Abstract
Atherosclerosis is the underlying cause of most heart attacks and strokes. It is thereby the leading cause of death in the Western world, and it places a significant financial burden on health care systems. There is evidence that complex, multi-scale arterial mass transport processes play a key role in the development of atherosclerosis. Such processes can be controlled both by blood flow patterns and by properties of the arterial wall. This short review focuses on one vascular-scale, flow-regulated arterial mass transport process, namely concentration polarization of low density lipoprotein at the luminal surface of the arterial endothelium, and on one cellular-scale, structural determinant of arterial wall mass transport, namely the endothelial glycocalyx layer. Both have attracted significant attention in recent years. In addition to reviewing and appraising relevant literature, we propose various directions for future work.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
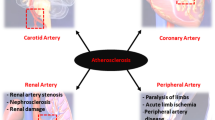
1.1 Atherosclerosis
Atherosclerosis is characterized by the formation of lipid-rich lesions within the walls of large- and medium-sized systemic arteries. The disease is associated with many risk factors, the main ones including:
-
High plasma concentrations of low density lipoprotein (LDL)
-
Low plasma concentrations of high density lipoprotein (HDL)
-
High blood pressure
-
Diabetes
-
Smoking
-
Gender (being male)
-
Genetic predisposition
-
Stress
-
Lack of exercise
-
Age
The processes thought to trigger development of early atherosclerotic lesions can be summarized as follows (Schwartz et al. 1993; Berliner et al. 1995):
-
Low density lipoprotein, which is the primary transporter of cholesterol within the blood, traverses the endothelium and accumulates in the intima of the arterial wall. Some of this LDL becomes modified (oxidized, for example), triggering the recruitment of monocytes into the wall
-
The monocytes differentiate into macrophages which further modify and ingest the accumulated LDL, creating lipid-rich foam cells, so-called because the fat droplets within them lead to a foamy appearance under the microscope
-
High density lipoprotein that enters the arterial wall can remove accumulated lipids from foam cells
-
If lipid influx into the arterial wall is consistently greater than lipid efflux, then the number of foam cells will continue to increase
-
Accumulation of lipid-rich foam cells leads to the development of early-stage atherosclerotic lesions known as fatty streaks
After a prolonged period of growth (also involving other processes such as smooth muscle cell proliferation, the deposition of fibrous proteins, remodeling, and complex inflammatory responses), such lesions may cause a significant stenosis, reducing blood flow rates and leading to ischemic symptoms (such as angina, when coronary artery stenoses restrict blood flow to the heart).
Atherosclerotic lesions, particularly those with a lipid-rich core and a thin fibrous cap, may also become unstable and prone to rupture. When a rupture occurs, blood comes into contact with thrombogenic material from the lesion or wall, and a clot will form. Clots may cause sudden and complete arterial occlusion at the site of rupture or may embolize and block vessels further downstream. Two well-known consequences of such occlusion are heart attacks (caused by occlusion of a coronary artery) and strokes (caused by occlusion of an artery that supplies the brain).
Atherosclerosis is prevalent in Western societies and has an increasing incidence in developing countries. According to the World Health Organization (WHO), cardiovascular disease, and in particular atherosclerosis, is now the leading cause of death globally each year (Mackay and Mensah 2004). Furthermore, the WHO predict that atherosclerosis will become the single most burdensome disease on the health systems of the world by 2020 (Faergeman 2003).
A notable feature of atherosclerosis is its propensity to develop non-uniformly in the vasculature, with variations most conspicuous in regions of arterial branching and high curvature. Since such regions are associated with complex blood flow patterns, it has been postulated that blood flow may play an important role in regulating atherogenesis (Woolf 1990; Hahn and Schwartz 2009). Indeed, correlations between blood flow patterns and sites of arterial disease have been suggested for over a century. One of the earliest proponents was Rindfleisch, who stated in 1872 that atherosclerotic lesions form in locations ‘exposed to the full stress and impact of the blood’ (Rindfleisch 1872).
Subsequently, a variety of mechanisms to explain correlations between flow and disease have been proposed. One view propounded during the 1960s was that flow-induced wall damage rendered particular regions of the vasculature more permeable to atherogenic species such as LDL and thus more susceptible to atherosclerosis (Scharfstein et al. 1963); this led to the supposition that regions exposed to high levels of hemodynamic wall shear stress were predisposed to developing atherosclerosis (Fry 1968). In the late 1960s and early 1970s, however, two papers by Caro et al. (1969, 1971) suggested that regions of arterial disease collocated with areas exposed to low levels of wall shear stress. Caro et al. also proposed a mechanism by which such colocation could occur. This mechanism relied on the shear-modulated efflux of species from the arterial wall into the lumen.
The low shear hypothesis of Caro et al. became widely accepted and remains so today (although the original mechanism proposed by Caro et al. to cause such collocation is now considered unfeasible). In recent decades, however, it has become increasingly evident that a direct correlation between disease patterns and wall shear stress magnitude alone may be too simplistic. A range of more complex relationships have been suggested, with a tentative consensus now developing that a combination of low and temporally oscillating wall shear stress predisposes regions of arteries to disease (Ku et al. 1985; Shaaban and Duerinckx 2000; Cheng et al. 2004).
1.2 Atherosclerosis and arterial mass transport
There is evidence that complex, multi-scale arterial mass transport processes involving various species play a key role in the development of atherosclerosis and its regulation by blood flow (see Table 1 for an overview of the scales involved). Important species include LDL, HDL, oxygen (O\(_2\)), nitric oxide (NO), adenosine triphosphate (ATP), and adenosine diphosphate (ADP).
Of these species, LDL has attracted the greatest attention since, as noted above, it is thought to be the primary source of lipid in atherosclerotic lesions. Alternative theories—that lipid in lesions is synthesized by the arterial wall or that it derives from the membranes of red blood cells—do not explain why the concentration of LDL in plasma correlates strongly with the risk of developing coronary heart disease or cerebrovascular disease (both of which are caused by atherosclerotic lesions). Nor do they explain why lowering plasma LDL concentration with statins reduces the incidence of atherosclerosis, or why lipid-rich lesions resembling atherosclerosis develop in animals after raising their plasma LDL concentrations by dietary or genetic means.
The other species listed above have been studied in less detail. However, they are also likely to play important roles. HDL is thought to be responsible for transport of lipids out of atherosclerotic lesions. This view is consistent with observations that plasma concentrations of HDL are inversely associated with the incidence of atherosclerosis (Rader 2003) and that over-expression of HDL in transgenic animals reduces the prevalence of experimental atherosclerosis (Valenta et al. 2006). The importance of O\(_2\) transport from the lumen to the arterial wall is implied by the suggestion that hypoxic conditions in the arterial wall trigger atherosclerosis (Adams 1973; Jellinek 1983) and by the fact that the arterial media is a particularly avascular tissue [up to 29 lamellae can develop before it is penetrated by vasa vasorum from the adventitia (Wolinsky and Glagov 1967)]. NO is a signaling molecule that has multiple putatively atheroprotective effects, including suppression of inflammation, reduction of LDL oxidation, and prevention of platelet aggregation and monocyte infiltration; a deficiency in the NO pathway is a strong risk factor for coronary heart disease (Napoli et al. 2006). ATP and ADP are implicated in the development of atherosclerosis through their influence on calcium concentrations within, and NO production by, endothelial cells (John and Barakat 2001; Choi et al. 2007; Choi and Barakat 2009).
A review of arterial mass transport in general (with a particular focus on its relation to localization of atherosclerosis) is given by Tarbell (2003), and a review of computational modeling techniques applied to arterial mass transport is given by Ethier (2002). The objective of this paper is to review one particular vascular-scale, flow-regulated mass transport process, namely the formation of an LDL concentration polarization layer at the luminal surface of the arterial wall, as well as one particular cellular-scale determinant of arterial wall mass transport properties, namely the endothelial glycocalyx layer (EGL). The formation of an LDL concentration polarization layer and effects of the EGL on transport are both likely to play a key role in atherogenesis.
