Abstract
In this position review, we propose to establish a path for replacing the empirical classification of tinnitus with a taxonomy from precision medicine. The goal of a classification system is to understand the inherent heterogeneity of individuals experiencing and suffering from tinnitus and to identify what differentiates potential subgroups. Identification of different patient subgroups with distinct audiological, psychophysical, and neurophysiological characteristics will facilitate the management of patients with tinnitus as well as the design and execution of drug development and clinical trials, which, for the most part, have not yielded conclusive results. An alternative outcome of a precision medicine approach in tinnitus would be that additional mechanistic phenotyping might not lead to the identification of distinct drivers in each individual, but instead, it might reveal that each individual may display a quantitative blend of causal factors. Therefore, a precision medicine approach towards identifying these causal factors might not lead to subtyping these patients but may instead highlight causal pathways that can be manipulated for therapeutic gain. These two outcomes are not mutually exclusive, and no matter what the final outcome is, a mechanistic-driven precision medicine approach is a win-win approach for advancing tinnitus research and treatment. Although there are several controversies and inconsistencies in the tinnitus field, which will not be discussed here, we will give a few examples, as to how the field can move forward by exploring the major neurophysiological tinnitus models, mostly by taking advantage of the common features supported by all of the models. Our position stems from the central concept that, as a field, we can and must do more to bring studies of mechanisms into the realm of neuroscience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tinnitus is defined broadly as a sound perception in the absence of an acoustic event, and is experienced by up to 15 % of the general population (Adams et al. 1999). Of the 40–50 million people in the USA with tinnitus, approximately 10 million seek medical attention (Seidman and Jacobson 1996) and 2.5 million of these are considered disabled by tinnitus due to its persistence, intensity, and the individual’s reaction to it (Shargorodsky et al. 2010). Tinnitus is the highest service-connected (SC) disability with over 1.2 million veterans suffering from it. Tinnitus is also the most prevalent SC disability amongst new compensation recipients, with 140,288 new veterans entering this pool in fiscal year 2016 (https://www.benefits.va.gov/REPORTS/annual_benefits_report.asp). Despite the high personal and financial cost of tinnitus, currently there is no available cure for tinnitus.
What does it mean to cure tinnitus? Approaches have proceeded from the logical premise that the symptomatic aspects of the percept should be rendered subclinical. Towards this end, approaches have been devised for quantifying reactions to tinnitus, characterizing the psychophysical properties of the percept and measuring the perceived impact on quality of life. However, the large within-subject variability in the psychophysical measures has contributed to the conclusion that valid and reliable ways need to be established for objective assessment of the perception of tinnitus. This limitation has not prevented the design of interventions to mitigate the various symptoms and decrease self-perceived handicap from tinnitus, with the goal to facilitate normal functioning and prevent significant impairment to quality of life. Although progress has occurred in mitigating the reaction to tinnitus, there is not a proven method to permanently eliminate or even reduce the perception of tinnitus.
The contemporary Clinical Practice Guideline for Tinnitus is empirical (Tunkel et al. 2014), distinguishing only primary tinnitus, “which may or may not be associated with sensorineural hearing loss,” and secondary tinnitus, “associated with a specific underlying cause other than sensorineural hearing loss or an identifiable organic condition.” These definitions are superficial and unclear and, as a result, no pharmaceutical or other treatments are recommended from an evidence-based perspective.
In this review, we propose to establish a path for replacing the empirical classification of tinnitus with a taxonomy from precision medicine. The goal of a classification system is to understand the inherent heterogeneity of individuals experiencing and suffering from tinnitus and to identify what differentiates potential subgroups. More importantly this differentiation will reveal what the members of a subgroup share in common based on the network, cellular, and molecular properties of their peripheral and central auditory and non-auditory networks involved in tinnitus. As such, this classification requires the understanding of the underlying mechanisms of tinnitus and will ultimately lead to a mechanistic-driven personalized medicine approach to the care of patients with tinnitus.
Is the Clinical Classification of Tinnitus Meaningful From a Neuroscience Point of View?
Diagnoses such as tinnitus, vertigo, fibromyalgia, and headache are based strongly upon subjective reports by patients. Based on the Clinical Practice Guideline for Tinnitus (Tunkel et al. 2014), if tinnitus is associated with a comorbid condition, it is relegated as a symptom in that diagnosis and treated accordingly as secondary tinnitus. If otherwise unexplained, it is considered as an idiopathic disorder to be treated in its own right. Thus, the patient with primary tinnitus is defined by symptom reports with no other explanation. Henry (2016) distinguishes functionally between an auditory sensorineural or neural origin as primary tinnitus and a somatic origin as secondary tinnitus. The somatic component may include pulsatile tinnitus from arteries and sensitivity to muscular, skeletal, or joint noises from the head; it also could include the rare condition of objective tinnitus, when the sound is discernable to an observer. This distinction seems ambiguous from a neural network perspective because multisensory integration occurs throughout the auditory pathways. For example, the spinal trigeminal nucleus projects extensively to the cochlear nuclei and to the inferior colliculus (Haenggeli et al. 2005; Zhou and Shore 2004, 2006). Because of multisensory integration in auditory pathways, the justification for using auditory versus somatic contributions as distinguishing features of different forms of tinnitus is questionable, further suggesting the need for a mechanistic approach for tinnitus classification.
Tinnitus Is a Disorder of Auditory Perception
In contemporary terminology, disorders of auditory perception include tinnitus, hyperacusis, phonophobia, misophonia, and polyacusis.
Hyperacusis designates both a decreased tolerance to sound in general and a specific dislike or sensation of discomfort or pain upon exposure to sounds above a given intensity (Baguley 2003; Tyler et al. 2014; Baguley and McFerran 2010). It is frequently comorbid with tinnitus and the patients with both disorders report a higher prevalence of onset-related triggers or events, headaches, association with stress, temporomandibular joint complaints, neck pain, and vertigo than patients reporting tinnitus alone (Schecklmann et al. 2014). Tyler et al. (2014) made the unifying proposition that hyperacusis be viewed as a general category of heightened sound sensitivity, which can be expressed in individuals as “loudness hyperacusis,” “annoyance hyperacusis,” “fear hyperacusis,” and “pain hyperacusis.”
Phonophobia designates the sensitivity to sound that is often associated with migraine. It is of interest to probe the auditory features of migraine-associated sound sensitivity to better define migraine-related hyperacusis.
The other disorders of auditory perception are more stimulus- or context-specific. Misophonia is a term for a dislike of particular sounds in specific contexts; the term “selective sound sensitivity syndrome” also has been proposed for this condition (Jastreboff and Jastreboff 2015; Møller 2010). Polyacusis and diplacusis refer to the perception of more than one pitch when the same stimulus frequency is presented binaurally (Corliss et al. 1968). For comprehensiveness, musical hallucinations (Kumar et al. 2014) and auditory verbal hallucinations in the absence of psychiatric disorders (de Leede-Smith and Barkus 2013; Johns et al. 2014) should be included in disorders of perception that may share neural substrates with tinnitus.
The high comorbidity between tinnitus and hyperacusis has motivated comparisons and speculation about both common underlying features and differential mechanisms, with elevated central gain as a feature of hyperacusis (Schecklmann et al. 2014; Sheldrake et al. 2015; Knipper et al. 2013). However, there may not be major differences in central sensory processing between hyperacusis and tinnitus. Specifically, Hébert et al. (2013) demonstrated convincingly that the properties of enhanced auditory sensitivity in ears with tinnitus are consistent with a maladaptive central gain in auditory pathways.
The Challenge of Perceptual Variability Associated With Tinnitus
It is puzzling that there is a lack of within-subject consistency between objective tinnitus assessment measures such as pitch matching, loudness matching, masking, residual inhibition after masking, and loudness discomfort level. This is ironic because these measures were introduced to provide psychophysically and neurobiologically meaningful descriptors that can standardize diagnosis and treatment. Although these measurements need to be improved (Henry 2016), we suggest that, rather than viewing this variability in reporting solely as a shortcoming of the measurements per se, this variability also may reflect a property of multiple input and multiple output properties of a global network mediating the tinnitus percept and its accompanying phenomena.
Tinnitus is associated with diagnoses such as hearing loss, Ménière disease, otosclerosis, neurovascular compression (e.g., pulsatile tinnitus), middle ear or external meatus blockage (with secretions, cerumen, or hair), temporomandibular joint disorders, migraine, fibromyalgia, some metabolic disorders such as hypothyroidism or hyperthyroidism, and drug intoxication (e.g., salicylate, NSAIDS, and quinine-based medicines) (Langguth et al. 2015; Langguth et al. 2017; Lopez-Escamez et al. 2014). The challenge of the perceptual variability and the task of modeling the neurobiological bases of tinnitus are complicated by the fact that these comorbid conditions are not completely distinct. These comorbidities can be explained by factors specific to auditory pathways and actions at sites of convergence (or overlap) of auditory pathways with pathways involved in producing symptoms associated with the comorbid disorders. It is conceivable that the involvement of multiple systems would undermine the objective consistency of the auditory perceptual dimension. We therefore suggest that the auditory perception that we term tinnitus applies to one dimension of a multidimensional perceptual space that is associated with distinct physiological states in the nervous system.
Recent interest in the cognitive and emotional effects accompanying tinnitus is directed at better defining the processes that account for the distinction between bothersome tinnitus and non-bothersome tinnitus (Tunkel et al. 2014). These features include symptoms that individuals with tinnitus and comorbid conditions often endorse on the Tinnitus Handicap Inventory and other clinical instruments assessing the severity of tinnitus (Newman et al. 1996). These considerations further support the possibility that although a tinnitus network exists, its boundaries may not be fully distinct from a migraine network, or a fibromyalgia network. In fact, the variability in symptom reports may reflect the perceptual expressions of the involvement and contribution of many different (sub)networks.
