Abstract
Laboratory studies often rely on a damaging sound exposure to induce tinnitus in animal models. Because the time course and ultimate success of the induction process is not known in advance, it is not unusual to maintain sound-exposed animals for months while they are periodically assessed for behavioral indications of the disorder. To demonstrate the importance of acoustic environment during this period of behavioral screening, sound-exposed rats were tested for tinnitus while housed under quiet or constant noise conditions. More than half of the quiet-housed rats developed behavioral indications of the disorder. None of the noise-housed rats exhibited tinnitus behavior during 2 months of behavioral screening. It is widely assumed that the “phantom sound” of tinnitus reflects abnormal levels of spontaneous activity in the central auditory pathways that are triggered by cochlear injury. Our results suggest that sustained patterns of noise-driven activity may prevent the injury-induced changes in central auditory processing that lead to this hyperactive state. From the perspective of laboratory studies of tinnitus, housing sound-exposed animals in uncontrolled noise levels may significantly reduce the success of induction procedures. From a broader clinical perspective, an early intervention with sound therapy may reduce the risk of tinnitus in individuals who have experienced an acute cochlear injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The most common form of human hearing loss in modern society is cochlear injury from damaging sound exposures (Rabinowitz 2012). The central auditory system compensates an impaired cochlea by altering the sensitivity and selectivity of sound-driven activity (Salvi et al. 2000; Cai et al. 2009; Middleton et al. 2011; Brotherton et al. 2015; Li et al. 2015; Heeringa and van Dijk 2016; Eggermont 2017). Injury-induced changes in the gain of auditory processing may generate abnormally high rates of spontaneous activity in the absence of sound stimulation (Szczepaniak and Moller 1996; Robertson et al. 2013; Caspary and Llano 2017). This hyperactive state is widely assumed to underlie the false perception of sound that is experienced by individuals with tinnitus (Zhang and Kaltenbach 1998; Kaltenbach and Godfrey 2008).
The neurophysiological basis of tinnitus is typically investigated with animal models that begin with a damaging sound exposure, advance through behavioral verification of tinnitus status (Heffner and Harrington 2002; Turner 2007b; Brozoski and Bauer 2016; Jones and May 2017), and end with an electrophysiological characterization of tinnitus-related neural activity (Kaltenbach et al. 2004; Ma et al. 2006; Munguia et al. 2013). Because the onset of the disorder is not known in advance, several months of post-exposure behavioral screening may elapse before the electrophysiological experiment. During our previous tinnitus studies (Ma et al. 2006; Ropp et al. 2014; Li et al. 2015), we noticed that the success of our induction method was strongly influenced by the facilities in which animals were housed.
It is our practice to maintain behaviorally trained rats in restricted facilities to control access to food and water, as well as ambient noise levels. When our capacity for laboratory housing was exceeded by ongoing electrophysiological studies (Ropp et al. 2014; Li et al. 2015), sound-exposed rats were placed in institutional rodent facilities for a 2-month period of behavioral screening. The change in housing coincided with a striking decrease in the number of positive tinnitus tests that we routinely observe with our induction procedures.
Most institutional rodent facilities place a premium on housing the maximum number of animals in the minimum space. This objective is achieved at the cost of the ambient noise that is associated with increased investigator activity and high-velocity air exchange systems (Lauer et al. 2009). We hypothesized that the louder noise levels in our high-density institutional facilities disrupted the induction of tinnitus behavior by increasing sound-driven activity in the central auditory pathways. Acoustic stimulation has been previously proposed as a mechanism for reversing the injury-induced homeostatic plasticity that leads to tinnitus-related hyperactivity (Schaette and Kempter 2006).