2 Flow-dependent concentration polarization of low density lipoprotein in arteries
2.1 Overview
Consider fluid containing a dissolved solute flowing through a membrane. If the membrane offers a higher resistance to the solute than to the fluid, then solute will be rejected by the membrane and accumulate on its upstream surface. The elevation of solute concentration above that in the bulk flow causes solute to diffuse back away from the membrane. A steady-state solute distribution is reached when solute convection toward the membrane balances solute diffusion away from the membrane and solute transport across it. At this steady state, the solute concentration near the membrane remains higher than in the bulk solution. It is this solute accumulation which is termed concentration polarization and the layer of rejected solute a concentration polarization layer (see Fig. 1).
Diagram illustrating how concentration polarization of a dissolved solute can occur adjacent to a membrane from which the solute is fully or partially rejected. A steady state is reached when convection toward the membrane (solid arrow) balances diffusion away from the membrane (checkered arrow) and transport across the membrane (striped arrow)
The phenomenon of concentration polarization is well known within various fields of science and engineering, in particular those involving filtration processes. LDL concentration polarization is thought to occur in arteries because of an imbalance between the measured velocity of the water that flows radially outwards from the lumen, through the arterial wall [\(\sim 4\times 10^{-2}\,\upmu \,\,\mathrm{ms}^{-1}\) (Tedgui and Lever 1984)], and the measured mass transport coefficient for LDL through the endothelium [\(\sim 2\times 10^{-4}\,\upmu \,\,\mathrm{ms}^{-1}\) (Bratzler et al. 1977)]. Because convection of LDL toward the luminal surface of the endothelium is far greater than the rate of transendothelial LDL transport, an LDL-rich concentration polarization layer will form adjacent to the endothelial surface.
Consider the formation of an LDL concentration polarization layer near an arbitrary point of interest adjacent to the luminal surface of the arterial endothelium. Further, consider defining a wall normal coordinate \(y\) at this point of interest (see Fig. 2), where \(y=0\) coincides with the luminal surface of the arterial endothelium. As already noted, LDL transport through the endothelium is two orders of magnitude slower than the transmural water flux which draws LDL from the lumen toward the endothelial surface. Consequently, when modeling LDL transport above the endothelium, one can assume LDL is completely rejected at \(y=0\). Hence, in steady state, lumen side convection and diffusion must balance at \(y=0\). If in addition one assumes that the concentration polarization layer can be modeled locally as a stagnant film (Zeman and Zydney 1996; Zydney 1997), then convection and diffusion must balance along the entire \(y\) coordinate within the concentration polarization layer. Hence, the \(y\)-dependent LDL distribution \(C=C(y)\) within the concentration polarization layer at the point of interest is a solution of
where \(D_L\) is the diffusivity of LDL in the lumen and \(V\) is the magnitude of the transmural flux velocity (assumed to be in the negative \(y\) direction, toward the endothelial surface).
A single boundary condition is required to solve Eq. (2.1). To obtain such a condition, it is assumed that the concentration polarization layer has a finite thickness \(\zeta \) near the point of interest (see Fig. 2). If LDL concentration in the bulk flow is denoted \(C_B\), then the above assumption requires that
Solving Eq. (2.1) subject to the boundary condition defined by Eq. (2.2) results in the following expression for \(C\) within the concentration polarization layer (i.e. within the region \(0<y<\zeta \)) at the point of interest
where
is the resulting LDL concentration adjacent the luminal surface of the endothelium at the point of interest.
It is clear that \(C_E\ge C_B\)—that is concentration polarization occurs and LDL concentration adjacent to the luminal surface of the endothelium is enhanced relative to LDL concentration in the bulk flow. It is also clear that \(C_E\) will depend on both the thickness \(\zeta \) of the concentration polarization layer and the magnitude \(V\) of the transmural flux velocity. \(\zeta \) will depend on the extent to which the concentration polarization layer has been able to evolve in the wall-parallel direction, which will in turn depend on the local blood flow patterns and in particular the local wall shear stress. \(V\) will depend in part on the hydraulic permeability of the endothelium, which has been shown to depend on the magnitude (Tarbell 2010) and/or direction (Adamson et al. 2013) of the local wall shear stress via a mechanochemical transduction mechanism. Blood flow patterns, and in particular wall shear stress, are therefore likely to play an important role in determining the degree of LDL concentration polarization and hence the degree of endothelial exposure to LDL.
Note that such flow-dependent exposure of the endothelium to LDL is not predicted by Tarbell (2003) or Tarbell and Qiu (2000), who characterize LDL transport from the lumen to the arterial wall as ‘wall-limited’, independent of blood flow patterns; a detailed explanation of this discrepancy is given by Vincent (2009).
2.2 Experimental studies
Deng et al. (1995) studied transport of labeled cholesterol in perfused, excised canine carotid arteries. They found that increased perfusion pressures led to increased transmural flux velocities and increased uptake of labeled cholesterol by the arterial wall. This increase in uptake was attributed to an increase in cholesterol concentration polarization adjacent to the luminal surface of the endothelium. However, no direct measurements of cholesterol concentration near the luminal surface of the endothelium were made, so the results must be interpreted carefully; several other interpretations are possible.
Wang et al. (2003) directly measured the concentration polarization of albumin in perfused, excised canine carotid arteries using a micro-syringe and sampling needle. As the transmural water flux velocity was increased, and as the wall shear rate was decreased, the degree of concentration polarization increased. Under certain conditions, albumin concentration at the luminal surface of the endothelium was found to be 65 % greater than albumin concentration in the bulk flow. Subsequently, Zhang et al. (2007) used similar techniques to measure concentration polarization of albumin downstream of artificial stenoses formed in perfused, excised canine carotid arteries. The presumably disturbed and recirculating flow downstream of the stenoses increased the concentration polarization relative to that seen in the regions of undisturbed flow. Under certain conditions, albumin concentration at the luminal surface of the endothelium downstream of a stenosis was found to be 77 % greater than in the bulk flow, whereas away from the stenosis, the surface concentration of albumin was 52 % greater than in the bulk flow. In both studies (Wang et al. 2003; Zhang et al. 2007), the degree of concentration polarization was significantly greater than expected for a small macromolecule like albumin, particularly considering the 280 \(\upmu \)m diameter of even the smallest sampling needle (and hence the relatively thick layer of perfusate that will have been sampled). It is telling that the experimental results of Wang et al. (2003) were matched by accompanying theoretical models that used an albumin diffusivity of 8.7 \(\upmu \mathrm{m}^{2}\,\mathrm{s}^{-1}\), which is approximately three times smaller than the measured diffusivity of albumin under similar conditions (Wakeman et al. 1976). We speculate that the sampling needle, which was placed in contact with the wall, damaged the endothelium, leading to a locally enhanced transmural water flux and, hence, a locally enhanced near-wall albumin concentration. Nevertheless, the experimental concept is ingenious and worthy of further development.
Ding et al. (2009) measured LDL concentration polarization above co-cultured endothelial and smooth muscle cells exposed to uniform flow in a parallel plate flow chamber. As concentration polarization increased, so too did the rate of LDL uptake by the cells. In the same year, Meng et al. (2009) cultured endothelial cells on the inner surface of a semi-permeable, anatomically realistic, plastic model of a carotid artery bifurcation. The cultured endothelium was presumed to be exposed to physiologically realistic flow patterns (induced by the geometry itself), and concentration polarization of HDL was measured at the endothelial surface. At certain locations, and under certain conditions, HDL concentration at the endothelial surface was measured to be 46 % greater than in the bulk flow. These results are intriguing. However, they should be interpreted carefully; not only because they employed the syringe/needle microaspiration technique discussed above, but also because transport properties of cultured endothelium currently do not replicate transport properties of normal intact endothelium in vivo. Specifically, much evidence suggests that the hydraulic permeability of cultured endothelium is \(\sim \)10 times greater than that of endothelium in vivo (Suttorp et al. 1988; Luckett et al. 1989; Turner 1992) [although in some studies the discrepancies are smaller (Dull et al. 1991; Chang et al. 2000)]. Also, the permeability of cultured endothelium to macromolecules is typically \(\sim \)10–100 times greater in vitro than in vivo (Albelda et al. 1988). Such discrepancies in the permeability to water and macromolecules may have a significant impact on the degree of concentration polarization above cultured endothelial cells relative to the situation in vivo.