Major Models of Tinnitus—Common Principles
Recent findings support the hypothesis that the perception of tinnitus is associated with the activation of a central network with multiple inputs and outputs, including auditory, perceptual, affective, and attention components (De Ridder et al. 2011). These networks exhibit intrinsic mechanisms to modify dynamic neuronal properties. These mechanisms are affected in tinnitus. For example, tinnitus is associated with neuronal hyperactivity or hypoactivity, with changes in neuronal transfer functions, with tonotopic reorganization, and with homeostatic or pathogenic plasticity and synchrony (Shore et al. 2016; Schaette and Kempter 2006; Li et al. 2013; Yang et al. 2011). These dynamic changes in the tinnitus network are crucial for understanding the individual components and mechanisms that are necessary and/or sufficient for the perception of tinnitus.
Thus, determining the localization of the different entry points to tinnitus may reveal the necessary conditions sufficient to trigger the disorder, albeit via different networks and mechanisms. Importantly, determining the molecular, cellular, and circuit mechanisms of the pathology associated with these different entry points will provide novel ways to disrupting them and hopefully stopping or at least mitigating the disorder.
Several steps already have been accomplished towards this direction and new challenges and opportunities are on the horizon. This review will not cover all the tinnitus studies, but will focus on the main principles underlying tinnitus and its mechanisms. Moreover, with this review we intend to highlight some new challenges and opportunities in basic and clinical research that ultimately will lead to better diagnostics and treatments for patients.
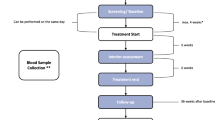
There are currently three major neurophysiological tinnitus models. The deafferentation neurophysiological model is a bottom-up model mostly involving auditory structures expressing structural and functional plasticity in response to various levels of deafferentation (Shore et al. 2016; Schaette and Kempter 2006; Eggermont and Roberts 2004; Norena 2011; Li et al. 2015; Welling and Jackler 2018). This model addresses the phenomenon of tinnitus from a classical bottom-up auditory sensorineural pathway approach. The noise-canceling model posits that tinnitus may reflect a deficiency in the top-down inhibition of auditory pathways, mediated primarily by frontostriatal circuits gating the relevance and affective value of internal and external percepts (Rauschecker et al. 2010, 2015). Hence, it focuses on perceptual and cognitive components. The neuronal global workspace model is a generalization of the other approaches (De Ridder et al. 2014). It encompasses multiple parallel auditory and non-auditory networks, including the frontostriatal circuits. The deafferentation and noise-canceling models can be viewed as subsystems embedded in the global model (Fig. 1).
Overall, these models suggest that tinnitus involves a multisystem network that includes perceptual, cognitive, and limbic components. During normal processing, acoustic energy is transduced by the conductive and sensorineural components of the ear into auditory nerve afferent activity, which enhances the resting state activity of hierarchical ascending neural networks (De Ridder et al. 2014). The acoustic signal travels via the cochlea-acoustic nerve input through the brainstem, midbrain, and thalamic nuclei to the auditory cortex—this process includes multisensory integration. Subsequent auditory cortex activation does not yield the percept itself. The signal has to be processed by the (non-auditory) salience network connecting the signal into the awareness network (De Ridder et al. 2014). Only at that point, is the auditory percept experienced consciously. Simultaneously, the network related to the limbic system assigns emotional significance to the percept (Seydell-Greenwald et al. 2012)—this is the bottom-up component. The top-down influence arises from the cognitive network, which steers both the salience and awareness network. Given that perception is an active process in which the brain searches for the expected information, the auditory perception involves both bottom-up (sensory) and top-down (prediction-driven) processing (De Ridder et al. 2014). Therefore, the common neurophysiologic pathway of patients with tinnitus involves plasticity in these networks that ultimately leads to the pathological linking of central auditory resting state activity and limbic activity to the awareness network without any external sound trigger. There are likely multiple combinations of sufficient conditions to produce a tinnitus percept, including enhanced activity of the network supporting spontaneous auditory activity and/or a decreased threshold for activating the network supporting salience (Schurger et al. 2015).
These models have resulted from many elegant MEG, EEG, and fMRI studies. Although there are several controversies and inconsistencies in the field, which will not be discussed here, we will give a few examples, as to how the field can move forward by exploring these three models, mostly by taking advantage of the common features supported by all of the models. Our position stems from the central concept that, as a field, we can and must do more to bring studies of mechanisms into the realm of neuroscience.
Slow-Wave Cortical Oscillations—Towards the Development of a Reliable Neurophysiological Correlate
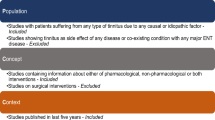
Based on all three models discussed earlier, it is commonly accepted that the most reliable neurophysiological correlate of tinnitus in humans is the appearance of slow-wave (delta/theta) oscillations in individuals with tinnitus (Weisz et al. 2007; Adjamian et al. 2012; Adjamian 2014; De Ridder et al. 2015; Kahlbrock and Weisz 2008; Sedley et al. 2016) (Fig. 2). However, these slow-wave variations are neither sensitive nor specific indicators of tinnitus; for example, they are observed in normal individuals performing cognitive tasking and in association with a variety of pathological conditions (Knyazev 2012; Pinheiro et al. 2016). Oscillations in the delta band (0–4 Hz) are most commonly observed in healthy subjects during the slow-wave sleep, i.e., stage N3, the stage of deepest sleep. Delta band activity is observed at the focus of cortical lesions or diffusively in various encephalopathies. Oscillations in the theta band (4–8 Hz) are observed in relaxed healthy individuals. In patients, both delta and theta band changes have been reported in the low-frequency activity during perceptions with high saliency, such as tinnitus and pain (Knyazev 2012; Pinheiro et al. 2016). Delta and theta activity patterns also are augmented in some psychiatric and neurodegenerative disorders, albeit at different parts of the brain.
Magnetoencephalography tinnitus imaging showing slow-wave oscillation as a reliable correlate of tinnitus. a Superposition of means of multi-taper power spectra for no tinnitus (TI) with clinically normal hearing (blue, n = 14), TI with hearing loss (red, n = 22), TI with clinically normal hearing (cyan, n = 8), and no TI with hearing loss (green, n = 6). b A persistent abnormal low-frequency power spectrum in a tinnitus patient (red). Source activity exhibits a peak in power at 8 Hz, which is reduced by applying a masking auditory stimulus (blue plot). c The ratio of the two power spectra in b demonstrates that masking produces a reduction in theta power of close to one log unit. a Modified from (Adjamian et al. 2012) and b, c modified from (Llinas et al. 2005)
In patients with tinnitus, the slow-wave oscillations do not appear to be correlated with either psychoacoustic or psychosocial measures of tinnitus severity (Pierzycki et al. 2016) and do not have consistent location or site of origin across patients. This heterogeneity, especially if correlated with measures of hearing loss, can form the basis for objective characterization of different types of tinnitus (see next section for details on this point). Moreover, the slow-wave oscillations may reflect thalamocortical activity that is generated during attention to tinnitus. This would signify that the slow-wave oscillations in patients with tinnitus reflect the attention to the internal percept, rather than generating the percept itself. In either case, a detailed mechanistic understanding of the slow-wave oscillations would be beneficial for tinnitus research and treatment.
The molecular, cellular, and circuit mechanisms underlying these oscillations are not understood. Such understanding would create novel targets for categorizing and disrupting tinnitus. One major mechanism that has been proposed, but not tested mechanistically, to explain the generation of the slow-wave oscillations in pathological positive-symptom disorders, such as tinnitus and chronic pain, is the thalamocortical dysrhythmia model (TCD) (Llinas et al. 1999). In TCD, intrinsic neuronal properties form the substrate for the disease-related physiology. The TCD state may be considered in three parts: (1) a brain region of persistent thalamic low-frequency activity due to thalamic hyperpolarization, (2) a brain region that serves as the trigger for thalamocortical dysfunction in which a core region of cortex oscillates at low frequency, and (3) this region is surrounded by an abnormal zone of high-frequency activity (Llinas et al. 2005). In summary, if thalamic hyperpolarization persists and a thalamocortical recurrent loop is established with an area of increased high-frequency activity, one proposed mechanism is that tinnitus results if the dysrhythmic area of thalamus projects to those regions of cortex related to the perception of sound and to feelings of distress.
Even though the existence of high-frequency oscillations is controversial, we suggest that TCD may be a valid mechanism for generating low-frequency oscillations in tinnitus. Moreover, most, if not all, tinnitus models include the deafferentation neurophysiological model, the noise-canceling model, and the neuronal global workspace converge in the thalamus, including the sensory and limbic thalamus, as well as the thalamic reticular nucleus (TRN) (Rauschecker et al. 2015; De Ridder et al. 2015; Caspary and Llano 2017)]. Namely, in the deafferentation model, the deafferentation itself might be causing the abnormal hyperpolarization in the thalamus that can trigger the TCD and in the noise-canceling model frontostriatal circuits affect the limbic thalamus, as well as the TRN, which can subsequently hyperpolarize the auditory thalamus.
