Abstract
An important element of the process by which new drugs achieve widespread use is their adoption by GPs. In this paper, we explore the factors that shape the timing of the first prescription of six new drugs by General Practitioners in Ireland. Our analysis is based on a dataset that matches prescription data with data on GP characteristics. We then use duration analysis to explore both equilibrium and non-equilibrium determinants of prescribing innovation. Our study highlights a range of commonalities across all of the drugs considered and suggests the importance of GP and practice characteristics in shaping prescribing decisions. We also find strongly significant, and consistently signed, stock and order effects across these drugs: GPs who have a track record of early adoption tend also to be early adopters of other new drugs; and, the larger the proportion of GPs which have already adopted a new drug the slower is subsequent adoption. Epidemic and learning effects are also evident with slower adoption by rural practices and among those GPs with narrower prescribing portfolios.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent years have witnessed the rapid development of drug treatments in a number of therapeutic areas. For example, some of the top selling prescription drugs include the following: statins for lowering blood cholesterol; proton-pump inhibitors for reducing gastric acid production; and long-acting beta agonists for the treatment of asthma and chronic obstructive pulmonary disease (COPD). In addition, primary care practitioners have increasingly moved into providing support to public health measures in areas such as depression, mental health and smoking. In Ireland, as in most other European Union (EU) economies, access to new drugs and treatments is mainly through primary healthcare providers such as general practitioners (GPs) or family doctors [1, 2]. An important element of the process by which new drugs achieve widespread use is therefore their adoption by GPs as part of the portfolio of drugs which they prescribe. In this paper, we explore the factors that shape the timing of the first prescription of new drugs by GPs in Ireland and hence their availability to potential patients [3, 4]. We focus specifically on the adoption of six new drugs that were introduced to the Irish market during the period October 1999–March 2004 and that represent different therapeutic areas.
Our study focuses on these prescribing innovations by GPs in Ireland.Footnote 1 Irish GPs are by and large self-employed, private practitioners who choose where they set up their practices, who they employ, and how much they charge for consultations and any additional services they provide [6, 7]. The majority of Irish GPs treat private patients but also hold a contract with the government to treat those patients who qualify for a Medical Card. Medical card or General Medical Services (GMS) patients are public patients who are entitled to attend GPs free of charge and also receive prescription medicines free of charge.Footnote 2 Approximately, 30% of the Irish population are entitled to these means-tested medical cards; however, it has been estimated that the GMS patients account for approximately 50% of all GP consultations [8], and that government spending through medical card patients makes up a substantial part of general practices’ funding [9]Footnote 3,Footnote 4. The remainder of the Irish population are classed as private patients, and they pay directly for each visit to a GP and for any additional services provided by each GP.Footnote 5
Along with the discretion which Irish GPs have in terms of the nature and location of their practice, they also have considerable autonomy in relation to prescribing decisions. Once a particular drug has been approved for use by the Irish Medicines Board, GPs can prescribe it to their patients.Footnote 6 In Ireland, there are no explicit guidelines in relation to prescribing decisions, such as the National Institute for Clinical Excellence (NICE) in the UK.Footnote 7 The commercial and prescribing autonomy that characterises Irish general practice suggests that the prescribing decisions of Irish GPs may reflect both medical and commercial factors. Prescribing innovation may enable GPs to provide more effective treatments but may also help to attract and retain mobile and commercially valuable private and public patients. This suggests the potential value of considering both informational and commercial factors as determinants of GPs’ prescribing innovation [13]. In the innovation literature, informational or learning effects are generally interpreted as disequilibrium determinants of adoption, while commercial factors are reflected in equilibrium elements reflecting the influence of individual practice heterogeneity (rank effects) and strategic behaviour (stock and order effects).
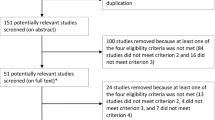
To our knowledge, our study is the first to use duration analysis to examine prescribing innovation [14]. Duration analysis focuses on the factors that determine the probability that a GP will prescribe a new drug by a specific point in time and provides a method of modelling the adoption S-curve for newly introduced drugs [4]. The advantage of duration analysis is that it enables us to adopt a holistic approach to modelling the determinants of prescribing innovation including a range of GP and practice characteristics, previous prescribing behaviour and equilibrium factors related to practices’ strategic behaviour. Our empirical approach is to apply duration analysis to a diverse group of prescribing innovations to try and identify commonalities in the determinants of prescribing innovation. Data are taken from a matched database that brings together information on GP’s prescribing history with information on the characteristics of GPs themselves. Data on GPs’ prescribing behaviour are derived from the General Medical Services (GMS) Prescribing Database which provides information on all prescriptions written by a sample of approximately 600 GPs for GMS patients. Matching background information on the GPs themselves is taken from administrative data provided on a confidential basis by the HSE.
The rest of the paper is organised as follows. Section 2 outlines the conceptual framework for our study emphasising the potential for both informational and strategic influences on the timing of GPs prescribing innovations. Section 3 describes our data sources, profiles the group of drugs which we consider and outlines our econometric approach. Section 4 summarises the main econometric results, and the implications are considered in Sect. 5.
Conceptual framework
Our unit of analysis here is the individual GP, and our focus is on the factors that shape their prescribing innovations. For the purposes of this paper and in line with previous literature, a GP makes a prescribing innovation when s/he prescribes a drug on at least one occasion to at least one patientFootnote 8 [3, 4]. Individual prescribing innovations will reflect the perceived benefits of the new drug compared to the alternatives and may reflect the availability of information on the efficacy of the new drug as well as any commercial implications. Taken together, the cumulative or aggregate result and timing of prescribing innovations by GPs will determine the level of diffusion of each new drug [4, 15, 16]. It is important to note that here we are concerned with the diffusion of these drugs in relation to GPs decisions to prescribe them for the first time, not the number of times which they prescribe or the extent to which these drugs penetrate the market, i.e. their market share.
Two complementary theoretical approaches have been used to explain the timing of innovation decisions. Equilibrium models, reflecting organisational characteristics and strategic interactions, have been used primarily to examine the first adoption of new technologies by firms [13], while disequilibrium models, which take account of epidemic and learning effects, have been used primarily to examine innovation by individuals [4]. In these models first adoption is seen primarily as the result of the spread of information, generally assuming that (i) a potential user will adopt a new technology upon learning of its existence and (ii) information on the existence of the technology is spread by direct contact between existing and potential users [4]. The implication of this simple epidemic model is that non-adopters are more likely to innovate the more widespread is existing adoption by other members of their social system.