More recently, Wei et al. (2012) used confocal microscopy to assess concentration polarization of labeled LDL in perfused, excised rabbit common carotid arteries with an artificial stenosis. Measurements were made possible by dehydrating the vessel and treating it with methyl salicylate to render it transparent. As in previous studies, significant concentration polarization was observed distal to the stenosis. Specifically, under certain conditions, the concentration of labeled LDL at the luminal surface of the endothelium downstream of the stenosis was found to be 47 % greater than in the bulk flow. This study avoids issues with the syringe/needle microaspiration technique and the permeability of cultured endothelium. However, the endothelium is a fragile organ, and it is inconceivable that its transport properties would not be drastically affected by the techniques required to make it transparent. Consequently, once again, results of the study should be interpreted carefully.
2.3 Theoretical studies
Fatouraee et al. (1998) undertook time-dependent (pulsatile) simulations of LDL concentration polarization in straight arteries (essentially straight cylindrical pipes). They predicted a 4–15 % time-averaged increase in LDL concentration adjacent to the endothelium, relative to LDL concentration in the bulk flow. Both increasing the transmural flux velocity and decreasing the wall shear rate increased the degree of concentration polarization. In the following year, Wada and Karino (1999) undertook similar steady-state studies and obtained similar results.
As a follow-up to these studies in simple straight pipes, Wada and Karino (2002) undertook steady-state simulations of LDL concentration polarization in an idealized arterial geometry with multiple bends. Flow-dependent LDL concentration polarization occurred at the luminal surface of the endothelium. It was greatest downstream of the inner curvature of each bend, in regions associated with re-circulating flow and low wall shear stress. More specifically, under physiologically realistic conditions, LDL concentration in these regions was up to 31.5 % greater than in the bulk flow. It was also found that increasing the transmural flux velocity and decreasing LDL diffusivity acted to increase the degree of concentration polarization. Also, Wada et al. (2002) conducted steady-state simulations of LDL concentration polarization in the vicinity of a small stenosis. Concentration polarization was enhanced downstream of the stenosis, again in regions associated with re-circulating flow, and low wall shear stress. Under physiologically realistic conditions, LDL concentration at the wall in these regions was up to 20 % greater than in the bulk flow.
More recently, Liu et al. (2009) performed steady-state simulations of LDL concentration polarization in the human aortic arch and descending thoracic aorta. Their results suggested that helical swirling flow in the ascending aorta and aortic arch suppressed LDL concentration polarization in these regions. Also, Lantz and Karlsson (2012) performed time-dependent simulations of LDL concentration polarization in the human aortic arch and descending thoracic aorta. The velocity field for their study was obtained using a Large Eddy Simulation approach, with patient-specific inflow boundary conditions. They found high levels of LDL concentration polarization were associated with regions of low wall shear stress.
Taken together, results from the vascular-scale studies detailed above suggest the degree of LDL concentration polarization depends upon the transmural water flux velocity, the diffusivity of LDL in blood, and local blood flow patterns (in particular the local wall shear stress). Specifically, increasing the transmural water flux velocity, lowering LDL diffusivity, and decreasing the local wall shear stress all appear to increase the degree of LDL concentration polarization. Such findings are in line with the simple 1D analysis presented in Sect. 2.1.
Various authors have also undertaken cellular-scale simulations of LDL concentration polarization in arteries. Studies include those of Wada and Karino (2002) and Vincent et al. (2009), both of which investigated the effect of a spatially heterogeneous transmural water flux, channeled through intercellular clefts only. Also, Vincent et al. (2010) and Liu et al. (2011) recently investigated the affect of the EGL on LDL concentration polarization. These latter studies are discussed further in Sect. 3.3.2.
2.4 Implications for atherosclerosis
The experimental and theoretical studies cited above suggest that a substantial LDL concentration polarization layer forms within arteries; the studies also suggest that LDL concentration polarization will be greatest in regions of re-circulating flow, characterized by low wall shear stress. Furthermore, the recent study of Ding et al. (2009) suggests that the degree of LDL concentration polarization determines the rate of transendothelial LDL transport and hence the likelihood of atherosclerosis occurring. Consequently, existence of flow-dependent LDL concentration polarization provides a plausible explanation for the observed flow-dependent, spatially non-uniform onset of atherosclerosis. However, further studies are required to ascertain whether this mechanism plays a significant role in practice.
2.5 Future studies
2.5.1 Future experimental studies
Future experimental studies should aim to refine the ingenious micro-syringe measurement technique pioneered by Wang et al. (2003). Nanotechnology has advanced dramatically since 2003, and it may now be feasible to sample a thinner layer of perfusate while avoiding contact with the endothelial surface. The confocal microscopy techniques recently employed by Wei et al. (2012) should also be developed further. We suggest that thin-walled vessels should be used in conjunction with two-photon confocal microscopy (which allows greater penetration than conventional confocal methods). This might allow measurement of the concentration of labeled LDL in near-wall perfusate from outside the vessel, without the need for chemical treatments to make the wall transparent.
2.5.2 Future theoretical studies
Low density lipoprotein concentration polarization layers are likely to be of order 10–100 \(\upmu \)m thick. Consequently, cellular-scale properties of blood and the vessel wall may affect their formation. Theoretical studies have already investigated the effects of a spatially heterogeneous transmural water flux, channeled through intercellular clefts only (Wada and Karino 2002; Vincent et al. 2009), and of the EGL (Vincent et al. 2010; Liu et al. 2011) on LDL concentration polarization. Future studies should continue in this direction. In particular, they should ascertain whether the discrete nature of red blood cells and the existence of a cell-free layer adjacent to the endothelium have an impact on LDL concentration polarization.
3 Mass transport in the endothelial glycocalyx layer
3.1 Overview
Attached to the luminal surface of vascular endothelial cells, and likely covering (and entering) the intercellular clefts, is a negatively charged structure known as the endothelial glycocalyx layer (EGL). Details of its structure and function have been reviewed by Pries et al. (2000), Weinbaum et al. (2003), Tarbell et al. (2005), Weinbaum et al. (2007), Reitsma et al. (2007), Van Teeffelen et al. (2007), and, most recently, Curry and Adamson (2012). Only a brief overview is given here.
The EGL is currently understood to be formed of two distinct yet closely interacting regions (Weinbaum et al. 2007; Reitsma et al. 2007). The first region is composed of long-chain macromolecules (predominantly proteoglycans and glycoproteins) firmly attached to the luminal surface of the underlying cells. This region of the EGL is often observed in ex-vivo electron microscope studies (see Fig. 3) and extends \(\sim \)0.05–0.4 \(\upmu \)m (van den Berg et al. 2006) from the endothelial surface. The second region, likely intertwined with the first, is thought to be more dynamic in nature; it is composed of hyaluronan and loosely attached plasma- and endothelium-derived proteins which extend the EGL \(\sim \)0.3–0.5 \(\upmu \)m (Vink and Duling 1996; Smith et al. 2003; Damiano et al. 2004) [or possibly further (van Haaren et al. 2003; Megens et al. 2007)] into the lumen. Indeed, recent experiments by Ebong et al. (2011) have suggested that the entire EGL extends up to \(11\,\upmu \)m into the lumen. There is evidence to suggest that the composition and thickness of the EGL depend on local hemodynamic forces such as wall shear stress (van den Berg et al. 2006; Lipowsky and Lescanic 2013; Koo et al. 2013).