To date, no molecular, cellular mechanisms have been confirmed experimentally for the specific mediation of the perception of tinnitus by slow-wave oscillations. However, the TCD model has attractive explanatory potential for production of tinnitus by multiple sufficient sets of underlying processes. Thalamic hyperpolarization may occur by excess inhibition, by disfacilitation resulting from thalamic deafferentation (as in sound-induced hearing loss), or by the inhibition of excitatory ligand-gated channels. Low-frequency thalamic oscillations are consistent with dysfunction of a well-characterized molecular target, the Cav3.1 channel. At the resting membrane potential, thalamic cells fire tonically. When these neurons are hyperpolarized, T-type calcium channels are activated, and thalamic cells fire in low-frequency bursts (Jahnsen and Llinas 1984). These bursts are not abnormal in themselves, as they normally hail sleep onset (Llinas and Steriade 2006; McCormick and Bal 1997; Steriade et al. 1993). However, in tinnitus such thalamic bursts are restricted to certain thalamic nuclei creating a localized low-frequency recurrent interaction between thalamic and cortical neurons that disrupts normal auditory circuit function. Due to thalamic activity as described above, neuronal activity in a localized cortical columnar area is restricted to low frequencies (delta 1–4 Hz, theta 4–8 Hz) and so there is deafness (negative symptoms) at a particular auditory frequency. Accordingly, the firing rate of cortical inhibitory interneurons within this area decreases. As a result, the inhibitory input to adjacent cortical areas is reduced. The reduced activity of inhibitory interneurons mentioned above leads to increased activity in adjacent disinhibited cortex, thus resulting in continuous high-frequency activation underlying the tinnitus perception. This increased continuous activity has been called an edge effect or Hartline effect because it was originally observed as lateral inhibition in the retina (Hartline et al. 1956). An edge effect has been observed as increased spontaneous gamma activity in tinnitus and has been suggested to be responsible for the phantom sounds (positive symptoms) typical of tinnitus (Llinas et al. 2005). This edge effect has been proposed to generate the positive symptoms in other disorders as well, including central pain (Choi et al. 2016) and movement disorders (Moazami-Goudarzi et al. 2008; Sarnthein and Jeanmonod 2007).
This mechanism has not been tested in tinnitus. In vitro and in vivo experiments in animal models could study the electrophysiological properties of single thalamic cells and thalamocortical circuit oscillatory patterns, for example, whether
-
i.
De-inactivation of T-type calcium channels (Cav3.1) and recurrent abnormal thalamocortical circuit activation are seen in tinnitus, but not in non-tinnitus wild type mice;
-
ii.
Abnormal oscillations in brain slices from tinnitus mice are prevented or reduced by T-type calcium channel blockers; and
-
iii.
Recurrent abnormal thalamocortical circuit activation is seen in global CaV3.1 KO mice and/or thalamus-specific CaV3.1 KO tinnitus mice exposed to a loud noise paradigm.
Where should we look for these changes? Cortico-thalamo-cortical circuits mediate sensation, perception, and consciousness, and generate neural network oscillations associated with physiological sleep-spindle activity and focal or generalized epileptic activities such as absence seizures (Steriade 1998). Communication between cerebral cortex and thalamic relay nuclei is mediated by reciprocally connected corticothalamic (CT) and thalamocortical (TC) glutamatergic excitatory pathways. Cortical input is thought to influence primary sensory thalamus by a feed-forward synaptic inhibition of TC relay neurons by GABAergic nRT or perigeniculate neurons (Steriade and Contreras 1995; Sillito and Jones 2002; von Krosigk et al. 1999; Warren et al. 1994; Destexhe et al. 1998). CT neurons excite reticular thalamic nucleus (nRT) neurons (nRT), which subsequently inhibit TC relay neurons. Cortico-thalamo-cortical oscillations are initiated if this inhibition is followed by post-inhibitory rebound bursts of action potentials in TC neurons that in turn re-excite nRT neurons. As this sequence iterates, a network oscillation is sustained (von Krosigk et al. 1999; Warren et al. 1994; von Krosigk et al. 1993). These events in the thalamus, which is an important element in the generation of neural oscillations in cortico-thalamo-cortical circuits, rely on a stronger synaptic excitation in the CT-nRT than in the CT-TC pathway, allowing the inhibition of TC cells to overcome direct CT-TC excitation. Dissection of these synaptic pathways has been challenging until recently, because cortex and thalamus are reciprocally connected and their axons are adjacent; thus, a selective stimulation of CT or TC axons is impossible with electrical stimulation, which activates both pathways. However, recent studies overcame this difficulty by expressing channelrhodopsin-2 (ChR2), a light-sensitive cation channel, in either CT or TC neurons (Nagel et al. 2003). ChR2 expression enables somata and axons to be activated by blue light with a high temporal precision (Yamawaki and Shepherd 2015). Moreover, specific mouse lines with specifically labeled TC cells can be used to for layer- and cell-specific studies in cortex. Therefore, the synaptic and intrinsic properties of these cell types and synapses need to be evaluated before and after noise-induced hearing loss and in animal models of tinnitus. Such an approach would allow the study in isolation of all the different synapses participating in the cortico-thalamo-cortical loops and determine which specific synapse or cell type is involved in tinnitus. Alternatively, such studies may reveal that the intrinsic properties of specific neurons participating in this loop are responsible for tinnitus-related changes in cortico-thalamo-cortical communication in tinnitus mice.
Recent results in the motor cortex have challenged the classic view of TC⇔CT loops. Namely, the motor cortex and the motor thalamus are not directly linked through monosynaptic TC⇔CT loops. It remains to be seen whether these results are relevant for the auditory cortex. The medial geniculate body (MGB) of the thalamus comprises distinct subdivisions, which innervate different layers and areas of AC in patterns that are only partially understood. The ventral subdivision (MGBv) projects tonotopically to multiple layers of primary AC, while the connectivity of the dorsal and medial subdivisions (MGBd and MGBm, respectively) are not as thoroughly characterized. One approach to further characterize these circuits would be to perform rabies virus (RV)-based monosynaptic tracing in cell-type-specific mouse lines which express Cre recombinase in projection-specific subtypes of cortical neurons. The basic experimental strategy would be to inject the cortex of mice from each of these Cre lines with Cre-dependent AAV helper viruses to achieve cell-type-specific expression of TVA such that only the pyramidal neurons of interest will be infected by subsequently injected EnvA-coated RV to enable monosynaptic tracing with fluorescent proteins. Using these RV-based tools, one can map the presynaptic inputs onto layer 5A/B intratelencephalic (IT) neurons (corticocallosal-type neurons; Tlx3-Cre line), layer 5B pyramidal-tract (PT) neurons (corticocollicular-type neurons; Sim1-Cre line), and layer 6 corticothalamic (CT) neurons (Ntsr1-Cre line), as well as onto Gad2-expressing interneurons (Gad2-Cre line). For example, such experiments might demonstrate that all subdivisions of the MGB project to IT, PT, and Gad2 neurons in AC, consistent with the original hypothesis. In contrast, CT neurons might receive the majority of their thalamic input from the MGBm, yet send their axons heavily to MGBv, providing an anatomical substrate for a putative non-direct TC⇔CT loop. Determining the details of the cortico-thalamo-cortical connections in AC and MGB will be important for determining the synaptic changes in these loops that might be associated with hearing loss and tinnitus.
TCD, via thalamo-layer6cortical loops, is not the only known mechanism for generating coherent slow oscillations. Slow-wave oscillations also may be generated by layer 5 cells in auditory cortex (Silva et al. 1991). Many pyramidal neurons in layer 5 of the neocortex show prolonged, 5–12-Hz rhythmic firing patterns at threshold. Rhythmic firing is due to intrinsic membrane properties. Sodium conductances are essential for rhythmicity, and calcium-dependent conductances strongly modify rhythmicity (Silva et al. 1991). Therefore, layer 5 can be both necessary and sufficient to produce slow-wave synchronized oscillations associated with tinnitus, and in vitro, as well as in vivo two photon studies can address this mechanism.
In recent years, the focus of cortical inhibition research has shifted from cellular or single-synapse effects to network effects. Although changes in network effects associated with pathology must originate from intrinsic and/or synaptic changes, appreciation of the network effects will be crucial for understanding the role of inhibition after hearing loss and tinnitus, as cellular or single-synapse changes might have seemingly unexpected network effects. Two current models describe the network effects of inhibition in the auditory cortex: the inhibition stabilized network (ISN) model (Kato et al. 2017), and the cascaded feed-forward (CFF) model (Moore et al. 2018). The ISN model is based on the strength of cortical recurrent inhibition; the CFF model is based on the multiple stages of cortical feed-forward inhibition. The two models are not mutually exclusive and explain how decreased inhibition by photoactivation of different types of interneurons leads to expected enhanced excitation and to paradoxical enhanced inhibition in cortical principal neurons. It will therefore be important to be aware of these models when trying to evaluate the effects of cellular properties on the overall activity of principal neurons and interneurons. For example, a decrease in the intrinsic excitability of PV interneurons might lead to enhanced PV activity in the network. Moreover, based on the CFF model, local decreases in inhibition can lead to layer- or site-specific changes in the net spiking of interneurons; whereas, such dependence on the location within the network is not expected based on the ISN model. As such, hearing loss and tinnitus also can be used as physiological changes to assess whether AC operates in either ISN or CFF or both regimes. At any rate, both in vivo and in vitro cell-, synapse-, and network-specific experiments are now doable and are needed to probe the cortical mechanisms underlying neuronal adaptations to hearing loss that might lead to tinnitus.