Unlike the implicit assumption of asymmetric information in disequilibrium or epidemic models of adoption, equilibrium models assume that information in the economy is perfect. In equilibrium models, differences in the timing of adoption therefore occur not because of the spread of information but because of the gains from adoption relative to its costs. As these gains change over time, so too does the number of adopters. Three equilibrium effects on the timing of adoption are generally identified: rank, stock and order effects. Rank (or probit) effects result from the assumption that potential adopters of a technology have different characteristics and therefore may obtain different returns from the use of a new technology. Here, potential adopters’ heterogeneity is the key driver of the timing of adoption [13]. Stock effects are based on the idea that as the number of users of a new technology increases, the benefits from adoption decline. This steadily reduces the benefit-cost ratio until, at a certain point in time, the number of accumulated adopters makes adoption by the remaining non-adopters undesirable. Finally, order effects suggest that an individual or organisation’s position in the adoption order determines its returns from the use of the technology. Earlier adopters—those higher in the adoption order—will obtain greater returns than later adopters. Therefore, if a potential adopter expects the number of future adopters to be high, it will decide to adopt earlier [13]. Both the stock and order effects capture strategic behaviour reflecting trade-offs between the costs and benefits of adoption by co-related agents.
Two main distinctions are evident between the disequilibrium and equilibrium approaches: their implicit assumption about the availability of information and their behavioural content. In disequilibrium models, information is asymmetric and adoption is driven by information flows; in equilibrium models information is perfect and adoption is driven by benefit-cost ratios. Despite these differences, most authors have viewed the equilibrium and disequilibrium models of diffusion as complementary rather than conflicting approaches and have modelled both simultaneously [13, 17]. We also adopt this approach but note that in the case of general practices, information about new drugs is likely to be readily available to GPs through pre-release marketing. Indeed, four of the drugs we consider here were prescribed by Irish GPs in the same month they entered the Irish market, and the diffusion curves we observe for each of the drugs exhibit relatively rapid early adoption again suggesting the general availability of information and the potential relevance of equilibrium models.
Recent literature has also focused on learning by using effects when modelling adoption decisions. McWilliams and Zilbermanfr [18] highlight three types of “learning” that play an important role in the adoption and demand for new technologies. “Learning by Doing”, as described by Rosenberg [19], which is producers of a new technology learning over time how to make the technology more cheaply and/or to improve the quality of technology. “Learning by Doing” explains the supply of technology, and so is not pertinent to this study. The second type of learning is “Learning by Using”, which Rosenberg [19] describes as the effect of the users of a given technology increasing their productivity over time as they learn how to better use this new technology. McWilliams and Zilbermanfr [18] highlight how economists use learning by doing and learning by using interchangeably, however, there is a clear supply and demand side distinction between the two [19]. Therefore, we will also refer to this particular learning process whereby a firm increases its’ stock of knowledge based on its’ previous experience with technologies as learning by using. McWilliams and Zilbermanfr [18] present the third type of learning as the ‘traditional’ form of learning which involves potential adopters gathering information about the performance of the new technology. These epidemic ‘learning’ effects, which have previously been discussed, capture a firm’s ability to absorb knowledge from external sources and exploit it for its own innovative activities.
Previous studies report that learning from the adoption of complementary technologies, complementarities between various functional groups of the same technology and the use of previous technology vintages impact on adoption decisions [18, 20–23]. In general, these studies consider learning by using effects to be within the context of the equilibrium model of adoption; specifically rank effects. The extent to which a firm has adopted previous technologies and learned from that experience can be considered a firm characteristic that distinguishes firms from each other.
To date, much of the empirical literature examining the adoption of new prescription drugs has focused on physician’s personal adoption decisions and the information asymmetries influencing these choices [24]. Kozyrskyj et al. [25], for example, conducted a study on newly marketed drugs in Canada to determine whether early prescribers had different socio-demographic or professional characteristics to later adopters. In two of the four drugs they examined, Kozyrskyj et al. [25] found that early prescribers were more likely than later adopters to be hospital affiliated. Adoption times for new drugs were also shorter for partnerships than single-handed practices [26, 27]. This may reflect the idea that the larger the number of patients in a practice, the more likely the GP is to see a patient who might be a candidate for a new drug [28, 29]. However, Williamson [26] puts forward a different explanation suggesting that the longer a doctor spends in discussion with his or her doctor colleagues, the more likely s/he is to be an early adopter.
Other studies have highlighted the potential importance of other practice characteristics on the timing of first adoption emphasising that most prescribing decisions are multi-factorial. For example, Tamblyn et al. [28] examined the initial utilisation rate of new prescription drugs among physicians in Quebec and found lower utilisation rates of new drugs among physicians with a rural or remote practice location. The same study also reports lower utilisation rates of new drugs among female physicians and those with a higher proportion of elderly patients in their practice who might, perhaps, be less receptive to ‘new’ drugs. Similarly, Prosser et al. [1], in a qualitative study of the factors influencing GPs’ uptake of new drugs in the North–West of England, emphasise the importance of biomedical factors on drug choice along with recommendations from hospital consultants and patient requests.
While previous drug adoption studies have not specifically modelled learning-by-using effects, they have examined whether experience with other drugs impacts on a GPs’ prescribing decisions. Florentinus [30], in a qualitative study examining the adoption of five drugs by a sample of approximately 100 GPs in the Netherlands, reports that a GP’s decision to prescribe a new drug was very much drug dependent and, therefore, did not identify GP characteristics specific to early drug adoption or an ‘innovator’ category of GP. Kozyrskyj et al. [25], in an examination of four newly marketed drugs, found that early prescribers of one new drug were not early prescribers of all four medications. They report that attributes of a drug, such as perceived efficacy and improvement over existing alternatives, impact early use. Steffensen et al. [27] also report that their data did not indicate a universal innovator or laggard with respect to adoption of all five studied drugs. Their data indicate that the shape and slope of the curve are both dependant on physician and drug characteristics. Similarly, Dybdahl et al. [29] report that early adoption of one type of drug is not associated with early adoption of another. In fact, in an examination of GPs’ adoption of new drugs and previous prescribing of drugs belonging to the same therapeutic class, Dybdahl et al. [29] find no consistent association between GPs’ level of drug prescribing and their adoption of new drugs of the same therapeutic group. Therefore, the empirical evidence suggests that GPs’ previous prescribing decisions do not impact on their decision to prescribe a new drug for the first time.