An electron micrograph of the firmly attached basal region of the EGL within a rat ventricular myocardial capillary (Berg et al. 2003). Reused with permission from H. Vink. Copyright 2003, Wolters Kluwer Health
The EGL is postulated to play an important role in several processes, including the prevention of interactions between red blood cells and the endothelium (Secomb et al. 2001) and the transmission of hemodynamic forces to the surface of endothelial cells (Weinbaum et al. 2003). However, it is the role of the EGL as a complex macromolecular filter and its consequent effects on vascular mass transport (and hence atherosclerosis) that will be the focus of the following discussion.
3.2 Experimental studies
3.2.1 Early evidence that plasma proteins interact with the endothelial glycocalyx layer
During the 1970s, a number of experimental studies suggested that albumin interacts with the endothelial surface of capillary walls, reducing their hydraulic conductivity (Levick and Michel 1973; Mason et al. 1977). Several mechanisms for this phenomenon were proposed, including blockage of ‘endothelial pores’ by albumin. In 1980, Michel proposed that the reduction in hydraulic conductivity could be attributed to an interaction of albumin with a fiber matrix layer on the endothelial surface (the EGL). In the same year, Curry and Michel (1980) presented a theoretical model of such interaction. Subsequent experimental studies throughout the 1980s and early 1990s added weight to the suggestion that plasma proteins interact with the EGL, reducing overall capillary permeability. Turner et al. (1983) demonstrated that cationized ferritin can penetrate into the EGL of frog mesenteric capillaries (see Fig. 4), reducing hydraulic conductivity, and Michel et al. (1985) showed that the hydraulic conductivity of frog mesenteric capillaries was reduced threefold when they were perfused with bovine serum albumin. Furthermore, Schnitzer et al. (1988) demonstrated that albumin interacts with a 60 kDa glycoprotein component [and possibly other components (Schnitzer et al. 1988)] of the EGL of cultured endothelial cells derived from the rat epididymal fat pad. Finally, Adamson and Clough (1992) used cationized ferritin to mark the EGL of frog mesenteric capillaries and subsequently demonstrated that albumin and other plasma proteins interact with and modify mass transport properties of the EGL. Hence, by the early 1990s, significant experimental evidence suggested that plasma proteins such as albumin interact with the EGL of capillaries and reduce their permeability. Additionally, Gorog and Born (1982) showed that removal of sialic acid (now understood to be a component of the EGL) from the endothelial surface of rabbit carotid arteries (not capillaries) resulted in increased uptake of LDL and fibrinogen by the arterial wall. Taken together, these studies constituted the first direct evidence that the EGL has a significant effect on mass transfer within the vasculature.
An electron micrograph of endothelial cells in a frog mesenteric capillary that has been perfused with cationized ferritin. The lumen is in the top left corner of the image. Cationized ferritin is clearly visible within the remaining components of the EGL, which coat the luminal surface of the endothelial cells. An intercellular cleft (between two adjacent endothelial cells) is visible near the center of the image. The bar represents 200 nm (Turner et al. 1983). Reused with permission from C. Michel. Copyright 1983, Elsevier
3.2.2 Determining mass transport properties with fluorescently labeled tracers
Vink and Duling (1996) used intra-vital microscopy to study the transport of fluorescein isothiocyanate (FITC)-labeled dextran 70 (negatively charged), and texas red (TR)-labeled dextran 70 (neutral) within hamster cremaster muscle capillaries. It was found that both FITC- and TR-labeled dextran 70 were excluded from a region adjacent to the endothelial surface. This region was deemed to be the EGL. A number of experimental studies followed, in which mass transport properties of the EGL were probed using fluorescently labeled tracers (such as FITC-labeled dextrans). Henry and Duling (1999) used intra-vital microscopy to study the interaction of FITC-labeled dextran 70, 145, 580, and 2000 with the EGL in hamster cremaster muscle microvessels. In line with the results of Vink and Duling (1996), all FITC-labeled dextrans were found to be excluded from the EGL. However, after degradation of hyaluronan within the EGL (by exposure to hyaluronidase), FITC-labeled dextran 70 and 145 were able to penetrate significantly. These results suggest that hyaluronan plays a critical role in determining mass transport properties of the EGL. Vink and Duling (2000) studied how FITC-labeled dextran 4, 17, 39, 70, 580, and 2000 (negative), TR-labeled dextran 40 and 70 (neutral), free rhodamine dye (neutral), dichlorotriazinylaminofluorescein (DTAF)-labeled bovine serum albumin (67 kDa), DTAF-labeled fibrinogen (340 kDa), and a FITC-labeled complex of albumin and dextran 70 interacted with the EGL of hamster cremaster muscle capillaries. TR-labeled dextran 40 and free rhodamine dye were able to penetrate into the EGL with half-times of 11–60 min, depending on tracer size. Also, in line with previous studies, it was found that both FITC- and TR-labeled dextran 70 were excluded from EGL. However DTAF-labeled albumin and fibrinogen (67 and 340 kDa, respectively), which are larger than FITC- and TR-labeled dextran 70, were able to penetrate into the EGL, with a half-time of 40 min, and the FITC-labeled complex of albumin and dextran 70 was also able to penetrate. Collectively, these results suggested that the EGL does not simply behave as a size-selective filter. Instead, they demonstrated that mass transport properties of a given species within the EGL depend on its charge and structure, as well as its size. Also Henry and Duling (2000), showed that application of Tumor Necrosis Factor-\(\alpha \) (TNF-\(\alpha \)) enabled FITC-labeled dextran 70 and dextran 580 to penetrate into the EGL and significantly increased the rate at which FITC-labeled dextran 40, FITC-labeled albumin, and FITC-labeled immunoglobulin G could penetrate. These results highlight how mass transport properties of the EGL will likely depend on the in vivo biological state of the endothelium and in particular on local inflammatory processes. Subsequently, van Haaren et al. (2003) used confocal microscopy to study the interaction of FITC-labeled dextran 4.4, 50.7, and 148 with the EGL of rat mesenteric microvessels. They found that FITC-labeled dextran 148 was excluded from the EGL, FITC-labeled dextran 50.7 penetrated slowly, and FITC-labeled dextran 4.4 penetrated very quickly. These results suggest that if the type of molecule and the biological state of the endothelium is kept constant, then the EGL does act as a size-selective filter.
Stevens et al. (2007) used fluorescence correlation spectroscopy to study albumin transport within the EGL of cultured bovine lung microvascular endothelial cells. AlexaFluor (AF) 532-labeled albumin could penetrate into the top layer of the EGL, within which its diffusion was inhibited by approximately 30 % relative to its free diffusivity. However, the tracer appeared to be excluded from the basal region of the EGL. Interestingly, the interaction altered if the EGL was exposed to an excess of albumin; in fact, even relatively low levels of unlabeled albumin significantly reduced penetration of the labeled albumin into the EGL. Moreover, digestion of the EGL with heparanase III allowed the labeled albumin to penetrate further into the EGL, and EGL digestion with hyaluronidase effectively stopped it interacting with the EGL at all. Taken together, these results suggest that albumin can penetrate into the loosely attached top layer of the EGL, within which its diffusion is inhibited via its interaction with hyaluronan. However, it cannot easily penetrate into the more firmly attached basal layer of the EGL, which is densely populated with heparan sulfate.