Together, we propose that a detailed understanding of the molecular, cellular, and circuit mechanisms underlying the generation and differential localization of tinnitus-related slow-wave oscillations is a key requirement for the advancement of tinnitus research and treatment. Elucidation of these mechanisms in animal models of tinnitus will be crucial for designing studies to test this hypothesis in humans. For example, could T-type channel blockers help patients with tinnitus? Moreover, the TCD paradigm and the proposed research will provide specific guidelines for the application of repetitive transcranial stimulation (rTMS). Repetitive transcranial magnetic stimulation is an investigative treatment involving application of strong magnetic field impulses to the scalp to induce an electrical current that alters neural activity directly in the brain. Systematic reviews of randomized trials have found conflicting results with respect to a benefit in patients with tinnitus (Bauer 2018; Soleimani et al. 2016). Because the TCD model predicts that focused stimulation in the area showing low-frequency entrainment would optimally remove or mitigate tinnitus and since the region of low-frequency activity varies from patient to patient, the proposed MEG localization onto a structural MRI of this area in every patient would be consistent with a precision medicine approach and beneficial for the patient.
Towards a Quantitative, Mechanistic Model for Predicting the Type of Tinnitus Caused by Noise-Induced or Aging-Dependent Hearing Loss
We propose that in vitro/vivo studies in animal models of tinnitus combined with research in humans may unmask a relationship between the mechanism and the localization of the slow-wave oscillation with the type and extent of the hearing loss in patients with tinnitus.
It is crucial to resolve the hypothesis whether there is a link between the detailed audiological/psychophysical profile of patients with tinnitus and the specific localization of slow-wave oscillations. Previous studies suggested that the extent of hearing loss determines whether pathological slow-wave oscillations are associated with auditory cortex, mostly happening for smaller hearing threshold changes < 30 dB (Vanneste and De Ridder 2016), or with memory systems such as the parahippocampus, seen in patients with tinnitus with more robust hearing threshold shifts. The audiological assessments in these studies were based on changes in hearing threshold criteria, but more accurate assessment of the amount, type, and localization of hearing loss and hearing function may provide better resolution.
Recent advancements highlight more sensitive assays for quantifying auditory nerve damage, even without changes in hearing thresholds, termed synaptopathy or hidden hearing loss, thus providing new opportunities for addressing the mechanistic links between peripheral damage and central changes that can ultimately predict and track tinnitus. Based on Liberman et al. (2016), using electrocochleography producing the ratio between the waveform peaks generated by hair cells (summating potential (SP)) vs. cochlear neurons (action potential (AP)), SP/AP ratio, may provide an objective diagnostic and quantitative tool for synaptopathy, despite the presence of normal thresholds at standard audiometric frequencies. This work is preliminary, but it sheds light on the potential of auditory biomarkers for identifying locations and mechanisms of tinnitus in humans. Different groups have used different assays for detecting hidden hearing loss, such as envelope following response (EFR) (Guest et al. 2017). EFR is the sustained response representing neural synchrony to the envelope of an amplitude-modulated stimulus. Although current studies disagree in the involvement of synaptopathy in tinnitus (Guest et al. 2017; Schaette and McAlpine 2011), such studies in humans hold the promise to link differential hearing loss with specific tinnitus mechanisms, further evidenced by the differential localization and underlying mechanisms/frequencies of slow oscillations, depending on the extent of the peripheral damage.
We propose that combinations of human-related studies with animal model studies which correlate tinnitus and its central correlates throughout auditory and non-auditory centers over time with different types and degrees of peripheral damage could be helpful towards developing a detailed model that can predict types of tinnitus based on the peripheral damage and different central neural correlates.
Towards a Precision Medicine Approach
The implementation of a nosology that is based on the underlying neurobiological mechanisms is the initial stage in a precision medicine approach to diagnosing patients experiencing tinnitus, hyperacusis, misophonia, and false percepts, including polycusis. A general schema in Fig. 3 suggests that the symptoms of disorders of auditory perception reflect an interaction between processing in auditory lemniscal pathways and limbic and affective pathways. Although tinnitus has mechanistic components that produce the unique features of tinnitus, as discussed earlier, symptoms of hyperacusis and tinnitus are often comorbid and hence they might share some common etiologic features, such as elevated gain. Misophonia, on the other hand, is dominated by a strong aversive component that may parallel the interoceptive and affective components of a conditioned taste aversion.
Schematic block diagram of mechanisms that produce misophonia, hyperacusis, tinnitus, polycusis, and other false auditory percepts. Afferents from the cochlea, saccule, somesthetic pathways, and visceral sensory pathways contribute to processing in auditory lemniscal pathways. Modular thalamocortical processing is hypothesized to contribute (1) a common component to comorbid features of hyperacusis and tinnitus, (2) a component that produces unique features of tinnitus, and (3) component(s) for other false auditory perceptions. A parallel, interoceptive, and affective network produces the aversion, annoyance, fear, and pain-like features that may be associated with hyperacusis and misophonia
The next step is to explore whether the underlying neurobiological mechanisms provide a rigorous explanation and perhaps a prediction of the signs and symptoms in patients with these disorders. If so, they will form the basis for a precision medicine nosology. In this context, audiological tests of speech comprehension need to test the implications of thalamocortical processing models for perceptual consequences of specific changes in performance during tinnitus, such as dysregulation of coherence within specific and non-specific thalamic loops, the status of low-frequency oscillations in one thalamocortical network region, and the status of high-frequency activation in a surrounding region. For example, one might predict alterations in the entrainment of delta and theta rhythms to speech stimuli that are strong in auditory cortical regions, including the augmented coupling between these rhythms at edges of a continuous speech envelope (Gross et al. 2013; Keitel et al. 2017). One critical gap in our understanding is the identification of the adequate stimulus dimensions of the speech envelope that are detected by auditory cortices, and may be disrupted by physiological alterations during tinnitus.
For patients with tinnitus and hyperacusis, our overall expectation for the next few years is a modified classification, instructed by different peripheral and central plasticity mechanisms associated with compensation for noise- and/or aging-dependent hearing loss. Such etiology-based identification is consistent with the modern approach of precision medicine—an approach that differentiates underlying causes and neurophysiological/network features.
Given the paucity of data related to the underlying mechanism of tinnitus in humans, it is difficult to produce a hypothesis-driven set of tests and test parameters. Alternatively, there are numerous publications that have reported differences in audiological tests between individuals reporting tinnitus and those who do not report tinnitus. One approach is to replicate these tests and further include tests across the entire auditory pathway (Table 1), increasing the chance of finding differences between individuals with and without tinnitus. The parallel execution and correlation of peripheral and central tests will provide further advantage in developing more precise models of tinnitus pathology. This type of big data set might be well suited to an unbiased machine learning analysis paradigm to assist in ultimately building a hypothesis-driven model.
Tests of peripheral function should include comprehensive audiometry and otoacoustic emissions. Comprehensive audiometry evaluates hearing sensitivity. It has been reported that hearing thresholds in subjects with normal hearing who have tinnitus were worse than subjects with normal hearing who do not have tinnitus (Fabijanska et al. 2012).
Otoacoustic emissions (OAEs) reflect the function of cochlear outer hair cells. There are several ways to record and report these results (distortion product OAEs [DPOAEs], transient-evoked OAEs [TEOAEs], spontaneous OAEs [SOAEs]). Data indicate that DPOAE amplitudes (Fabijanska et al. 2012; Paglialonga et al. 2010; Sztuka et al. 2010; Shiomi et al. 1997) and TEOAE amplitudes (Paglialonga et al. 2010; Omidvar et al. 2016; Chery-Croze et al. 1994) are reduced in subjects with tinnitus. Additionally, SOAEs are significantly different between subjects with tinnitus and those without tinnitus (Kim et al. 2011). Contralateral suppression of the OAE response using noise is thought to reflect the status of the medial olivocochlear system and has been shown to differ in the presence of tinnitus (Paglialonga et al. 2010; Favero et al. 2006; Riga et al. 2007).
Questionnaires are often used to evaluate the self-perceived handicap that a subject experiences as a result of their tinnitus (for example, the Tinnitus Handicap Inventory and Tinnitus Functional Index). For some people, tinnitus is a catastrophic disturbance. For others, it has little-to-no effect on their lives. Additionally, subjects with tinnitus frequently have comorbid mental health issues (Pinto et al. 2014) which affect their ability to cope with the tinnitus. We are interested in determining whether the neuroimaging data obtained from the magnetoencephalography and electroencephalography testing which allows us to evaluate slow brain wave oscillations will be predictive of how the subjects are experiencing or suffering from their tinnitus.
Because there is no objective measurement available which will demonstrate the perception of the subject’s tinnitus, pitch and loudness measurements are often completed. It has been suggested that the audiogram configuration may correlate to the subjective report of the tinnitus (Pan et al. 2009; Sereda et al. 2011; Moore et al. 2010; Schecklmann et al. 2012; Shekhawat et al. 2014). Some data suggest that the majority of subjects with tinnitus match the pitch of their tinnitus to be at or above 3000 Hz (Reed 1960; Meikle and Taylor-Walsh 1984). Additionally, an estimated 90 % of subjects who perceive tinnitus experience the phenomenon of residual inhibition in which the tinnitus percept is decreased following the presentation of a masking stimulus (Henry and Meikle 2000; Vernon and Meikle 2003).
Psychoacoustic testing evaluates a subject’s ability to identify small differences in stimuli (i.e., discriminate between different frequencies and intensities or detect modulation). Jain and Sahoo (2014) suggest that subjects with tinnitus display impairments in these abilities when compared to subjects without tinnitus. Additionally, patients with tinnitus demonstrated better the same or worse performance on a modulation detection task depending on the carrier frequency (Jain and Sahoo 2014; Moon et al. 2015; Paul et al. 2017).
