch Bronconeumol 38:421–426
Sayeed RA, Nyamekye I, Ghauri ASK et al (1998) Quality of life after transthoracic endoscopic sympathectomy for upper limb hyperhidrosis. Eur J Surg Suppl 580:39–42
Al Dohayan A (1999) Transaxillary thoracoscopic sympathectomy experience in a hot climate: management of the dominant hand. Surg Laparosc Endosc Percutan Tech 9:317–321
Byrne J, Walsh TN, Hederman WP (1990) Endoscopic transthoracic electrocautery of the sympathetic chain for palmar and axillary hyperhidrosis. Br J Surg 77:1046–1049
Chiou TSM (2005) Chronological changes of postsympathectomy compensatory hyperhidrosis and recurrent sweating in patients with palmar hyperhidrosis. J Neurosurg Spine 2:151–154
Hsu C-P, Chen C-Y, Lin C-T et al (1994) Video-assisted thoracoscopic T2 sympathectomy for hyperhidrosis palmaris. J Am Coll Surg 179:59–64
Yazbek G, Wolosker N, de Campos JRM et al (2005) Palmar hyperhidrosis–which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg 42:281–285
Fritsch A, Kokoschka R, Mach K (1975) Results of thoracoscopic sympathectomy in hyperhidrosis of the upper extremity. Wien Klin Wochenschr 87:548–550
Atkinson JLD, Fealey RD (2003) Sympathotomy instead of sympathectomy for palmar hyperhidrosis: minimizing postoperative compensatory hyperhidrosis. Mayo Clin Proc 78:167–172
Goh PMY, Cheah W-K, de Costa M et al (2000) Needlescopic thoracic sympathectomy: treatment for palmar hyperhidrosis. Ann Thorac Surg 70:240–242
Fox AD, Hands L, Collin J (1999) The results of thoracoscopic sympathetic trunk transection for palmar hyperhidrosis and sympathetic ganglionectomy for axillary hyperhidrosis. Eur J Vasc Endovasc Surg 17:343–346
Hsia J-Y, Chen C-Y, Hsu C-P et al (1999) Outpatient thoracoscopic limited sympathectomy for hyperhidrosis palmaris. Ann Thorac Surg 67:258–259
Yoon S-H, Rim D-C (2003) The selective T3 sympathicotomy in patients with essential palmar hyperhidrosis. Acta Neurochir 145:467–471
Leão LEV, de Oliveira R, Szulc R et al (2003) Role of video-assisted thoracoscopic sympathectomy in the treatment of primary hyperhidrosis. Sao Paulo Med J 121:191–197
Han PP, Gottfried ON, Kenny KJ et al (2002) Bipolar thoracoscopic sympathectomy: surgical techniques and clinical results for the treatment of hyperhidrosis. Neurosurgery 50:306–312
Baumgartner FJ, Toh Y (2003) Severe hyperhidrosis: clinical features and current thoracoscopic surgical management. Ann Thorac Surg 76:1878–1883
Licht PB, Pilegaard HK (2004) Severity of compensatory sweating after thoracoscopic sympathectomy. Ann Thorac Surg 78:427–431
Young O, Neary P, Keaveny TV et al (2003) Evaluation of the impact of transthoracic endoscopic sympathectomy on patients with palmar hyperhidrosis. Eur J Vasc Endovasc Surg 26:673–676
Yamamoto H, Kanehira A, Kawamura M et al (2000) Needlescopic surgery for palmar hyperhidrosis. J Thorac Cardiovasc Surg 120:276–279
Erak S, Sieunarine K, Goodman M et al (1999) Endoscopic thoracic sympathectomy for primary palmar hyperhidrosis: intermediate term results. Aust N Z J Surg 69:60–64
Kim B-Y, Oh B-S, Park Y-K et al (2001) Microinvasive video-assisted thoracoscopic sympathicotomy for primary palmar hyperhidrosis. Am J Surg 181:540–542
Neumayer C, Bischof G, Függer R et al (2001) Efficacy and safety of thoracoscopic sympathicotomy for hyperhidrosis of the upper limb. Ann Chir Gynaecol 90:195–199
Noppen M, Herregodts P, D’Haese J et al (1996) A simplified T2–T3 thoracoscopic sympathicolysis technique for the treatment of essential hyperhidrosis: short-term results in 100 patients. J Laparoendosc Surg 6:151–159
Lin T-S, Kuo S-J, Chou M-C (2002) Uniportal endoscopic thoracic sympathectomy for treatment of palmar and axillary hyperhidrosis: analysis of 2000 cases. Neurosurgery 51(Suppl 2):S2/84–S2/87
van’t Riet M, de Smet AAEA, Kuiken H et al (2001) Prevention of compensatory hyperhidrosis after thoracoscopic sympathectomy for hyperhidrosis. Surg Endosc 15:1159–1162
Lardinois D, Ris HB (2002) Minimally invasive video-endoscopic sympathectomy by use of a transaxillary single port approach. Eur J Cardiothorac Surg 21:67–70
Duarte JBV, Kux P (1998) Improvements in video-endoscopic sympathicotomy for the treatment of palmar, axillary, facial, and palmar-plantar hyperhidrosis. Eur J Surg Suppl 580:9–11
