Abstract
Objective
To analyse associations between indicators for adoption of new drugs and to test the hypothesis that physicians’ early adoption of new drugs is a personal trait independent of drug groups.
Methods
In a population-based cohort study using register data, we analysed the prescribing of new drugs by Danish general practitioners. Angiotensin-II antagonists, triptans, selective cyclo-oxygenase-2 antagonists and esomeprazol were used in the assessment. As indicators of new drug uptake, we used adoption time, cumulative incidence, preference proportion, incidence rate and prescription cost and volume. For each measure, we ranked the general practices. Ranks were pair-wise plotted, and Pearson’s correlation coefficient (r) was calculated. Next, we analysed the correlation between ranks across different drug classes.
Results
For all indicators, the general practitioners’ adoption of one group of drugs was poorly associated with adoption of others (r≤0.49), indicating that early adoption of one type of drugs is not associated with early adoption of another. For all drug groups, adoption time adjusted for practice size was only weakly associated with other indicators (r: −0.56 to −0.27). Indicators, based on cost and volume of drugs, were highly correlated (r: 0.96–0.99), and the others correlated reasonably well (r: 0.51–0.91).
Conclusions
Within drug groups, indicators of drug adoption, except for adoption time, correlate reasonably well. However, the theory that physicians’ early adoption of new drugs is a personal trait independent of the type of drug could not be confirmed. The notion of the early-drug-adopting general practitioner may be mistaken.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug expenditures increase rapidly in primary care, mainly because physicians adopt new drugs that are more expensive than those they intend to replace (old drugs) [1–3]. Although health authorities strive to reduce drug expenses, no intervention has yet proved to be consistently effective [4–6]. This lack of impact may partly be caused by the fact that most attempts to improve practice are based on insufficient knowledge about mechanisms responsible for adoption of new drugs. It is, for example, believed that there is a group of physicians who generally prescribe (adopt) new drugs early and that interventions should be tailored accordingly [7–14]. However, the theory that doctors can be grouped into adopter categories that are likely to share specific characteristics has, to our knowledge, not been challenged. We aimed to analyse associations among different indicators for adoption of new drugs and to test the hypothesis that physicians’ early adoption of new drugs is a personal trait independent of the type of drug.
Materials and methods
Data sources
We used data from the Odense University Pharmacoepidemiologic Database and the National Health Insurance (NHI) Register [15]. The Odense University Pharmacoepidemiologic Database comprises information on all prescriptions redeemed at pharmacies in the County of Funen (approximately 470,000 inhabitants), Denmark. For the selected drugs, we extracted information on all prescriptions issued from 1993 to 2001 to patients aged 20 years or older. Information includes date of redemption, the patients’ identity, age and gender, the brand, quantity and form of the drug and the identity of the prescriber (general practice, specialist or hospital department). All doctors in a general practice share the same prescriber identifier.
Approximately 97% of the Danish population is listed with a general practice. The tax-financed NHI covers general practitioners’ (GPs’) fees for visits and services and keeps records on the identity, age and gender of persons listed with each practice, as well as of the physicians. From the NHI Register, we extracted information on the number, age and gender of all patients listed with each practice during 1998–2001.
Selection of study drugs
We selected four groups of prescription drugs launched in Denmark from 1994 through 1999 (Table 1). All these new and more expensive drugs were marketed with the claim of having significant benefits over older alternatives. The selected drug groups were angiotensin-II-receptor antagonists for hypertension or heart failure, triptans for acute migraine attacks, selective cyclo-oxygenase-2 (COX-2) inhibitors for rheumatoid arthritis or osteoarthritis and proton-pump inhibitors for peptic ulcer or gastro-oesophageal reflux diseases.
Study period
The length of each study period was chosen to ensure that at least 95% of all practices had prescribed the new drug. The periods were 4 years for angiotensin-II-receptor antagonists, 2 years for triptans and 1 year for COX-2 inhibitors and proton-pump inhibitors. For each group of drugs, the first day of the study period was the day the first new drug in the group was released for reimbursement (Table 1).