Loudness discomfort levels are a subjective measurement of perceptual loudness and indicate the maximum sound intensity that a patient can tolerate. Decreased ability to tolerate specific environmental sounds has been commonly noted in subjects with tinnitus (Jastreboff and Jastreboff 2000). In subjects with tinnitus, sensitivity to loud sounds was enhanced (Hebert et al. 2013). Additionally, measurements indicate that subjects with tinnitus have abnormal perception of loudness scaling (Weisz et al. 2004; Newman et al. 1994).
Immittance testing includes tympanometry and acoustic reflex results. Tympanometry evaluates the status of the middle ear and the acoustic reflex response reflects the function of the stapedius muscle contraction in response to loud sounds. This acoustic reflex is different from the gap prepulse inhibition of the acoustic startle reflex (GPIAS) often used in animal models of testing. In subjects with tinnitus, acoustic reflexes have been reduced or absent (Wojtczak et al. 2017; Fernandes Lda et al. 2013).
Auditory processing ability reflects the brain’s ability to interpret complex stimuli. Tests of auditory processing ability in patients with tinnitus often reveal deficits in this area (Araneda et al. 2015). There are several domains that are typically assessed: binaural integration, binaural separation, temporal, auditory closure, auditory figure-ground, and binaural interaction. In subjects with tinnitus, abnormal scores on this test battery are common (Jain and Sahoo 2014; Newman et al. 1994; Fournier and Hebert 2013; Mehdizade Gilani et al. 2013; Epp et al. 2012; Goldstein and Shulman 1999; Ryu et al. 2012).
Short-latency electrophysiologic responses (electrocochleography, auditory brainstem response [ABR], envelope following response [EFR], and frequently following response [FFR]) measure the electrical impulses generated by the auditory nerve and brainstem that occur in the first 0–10 ms following a transient stimulus. Data show that waveform latencies (Singh et al. 2011; Gerken et al. 2001) and amplitudes (Schaette and McAlpine 2011; Attias et al. 1996; Konadath and Manjula 2016) are different between ears with tinnitus and ears without tinnitus. Tinnitus has not definitively been shown to affect the EFR, although recent data have demonstrated a non-significant trend for lower amplitude in individuals with tinnitus (Guest et al. 2017; Paul et al. 2017).
Electrical (EEG) and magnetic (MEG) neuronal activity can test stages of information processing from the thalamus throughout auditory cortices and executive control cortex in posterior parietal and frontal cortices. Here is a battery of proposed tasks:
-
Task 1.
Resting state EEG/MEG both in silent and with white noise to mask the tinnitus.
-
Task 2.
Auditory-evoked potentials. Presentations of a series of 600 click stimuli to allow recording of mid-latency (thalamic and auditory sensory cortex, 25–50 ms) and long-latency (primary and associative auditory sensory cortex, 50–200 ms) evoked potentials to test early and late sensory-perceptual processing.
-
Task 3.
Auditory steady state response. Presentation of short (500 ms) bursts of clicks at 20 (betaband) and at 40 Hz (gammaband). This steady state-evoked potential, especially at gamma frequencies, will allow for assessment of auditory sensory circuits to coordinate activity at high processing speeds.
-
Task 4.
Roving standard mismatch negativity. Presentations of short sequences of repeated tone pips, changing the frequency every two to four tones. This will allow for probing sensory activity in the area of specific frequency loss and also the ability to detect frequency changes as well as cortical repetition suppression.
-
Task 5.
P300 oddball target detection. Presentation of an “oddball” task with a highly frequent standard tone (85 %) and an infrequent target tone (15 %). Participants will either ignore the tones or detect the oddball. This will allow for detection of auditory cognitive processing, and for the activation of frontal and parietal executive control areas in the service of selective attention.
-
Task 6.
Dichotic word task. Presentation of different words to each ear, and ask participants to concentrate on one ear. This will allow for probing of attentional systems and cognitive control to naturalistic speech stimuli in the disorder.
These data should be collected with high-resolution structural MRI information and use the Human Connectome Project parcellation scheme to source-resolve sensor-level activity to the cortical surface. Connectivity analyses of MEG including phase-locking (PLV) methods (Ghuman et al. 2008, 2011, 2013) are useful for these studies. Connectivity maps can be created from analysis of the MEG data and can be quantitatively compared across conditions. PLVs between these regions can be determined by analyzing the variability in the phase difference across trials or time (Lachaux et al. 1999) and comparing the PLVs in individuals who suffer from tinnitus to controls. Finally, sensitive multivariate classification methods from machine learning on these data for careful examination of neural differences between individuals with tinnitus and controls would be helpful. Briefly, all-to-all connectivity matrices with respect to frequency can be split into training and test sets. Classifiers can be trained on the training set and the accuracy of the model can be assessed by determining classification accuracy on the test set.
Here are some examples where testing can become more hypothesis driven and therefore more “precise” given what the participant presents with in terms of tinnitus.
When exploring the Envelope Modulation Detection, individuals with tinnitus complete a pitch matching process. This pitch is then being use as the base stimulus in the modulation distortion task for this individual. Therefore, each subject will have a customized signal in the Envelope Modulation Detection task based on their perceived tinnitus. Previous studies have shown mixed results with this task in differentiating individuals with and without tinnitus and this may be related to the proximity of the test signal to the individual’s tinnitus. Using one fixed signal could significantly add to the variability seen. This variability will be reduced by matching the test stimulus to the individual’s perceived tinnitus.
Regarding OAE suppression, the animal model supports a lack of inhibition in animals suspected of having tinnitus. In the human, we expect suppression of the OAE when noise is presented to the contralateral ear. If the system has a lack of inhibition, one would hypothesize that the OAE would not be suppressed in individuals with tinnitus. Several researchers have reported a difference in suppression for individuals with perceived tinnitus (Paglialonga et al. 2010; Favero et al. 2006; Riga et al. 2007).
In the envelope following response, tinnitus has not definitively been shown to affect the EFR, although recent data have demonstrated a non-significant trend for lower amplitude in individuals with tinnitus (Guest et al. 2017; Paul et al. 2017). Using individualized stimuli to elicit the EFR based on the subject’s perceived tinnitus frequency may reduce the variability seen in previous studies and allow us to see an effect specific to the frequency area of the tinnitus.
Overall, based on extensive peripheral and central testing of the same subjects with tinnitus as described earlier, we anticipate that identification of particular groups of patients with tinnitus would be more likely to respond to treatment if a selection is made on the basis of symptoms, objective tests, and neurobiological models of etiology. This approach will need to encompass features such as where the slow oscillations are observed, the frequency content and temporal relations of the slow oscillations, and characterization of central adaptations in the context of well-characterized peripheral hearing loss. Identification of different patient subgroups with distinct audiological, psychophysical, and neurophysiological characteristics will facilitate the management of patients with tinnitus as well as the design and execution of drug development and clinical trials, which, for the most part, have not yielded conclusive results.
An alternative outcome of a precision medicine approach in tinnitus would be that additional mechanistic phenotyping might not lead to the identification of distinct drivers in each individual, but instead, it might reveal that each individual may display a quantitative blend of causal factors. Therefore, a precision medicine approach towards identifying these causal factors might not lead to subtyping these patients but may instead highlight causal pathways that can be manipulated for therapeutic gain. These two outcomes are not mutually exclusive, and no matter what the final outcome is, a mechanistic-driven precision medicine approach is a win-win approach for advancing tinnitus research and treatment.
Animal Models Towards Understanding Plasticity Mechanisms—What If We Never Develop or Globally Accept an Animal Model of Tinnitus?
The brain is plastic, capable of continuous, small- and large-scale anatomical, neurochemical, and functional change—in either a positive or negative direction and across the life span. The neuroplastic processes that underlie the emergence of—and that perpetuate and elaborate the deficits of—tinnitus are the same processes that can be used to drive changes in a corrective direction, and can potentially ameliorate tinnitus.
Animal models will be crucial in developing a deeper mechanistic understanding of molecular, cellular, and circuit mechanisms of brain plasticity in response to sound exposure. One current problem in the tinnitus field is the lack of a commonly accepted animal model for tinnitus. This problem, which needs to be addressed by the improvement and standardization existing animal models, use of appropriate statistics, such as ANOVA tests and corrections for multiple comparisons, distinction between correlative and causative statements, and control of the acoustic environment in tinnitus behavioral experiments (Jones and May 2018), has been discussed in previous reviews (Galazyuk and Hebert 2015) and has resulted in some hesitation or skepticism regarding mechanistic studies in animal models. We still propose that a detailed understanding of the cellular/molecular/circuit plasticity of brain circuits in response to aging or exposure to loud sounds and hearing loss (hidden or not) will be crucial not only for tinnitus but also for the understanding and treating of many other hearing-related pathologies, such as neuropathies, hyperacusis, and hearing loss. Tinnitus is part of a pathological continuum in the consequences of noise-induced or aging-dependent hearing loss, including hair cell loss, synaptopathy, subsequent changes in the central gain, balance of excitation and inhibition, and synchrony and tonotopy. These plasticity mechanisms are found in the cochlear nucleus, midbrain, thalamus, auditory cortex, and other non-auditory-related structures. Detailed understanding of this continuum will be crucial for understanding the peripheral and central neural mechanisms that can cause and correct hearing-related disorders, such as tinnitus and hyperacusis. Such understanding is useful and crucial, even if we are not sure at the moment whether our animal models are detecting (only) tinnitus.