The commercial and prescribing autonomy of Irish GPs suggests the potential for both equilibrium—i.e. market—and disequilibrium—i.e. informational—influences on the timing of prescribing innovation. Previous studies of prescribing innovation by GPs—based almost solely in the disequilibriumm tradition—have also emphasised the potential importance of informational effects. The justification for the potential importance of rank effects—reflecting the impact of the heterogeneity of general practices on the costs and benefits of adoption—is also clear.Footnote 9 Nursing and clerical support, for example, would be expected to reduce time to adoption, whereas increasing GP age would be expected to increase time to adoption. Given the nature of prescribing decisions—i.e. a GP prescribes a drug to a patient to treat a medical condition—we do not anticipate significant stock and order effects. That is, we do not expect that the perceived benefits from adopting a new drug for the first time would be diminished by the stock of previous adopters (stock effect), or that adopting a new drug later in the adoption order would adversely impact on the benefit from adoption (order effects). However, health economics literature frequently profiles GPs as economic agents who respond to economic incentives and are aware of the competitive structure of their environment [32, 33], so there may be some evidence of strategic interaction.
Data and methods
Our empirical analysis is based on two matched databases: the GMS Prescribing Database and the GP Characteristics Database. The GMS Prescribing Database derives from the administration of the GMS Payments Board which provides reimbursement to primary care contractors for the provision of health services to GMS patients. It contains patient-level data for every prescription filled in the Health Service Executive (HSE) South, South–East and North–East regions on a monthly basis for the period October 1999–March 2004.Footnote 10 Items included in the GMS database for each prescription include a GP identifier, dispenser identifiers, drug details which follow the anatomical therapeutic chemical (ATC) classification system and the quantity prescribed. Each monthly datafile in the GMS database contains details of between 600,000 to 1,000,000 individual prescriptions for a total of 1,137 different drugs. The original GMS patient-level database was restructured for our analysis to provide data on whether or not each GP prescribed each drug in each of the 54 months covered by the data. This allowed us to identify the date of first adoption of each drug by each GP and to construct adoption curves for each drug reflecting the proportion of GPs prescribing each drug each month. In general, these adoption curves follow one of three patterns; a relatively constant proportion of GPs prescribing a drug; an increase in the proportion of GPs prescribing each drug; or, a decrease in the proportion of GPs prescribing the drug. Almost 70% of the 1,137 drugs represented in the GMS database were prescribed by a similar proportion of GPs over the entire 54 months covered by the database. These are likely to be established drugs for which no alternative became available during the sample period. The level of adoption of 214 drugs (approx. 18%) increased over the time period, with the level of adoption of 134 drugs (approx. 11%) decreasing over the same period.
Here, our focus is on the factors that shape the timing of GPs’ prescribing innovations, i.e. the date at which they first adopt a new prescription drug. We therefore focus on a group of six drugs that have increasing adoption curves and that operate on different physiological organs or systems. Using this diverse range of drugs should help to eliminate any potential inter-relationships between adoption patterns which might stem from individual GPs having a particular interest in a certain therapeutic area or medical condition.
The drugs we consider are as follows: (1) esctialopram an antidepressant used in the treatment of major depressive episodes, panic disorder with or without agoraphobia, social anxiety disorder, generalised anxiety disorder and obsessive–compulsive disorder; (2) esmoprazole a proton pump inhibitor used in the treatment of active duodenal ulcer, active benign gastric ulcer, symptomatic erosive or ulcerative gastro-oesophageal, reflux disease (GORD), gastro-oesophageal reflux disease long-term management (GORD Maintenance), symptomatic treatment of moderate to very severe gastro-oesophageal reflux disease (symptomatic GORD), and Zollinger-Ellison Syndrome; (3) rofecoxib a nonsteroidal anti-inflammatory drugs (NSAID), used to reduce pain, inflammation, and stiffness caused by osteoarthritis, rheumatoid arthritis and certain forms of juvenile rheumatoid arthritis, to manage acute pain in adults, to treat migraines, and to treat menstrual pain; (4) desloratadine an antihistamine, is used to relieve the symptoms of allergic rhinitis (inflammation of the nasal passages caused by an allergy, for example, hay fever or allergy to dust mites) or urticaria (a skin condition caused by an allergy, with symptoms including itching and hives); (5) nicotine is used for the treatment of tobacco dependence by relieving nicotine craving and withdrawal symptoms, thereby facilitating smoking cessation in smokersFootnote 11; and (6) drospirenone and oestrogen is a hormonal contraceptive which acts on the endocrine system.
Under European and Irish legislation, all medicinal products must be authorised before being marketed. Medicinal products marketed in Ireland must be authorised by the Irish Medicines Board (IMB). Table 1 provides information on the date of authorisation of these six drugs to the Irish market. Once authorised by the IMB, Irish GPs can prescribe these drugs to both public and private patients. However, pharmacists can only dispense drugs assigned a GMS code to public patients free of charge. This information is also provided in Table 1, along with the date when the first prescription for each drug was written by a GP(s) in the sample. For instance, Escitalopram was first licensed in Ireland on the 21st October 2002 and received a GMS code on 1st November 2002 (Table 1).
Diffusion curves for each of these drugs are included in Fig. 1. Escitalopram was first prescribed in November 2002, with approximately 10% of the sample prescribing escitalopram to their patients. From the time of first adoption, levels of adoption increased rapidly and by March 2004 (the last month of the sample period), the level of adoption was approximately 70% (Fig. 1a). Similar diffusion curves are evident for esmoprazole (Fig. 1b), rofecoxib (Fig. 1c) and drospirenone and oestrogen (Fig. 1d) where the proportion of GPs prescribing the drugs increased steadily throughout the sample period. As expected with an antihistamine, we see a marked seasonal pattern to the proportion of GPs prescribing desloratadine with up to 70% of GPs prescribing it during the summer months, and lower prescribing levels during the winter months (Fig. 1e). The diffusion curve for nicotine also displays a seasonal pattern with more GPs prescribing this drug at the beginning of the calendar year.Footnote 12
a Proportion of GPs prescribing Escitalopram—October 1999–March 2004. b Proportion of GPs prescribing Esomeprazole—October 1999–March 2004. c Proportion of GPs prescribing Rofecoxib—October 1999–March 2004. d Proportion of GPs prescribing Desloratadine—October 1999–March 2004. e Proportion of GPs prescribing Nicotine—October 1999–March 2004. f Proportion of GPs prescribing Drospirenone and Oestrogen—October 1999–March 2004
A notable feature of each of these drugs is the extremely short time period from authorisation under the GMS scheme and their prescription by Irish GPs to their patients. This very rapid rise in the initial adoption of each new drug is also evident in the drug adoption curves (Fig. 1a–f) and is reported in previous literature [29, 30, 34]. This differs from the slower initial adoption which characterises most new technologies [13, 35, 36] and may be a result of intensive pre-release marketing by pharmaceutical companies.