Lee DY, Paik HC, Kim DH et al (2003) Comparative analysis of T3 selective transection of rami communicantes (ramicotomy) to T3 sympathetic clipping in treatment of palmar hyperhidrosis. Clin Auton Res 13(Suppl 1):I/45–I/47
Cheng Y-J, Wu H-H, Kao E-L (2001) Video-assisted thoracoscopic sympathetic ramicotomy for hyperhidrosis: a way to reduce the complications. Ann Chir Gynaecol 90:172–174
Kux M (1978) Thoracic endoscopic sympathectomy in palmar and axillary hyperhidrosis. Arch Surg 113:264–266
Lin T-S, Huang L-C, Wang N-P et al (2001) Endoscopic thoracic sympathetic block by clipping for palmar and axillary hyperhidrosis in children and adolescents. Pediatr Surg Int 17:535–537
Choi BC, Lee YC, Sim SB (2003) Treatment of palmar hyperhidrosis by endoscopic clipping of the upper part of the T4 sympathetic ganglion. Preliminary results. Clin Auton Res 13(Suppl 1):I/48–I/51
Neumayer C, Panhofer P, Zacherl J et al (2005) Effect of endoscopic sympathetic block on plantar hyperhidrosis. Arch Surg 140:676–680
Shachor D, Jedeikin R, Olsfanger D et al (1994) Endoscopic transthoracic sympathectomy in the treatment of primary hyperhidrosis. A review of 290 sympathectomies. Arch Surg 129:241–244
Lin T-S, Chou M-C (2004) Treatment of palmar hyperhidrosis using needlescopic T2 sympathetic block by clipping: analysis of 102 cases. Int Surg 89:198–201
Schick CH, Fronek K, Held A et al (2003) Differential effects of surgical sympathetic block on sudomotor and vasoconstrictor function. Neurology 60:1770–1776
Ramsaroop L, Singh B, Moodley J et al (2004) Anatomical basis for a successful upper limb sympathectomy in the thoracoscopic era. Clin Anat 17:294–299
Singh B, Ramsaroop L, Partab P et al (2005) Anatomical variations of the second thoracic ganglion. Surg Radiol Anat 27:119–122
Chung I-H, Oh C-S, Koh K-S et al (2002) Anatomic variations of the T2 nerve root (including the nerve of Kuntz) and their implications for sympathectomy. J Thorac Cardiovasc Surg 123:498–501
Wang Y-C, Sun M-H, Lin C-W et al (2002) Anatomical location of T2-3 sympathetic trunk and Kuntz nerve determined by transthoracic endoscopy. J Neurosurg (Spine 1) 96:68–72
Cho HM, Lee DY, Sung SW (2005) Anatomical variations of rami communicantes in the upper thoracic sympathetic trunk. Eur J Cardiothorac Surg 27:320–324
Ramsaroop L, Partab P, Singh B et al (2001) Thoracic origin of a sympathetic supply to the upper limb: the “nerve of Kuntz” revisited. J Anat 199:675–682
Satyapal KS, Singh B, Partab P et al (2003) Thoracoscopy: a new era for surgical anatomy. Clin Anat 16:538–541
Hashmonai M, Kopelman D (2006) The level of ganglion clipping for hyperhidrosis. Clin Auton Res 16:407
Singh B, Moodley J, Allopi L et al (2006) Horner syndrome after sympathectomy in the thoracoscopic era. Surg Laparosc Endosc Percutan Tech 16:222–225
Lange JF (1995) Inferior brachial plexus injury during thoracoscopic sympathectomy. Surg Endosc 9:830
Hashmonai M, Assalia A, Kopelman D (2001) Thoracoscopic sympathectomy for palmar hyperhidrosis. Ablate or resect? Surg Endosc 15:435–441
Chang Y-T, Li H-P, Lee J-Y et al (2007) Treatment of palmar hyperhidrosis. T4 level compared with T3 and T2. Ann Surg 246:330–336
Goetz RH, Marr JAS (1944) The importance of the second thoracic ganglion for the sympathetic supply of the upper extremities–two new approaches for its removal. Clin Proc 3:102–114
Lin CC, Telaranta T (2001) Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol 90:161–166
Hsu C-P, Chen C-Y, Hsia J-Y et al (1998) Resympathectomy for palmar and axillary hyperhidrosis. Br J Surg 85:1504–1505
Hashmonai M, Kopelman D, Klein O et al (1992) Upper thoracic sympathectomy for primary palmar hyperhidrosis: long-term follow-up. Br J Surg 79:268–271
Acknowledgment
The authors thank Mrs. T. Mashiach, MS, for her laborious statistical guidance and evaluation of data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kopelman, D., Hashmonai, M. The Correlation Between the Method of Sympathetic Ablation for Palmar Hyperhidrosis and the Occurrence of Compensatory Hyperhidrosis: A Review. World J Surg 32, 2343–2356 (2008). https://doi.org/10.1007/s00268-008-9716-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9716-4