More recently, Gao and Lipowsky (2009) combined intra-vital microscopy and computational simulations to quantify various properties of the EGL. Experimentally, they found that FITC-labeled dextran 70 did not penetrate significantly into the EGL of the rat ileocolic artery, but unbound FITC did. Additionally, they showed that diffusion of FITC within the EGL was hindered (relative to its free diffusivity) by a factor of order 400. As the authors pointed out, this is significantly more than predicted by either pore or fiber models of the EGL, suggesting that mass transport properties within the EGL are not determined by its structure alone. Also, in a follow-up study, Gao and Lipowsky (2010) investigated how mass transport properties vary spatially within the EGL. Specifically, they calculated the diffusion coefficient of FITC in the entire EGL and in a smaller sub-layer rising 173 nm above the endothelial cell surface. Diffusion in this sub-layer was found to be half that in the EGL as a whole. Moreover, chondroitinase and hyaluronidase both caused the diffusion of FITC to increase significantly, whereas heparinase decreased the diffusion coefficient of FITC in the EGL as a whole, but did not affect diffusivity in the sub-layer. Collectively, the results suggest that the EGL is denser near the endothelial surface. They also suggest a non-uniform distribution of components throughout EGL and that the EGL may compact when some components are removed.
3.3 Theoretical studies
3.3.1 Modification of Starling’s hypothesis (the Michel–Weinbaum model)
Michel (1997) and Weinbaum (1997) independently proposed a revised version of Starling’s hypothesis, now referred to as the Michel–Weinbaum model, in which the EGL plays a central role. Starling introduced the idea that water flux across the capillary wall is driven by hydrostatic and colloid osmotic (‘oncotic’) pressure gradients, the latter being multiplied by a reflection coefficient indicating the ability of the wall to hold back plasma proteins. The expectation was that water would leave the capillary at its arterial end, where the luminal hydrostatic pressure is relatively high, and would be reabsorbed at the venous end, where this pressure is lower. However, when modern techniques permitted accurate measurement of the pressures and reflection coefficient, it became clear that water would leave the capillary over its entire length and would not be reabsorbed. Since lymph flow is inadequate to explain the return of all of the extravasated water, Starling’s hypothesis is untenable in its original form. Michel and Weinbaum suggested that the main semi-permeable membrane restricting the transmural transport of plasma proteins, while permitting water flux, was the EGL and that consequently the classic Starling force balance should be applied across the EGL alone and not across the entire wall (see Hu and Weinbaum 1999 for further details and implications). The Michel–Weinbaum model and its subsequent experimental validation (Hu et al. 2000; Pang and Tarbell 2003; Adamson et al. 2004) brought the EGL to the fore as a key determinant of arterial wall mass transport properties.
3.3.2 Modeling transport of low density lipoproteins
Dabagh et al. (2009) included the EGL when developing a model of LDL transport across a deformable arterial wall. Their study was one of the first to consider how pressure-induced deformation (compaction) of layers within the arterial wall can modulate transport of LDL through it. However, it did not explicitly model the interaction of LDL with the EGL. Subsequent studies by Vincent et al. (2010) simulated LDL concentration polarization at the luminal surface of the endothelium, including the effect of intercellular clefts and the EGL. They found that the degree of LDL concentration polarization depended critically on how LDL interacted with the EGL. In particular, the degree of concentration polarization depended on the depth to which LDL could penetrate into the EGL and the diffusivity of LDL within the EGL. More recently, Liu et al. (2011) developed a theoretical model of LDL transport in an idealized arterial geometry that included various layers of the arterial wall, as well as the EGL. Once again, the results suggested that the EGL plays a critical role in regulating LDL transport into the arterial wall. Specifically, they predicted that reducing the thickness of the EGL, or reducing its barrier function (by damaging it), would lead to enhanced accumulation of LDL in the intima. Their results also suggested that raised blood pressure (hypertension) or an increased number density of ‘leaky’ intercellular clefts have a much more limited effect on transendothelial LDL transport when an EGL is present.
3.3.3 Modeling transport of nitric oxide and oxygen
Chen et al. (2006) developed a theoretical model to study O\(_2\) and NO transport in capillaries. While the model did not explicitly include interaction of O\(_2\) and NO with the EGL, it did predict that the thickness of the EGL would affect O\(_2\) and NO transport via its effect on the hematocrit and thus the rate at which O\(_2\) and NO were scavenged in the blood. More precisely, the model suggested that as the thickness of the EGL increased, the luminal space for red blood cells would be reduced and hematocrit would rise, leading to an increase in the rate at which O\(_2\) and NO were scavenged. While this result is interesting, it is only relevant in capillaries, where the EGL thickness is a significant fraction of the luminal diameter.
3.3.4 Modeling transport of charged species
Stace and Damiano (2001) developed a one-dimensional axisymmetric model of electrodiffusion within the EGL of capillaries. The model, which was motivated by Vink and Duling’s (2000) charge-dependent transport observations, combined classical Fickian diffusion with Ohm’s Law, Gauss’s Law, and conservation of mass in order to model transport of a free anionic tracer outside and within the EGL. The EGL was modeled as a fixed distribution of negative charge, and the effect of free ionic salts (Na\(^+\) and Cl\(^-\)) was also included. It was found that in steady state, anionic tracers were excluded from the EGL and that the degree of such exclusion increased as the negative charge associated with the EGL and tracers increased. Also, dynamic analysis suggested that the diffusion time for anionic tracers through the EGL increased exponentially with tracer charge.
Fu et al. (2003) extended their earlier mathematical model of mass transport through the EGL and intercellular clefts (with broken tight-junction strands) (Fu et al. 1994) to include the effects of electric charge. They developed a two-dimensional model of electrodiffusion above and within the clefts that included a negatively charged EGL. The model predicted that a negatively charged EGL would inhibit transport of negatively charged solutes across the endothelium more than it would inhibit transport of positively charged ones. Interestingly, however, the model also suggested that this effect would be counteracted by an excess of Na\(^+\) over Cl\(^-\) ions near the luminal surface of the EGL—an excess would occur if negatively charged proteins were present near the surface. Finally, the model predicted that the overall permeability of the endothelium to charged solutes would be independent of the charge distribution within the EGL so long as the maximum and overall charge remain constant.
The model of Fu et al. (2003) was further extended by Chen and Fu (2004) to include the effects of convection through the intercellular clefts. This revised model predicted that convective transport of negatively charged albumin through the endothelium would be greatly inhibited by the presence of a negatively charged EGL. Additionally, the model predicted that while increasing the width of the intercellular clefts would increase hydraulic permeability, it would have little effect on transport of albumin across the endothelium so long as a negatively charged EGL was present.
3.4 Implications for atherosclerosis
The studies cited above suggest that the EGL plays a critical role in vascular mass transport. However, none of the experimental studies, and only a handful of the theoretical studies, focus on the transport of LDL, HDL, ATP, ADP, NO, or O\(_2\), which are the species most heavily implicated in atherogenesis. The interaction of these six species with the EGL remains ill-understood. It is reasonable, however, to speculate as follows:
-
LDL macromolecules have a mass of approximately 3 MDa. Consequently, the studies of fluorescently labeled dextran transport (Vink and Duling 2000; van Haaren et al. 2003) suggest that LDL will be excluded from the EGL. However, experiments with other tracers suggest that the EGL does not behave as a purely size-selective filter (Vink and Duling 2000) and that macromolecules such as albumin and fibrinogen can penetrate into, and interact with, the EGL (Turner et al. 1983; Adamson and Clough 1992; Vink and Duling 2000), or at least its most luminal layer (Stevens et al. 2007). It is therefore possible that some LDL penetrates into, or forms part of, the more loosely attached top layer of the EGL. It is also possible that this process is enhanced by a convective transmural flux causing concentration polarization of LDL at the luminal surface of arteries. The exact nature of interactions between LDL and the EGL, once established, will likely have important implications for both transcellular and paracellular transendothelial LDL transport, and thus atherogenesis.
-
HDL macromolecules have a mass of order 100 kDa [possibly as low as 70 kDa (Atmeh 1990)]. This is similar to the FITC-labeled albumin and dextran complex, and the FITC-labeled fibrinogen, which Vink and Duling (2000) found could penetrate into the EGL. Consequently, it is plausible that HDL is able to penetrate into, and interact with, the EGL. As with LDL, the exact nature of interactions between HDL and the EGL, once established, will likely have important implications for both transcellular and paracellular transendothelial HDL transport and thus atherogenesis.