The variables reflecting the timing of GPs’ prescribing innovations for the six drugs we consider form the dependent variables for our econometric analysis. We also derive a range of other independent variables from the GMS Prescribing Database to reflect epidemic or non-equilibrium effects, stock and order effects on prescribing innovation. We anticipate, for example, that GPs which are already prescribing a wide range of drugs—i.e. have a broad prescribing portfolio—may be better informed about drug options. This may influence their access to information on new drugs—an epidemic effect—potentially reducing their time to adoption. To reflect this possibility, we create a prescribing portfolio variable defined as the range of drugs prescribed by each GP as a percentage of the total number of drugs being prescribed by all GPs. This variable was constructed from the June 2001 GMS Prescribing Database to provide consistency with the 2001 GP Characteristics Database. In the GMS Prescribing Database for June 2001, a total of 874 different drugs were prescribed by GPs, with each GP prescribing on average 25% of these drugs. The broadest prescribing portfolio of any GP was 45% of all drugs prescribed (Table 2).
Previous studies report conflicting evidence in relation to stock and order effects. Some studies have found no evidence of such stock and order effects [13], some have found mixed evidence of such effects [14, 22], and others have chosen not to include variables capturing these effects in their models [37, 38]. While there is conflicting evidence of such effects, we do include them in the model particularly as they have been found in adoption studies of multiple technologies [20, 22]. A priori, it is difficult to have definitive expectations as to the outcome of their inclusion in the models. To capture potential order effects, we create an order variable for each of the six drugs. Each order variable takes a value of one where a GP was among the first adopters in at least one of the other five drugs being examined.Footnote 13 This variable may in fact capture cross-technology effects. A stock effect variable was also constructed for each of the six drugs. This is defined as the cumulative percentage of GPs who had adopted the drug so this variable is time-variant and is intended to reflect the potential benefits of adopting a new drug at each point in time (Table 2).
In the GMS Prescribing Database, each GP has a unique numerical identifier which is also included in the GP Characteristics Database. These identifiers were used to match each GP’s prescribing innovations to their background characteristics in the GP Characteristics Database. Compiled in 2001—approximately the middle of the time period covered by prescribing data—the GP Characteristics Database provides GP and practice characteristics for 625 GPs in the HSE South, South–East and North–East regions. This sample of GPs comprises almost a quarter of the GP population in Ireland and provides this study with time-invariant GP and practice characteristics variablesFootnote 14 (Table 2). For example, in 2001, 58 and 79% of GPs in the sample worked in a practice with a nurse and secretary respectively while 12% of GPs worked in a dispensing practice. We assume that each of these factors would have a positive impact on the benefit-cost ratio from prescribing innovation and will therefore have a negative effect on the time to innovation. GP age may also have an effect on time to adoption. As in previous studies, we anticipate this effect to be positive, i.e. older GPs will be slower to adopt new drugs. Other practice characteristics may be shaping GPs access to information about new drugs. In particular, 12% of GPs in this sample were in receipt of a rural practice allowance, as they live and practice in an area with a population of less than 500 people. GPs in rural practices are perhaps less likely to have frequent contact with colleagues or drug company representatives.
In addition to these GP and practice characteristics, the GP Characteristics Database also contains variables identifying whether GPs were beneficiaries from the Indicative Drug Treatment Scheme (IDTS). This initiative, intended to reduce overall prescribing costs, provided incentives for GPs able to reduce their prescribing costs and receive a percentage of the savings made to invest in their practice. Targets were calculated based on their previous year’s prescribing costs, controlling for the age and sex of the patients.Footnote 15 GPs were placed in one of three categories, which indicated the percentage of savings they were entitled to as a result of meeting drug costs targets. Thirty-seven per cent of GP’s previous years’ prescribing costs were less than 95% of the national age-related average costs and qualified for 60% of any savings made due to meeting targets. Twenty-four per cent of GPs qualified for 50% of any savings made due to meeting targets. A further 39% of GPs qualified for 40% of any savings made due to meeting targets. In each of these categories, the remaining savings were made available to the local health board. A priori it is difficult to anticipate how the Indicative Drug Treatment Scheme would influence prescribing innovation. GPs seeking to reduce prescribing costs in order to benefit from the scheme might delay prescribing new—and possibly more costly—drugs. Alternatively, if new drugs were more cost effective than existing treatments, the IDTS might actually encourage prescribing innovation.
To model the time to adoption or prescribing innovation for each of the six drugs, we use duration analysis. This approach allows us to develop a multivariate model for time to adoption as well as allowing for the conditional nature of adoption decisions due to potential stock effects [38]. The aim of duration analysis is to identify those factors that have a significant effect on the length of a spell and the dependent variable therefore measures the time elapsed before an event occurs [14]. In our analysis, the dependent variables therefore measure the time elapsed before a drug is prescribed by a GP after the drug is first adopted by any GP in the sample. In other words, we are defining the length of a spell for a GP in the sample as the realisation of a continuous random variable, T, that has the following cumulative distribution function or failure function:
For example, the Accelerated Failure Time (AFT) model assumes a linear relationship between the log of (latent) survival time T and characteristics X:
where β* is a vector of parameters and z is an error term. An AFT regression coefficient relates proportionate changes in time to adoption to a unit change in a given regressor, with all other characteristics held constant [41].
The probability distribution of duration can be specified by the Weibull, exponential, log-logistic and log-normal distribution (Eq. 2). To identify the appropriate distribution in any specific application, specification tests can be used to determine which distribution best fits the failure time regressions. In line with previous studies [14, 42, 43], specification testing of the failure time models in this study included an examination of pseudo-residuals, or generalised residuals, log-likelihood scores and Akaike’s Information Criterion (AIC). These specification tests suggested that the log-logistic distribution was the best fit for five (esctialopram, esmoprazole, rofecoxib, desloratadine, nicotine) of the six failure time regressions and that the log-normal distribution was the best fit for the remaining failure time regression (drospirenone and oestrogen).