An analogue that comes to mind is the extensive research of synaptic plasticity mechanisms in the hippocampus, such as long-term potentiation (LTP) and long-term depression (LTD), in the 90s. The main justification for this research at the time was the involvement of these mechanisms in memory and learning—such causal linkage was far from concrete at the time. Despite this uncertainty, the thorough and high-quality research of these mechanisms advanced tremendously the field of neuroscience, not only in terms of addressing memory and learning but most importantly in uncovering fundamental mechanisms of synaptic function, such as receptor trafficking and synaptic structure/function, which are now crucial for many disorders, such as addiction, autism, and schizophrenia. Therefore, we suggest that high-quality mechanistic work on all aspects of peripheral and central mechanisms in response to sound or aging are crucial for understanding, characterizing, and curing hearing-related disorders, including tinnitus.
There is a possibility that there will never be a globally accepted animal model for tinnitus. However, mechanistic insight on plasticity mechanisms gained by animal models of noise-induced hearing loss along with the human studies described in the previous section will produce a revolutionary new dynamic picture of the tinnitus brain that, for the first time, will show how individual cells and complex neural circuits interact in both time and space after noise-induced hearing loss and tinnitus. By extension, abnormally organized auditory and non-auditory networks, and their associated perceptual and cognitive deficits, should be amenable to pharmacological or intensive training-based remediation. The idea is to apply novel strategies and technology that customize training, based on the location of the mechanism of pathogenic plasticity, to address the specific neurological deficits of each person.
Towards Enhancing Access to Evidence-Based Information and Medical Services for Health Care Providers and Patients With Tinnitus
The Clinical Practice Guideline: Tinnitus, which was based on a systematic review of randomized controlled trials (Tunkel et al. 2014), was completed in early-mid 2013, and numerous new findings have been reported since then. It is therefore crucial that findings from those trials are integrated with the recommendations from the Clinical Practice Guideline: Tinnitus.
Moreover, concerted effort by Clinics and Tinnitus Centers to provide current data-driven knowledge to health care providers and patients would be extremely helpful. Unfortunately, when patients with tinnitus search the internet for tinnitus information, they are bombarded with sites that falsely claim a product or service will cure or mitigate tinnitus. A website from AAO-HNSF and the American Academy of Audiology (AAA) specific to patients with tinnitus to address their education and information would be a service to patients seeking accurate information. Otolaryngologists and audiologists form the team who currently diagnose and treat these patients, and it would be ideal for these two professional organizations to present consistent information to the patients suffering from tinnitus.
References
Adams PF, Hendershot GE, Marano MA, C. Centers for Disease, S. Prevention/National Center for Health (1999) Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10:1–203
Adjamian P (2014) The application of electro- and magneto-encephalography in tinnitus research - methods and interpretations. Front Neurol 5:228
Adjamian P, Sereda M, Zobay O, Hall DA, Palmer AR (2012) Neuromagnetic indicators of tinnitus and tinnitus masking in patients with and without hearing loss. J Assoc Res Otolaryngol 13:715–731
Araneda R, de Volder AG, Deggouj N, Philippot P, Heeren A, Lacroix E, Decat M, Rombaux P, Renier L (2015) Altered top-down cognitive control and auditory processing in tinnitus: evidences from auditory and visual spatial stroop. Restor Neurol Neurosci 33:67–80
Attias J, Pratt H, Reshef I, Bresloff I, Horowitz G, Polyakov A, Shemesh Z (1996) Detailed analysis of auditory brainstem responses in patients with noise-induced tinnitus. Audiology 35:259–270
Baguley DM (2003) Hyperacusis. J R Soc Med 96:582–585
Baguley DM, McFerran DJ (2010) Hyperacusis and disorders of loudness perceptionHyperacusis and disorders of loudness perception. In: Møller A, Langguth B, De Ridder D, Kleinjung T (eds) Textbook of Tinnitus. Springer, New York, pp 13–23
Barnea G, Attias J, Gold S, Shahar A (1990) Tinnitus with normal hearing sensitivity: extended high-frequency audiometry and auditory-nerve brain-stem-evoked responses. Audiology 29(1):36–45
Bauer CA (2018) Tinnitus. N Engl J Med 378:1224–1231
Caspary DM, Llano DA (2017) Auditory thalamic circuits and GABAA receptor function: putative mechanisms in tinnitus pathology. Hear Res 349:197–207
Chery-Croze S, Moulin A, Collet L, Morgon A (1994) Is the test of medial efferent system function a relevant investigation in tinnitus? Br J Audiol 28:13–25
Choi S, Yu E, Hwang E, Llinas RR (2016) Pathophysiological implication of CaV3.1 T-type Ca2+ channels in trigeminal neuropathic pain. Proc Natl Acad Sci U S A 113:2270–2275
Corliss EL, Burnett ED, Stimson HF (1968) "Polyacusis", a hearing anomaly. J Acoust Soc Am 43:1231–1236
da Cruz Fernandes L, Momensohn-Santos TM, Carvalho JSM, de Queiroz Carvalho FL (2013) Tinnitus and normal hearing: A study on contralateral acoustic reflex. Am J Audiol 22(2):291–296
de Leede-Smith S, Barkus E (2013) A comprehensive review of auditory verbal hallucinations: lifetime prevalence, correlates and mechanisms in healthy and clinical individuals. Front Hum Neurosci 7:367
De Ridder D, Elgoyhen AB, Romo R, Langguth B (2011) Phantom percepts: tinnitus and pain as persisting aversive memory networks. Proc Natl Acad Sci U S A 108:8075–8080
De Ridder D et al (2014) An integrative model of auditory phantom perception: tinnitus as a unified percept of interacting separable subnetworks. Neurosci Biobehav Rev 44:16–32
De Ridder D, Vanneste S, Langguth B, Llinas R (2015) Thalamocortical dysrhythmia: a theoretical update in tinnitus. Front Neurol 6:124
Delb W, Strauss DJ, Low YF, Seidler H, Rheinschmitt A, Wobrock T, D’Amelio R (2008) Alterations in Event Related Potentials (ERP) associated with tinnitus distress and attention. Appl Psychophysiol Biofeedback 33(4):211–221
Destexhe A, Contreras D, Steriade M (1998) Mechanisms underlying the synchronizing action of corticothalamic feedback through inhibition of thalamic relay cells. J Neurophysiol 79:999–1016
Diesch E, Andermann M, Flor H, Rupp A (2010). Interaction among the components of multiple auditorys steady-state responses: enhancement in tinnitus patients, inhibition in controls. Neuroscience 167(2):540–553
Dornhoffer J, Danner C, Mennemeier M, Blake D, Garcia-Rill E (2006) Arousal and attention deficits in patients with tinnitus. Int Tinnitus J 12(1):9
dos Santos Filha VAV, Matas CG (2010) Late Auditory evoked potentials in individuals with tinnitus. Braz J Otorhinolaryngol 76(2):263–270
Eggermont JJ, Roberts LE (2004) The neuroscience of tinnitus. Trends Neurosci 27:676–682
Epp B, Hots J, Verhey JL, Schaette R (2012) Increased intensity discrimination thresholds in tinnitus subjects with a normal audiogram. J Acoust Soc Am 132:EL196–EL201
Fabijanska A et al (2012) The relationship between distortion product otoacoustic emissions and extended high-frequency audiometry in tinnitus patients. Part 1: normally hearing patients with unilateral tinnitus. Med Sci Monit 18:CR765–CR770
Favero ML, Sanchez TG, Bento RF, Nascimento AF (2006) Contralateral suppression of otoacoustic emission in patients with tinnitus. Braz J Otorhinolaryngol 72:223–226
Fernandes Lda C, Momensohn-Santos TM, Carvalho JS, Carvalho FL (2013) Tinnitus and normal hearing: a study on contralateral acoustic reflex. Am J Audiol 22:291–296
Fournier P, Hebert S (2013) Gap detection deficits in humans with tinnitus as assessed with the acoustic startle paradigm: does tinnitus fill in the gap? Hear Res 295:16–23
Galazyuk A, Hebert S (2015) Gap-Prepulse inhibition of the acoustic startle reflex (GPIAS) for tinnitus assessment: current status and future directions. Front Neurol 6:88
Gerken GM, Hesse PS, Wiorkowski JJ (2001) Auditory evoked responses in control subjects and in patients with problem-tinnitus. Hear Res 157(1):52–64
Ghuman AS, Bar M, Dobbins IG, Schnyer DM (2008) The effects of priming on frontal-temporal communication. Proc Natl Acad Sci U S A 105:8405–8409
Ghuman AS, McDaniel JR, Martin A (2011) A wavelet-based method for measuring the oscillatory dynamics of resting-state functional connectivity in MEG. Neuroimage 56:69–77
Ghuman AS, van den Honert RN, Martin A (2013) Interregional neural synchrony has similar dynamics during spontaneous and stimulus-driven states. Sci Rep 3:1481