-
ATP, ADP, NO, and O\(_2\) are much smaller than LDL and HDL. Based on their small size, it is unlikely that the EGL will impact either their diffusion or convection. However, it is possible that they interact with the EGL in some other way; there is evidence to suggest that O\(_2\), at least, can have an effect on the composition of the EGL (Annecke et al. 2011). Finally, as suggested by Chen et al., it is possible that the thickness of the EGL can affect the blood hematocrit and hence the rate at which NO and O\(_2\) are scavenged in the blood. However, this effect would only be significant in capillaries, not in the large- and medium-sized arteries where atherogenesis occurs.
In summary, while the details remain unclear, experimental and theoretical studies suggest that the EGL could have an important effect on transport of species involved in atherogenesis and hence on atherogenesis itself.
3.5 Future studies
3.5.1 Future experimental studies
Future experimental studies should determine how LDL interacts with the EGL, since this is likely to have important implications for both transcellular and paracellular LDL transport across the endothelium and thus atherogenesis. Specifically, it is important to ascertain the extent to which LDL can penetrate into the EGL and, if it does penetrate into the EGL, how its transport properties are affected. It is also important to ascertain whether LDL reacts or combines with the EGL in any way. LDL is known to bind to components of the interstitial matrix that are similar to components of the EGL. Answering these questions in vivo currently poses a significant challenge. However, similar questions concerning albumin have been successfully addressed in vitro using fluorescence correlation spectroscopy (Stevens et al. 2007). Extension of such experiments to investigate the interaction of LDL with the EGL might be feasible.
3.5.2 Future theoretical studies
Given its complex and heterogeneous structure, it may be impossible to capture all mass transport properties of the EGL using ‘classical’ continuum mechanics alone, especially when modeling interactions of large macromolecules such as LDL. Instead, it may be necessary to model the EGL at an atomistic or molecular level. An ‘all atom’ molecular dynamics simulation of the EGL remains unfeasible [currently such simulations have time-scales of order 100 ns and length-scales of order 10 nm (Lervik et al. 2013)]. However, so-called coarse-grained approaches (Venturoli et al. 2006; Yin et al. 2009; Flores et al. 2012), in which the total number of degrees of freedom are reduced by combining relevant groups of atoms, offer a viable alternative. Indeed, coarse-grained molecular dynamics simulations of the EGL have already been attempted by Danova-Okpetu (2005), and more recently by Gniewek and Kolinski (2012). It is hoped that the advent of massively parallel, many-core platforms such as Graphical Processing Units will further increase the feasibility of such calculations in the future, due to the natural mapping of molecular dynamics algorithms to these architectures.
4 Conclusions
Research over the past decades has placed significant emphasis on understanding how mechanical flow forces per se are involved in regulating the development of atherosclerosis. However, far less attention has been paid to the role of arterial mass transport. While a significant body of work suggests flow forces per se are important, there is increasing evidence to suggest that complex, multi-scale arterial mass transport processes involving various species also play a critical role in the development of atherosclerosis and its regulation by blood flow.
This short review has focused on one vascular-scale flow-regulated arterial mass transport process, namely the formation of an LDL concentration polarization layer at the luminal surface of the arterial endothelium, as well as one cellular-scale determinant of arterial wall mass transport, namely the EGL. A literature review has revealed that several important aspects of both remain to be elucidated. A range of possible future studies have been suggested. It is hoped that such studies will provide further understanding of how atherosclerosis develops and lead to novel therapies for treating the disease.
References
Adams CMW (1973) Tissue changes and lipid entry in developing atheroma. In: Porter R, Knight J (eds) Ciba foundation symposium 12-atherogenesis: initiating factors, Novartis Foundation Symposia. Wiley, Chichester
Adamson RH, Clough G (1992) Plasma proteins modify the endothelial cell glycocalyx of frog mesenteric microvessels. J Physiol 445:473
Adamson RH, Lenz JF, Zhang X, Adamson GN, Weinbaum S, Curry FE (2004) Oncotic pressures opposing filtration across non-fenestrated rat microvessels. J Physiol 557:889
Adamson RH, Sarai RK, Altangerel A, Clark JF, Weinbaum S, Curry FE (2013) Microvascular permeability to water is independent of shear stress, but dependent on flow direction. Am J Physiol Heart Circ Physiol 304:H1077
Albelda SM, Sampson PM, Haselton FR, McNiff JM, Mueller SN, Williams SK, Fishman AP, Levine EM (1988) Permeability characteristics of cultured endothelial cell monolayers. J Appl Physiol 64:308
Annecke T, Fischer J, Hartmann H, Tschoep J, Rehm M, Conzen P, Sommerhoff CP, Becker BF (2011) Shedding of the coronary endothelial glycocalyx: effects of hypoxia/reoxygenation vs ischaemia/reperfusion. Brit J Anaesth 107:679
Atmeh RF (1990) Isolation and identification of HDL particles of low molecular weight. J Lipid Res 31:1771
Berliner JA, Navab M, Fogelman AM, Frank JS, Demer LL, Edwards PA, Watson AD, Lusis AJ (1995) Atherosclerosis: basic mechanisms. Oxidation, inflammation, and genetics. Circulation 91:2488
Bratzler RL, Chisolm GM, Colton CK, Smith KA, Lees RS (1977) The distribution of labeled low-density lipoproteins across the rabbit thoracic aorta in vivo. Atherosclerosis 28:289
Caro CG, Fitz-Gerald JM, Schroter RC (1969) Arterial wall shear and distribution of early atheroma in man. Nature 223:1159
Caro CG, Fitz-Gerald JM, Schroter RC (1971) Atheroma and arterial wall shear. Observation, correlation and proposal of a shear dependent mass transfer mechanism for atherogenesis. Proc R Soc Lond B Biol Sci 177:109
Chang YS, Munn LL, Hillsley MV, Dull RO, Yuan J, Lakshminarayanan S, Gardner TW, Jain RK, Tarbell JM (2000) Effect of vascular endothelial growth factor on cultured endothelial cell monolayer transport properties. Microvasc Res 59:265
Chen B, Fu BM (2004) An electrodiffusion-filtration model for effects of endothelial surface glycocalyx on microvessel permeability to macromolecules. J Biomech Eng 126:614
Chen X, Jaron D, Barbee KA, Buerk DG (2006) The influence of radial RBC distribution, blood velocity profiles, and glycocalyx on coupled NO/O\(_2\) transport. J Appl Physiol 100:482
Cheng C, de Crom R, van Haperen R, Helderman F, Mousavi GB, van Damme LCA, Kirschbaum SW, Slager CJ, van der Steen AFW, Krams R (2004) The role of shear stress in atherosclerosis: action through gene expression and inflammation. Cell Biochem Biophys 41:279
Choi HW, Ferrara KW, Barakat AI (2007) Modulation of ATP/ADP concentration at the endothelial surface by shear stress: effect of flow recirculation. Ann Biomed Eng 35:505
Choi HW, Barakat AI (2009) Modulation of ATP/ADP concentration at the endothelial cell surface by flow: effect of cell topography. Ann Biomed Eng 37:2459
Curry FE, Adamson RH (2012) Endothelial glycocalyx: permeability barrier and mechanosensor. Ann Biomed Eng 40:828