Two of the main benefits of duration models include the consideration of time and the capacity to control for unobserved heterogeneity in the analysis. Unobserved heterogeneity, or ‘frailty’ as it is called in the biomedical literature, eliminates the effects of unobserved characteristics that remain constant over time [44]. So in our study, unobserved heterogeneity may include characteristics, such as the number of GPs in a practice or the practice’s patient profile, which we could reasonably assume to be constant over the sample period.Footnote 16
Econometric results
A duration, or failure time model, is used to explain time to adoption as a function of the independent variablesFootnote 17,Footnote 18 Initial baseline models were estimated and are presented in Table 3 including a wide range of explanatory variables. Subsequently, in a ‘stepwise’ fashion, variables with z-statistics of less than |0.5| were excluded from the relevant failure time models. Our preferred models, with marginal effects reported, are given in Table 4. Comparison of Tables 3 and 4 suggests that the exclusion of a number of insignificant variables has little effect on coefficient values. When interpreting the results of a duration model, a negative marginal effect means a factor reduces duration, i.e. reduces the time to adoption [14].
In the models, we represent potential rank effects using a series of variables reflecting the characteristics of GPs and their practices. GP practices with a nurse have lower times to adoption than those without a nurse for two of the drugs examined. This finding is statistically significant at the 1% level for the anti-depressant and statistically significant at the 5% level for the hormonal contraceptive drug. However, it is worth noting that the size of the practice nurse effect is relatively small, in that time to adoption decreases by one to 2 weeks (0.25 and 0.56 of a month) for practices with a nurse in relation to these two drugs. Similarly, a decrease in time to adoption is reported for practices with a secretary in two of the six drugs. This finding is statistically significant at the 5% level for the antihistamine and at the 1% level for the hormonal contraceptive drug. Again, this is a relatively small effect with time to adoption decreasing by approximately 2 weeks (−0.50 and −0.58 of a month) for practices with a secretary in relation to these two drugs. These findings are in line with much of the literature which report organisation size and human capital impacting positively on the adoption of innovations [13, 14]. Also, as expected, GP age is found to have a statistically significantly positive effect on time to adoption in four of the drugs considered here (the anti-depressant, the antihistamine, the smoking cessation drug and the hormonal contraceptive). However, the size of this effect is again relatively small, with time to adoption increasing in the region of 0.1–0.4 of a month for each increasing year. Masters [46], following a systematic review of the literature, reports similar findings in relation to doctors and internet adoption, with adoption being greater among younger doctors. Meade et al. [47] in a study examining the factors affecting the use of electronic patient records by Irish GPs also report greater adoption of electronic patient records by younger GPs.Footnote 19
Results in relation to the dispensing practice variable are generally insignificant, although there is a statistically significant relationship between time to adoption of the hormonal contraceptive drug and being a dispensing practice. Time to adoption for this drug increases by approximately 3 weeks (0.72 of a month) if the practice dispenses medication. Finally, the effect of IDTS, which reflects the effect on time to adoption of receipts from drug cost savings, impacts on one drug, the antihistamine. Time to adoption decreases by a little less than 2 weeks for the antihistamine drug for practices eligible for 50% of savings from meeting prescribing targets and also for those practices that receive 60% of savings relative to those practices eligible for 40% of savings. It is worth acknowledging that the dispensing practice variable and the IDTS variables may also be capturing informational or experiential effects. Dispensing practices are usually located in isolated rural areas. The impact of a rural location on time to adoption is discussed in the next paragraph. The IDTS variables capture GPs that are willing to change their prescribing practices to meet budgetary targets and are learning and gaining experience from these prescribing decisions.
Epidemic effects are captured in the models specifically by the rural practice variable. An increase in time to adoption is reported for practices in receipt of a rural practice allowance for two of the drugs examined. This finding is statically significant at the 5% level for the antidepressant and hormonal contraceptive drugs, with time to adoption increasing by 0.2 and 0.9 of a month for rural practices. Tamblyn et al. [28] found similar results with lower utilisation rates of new drugs among physicians with a rural or remote practice location. Coleman et al. [24] report in the classic drug diffusion study where physicians’ decisions to prescribe a new antibiotic tetracycline were investigated that early adopters attend more out-of-town medical meetings that late adopters. While similar data are not available for this study, it is fair to suggest that GPs with practices in receipt of a rural practice allowance are less likely to be able to attend meetings and conferences than urban based GPs. Similarly, it is likely that such practices are visited less frequently by drug company representatives, which might be an important source of information for GPs in relation to prescribing decisions [3].
The portfolio breadth variable, which was constructed to capture learning-by-using effects, reveals a consistent effect. Across all six drugs and statistically significant at the 1% level, time to adoption decreases for GPs who prescribe drugs from larger portfolios. As demonstrated by the marginal effects for this variable, time to adoption decreases substantially for all six drugs for GPs who have larger prescribing portfolios. A percentage increase in a GPs portfolio decreases time to adoption of these drugs from three to ten and a half months. As discussed in the previous section, this relationship between portfolio size and time to adoption is nonlinear in relation to the nicotine drugs, suggesting a u-shaped relationship between portfolio breadth and time to adoption. Previous studies have highlighted that being an early adopter of one drug does not impact on subsequent adoption decisions [25, 27, 29]; however, our study highlights that the relative size of a GP’s prescribing portfolio significantly impacts on the decision to prescribe a new drug. It is also possible that our portfolio breadth variable could also be considered a proxy for practice size, as the more patients a GP sees the more likely they require a larger portfolio of drugs from which to prescribe. Previous studies have reported higher utilisation rates of new drugs for larger practices, as measured by practice volume [28].
In our duration models, potential order effects variables for each drug are represented by a dummy variable taking value one where a GP prescribed at least one of the remaining five drugs in the first 6 months after their first adoption. As expected, we see strongly statistically significant negative order effects for all of the six drugs. As is evident from Table 4, time to adoption decreases in all drugs for GPs who are deemed ‘first-movers’ in the other drugs being examined. In relation to four of the drugs (the antidepressant, the proton pump inhibitor, nicotine drugs and the hormonal contraceptive), time to adoption decreases by approximately one to 6 weeks for ‘first-movers’. The order effect is quite large in relation to the anti-inflammatory and antihistamine drugs with time to adoption decreasing by six and 8 months for ‘first-movers’, respectively. In standard terms, this suggests that some GPs are early adopters of new drugs in order to maximise the returns from that new adoption given anticipated future levels of adoption [13]. Previous literature has reported order effects in relation to the adoption of multiple technologies, where the technologies are complementary [20] or simultaneously adopted [22]. While the 6 drugs in this study are not complementary therapies, they were adopted over a similar time-period. A plausible explanation here is that some GPs, who for whatever reason, were early adopters of one drug, have learnt the benefits of early adopting and therefore tend to be early adopters of other drugs.