Gilani VM, Ruzbahani M, Mahdi P, Amali A, Khoshk MHN, Sameni J et al (2013) Temporal processing evaluation in tinnitus patients: results on analysis of gap in noise and duration pattern test. Iran J Otorhinolaryngol 25(73):221
Goldstein B, Shulman A (1999) Central auditory speech test findings in individuals with subjective idiopathic tinnitus. Int Tinnitus J 5:16–19
Gross J, Hoogenboom N, Thut G, Schyns P, Panzeri S, Belin P, Garrod S (2013) Speech rhythms and multiplexed oscillatory sensory coding in the human brain. PLoS Biol 11:e1001752
Guest H, Munro KJ, Prendergast G, Howe S, Plack CJ (2017) Tinnitus with a normal audiogram: relation to noise exposure but no evidence for cochlear synaptopathy. Hear Res 344:265–274
Haenggeli CA, Pongstaporn T, Doucet JR, Ryugo DK (2005) Projections from the spinal trigeminal nucleus to the cochlear nucleus in the rat. J Comp Neurol 484:191–205
Hartline HK, Wagner HG, Ratliff F (1956) Inhibition in the eye of limulus. J Gen Physiol 39:651–673
Hebert S, Fournier P, Norena A (2013) The auditory sensitivity is increased in tinnitus ears. J Neurosci 33:2356–2364
Henry JA (2016) "Measurement" of tinnitus. Otol Neurotol 37:e276–e285
Henry JA, Meikle MB (2000) Psychoacoustic measures of tinnitus. J Am Acad Audiol 11:138–155
Horowitz G, Polyakov A, Shemesh Z (1996) Detailed analysis of auditory brainstem responses in patients with noise-induced tinnitus. Audiology 35(5):259–270
Jacobson GP, McCaslin DL (2003) A reexamination of the long latency N1 response in patients with tinnitus. J Am Acad Audiol 14(7):393–400
Jacobson GP, Calder JA, Newman CW, Peterson EL, Wharton JA, Ahmad BK (1996) Electrophysiological indices of selective auditory attention in subjects with and without tinnitus. Hear Res 97(1):66–74
Jahnsen H, Llinas R (1984) Ionic basis for the electro-responsiveness and oscillatory properties of Guinea-pig thalamic neurones in vitro. J Physiol 349:227–247
Jain C, Sahoo JP (2014) The effect of tinnitus on some psychoacoustical abilities in individuals with normal hearing sensitivity. Int Tinnitus J 19:28–35
Jastreboff PJ, Jastreboff MM (2000) Tinnitus retraining therapy (TRT) as a method for treatment of tinnitus and hyperacusis patients. J Am Acad Audiol 11:162–177
Jastreboff PJ, Jastreboff MM (2015) Decreased sound tolerance: hyperacusis, misophonia, dplacusis, and polycusis. In: Celesia CC, Hickok G (eds) The Human Auditory System. Elsevier, Amsterdam, pp 375–387
Johns LC, Kompus K, Connell M, Humpston C, Lincoln TM, Longden E, Preti A, Alderson-Day B, Badcock JC, Cella M, Fernyhough C, McCarthy-Jones S, Peters E, Raballo A, Scott J, Siddi S, Sommer IE, Larøi F (2014) Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull 40(Suppl 4):S255–S264
Jones A, May BJ (2018) Effects of acoustic environment on tinnitus behavior in sound-exposed rats. J Assoc Res Otolaryngol 19:133–146
Kahlbrock N, Weisz N (2008) Transient reduction of tinnitus intensity is marked by concomitant reductions of delta band power. BMC Biol 6:4
Kato HK, Asinof SK, Isaacson JS (2017) Network-Level Control of Frequency Tuning in Auditory Cortex. Neuron 95:412–423 e414
Keitel A, Ince RAA, Gross J, Kayser C (2017) Auditory cortical delta-entrainment interacts with oscillatory power in multiple fronto-parietal networks. Neuroimage 147:32–42
Kim DK, Park SN, Park KH, Choi HG, Jeon EJ, Park YS, Yeo SW (2011) Clinical characteristics and audiological significance of spontaneous otoacoustic emissions in tinnitus patients with normal hearing. J Laryngol Otol 125:246–250
Knipper M, Van Dijk P, Nunes I, Ruttiger L, Zimmermann U (2013) Advances in the neurobiology of hearing disorders: recent developments regarding the basis of tinnitus and hyperacusis. Prog Neurobiol 111:17–33
Knyazev GG (2012) EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci Biobehav Rev 36:677–695
Konadath S, Manjula P (2016) Auditory brainstem response and late latency response in individuals with tinnitus having normal hearing. Intractable Rare Dis Res 5:262–268
Kumar S, Sedley W, Barnes GR, Teki S, Friston KJ, Griffiths TD (2014) A brain basis for musical hallucinations. Cortex 52:86–97
Lachaux JP, Rodriguez E, Martinerie J, Varela FJ (1999) Measuring phase synchrony in brain signals. Hum Brain Mapp 8:194–208
Langguth B et al (2015) Tinnitus and Headache. Biomed Res Int 2015:797416
Langguth B, Hund V, Landgrebe M, Schecklmann M (2017) Tinnitus patients with comorbid headaches: the influence of headache type and laterality on tinnitus characteristics. Front Neurol 8:440
Lee CY, Jaw FS, Pan SL, Lin MY, Young YH (2007) Auditory cortical evoked potentials in tinnitus patients with normal audiological presentation. J Formos Med Assoc 106(12):979–985
Li S, Choi V, Tzounopoulos T (2013) Pathogenic plasticity of Kv7.2/3 channel activity is essential for the induction of tinnitus. Proc Natl Acad Sci U S A 110:9980–9985
Li S, Kalappa BI, Tzounopoulos T (2015) Noise-induced plasticity of KCNQ2/3 and HCN channels underlies vulnerability and resilience to tinnitus. Elife. 4. https://doi.org/10.7554/eLife.07242
Liberman MC, Epstein MJ, Cleveland SS, Wang H, Maison SF (2016) Toward a differential diagnosis of hidden hearing loss in humans. PLoS One 11:e0162726
Llinas RR, Steriade M (2006) Bursting of thalamic neurons and states of vigilance. J Neurophysiol 95:3297–3308
Llinas RR, Ribary U, Jeanmonod D, Kronberg E, Mitra PP (1999) Thalamocortical dysrhythmia: a neurological and neuropsychiatric syndrome characterized by magnetoencephalography. Proc Natl Acad Sci U S A 96:15222–15227
Llinas R, Urbano FJ, Leznik E, Ramirez RR, van Marle HJ (2005) Rhythmic and dysrhythmic thalamocortical dynamics: GABA systems and the edge effect. Trends Neurosci 28:325–333
Lopez-Escamez JA et al (2014) Accompanying symptoms overlap during attacks in Meniere's disease and vestibular migraine. Front Neurol 5:265
McCormick DA, Bal T (1997) Sleep and arousal: thalamocortical mechanisms. Annu Rev Neurosci 20:185–215
Mehdizade Gilani V, Ruzbahani M, Mahdi P, Amali A, Nilforush Khoshk MH, Sameni J, Karimi Yazdi A, Emami H (2013) Temporal processing evaluation in tinnitus patients: results on analysis of gap in noise and duration pattern test. Iran J Otorhinolaryngol 25:221–226
Meikle M, Taylor-Walsh E (1984) Characteristics of tinnitus and related observations in over 1800 tinnitus clinic patients. J Laryngol Otol Suppl 9:17–21
Moazami-Goudarzi M, Sarnthein J, Michels L, Moukhtieva R, Jeanmonod D (2008) Enhanced frontal low and high frequency power and synchronization in the resting EEG of parkinsonian patients. Neuroimage 41:985–997
Møller A (2010) Misophonia, phonophobia and “exploding head” syndrome. In: Møller A, Langguth B, De Ridder D, Kleinjung T (eds) Textbook oo Tinnitus. Springer, New York, pp 25–27
Moon IJ, Won JH, Kang HW, Kim DH, An YH, Shim HJ (2015) Influence of tinnitus on auditory spectral and temporal resolution and speech perception in tinnitus patients. J Neurosci 35:14260–14269
Moore BC, Vinay, Sandhya (2010) The relationship between tinnitus pitch and the edge frequency of the audiogram in individuals with hearing impairment and tonal tinnitus. Hear Res 261:51–56
Moore AK, Weible AP, Balmer TS, Trussell LO, Wehr M (2018) Rapid Rebalancing of Excitation and Inhibition by Cortical Circuitry. Neuron 97:1341–1355 e1346
Nagel G, Szellas T, Huhn W, Kateriya S, Adeishvili N, Berthold P, Ollig D, Hegemann P, Bamberg E (2003) Channelrhodopsin-2, a directly light-gated cation-selective membrane channel. Proc Natl Acad Sci U S A 100:13940–13945
Newman CW, Wharton JA, Shivapuja BG, Jacobson GP (1994) Relationships among psychoacoustic judgments, speech understanding ability and self-perceived handicap in tinnitus subjects. Audiology 33:47–60
Newman CW, Jacobson GP, Spitzer JB (1996) Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg 122:143–148
Norena AJ (2011) An integrative model of tinnitus based on a central gain controlling neural sensitivity. Neurosci Biobehav Rev 35:1089–1109
Norena A, Cransac H, Chery-Croze S (1999) Towards an objectification by classification of tinnitus. Clin Neurophysiol 110(4):666–675
Omidvar S et al (2016) The relationship between ultra-high frequency thresholds and transient evoked otoacoustic emissions in adults with tinnitus. Med J Islam Repub Iran 30:449
Paglialonga A, Del Bo L, Ravazzani P, Tognola G (2010) Quantitative analysis of cochlear active mechanisms in tinnitus subjects with normal hearing sensitivity: multiparametric recording of evoked otoacoustic emissions and contralateral suppression. Auris Nasus Larynx 37:291–298
Pan T, Tyler RS, Ji H, Coelho C, Gehringer AK, Gogel SA (2009) The relationship between tinnitus pitch and the audiogram. Int J Audiol 48:277–294
Paul BT, Bruce IC, Roberts LE (2017) Evidence that hidden hearing loss underlies amplitude modulation encoding deficits in individuals with and without tinnitus. Hear Res 344:170–182