Selection of study practices
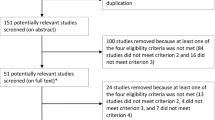
We used data from 191 practices that existed at some point in time during the period 1994–2001. They had a median practice size of 1439 patients (10–90th percentile: 851–3627). There were 121 solo and 70 group practices with a median practice size of 1168 (770–1613) and 2772 (1843–4592), respectively. For each study period, we selected practices established at least 1 year prior to the date that the first drug in a group was released for reimbursement. For each drug group, we excluded practices in which there had been a change of GP staff during the study period (Table 1). Among the 191 practices, 105 practices (30 partnership practices with 67 GPs and 75 single-handed practices) had the same GPs for the whole period.
Outcome measures
We selected measures commonly used in drug utilisation studies as well as measures based on individual patients’ drug use. For each practice and each drug group, we calculated the following six indicators or measures of adoption:
-
1.
Adoption time adjusted for practice size: the time from the first day of reimbursement until a GP within the practice issued the first prescription of a new drug to a patient who had never purchased the drug before. The time was adjusted for practice size by multiplying with the number of patients in the practice divided by the mean practice population size.
-
2.
Cumulative incidence of prescribing a new drug: the proportion of the listed patients prescribed a new drug. Only patients not previously treated with an old drug belonging to the group were included.
-
3.
Preference proportion for new drugs: the proportion of patients prescribed a new drug among patients prescribed either a new or an old drug for the first time.
-
4.
Rate of switching from an old to a new drug (switching rate): 1 year prior to the study period, we identified patients who used the older drugs. Among these, we identified first purchases of a new drug (switch). We calculated the switching rate as the number of switches divided by the person time elapsed from the start of the study period.
-
5.
Prescribed volume of new drugs: the number of defined daily doses [16] prescribed of new drugs during the study period per 1000 listed patients.
-
6.
Prescription costs of new drugs: the total drug expenditure for new drugs (in pharmacy retail price including value-added tax) during the study period per 1000 listed patients.
Indicators 2–6 were standardised according to age and gender of listed patients by means of direct standardisation to the total practice population, except for switching rate, where the reference population were users of an old drug.
Analyses
Within drug groups, we analysed the correlations between adoption indicators. For each indicator, we ranked the practices, made pair-wise plots of the ranks and calculated Pearson’s correlation coefficients (r). To outbalance the differences in practice size, we made the analyses both with and without weighting for practice size. Similarly, we analysed the correlations between each indicator across different drug groups.
Finally, for each group of new drugs, we analysed the time to the first prescription using practice type and size as covariates in a Cox proportional hazards model [17].
Results
For all adoption measures, there was considerable variation between practices, with wide 10–90th percentile ranges (Table 2).
The associations between adoption indicators within each drug group are presented in Table 3. Correlations between indicators were all statistically significant (P<0.05). Adoption time adjusted for practice size correlated poorly with other measures (r: −0.56 to −0.27, unweighted −0.55 to −0.20). Indicators, based on cost and volume, were highly correlated (r: 0.96–0.99, unweighted 0.96–0.99), and the remaining correlated reasonably well with r, ranging from 0.51 to 0.91 (unweighted 0.44–0.90).
The associations between adoption indicators across drug groups are presented in Table 4. The correlations varied with r, ranging from −0.08 to 0.49 (unweighted −0.10–0.45), and only 14 (unweighted 12) of 36 correlation coefficients were significantly different from zero (P<0.05). The highest correlation was between cumulative incidence of prescribing COX-2 inhibitors and proton-pump inhibitors with r=0.49 (unweighted 0.45) (Fig. 1).