Finally, in our models, potential stock effects are represented by the proportion of GPs who had adopted a drug at any given point in time [13]. We find a positive effect (i.e. time to adoption increases as the stock of previous adopters increases) for five of the six drugs examined. As is evident from Table 4, for each percentage increase in the stock of previous adopters, time to adoption increases from six to 20 months for these five drugs. This result is somewhat counter intuitive as it is unlikely GPs have sufficient information or ability to correctly anticipate future adoption patterns. However, the stock of previous adopters in all 6 drugs over the time-period in question is high relative to the non-adopters. For instance, within the first year of the adoption of all 6 drugs, over half of GPs in the sample have adopted them; sometimes, this figure is greater than 70%. Therefore, given the rapid adoption rates of these drugs, it is perhaps not surprising that as the stock of previous adopters increases time to adoption increases for the remaining GPs (some of whom may remain non-adopters). Stoneman and Kwon [20] in a study of the adoption of complementary technologies also report evidence of stock effects.
In this paper, we examine the factors that lie behind the rapid adoption by Irish GPs of six prescription drugs following their launch in the Irish market. Our study highlights a range of commonalities across all of the drugs considered and suggests the importance of GP and practice characteristics in shaping prescribing decisions. We also find evidence of both equilibrium (strategic) and disequilibrium (or informational) effects on the timing of GPs’ prescribing innovations. Our evidence on rank effects, intended to capture the differential benefit-cost ratio of adoption by GPs with different characteristics, largely mirrors that of other studies. Practices with either a nurse or clerical support are more likely to be early adopters of new drugs as are younger GPs. We also find evidence that the IDTS, designed primarily to reduce prescribing costs, may also be having additional benefits by stimulating early adoption. However, it is important to note that in general, the size of these rank effects is relatively small in terms of reducing or increasing time to adoption.
More surprising perhaps is that we find strongly significant, and consistently signed, stock and order effects across five and six of the drugs considered respectively: GPs who have a track record of early adoption tend also to be early adopters of any new drug (order effect)Footnote 20; and, the larger the proportion of GPs which have already adopted a new drug the slower is subsequent adoption (stock effect). The standard interpretation of the stock and order effects in studies of new technology adoption by firms relates to the impact of the timing of adoption on the subsequent returns [13]. Here, given the commercial autonomy of Irish GPs, similar effects may be operating. Other potential, and observationally equivalent, explanations for these effects may relate more directly to information flows, a suggestion reinforced by the consistent epidemic and learning-by-using effects we also find. Prescribing innovation tends to be slower in rural practices and also among GPs with narrower prescribing portfolios.
The duration models used here enable us to consider a wide range of GP and practice effects on the timing of prescribing innovations. In fact, the innovation literature highlights the lack of panel data in relation to adoption of new innovations [17]. Three important limitations of our study are worth highlighting, however. First, a common idea in the literature is that new drugs diffuse into general practice through a two-step model with hospital consultants as the innovators and GPs as the followers. In other words, it is the consultant who initially prescribes the new drug and GPs repeat prescribe these drugs when the patient returns to the primary care setting. Florentinus’ [30] study of the adoption of new drugs in a Danish primary care setting, however, contradicts this two-step model. While acknowledging the influence of medical specialists in GPs’ prescribing decisions, Florentinus [30] finds that GPs themselves are responsible for a considerable amount of all early prescriptions for new drugs. Here, data restrictions mean that we are not able to control for the potential influence of hospital consultants on GPs’ prescribing decisions. However, of the six drugs examined, four (the antihistamine, the smoking cessation medication, the hormonal contraceptive and the antidepressant) are unlikely to be repeat prescriptions following an initial prescription by a hospital consultant. It is perhaps more likely that prescribing decisions for the proton pump inhibitor and the anti-inflammatory considered here may be more strongly influenced by hospital consultants’ initial prescribing decisions. Secondly, due to data restrictions, we do not control for the impact of advertising in relation to GPs decisions to adopt these six drugs. However, this is something to be considered in future research. Advertising noise or impact could be measured through a citation search in medical journals or ranking the market power of the pharmaceutical companies which initially released these drugs.
As discussed in the methodology section, an advantage of duration models is the ability to control for unobserved heterogeneity. However, our duration models did not fit when we attempted to control for observed heterogeneity.Footnote 21 Jenkins [44] acknowledges that the frailty models can be relatively ‘fragile’ in the statistical sense, as they can be relatively hard to fit particularly if the frailty variance is close to zero. Jenkins [44] highlights three sources of potential bias in ‘non-frailty’ duration models. Firstly there is potential to over-estimate the degree of negative duration dependence and under-estimate the degree of positive duration dependence. Secondly, the proportionate effect of a given regressor on the hazard rate may no longer be constant and independent of survival time. Thirdly, the estimate of a positive (negative) coefficient derived from the non-frailty model will underestimate (over-estimate) the ‘true’ estimate. Jenkins [44] also reports that the empirical literature generally confirms these theoretical propositions. However, he concludes that if a fully flexible specification of the baseline hazard function is used, then the magnitude of the biases in the ‘non-frailty’ model is diminished. While unobserved heterogeneity is likely to exist in these duration models, our explanatory variables differentiate between individual GPs well.
Conclusion
Our results clearly suggest that the adoption of new prescription drugs is not uniform across all GPs suggesting the potential for targeted intervention to stimulate prescribing innovation. For example, the fact that older GPs, and GPs practicing without the assistance of a nurse or secretary, are in general slower to adopt new drugs might suggest these groups as a specific target for support. Likewise, the significant learning effects we identify, captured by the rural practice allowance, portfolio breadth, stock and order effects variables, suggest the importance of GPs’ ability to obtain information on new drugs. Pharmaceutical companies and Continuing Medical Education (CME) meetings do provide information on new drugs. However, if policymakers want to influence the uptake of new drugs, whether new compounds to the market or generics of existing compounds, additional means of conveying information to remote GPs and GPs who do not prescribe from a large portfolio of drugs could be considered. Such policy initiatives need to be considered, however, both in the light of the potential benefits of the adoption of new drugs and their potential risks [30]. For instance, rofecoxib was first licensed in Ireland on the 12th November 1999 and by March 2004, almost three-quarters of GPs in our sample were prescribing rofecoxib to patients. Merck and Co Inc., who produced rofecoxib under the brand names Voixx and Ceoxx, voluntarily recalled the drug on September 30, 2004, amidst evidence that it drastically increased users’ risk of heart attack and stroke.