Pierzycki RH, McNamara AJ, Hoare DJ, Hall DA (2016) Whole scalp resting state EEG of oscillatory brain activity shows no parametric relationship with psychoacoustic and psychosocial assessment of tinnitus: a repeated measures study. Hear Res 331:101–108
Pinheiro ES et al (2016) Electroencephalographic patterns in chronic pain: a systematic review of the literature. PLoS One 11:e0149085
Pinto PC et al (2014) Tinnitus and its association with psychiatric disorders: systematic review. J Laryngol Otol 128:660–664
Rauschecker JP, Leaver AM, Muhlau M (2010) Tuning out the noise: limbic-auditory interactions in tinnitus. Neuron 66:819–826
Rauschecker JP, May ES, Maudoux A, Ploner M (2015) Frontostriatal gating of tinnitus and chronic pain. Trends Cogn Sci 19:567–578
Reed GF (1960) An audiometric study of two hundred cases of subjective tinnitus. AMA Arch Otolaryngol 71:84–94
Riga M, Papadas T, Werner JA, Dalchow CV (2007) A clinical study of the efferent auditory system in patients with normal hearing who have acute tinnitus. Otol Neurotol 28:185–190
Ryu IS, Ahn JH, Lim HW, Joo KY, Chung JW (2012) Evaluation of masking effects on speech perception in patients with unilateral chronic tinnitus using the hearing in noise test. Otol Neurotol 33:1472–1476
Sarnthein J, Jeanmonod D (2007) High thalamocortical theta coherence in patients with Parkinson's disease. J Neurosci 27:124–131
Schaette R, Kempter R (2006) Development of tinnitus-related neuronal hyperactivity through homeostatic plasticity after hearing loss: a computational model. Eur J Neurosci 23:3124–3138
Schaette R, McAlpine D (2011) Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. J Neurosci 31:13452–13457
Schecklmann M, Vielsmeier V, Steffens T, Landgrebe M, Langguth B, Kleinjung T (2012) Relationship between audiometric slope and tinnitus pitch in tinnitus patients: insights into the mechanisms of tinnitus generation. PLoS One 7:e34878
Schecklmann M, Landgrebe M, Langguth B, T. R. I. D. S. Group (2014) Phenotypic characteristics of hyperacusis in tinnitus. PLoS One 9:e86944
Schlee W, Weisz N, Bertrand O, Hartmann T, Elbert T (2008). Using auditory steady state responses to outline the functional connectivity in tinnitus brain. PLoS One 3(11):e3720
Schurger A, Sarigiannidis I, Naccache L, Sitt JD, Dehaene S (2015) Cortical activity is more stable when sensory stimuli are consciously perceived. Proc Natl Acad Sci U S A 112:E2083–E2092
Sedley W, Friston KJ, Gander PE, Kumar S, Griffiths TD (2016) An integrative tinnitus model based on sensory precision. Trends Neurosci 39:799–812
Seidman MD, Jacobson GP (1996) Update on tinnitus. Otolaryngol Clin N Am 29:455–465
Sereda M, Hall DA, Bosnyak DJ, Edmondson-Jones M, Roberts LE, Adjamian P, Palmer AR (2011) Re-examining the relationship between audiometric profile and tinnitus pitch. Int J Audiol 50:303–312
Seydell-Greenwald A, Leaver AM, Turesky TK, Morgan S, Kim HJ, Rauschecker JP (2012) Functional MRI evidence for a role of ventral prefrontal cortex in tinnitus. Brain Res 1485:22–39
Shargorodsky J, Curhan GC, Farwell WR (2010) Prevalence and characteristics of tinnitus among US adults. Am J Med 123:711–718
Shekhawat GS, Searchfield GD, Stinear CM (2014) The relationship between tinnitus pitch and hearing sensitivity. Eur Arch Otorhinolaryngol 271:41–48
Sheldrake J, Diehl PU, Schaette R (2015) Audiometric characteristics of hyperacusis patients. Front Neurol 6:105
Shim HJ, Kim SK, Park CH, Lee SH, Yoon SW, Ki AR et al (2009) Hearing abilities at ultra-high frequency in patients with tinnitus. Clin Exp Otorhinolaryngol 2(4):169
Shiomi Y, Tsuji J, Naito Y, Fujiki N, Yamamoto N (1997) Characteristics of DPOAE audiogram in tinnitus patients. Hear Res 108:83–88
Shore SE, Roberts LE, Langguth B (2016) Maladaptive plasticity in tinnitus - triggers, mechanisms and treatment. Nat Rev Neurol 12:150–160
Sillito AM, Jones HE (2002) Corticothalamic interactions in the transfer of visual information. Philos Trans R Soc Lond Ser B Biol Sci 357:1739–1752
Silva LR, Amitai Y, Connors BW (1991) Intrinsic oscillations of neocortex generated by layer 5 pyramidal neurons. Science 251:432–435
Singh S, Munjal SK, Panda NK (2011) Comparison of auditory electrophysiological responses in normal-hearing patients with and without tinnitus. J Laryngol Otol 125:668–672
Soleimani R, Jalali MM, Hasandokht T (2016) Therapeutic impact of repetitive transcranial magnetic stimulation (rTMS) on tinnitus: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 273:1663–1675
Steriade M (1998) Corticothalamic networks, oscillations, and plasticity. Adv Neurol 77:105–134
Steriade M, Contreras D (1995) Relations between cortical and thalamic cellular events during transition from sleep patterns to paroxysmal activity. J Neurosci 15:623–642
Steriade M, McCormick DA, Sejnowski TJ (1993) Thalamocortical oscillations in the sleeping and aroused brain. Science 262:679–685
Sztuka A, Pospiech L, Gawron W, Dudek K (2010) DPOAE in estimation of the function of the cochlea in tinnitus patients with normal hearing. Auris Nasus Larynx 37:55–60
Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, Archer SM, Blakley BW, Carter JM, Granieri EC, Henry JA, Hollingsworth D, Khan FA, Mitchell S, Monfared A, Newman CW, Omole FS, Phillips CD, Robinson SK, Taw MB, Tyler RS, Waguespack R, Whamond EJ (2014) Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg 151:S1–S40
Tyler RS, Pienkowski M, Roncancio ER, Jun HJ, Brozoski T, Dauman N, Coelho CB, Andersson G, Keiner AJ, Cacace AT, Martin N, Moore BCJ (2014) A review of hyperacusis and future directions: part I. Definitions and manifestations. Am J Audiol 23:402–419
Vanneste S, De Ridder D (2016) Deafferentation-based pathophysiological differences in phantom sound: tinnitus with and without hearing loss. Neuroimage 129:80–94
Vernon JA, Meikle MB (2003) Tinnitus: clinical measurement. Otolaryngol Clin N Am 36:293–305, vi
von Krosigk M, Bal T, McCormick DA (1993) Cellular mechanisms of a synchronized oscillation in the thalamus. Science 261:361–364
von Krosigk M, Monckton JE, Reiner PB, McCormick DA (1999) Dynamic properties of corticothalamic excitatory postsynaptic potentials and thalamic reticular inhibitory postsynaptic potentials in thalamocortical neurons of the Guinea-pig dorsal lateral geniculate nucleus. Neuroscience 91:7–20
Warren RA, Agmon A, Jones EG (1994) Oscillatory synaptic interactions between ventroposterior and reticular neurons in mouse thalamus in vitro. J Neurophysiol 72:1993–2003
Weinbruch C, Paul I, Weisz N, Elbert T, Roberts LE (2006). Frequency organization of the 40-Hz auditory steady-state response in normal hearing and in tinnitus. Neuroimage 33(1):180–194
Weisz N, Voss S, Berg P, Elbert T (2004) Abnormal auditory mismatch response in tinnitus sufferers with high-frequency hearing loss is associated with subjective distress level. BMC Neurosci 5:8
Weisz N, Muller S, Schlee W, Dohrmann K, Hartmann T, Elbert T (2007) The neural code of auditory phantom perception. J Neurosci 27:1479–1484
Welling DB, Jackler RK (2018) Reflections on the last 25 years of the American Otological Society and thoughts on its future. Otol Neurotol 39:S81–S94
Wojtczak M, Beim JA, Oxenham AJ (2017) Weak middle-ear-muscle reflex in humans with noise-induced tinnitus and Normal hearing May reflect Cochlear Synaptopathy. eNeuro 4:ENEURO.0363–ENEU17.2017
Yamawaki N, Shepherd GM (2015) Synaptic circuit organization of motor corticothalamic neurons. J Neurosci 35:2293–2307
Yang S, Weiner BD, Zhang LS, Cho SJ, Bao S (2011) Homeostatic plasticity drives tinnitus perception in an animal model. Proc Natl Acad Sci U S A 108:14974–14979
Yu KK, An YH, Won JH, Shim HJ, Yoon SW (2014) Influence of Tinnitus on Auditory Spectral, Temporal Resolution, and Speech Perception Ability in Tinnitus Patients. Otolaryngol Head Neck Surg 151(1_suppl):P210–P210
Zhou J, Shore S (2004) Projections from the trigeminal nuclear complex to the cochlear nuclei: a retrograde and anterograde tracing study in the Guinea pig. J Neurosci Res 78:901–907
Zhou J, Shore S (2006) Convergence of spinal trigeminal and cochlear nucleus projections in the inferior colliculus of the Guinea pig. J Comp Neurol 495:100–112
Acknowledgements
We thank Drs. Dean Salisbury, Avniel Ghuman, Chris Brown, Bharath Chandrasekaran, Maria Rubio, Barbara Shinn-Cunningham and Karl Kandler for their helpful discussions.
Funding
This work was supported by US Department of Defense grant W81XWH-14-1-0117 and NIH grant R01-DC007905 (both grants to T.T.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tzounopoulos, T., Balaban, C., Zitelli, L. et al. Towards a Mechanistic-Driven Precision Medicine Approach for Tinnitus. JARO 20, 115–131 (2019). https://doi.org/10.1007/s10162-018-00709-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10162-018-00709-9