Curry FE, Michel CC (1980) A fiber matrix model of capillary permeability. Microvasc Res 20:96
Dabagh M, Jalali P, Tarbell JM (2009) The transport of LDL across the deformable arterial wall: the effect of endothelial cell turnover and intimal deformation under hypertension. Am J Physiol Heart Circ Physiol 297:H983
Damiano ER, Long DS, Smith ML (2004) Estimation of viscosity profiles using velocimetry data from parallel flows of linearly viscous fluids: application to microvascular haemodynamics. J Fluid Mech 512:1
Danova-Okpetu D (2005) Macromolecular studies of the dynamic structure and mechanical properties of the endothelial surface layer, PhD thesis. Johns Hopkins
Deng X, Marois Y, How T, Merhi Y, King M, Guidoin R, Karino T (1995) Luminal surface concentration of lipoprotein (LDL) and its effect on the wall uptake of cholesterol by canine carotid arteries. J Vasc Surg 21:135
Ding Z, Fan Y, Deng X (2009) Effect of LDL concentration polarization on the uptake of LDL by human endothelial cells and smooth muscle cells co-cultured. Acta Bioch Bioph Sin 41:146
Dull RO, Jo H, Sill H, Hollis TM, Tarbell JM (1991) The effect of varying albumin concentration and hydrostatic pressure on hydraulic conductivity and albumin permeability of cultured endothelial monolayers. Microvasc Res 41:390
Ebong EE, Macaluso FP, Spray DC, Tarbell JM (2011) Imaging the endothelial glycocalyx in vitro by rapid freezing/freeze substitution transmission electron microscopy. Arterioscl Throm Vas 31:1908
Ethier CR (2002) Computational modeling of mass transfer and links to atherosclerosis. Ann Biomed Eng 30:461
Faergeman O (2003) Coronary artery disease—genes, drugs and the agricultural connection. Elsevier, Amsterdam
Fatouraee N, Deng X, Champlain A, Guidoin R (1998) Concentration polarization of low density lipoproteins (LDL) in the arterial system. Ann NY Acad Sci 858:137
Flores SC, Bernauer J, Shin S, Zhou R, Huang X (2012) Multiscale modeling of macromolecular biosystems. Brief Bioinform 13:395
Fry DL (1968) Acute vascular endothelial changes associated with increased blood velocity gradients. Circ Res 22:165
Fu BM, Weinbaum S, Tsay RY, Curry FE (1994) A junction-orifice-fiber entrance layer model for capillary permeability: application to frog mesenteric capillaries. J Biomech Eng 116:502
Fu BM, Chen B, Chen W (2003) An electrodiffusion model for effects of surface glycocalyx layer on microvessel permeability. Am J Phys Heart Circ Physiol 284:H1240
Gao L, Lipowsky HH (2009) Measurement of solute transport in the endothelial glycocalyx using indicator dilution techniques. Ann Biomed Eng 37:1781
Gao L, Lipowsky HH (2010) Composition of the endothelial glycocalyx and its relation to its thickness and diffusion of small solutes. Microvasc Res 80:394
Gniewek P, Kolinski A (2012) Coarse-grained modeling of mucus barrier properties. Biophys J 102:195
Gorog P, Born GV (1982) Increased uptake of circulating low-density lipoproteins and fibrinogen by arterial walls after removal of sialic acids from their endothelial surface. Br J Exp Pathol 63:447
Hahn C, Schwartz MA (2009) Mechanotransduction in vascular physiology and atherogenesis. Nat Rev Mol Cell Biol 10:53
Henry CBS, Duling BR (1999) Permeation of the luminal capillary glycocalyx is determined by hyaluronan. Am J Physiol Heart Circ Physiol 277:H508
Henry CB, Duling BR (2000) TNF-\({\alpha }\) increases entry of macromolecules into luminal endothelial cell glycocalyx. Am J Physiol Heart Circ Physiol 279:H2815
Hu X, Weinbaum S (1999) A new view of Starling’s hypothesis at the microstructural level. Microvasc Res 58:281
Hu X, Adamson RH, Liu B, Curry FE, Weinbaum S (2000) Starling forces that oppose filtration after tissue oncotic pressure is increased. Am J Physiol Heart Circ Physiol 279:1724
Jellinek H (1983) The drainage of transmural flow and the consequences of its insufficiency. In: Schettler G, Nerem RM, Schmid-Schonbein H, Morl H, Diehm C (eds) Fluid dynamics as a localizing factor for atherosclerosis. Springer, Berlin
John K, Barakat AI (2001) Modulation of ATP/ADP concentration at the endothelial surface by shear stress: effect of flow-induced ATP release. Ann Biomed Eng 29:740
Koo A, Dewey CF, García-Cardeña G (2013) Hemodynamic shear stress characteristic of atherosclerosis-resistant regions promotes glycocalyx formation in cultured endothelial cells. Am J Physiol Cell Physiol 304:C137
Ku DN, Giddens DP, Zarins CK, Glagov S (1985) Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arteriosclerosis 5:293
Lantz J, Karlsson M (2012) Large eddy simulation of LDL surface concentration in a subject specific human aorta. J Biomech 45:537
Lervik A, Bresme F, Kjelstrup S (2013) Molecular dynamics simulations of the Ca\(^{2+}\) pump: a structural analysis. Phys Chem Chem Phys 14:3543
Levick JR, Michel CC (1973) The effect of bovine albumin on the Permeability of frog mesenteric capillaries. Exp Physiol 58:87
Lipowsky HH, Lescanic A (2013) Shear-dependent adhesion of leukocytes and lectins to the endothelium and concurrent changes in thickness of the glycocalyx of post-capillary venules in the low-flow state. Microcirculation 20:149
Liu X, Pu F, Fan Y, Deng X, Li D, Li S (2009) A numerical study on the flow of blood and the transport of LDL in the human aorta: the physiological significance of the helical flow in the aortic arch. Am J Physiol-Heart C 297:H163
Liu X, Fan Y, Deng X (2011) Effect of the endothelial glycocalyx layer on arterial LDL transport under normal and high pressure. J Theor Biol 283:71
Luckett PM, Fischbarg J, Bhattacharya J, Silverstein SC (1989) Hydraulic conductivity of endothelial cell monolayers cultured on human amnion. Am J Physiol 256:H1675
Mackay J, Mensah G (2004) The atlas of heart disease and stroke. World Health Organization, Geneva
Mason J, Curry F, Michel C (1977) The effects of proteins upon the filtration coefficient of individually perfused frog mesenteric capillaries. Microvasc Res 13:185
Megens RTA, Reitsma S, Schiffers PHM, Hilgers RHP, De Mey JGR, Slaaf DW, oude Egbrink MGA, van Zandvoort MAMJ (2007) Two-photon microscopy of vital murine elastic and muscular arteries. Combined structural and functional imaging with subcellular resolution. J Vasc Res 44:87
Meng W, Yu F, Chen H, Zhang J, Zhang E, Dian K, Shi Y (2009) Concentration polarization of high-density lipoprotein and its relation with shear stress in an in vitro model. J Biomed Biotechnol 2009: 695838
Michel CC (1980) Filtration coefficients and osmotic reflexion coefficients of the walls of single frog mesenteric capillaries. J Physiol 309:341
Michel CC, Phillips ME, Turner MR (1985) The effects of native and modified bovine serum albumin on the permeability of frog mesenteric capillaries. J Physiol 360:333
Michel CC (1997) Starling: the formulation of his hypothesis of microvascular fluid exchange and its significance after 100 years. Exp Physiol 82:1
Napoli C, de Nigris F, Williams-Ignarro S, Pignalosa O, Sica V, Ignarro LJ (2006) Nitric oxide and atherosclerosis: an update. Nitric Oxide-Biol Ch 15:265
Pang Z, Tarbell JM (2003) In vitro study of Starling’s hypothesis in a cultured monolayer of bovine aortic endothelial cells. J Vasc Res 40:351
Pries AR, Secomb TW, Gaehtgens P (2000) The endothelial surface layer. Pflugers Arch 440:653
Rader DJ (2003) Regulation of reverse cholesterol transport and clinical implications. Am J Cardiol 92:42
Reitsma S, Slaaf DW, Vink H, van Zandvoort MAMJ, Oude Egbrink MGA (2007) The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch 454:345