The GMS and GP Characteristics Databases provide a rich source of hard data in relation to Irish GPs and their prescribing patterns. Opportunities for future research include a similar analysis focusing on a number of drugs from the same therapeutic class, to determine whether the commonalties reported in the adoption of the drugs in this study are evident to the same or a greater extent when examining drugs prescribed for similar conditions. We would also like to examine GPs decisions to adopt complementary drugs. Such analysis would allow for an investigation for cross drug effects similar to those identified in multiple technology and complementary technology diffusion studies. We would also like to conduct a separate analysis on the adoption of drugs with a relatively high degree of pharmacological innovation compared to those with a relatively low degree of innovation.
Notes
Ireland has a low number of GPs per capita in comparison with other EU countries. It is estimated Ireland has approximately 52–56 GPs per 100,000 of the population. Countries such as Austria, France and Germany have over 100 GPs per 100,000. Irish GPs are, however, considered well paid in relation to their EU colleagues; Irish GPs are paid four times the GDP per capita value, a higher multiple than in the UK, Germany, the Netherlands, France and Sweden [5].
In Budget 2010, a new charge of 50% item was announced to be introduced in October 2010. This charge did not apply within the timeframe of this study.
GPs are remunerated for treating GMS patients on a capitation basis. The capitation fees are calculated based on the following factors: (1) a demographic factor designed to reflect differences in demands by various age and gender groups, and (2) a geographic factor designed to reflect the expenses incurred in visiting patients in various age/distance categories [5].
In 2008, the average income for a GP in Ireland with a GMS contract was €220,000 [8].
General practices are not obliged to display the price of a consultation, although an updated Guide to Professional Conduct and Ethics for Registered Medical Practitioners specifies that GPs can display prices. In 2009, the Competition Authority estimated that the average cost of a GP visit for a private patient is approximately €50–55 in urban areas, with slightly lower charges in rural areas [8]. The National Consumer Agency also reported a wide range of prices for GP visits, averaging at €51, with a minimum of €35 and a maximum of €70 [5].
Drugs authorised by the IMB do not automatically receive a GMS code, although most drugs do. This is discussed in more detail in Sect. 3.
We are concerned with the ‘prescribing innovation’, i.e. a GPs decision to prescribe a new drug for the first time rather than the ‘new drug’ innovation.
Irish general practices vary widely in size and personal characteristics with O’Dowd et al. [31] estimating that 35% of general practices were solo-practitioner practices, with the remainder comprising of two GP practices (30%), three GP practices (20%) or four or more GP practices (15%). Not all general practices have nursing and clerical support. 35% of practices employ a full-time nurse and 70% of practices employ full-time clerical assistance. Less than one in three practices employ a practice manager [31].
When a GMS patient gets a prescription from a GP, they fill it either in a pharmacy or, if their GP has a dispensing licence, at the GP practice. The medicine is dispensed free of charge to the patient and a duplicate of the prescription is sent by the dispenser to the GMS (Payments) Board for payment.
Nicotine drugs, nasal sprays and chewing gum, are also available to purchase without prescription.
This may reflect a ‘new year resolution’ effect as people seek support for giving up smoking.
Specifically, the order variables take a value of one where a GP first prescribed one of the other five drugs considered here in the first 6 months after its first adoption. Between 25 and 35% of GPs may be considered ‘first adopters’ and take a value of one in relation to these order variables.
Participation in the Indicative Drug Treatment Scheme was voluntary and GPs retained the right and obligation to prescribe as they considered necessary. No sanctions were in place for those GPs who failed to reduce costs.
In practice, and despite some experimentation, we found that our duration models did not converge when we attempted to control for unobserved heterogeneity. This issue has been noted in the literature [44] and we discuss the implications of this in the following section.
The data analysis and statistical software package Stata 11 is used to conduct the econometric analysis [45].
Given that not all GPs have adopted each drug by the end of the sample period, the data are right-censored. As a robustness check, we removed the non-adopters for each drug from the sample and ran the duration models individually. The same results as those reported were obtained. We are grateful to a referee for highlighting this point.
However, not all small business adoption studies report significant findings in relation to age, For example, Burton et al. [38] report no statistically significant relationship between age of a farmer and the adoption of organic horticultural technology.
Being an early prescriber of one drug in our data does predict early adoption of some drugs. However, it is not a strong predictor of being an early adopter of all drugs examined. For instance, no GP in the sample adopted all six drugs within the first 6 months of them being adopted. This contradicts the image of early adopters as being related to a general innovative predisposition. Therefore, it appears that a GPs decision to prescribe is heavily dependent on the new drugs in question [27, 34].
The Stata command ‘streg’ is used in our analysis. We included the ‘frailty’ option to control for unobserved heterogeneity.