The distribution of adoption times was asymmetrical, with a long upper tail representing late prescribers (Fig. 2). The apparent difference in adoption time between single-handed and partnership practices disappeared after adjustment for practice size. This was supported by the Cox regression model in which the diffusion of COX-2 inhibitors, not considering practice size, was fastest among partnership practices [hazard ratio 2.03 (95% confidence interval 1.46–2.82)]. Including practice size as covariate in the model reduced the difference between single-handed and partnership practices [hazard ratio 1.14 (0.66–1.99)], and practice size had a positive influence upon adoption time [hazard ratio 1.35 (1.08–1.67) for an increase of 1000 listed patients]. The same effects were present for the other drug groups.
Discussion
The results of our study suggest that most indicators of drug adoption, except for adoption time, are reasonably well correlated within the individual drug groups. However, adoption indicators are not correlated across drug groups, which may indicate that the notion of the early-drug-adopting GP may be mistaken.
These results, however, should be considered in relation to the strengths, weaknesses and limitations of the study. Many studies of drug prescribing are hampered by incomplete data on drug use. We had complete data on individual patients’ drug use for more than a decade for all inhabitants in a well-defined area [15]. Data are collected automatically in the pharmacies, and health care providers as well as pharmacies have an incentive to provide complete information, because their income depends on it. Previous studies indicate that less than 0.5% of all reimbursed prescriptions are redeemed at pharmacies outside the county [15]. This enabled us to make accurate estimates of GPs’ prescribing while distinguishing between initial prescriptions and renewals and excluding prescriptions made by other doctors (e.g. in hospitals).
We used patients’ purchases of drugs as a proxy for GPs’ prescribing. Patients’ failures to redeem a prescription—“primary non-compliance” —may, therefore, bias the results. Previous studies, however, indicate that non-redemption rates are relatively low on Funen [18].
By excluding general practices with change of GP staff during study periods, we restricted the study to about 80% of all GPs who practiced on Funen during each study period (Table 1). This, however, was a deliberate choice that allowed us to exclude changes in GP staff as explanation for any of the results. Consequently, the findings may not be representative of young doctors who had recently joined a general practice. However, other studies indicate that this would only be a small problem, since age does not appear to be associated with early adoption [7, 14].
Previous studies indicate that adoption time for new drugs is shorter for partnership than single-handed practices [11, 14]. However, they did not adjust for the number of patients in practice. In our study, after adjustment for practice size, there was no earlier adoption in partnership practices. A simple explanation might be that the larger the number of patients in a practice, the more likely it is to see a patient who might be a candidate for a new drug.
Adoption time, unlike the other indicators, is determined by one single event (the first prescription of a new drug). There is a substantial difference in making the decision to prescribe a new drug for the first time ever and to prescribe the drug routinely. This may explain the poor correlation between adoption time and all other indicators. Small sample variation may be one reason why we did not find a perfect correlation between the epidemiological measures of adoption. However, there were only modest increases of r when weighting for practice size, suggesting that there are other causes. Unequal distribution of patients’ health problems may be a confounder. Though we adjusted for differences in the distribution of patients’ age and sex in each practice, we did not have access to data concerning the co-morbidity of the patients. Future studies should include information on the diagnosis of included patients. Another reason for the differences between adoption indicators may be that the indicators are likely to capture different aspects of adoption. For example, to initiate treatment for a patient with a new drug is different than switching a patient from a well-tolerated treatment to a new drug. The issue of measuring different aspects of adoption should be addressed in future studies.
The term “early adopter” is frequently used in the literature on innovation and diffusion of new technologies. Rogers uses categories such as “innovators”, “early adopters”, etc., down to “laggards” [7]. The notion that early adoption is a personal characteristic is prevalent in the literature on drug prescribing as well. Haines and Donald [10] state that marketing of pharmaceuticals is tailored according to characteristics of the target audience. In a review paper, Groves et al. [11] use the term early adopters and propose that formulary committees target their resources “at those physicians who are more likely to be laggards”. While the literature on adoption of new drugs seems to imply that some doctors are early adopters and others not, our results would indicate that doctors who adopt one new drug early may adopt others late. This was the case whether we used adoption time or one of the other adoption measures. Steffensen et al. [14] also concluded that being an early adopter is not consistent over drug groups. However, they used adoption time only for quantifying new drug uptake. These results do not necessarily mean that adoption of new drugs is a random process, but rather that it varies across doctors, depending on the drug in question and other factors.