Rindfleisch E (1872) A manual of pathological histology to serve as an introduction to the study of mordib anatomy. The New Sydenham Society, London
Scharfstein H, Gutstein WH, Lewis L (1963) Changes of boundary layer flow in model systems: implications for initiation of endothelial injury. Circ Res 13:580
Schnitzer JE, Carley WW, Palade GE (1988) Albumin interacts specifically with a 60-kDa microvascular endothelial glycoprotein. PNAS 85:6773
Schnitzer JE, Carley WW, Palade GE (1988) Specific albumin binding to microvascular endothelium in culture. Am J Physiol 254:H425
Schwartz CJ, Valente AJ, Sprague EA (1993) A modern view of atherogenesis. Am J Cardiol 71:9B
Secomb TW, Hsu R, Pries AR (2001) Motion of red blood cells in a capillary with an endothelial surface layer: effect of flow velocity. Am J Physiol Heart Circ Physiol 281:H629
Shaaban AM, Duerinckx AJ (2000) Wall shear stress and early atherosclerosis: a review. Am J Roentgenol 174:1657
Smith ML, Long DS, Damiano ER, Ley K (2003) Near-wall micro-PIV reveals a hydrodynamically relevant endothelial surface layer in venules in vivo. Biophys J 85:637
Stace TM, Damiano ER (2001) An electrochemical model of the transport of charged molecules through the capillary glycocalyx. Biophys J 80:1670
Stevens AP, Hlady V, Dull RO (2007) Fluorescence correlation spectroscopy can probe albumin dynamics inside lung endothelial glycocalyx. Am J Physiol Lung Cell Mol Physiol 293:L328
Suttorp N, Hessz T, Seeger W, Wilke A, Koob R, Lutz F, Drenckhahn D (1988) Bacterial exotoxins and endothelial permeability for water and albumin in vitro. Am J Physiol 255:C368
Tarbell JM, Qiu Y (2000) Arterial wall mass transport: the possible role of blood phase resistance in the localization of arterial disease. In: Bronzino JD (ed) The biomedical engineering handbook, 2nd edn. CRC Press, New York
Tarbell JM (2003) Mass transport in arteries and the localization of atherosclerosis. Annu Rev Biomed Eng 5:79
Tarbell JM, Weinbaum S, Kamm RD (2005) Cellular fluid mechanics and mechanotransduction. Ann Biomed Eng 33:1719
Tarbell JM (2010) Shear stress and the endothelial transport barrier. Cardiovasc Res 87:320
Tedgui A, Lever MJ (1984) Filtration through damaged and undamaged rabbit thoracic aorta. Am J Physiol 247:H784
Turner MR, Clough G, Michel CC (1983) The effects of cationised ferritin and native ferritin upon the filtration coefficient of single frog capillaries. Evidence that proteins in the endothelial cell coat influence permeability. Microvasc Res 25:205
Turner MR (1992) Flows of liquid and electrical current through monolayers of cultured bovine arterial endothelium. J Physiol 449:1
Valenta DT, Bulgrien JJ, Banka CL, Curtiss LK (2006) Overexpression of human ApoAI transgene provides long-term atheroprotection in LDL receptor-deficient mice. Atherosclerosis 189:255
van den Berg BM, Vink H, Spaan JAE (2003) The endothelial glycocalyx protects against myocardial edema. Circ Res 92:592
van den Berg BM, Spaan JAE, Rolf TM, Vink H (2006) Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation. Am J Physiol Heart Circ Physiol 290:915
van Haaren PMA, Van Bavel E, Vink H, Spaan JAE (2003) Localization of the permeability barrier to solutes in isolated arteries by confocal microscopy. Am J Physiol Heart Circ Physiol 285:H2848
Van Teeffelen JW, Brands J, Stroes ES, Vink H (2007) Endothelial glycocalyx: sweet shield of blood vessels. Trends Cardiovas Med 17:101
Venturoli M, Maddalenasperotto M, Kranenburg M, Smit B (2006) Mesoscopic models of biological membranes. Phys Rep 437:1
Vincent PE (2009) A cellular scale study of low density lipoprotein concentration polarisation in arteries, PhD thesis. Imperial College, London
Vincent PE, Sherwin SJ, Weinberg PD (2009) The effect of a spatially heterogeneous transmural water flux on concentration polarization of low density lipoprotein in arteries. Biophys J 96:3102
Vincent PE, Sherwin SJ, Weinberg PD (2010) The effect of the endothelial glycocalyx layer on concentration polarisation of low density lipoprotein in arteries. J Theor Biol 265:1
Vink H, Duling BR (1996) Identification of distinct luminal domains for macromolecules, erythrocytes, and leukocytes within mammalian capillaries. Circ Res 79:581
Vink H, Duling BR (2000) Capillary endothelial surface layer selectively reduces plasma solute distribution volume. Am J Physiol Heart Circ Physiol 278:H285
Wada S, Karino T (1999) Theoretical study on flow-dependent concentration polarization of low density lipoproteins at the luminal surface of a straight artery. Biorheology 36:207
Wada S, Karino T (2002) Theoretical prediction of low-density lipoproteins concentration at the luminal surface of an artery with a multiple bend. Ann Biomed Eng 30:778
Wada S, Koujiya M, Karino T (2002) Theoretical study of the effect of local flow disturbances on the concentration of low-density lipoproteins at the luminal surface of end-to-end anastomosed vessels. Med Biol Eng Comput 40:576
Wada S, Karino T (2002) Prediction of LDL concentration at the luminal surface of a vascular endothelium. Biorheology 39:331
Wakeman W, Salpadoru N, Caro C (1976) Diffusion coefficients for protein molecules in blood serum. Atherosclerosis 25:225
Wang G, Deng X, Guidoin R (2003) Concentration polarization of macromolecules in canine carotid arteries and its implication for the localization of atherogenesis. J Biomech 36:45
Wei D, Wang G, Tang C, Qiu J, Zhao J, Gregersen H, Deng L (2012) Upregulation of SDF-1 is associated with atherosclerosis lesions induced by LDL concentration polarization. Ann Biomed Eng 40:1018
Weinbaum S (1997) Whitaker distinguished lecture: models to solve mysteries in biomechanics at the cellular level; a new view of fiber matrix layers. Ann Biomed Eng 26:627
Weinbaum S, Zhang X, Han Y, Vink H, Cowin SC (2003) Mechanotransduction and flow across the endothelial glycocalyx. Proc Natl Acad Sci USA 100:7988
Weinbaum S, Tarbell JM, Damiano ER (2007) The structure and function of the endothelial glycocalyx layer. Annu Rev Biomed Eng 9:121
Wolinsky H, Glagov S (1967) Nature of species differences in the medial distribution of aortic vasa vasorum in mammals. Circ Res 20:409
Woolf N (1990) Pathology of atherosclerosis. Br Med Bull 46:960
Yin Y, Arkhipov A, Schulten K (2009) Simulations of membrane tubulation by lattices of amphiphysin N-bar domains. Structure 17:882
Zeman LJ, Zydney AL (1996) Microfiltration and ultrafiltration: principles and applications. CRC Press, Boca Raton
Zhang Z, Deng X, Fan Y, Li D (2007) Ex vitro experimental study on concentration polarization of macromolecules (LDL) at an arterial stenosis. Sci China Ser C 50:486
Zydney AL (1997) Stagnant film model for concentration polarization in membrane systems. J Membrane Sci 130:275
Acknowledgments
The authors are grateful to the British Heart Foundation (BHF) and the BHF Centre of Research Excellence at Imperial College London for funding studies of arterial mass transport and its modulation by the EGL. The authors would also like to thank Fernando Bresme and Amparo Galindo for useful discussions regarding molecular-scale modeling of the EGL.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vincent, P.E., Weinberg, P.D. Flow-dependent concentration polarization and the endothelial glycocalyx layer: multi-scale aspects of arterial mass transport and their implications for atherosclerosis. Biomech Model Mechanobiol 13, 313–326 (2014). https://doi.org/10.1007/s10237-013-0512-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-013-0512-1