References
Prosser, H., Almond, S., Walley, T.: Influences on GPs’ decision to prescribe new drugs—the importance of who says what. Family Pract. 20, 61–68 (2009)
Thistlehwaite, J.E., Ajjawi, R., Aslani, P.: The decision to prescribe: influences and choice. InnovAiT 3(4), 237–243 (2010)
Jones, M.I., Greenfield, S.M., Bradley, C.P.: Prescribing new drugs: qualitative study of influences on consultants and general practitioners. BMJ 323(7309), 378 (2001)
Rogers, E.M.: Diffusion of Innovations, 5th edn. Free Press, New York (2003)
Layte, R., et al.: Projecting the impact of demographic change on the demand for and delivery of health care in Ireland. In: Layte, R. (ed). ESRI, Dublin (2009)
Wren, M.-A.: Unhealthy State: Anatomy of a Sick Society. New Island, Dublin (2003)
Ireland: Primary Care: A New Direction. Government of Ireland, Dublin (2001)
Competition Authority: Competition in Professional Services. General Medical Practitioners. Competition Authority, Dublin (2009)
Thomas, S., Normand, C., Smith, S.: Social Health Insurance: Further Options for Ireland, pp. 1–45. Trinity College Dublin, Dublin (2008)
Carlsen, B., Glenton, C., Pope, C.: Thou shalt versus thou shalt not: a meta-analysis of GPs’ attitudes to clinical practice guidelines. Br. J. Gen. Pract. 57, 971–978 (2007)
Mason, A.: New medicines in primary care: a review of influences on general practitioner prescribing. J. Clin. Pharm. Ther. 33, 1–10 (2008)
Wathen, B., Dean, T.: An evaluation of the impact of NICE guidance on GP prescribing. Br. J. Gen. Pract. 54, 103–107 (2004)
Karshenas, M., Stoneman, P.L.: Rank, Stock, Order, and epidemic effects in the diffusion of new process technologies: an empirical model. RAND J. Econ. 24(4), 503–528 (1993)
Baptista, R.: Do innovations diffuse faster within geographical clusters? Int. J. Ind. Organization 18(3), 515–535 (2000)
Schumpeter, J.A.: Capitalism, Socialism and Democracy. Harper and Brothers, New York (1942)
Hall, B.: Innovation and diffusion. In: Fagerberg, J., Mowery, D., Nelson, R.R. (eds.) Handbook of Innovation. Oxford University Press, Oxford (2004)
Battisti, G., et al.: Inter and intra firm diffusion of ICT in the United Kingdom (UK) and Switzerland (CH): an internationally comparative study base on firm-level data. Econ. Innovation New Technol. 16(8), 669–687 (2007)
McWilliams, B., Zilbermanfr, D.: Time of technology adoption and learning by using. Econ. Innovation New Technol. 4(2), 139–154 (1996)
Rosenberg, N.: Inside the Black Box: Technology and Economics. Cambridge University Press, Cambridge (1982)
Stoneman, P., Kwon, M.-J.: The diffusion of multiple process technologies. Econ. J. 104(423), 420–431 (1994)
Colombo, M.G., Mosconi, R.: Complementarity and cumulative learning effects in the early diffusion of multiple technologies. J. Ind. Econ. 43(1), 13–48 (1995)
Stoneman, P., Toivanen, O.: The diffusion of multiple technologies: an empirical study. Econ. Innovation New Technol. 5(1), 1–17 (1997)
Arvantis, S., Hollenstein, H.: The determinants of the adoption of advanced manufacturing technology. Econ. Innovation New Technol. 10, 377–414 (2001)
Coleman, J., Katz, E., Menzel, H.: Medical Innovation: A Diffusion Study. Bobbs Merrill, New York (1966)
Kozyrskyj, A., Raymond, C., Racher, A.: Characterizing early prescribers of newly marketed drugs in Canada: a population-based study. Eur. J. Clin. Pharmacol. 63, 597–604 (2007)
Williamson, P.M.: The adoption of new drugs by doctors practising in group and Solo practice. Social Sci. Med. 9, 233–236 (1975)
Steffensen, F.H., Toft Sorensen, H., Olesen, F.: Diffusion of new drugs in Danish general practice. Family Pract. 16(4), 407–413 (1999)
Tamblyn, R., et al.: Physician and practice characteristics associated with the early utilisation of new prescription drugs. Med. Care 41(8), 895–908 (2003)
Dybdahl, T., et al.: Does the early adopter of drugs exist? a population-based study of general practitioners’ prescribing of new drugs. Eur. J. Clin. Pharmacol. 60, 667–672 (2004)
Florentinus, S.R.: New drugs in general practice: prescribing patterns and external influences. In: Utrecht Institute for Pharamacutical Devices, Utrecht (2006)
O’Dowd, T., O’Kelly, M., O’Kelly, F.: Structure of general practice in Ireland, 1982–2005. Irish College of General Practitioners and Trinity College Dublin, Dublin (2006)
Scott, A.: Economics of general practice. In: Anthony, J.C.J. (ed.) Handbook of Health Economic. Elsevier (2000)
Kann, I.C., Biorn, E., Luras, H.: Competition in general practice: prescriptions to the elderly in a list patient system. J. Health Econ. 29, 751–764 (2010)
Dybdahl, T., et al.: General practitioners’ adoption of new drugs and previous prescribing of drugs belonging to the same therapeutic class: a pharmacoepidemiological study. Br. J. Clin. Pharmacol. 60(5), 526–533 (2005)
Baptista, R.: The diffusion of process innovations: a selective review. Int. J. Econ. Bus. 6(1), 107–129 (1999)
Battisti, G., Stoneman, P.: The intra-firm diffusion of new process technologies. Int. J. Ind. Organization 23(1–2), 1–22 (2005)
Hollenstein, H., Woerter, M.: The decision to adopt internet-based E-commerce. An empirical analysis based on swiss firm-level data. In: KOF Working Paper. Zurich (2004)
Burton, M., Rigby, D., Young, T.: Modelling the adoption of organic horticulture technology in the UK using duration analysis. Aust J. Agricultual Resour. Econ. 47(1), 29–54 (2003)
Leahy, A., Wiley, M.: The Irish Health System in the 21st Century. Oak Tree Press, Dublin (1998)
Barry, M., et al.: Projecting the impact of demographic change on the demand for and delivery of health care in Ireland. In: Layte, R. (ed.) p. 178. Economic and Social Research Institute, Dublin (2009)
Jenkins, S.P.: Lessons on survival analysis. Available from. http://www.iser.essex.ac.uk/study/resources/module-ec968 (2005)
Greene, W.H.: Econometric Analysis, 5th edn. Prentice Hall, New Jersey (2003)
Kiefer, N.M.: Economic duration data and hazard functions. J. Eco. Literature 26(2), 646–679 (1988)
Jenkins, S.P.: Survival analysis. In: Unpublished Lecture Notes (2003)
StataCorp: Stata Statistical Software: Release 11. StataCorp LP, College Station, TX (2009)
Masters, K.: For what purpose and reasons do doctors use the internet: a systematic review. Int. J. Med. Informatics 77(1), 4–16 (2008)
Meade, B., Buckley, D., Boland, M.: What factors affect the use of electronic patient records by Irish GPs? Int. J. Med. Informatics 78(8), 551–558 (2009)
Acknowledgments
Valuable comments on earlier drafts were received from participants at the Irish Economic Association (IEA) Conference April 2010, the Health Economists Association of Ireland (HEAI) May 2010, the Health Economics Study Group (HESG) June 2010 and a number of New Staff Development Workshops, Department of Economics, University College Cork. Valuable comments were also received from two anonymous referees. We would like to thank Dr. Brendan McElroy for his generous assistance in relation to acquiring the prescribing and GP characteristics databases from the HSE’s Primary Care Reimbursement Service. Opinions and errors in the paper are the sole responsibility of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bourke, J., Roper, S. In with the new: the determinants of prescribing innovation by general practitioners in Ireland. Eur J Health Econ 13, 393–407 (2012). https://doi.org/10.1007/s10198-011-0311-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-011-0311-5
Keywords
- Prescribing innovation
- Equilibrium and non-equilibrium models of adoption
- General practitioners
- Ireland