If the findings in this study reflect a general phenomenon, it would mean that the research into adoption of new drugs should be directed not only towards doctor characteristics but also towards the interaction between these characteristics, the drug in question, patient case mix and possibly other factors. Even though this study was not directly exploring the mechanisms responsible for adoption, it may have implications for health policy in that interventions aimed at influencing prescribers are not likely to be effective if they are based on the notion of the universal “early adopter”. They might only be successful if they target physician groups that are early adopters of the drug or the drugs in question.
In conclusion, for each group of drugs, there is a reasonably good correlation between various indicators of drug adoption except for time until first prescription of a new drug. We could not confirm the theory that physicians’ early adoption of new drugs is a personal trait independent of drug types.
References
Department of Health (2003) Delivering the NHS plan—expenditure report. Department of Health publications, London
The National Institute for Health Care Management Research and Educational Foundation (2001) Prescription drug expenditure 2000: the upward trend continues. The Institute, Washington, DC
The National Institute for Health Care Management Research and Educational Foundation (2002) Changing patterns of pharmaceutical innovation. The Institute, Washington DC
Pearson SA, Ross-Degnan D, Payson A, Soumerai SB (2003) Changing medication use in managed care: a critical review of the available evidence. Am J Manag Care 9(11):715–731
NHS Centre for Reviews and Dissemination (1999) Getting evidence into practice. Effective Health Care, University of York, York
Granados A, Jonsson E, Banta HD, Bero L, Bonair A, Cochet C et al (1997) EUR-ASSESS project subgroup report on dissemination and impact. Int J Technol Assess Health Care 13(2):220–286
Rogers EM (1995) Diffusion of innovations. The Free Press, New York
Coleman JS, Katz E, Menzel H (1966) Medical innovation: a diffusion study. The Bobbs-Merrill Co., Indianapolis
Lomas J (1994) Teaching old (and not so old) Docs new tricks: effective ways to implement research findings. In: Dunn EV et al (eds) Disseminating new knowledge and having an impact on practice. Sage Publication, Newbury Park
Haines A, Donald A (1998) Making better use of research findings. BMJ 317:72–75
Groves KEM, Fanagan PS, MacKinnon NJ (2002) Why physicians start or stop prescribing a drug: literature review and formulary implications. Formulary 37:186–194
DeCherney GS (1999) Accelerating acceptance. Physician Exec 25:32–38
Moulding NT, Silagy CA, Weller DP (1999) A framework for effective management of change in clinical practice: dissemination and implementation of clinical practice guidelines. Qual Health Care 8:177–183
Steffensen FH, Sorensen HT, Olesen F (1999) Diffusion of new drugs in Danish general practice. Fam Pract 16:407–413
Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44:445–448
WHO Collaborating Centre for Drug Statistics Methodology (2002) Guidelines for ATC classification and DDD assignment. WHO Collaborating Centre, Oslo
Hosmer DW, Lemeshow S (1999) Applied survival analysis: regression modelling of time to event data. Wiley, New York
Sondergaard J, Andersen M, Vach K, Kragsrup J, Maclure M, Gram LF (2002) Detailed postal feedback about prescribing to asthma patients combined with a guideline statement showed no impact: a randomised controlled trial. Eur J Clin Pharmacol 58:127–132
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00228-005-0899-4
Rights and permissions
About this article
Cite this article
Dybdahl, T., Andersen, M., Søndergaard, J. et al. Does the early adopter of drugs exist? A population-based study of general practitioners’ prescribing of new drugs. Eur J Clin Pharmacol 60, 667–672 (2004). https://doi.org/10.1007/s00228-004-0797-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0797-1