To test this hypothesis, two groups of rats were given identical sound exposures, then placed in a quiet or constant noise environment. Over the next 2 months, the rats were periodically tested with a behavioral assay that was designed to reveal the presence of tinnitus. Positive tinnitus tests were observed in more than half of the rats in the quiet environment, but none of the rats in the noise environment. These results suggest that the predictions of current neurophysiological models can be extended beyond neural hyperactivity to perceptual behavior (Schaette and Kempter 2006; Norena 2011). Regardless of the underlying mechanism, the elimination of tinnitus in our behavioral model confirms the powerful effects of acoustic stimulation on the immediate stages of tinnitus induction. For animal models of tinnitus, the effects of noise must be controlled because they compromise conventional testing procedures. For the clinical treatment of tinnitus, sound therapy represents a potential strategy for reducing the risk of the disorder after acoustic injury.
METHODS
Subjects
Experiments were performed on 18 male Sprague-Dawley rats that were obtained from Harlan Laboratories (now Envigo) at approximately 2 months of age (225–250 g). All of the rats were first trained with a conditioned suppression task and then exposed to a damaging sound. Immediately after the sound exposure, the rats were divided into a quiet-treatment group (N = 9) that was housed in a low ambient noise environment, or a noise-treatment group (N = 9) that was housed in a high ambient noise environment. Both groups were tested for behavioral indications of tinnitus at varying time intervals after the sound exposure. Behavioral assessments were stopped when a rat produced a positive test or showed no signs of tinnitus after 2 months of testing. Results from quiet-treatment rats were previously reported (Jones and May 2017).
The rats were housed for the duration of behavioral testing in laboratory facilities to allow precise control of ambient sound levels. They were given free access to food but restricted access to water to promote high rates of drinking during behavioral tests. After the rats learned to drink from a contact-sensitive spout in the behavioral apparatus, the water source was removed from the home cages. On days when the rats were not tested, water-infused gel packs were placed in the cages. The amount of water earned during behavioral sessions was monitored to ensure that the rats received a sufficient daily water allotment. The complete details of our behavioral methods are presented in Jones and May (2017). All procedures were reviewed and approved by the Institutional Animal Care and Use Committee of The Johns Hopkins University School of Medicine.
Apparatus
Behavioral tests were conducted inside a double-walled, sound-attenuating chamber (Industrial Acoustics Company). The interior walls, ceiling, and floor of the chamber were lined with anechoic foam to control reflections. An operant conditioning box was positioned near the center of the chamber. A contact-sensitive spout protruded from the front wall of the box to deliver water or electrical shocks, depending on the current reinforcement contingency. Contact with the spout delivered water when a speaker in front of the box was silent. It delivered shocks when the speaker was presenting sound.
Warning Sound Training
Warning sound training began by rewarding licking behavior with water when the testing environment was silent. The water delivery system was turned off during intermittent presentations of broadband noise (BBN, 50-kHz bandwidth, 50 dB SPL). The duration of each noise presentation gradually increased over the initial training days until water was only available during silent “safe trials” that occurred at random intervals throughout the session.
After the rats learned to acquire water from the spout during safe trials, drinking in the presence of sound was suppressed by adding “warning” trials to the behavioral procedure. When the rats contacted the spout during a warning trial, a mild shock was delivered through the spout. The initial warning trial stimulus was BBN (50-kHz bandwidth, 50 dB SPL). Because warning trials were indistinguishable from the background noise that was present between trials, the rats learned to avoid shocks by contacting the spout only when the speaker was silent.
At the completion of warning sound training, silence elicited high lick rates because it was associated with water rewards. BBN suppressed lick rates because it was associated with shocks. To separate the conditioned response (CR) to silence and BBN from the unconditioned response (UCR) to water or shocks, the spout was inactive for a variable interval at the beginning of each trial (3.5–6 s). Upon activation, the spout delivered water or shocks with each contact for 15 s. Our analysis of conditioned suppression was based on lick rates that were elicited by silence and BBN prior to the delivery of water or shocks.
Figure 1 summarizes the warning sound training of a representative rat. The upper panel displays peri-stimulus time histograms of lick rates that were observed during a training session with BBN warning trials and silent safe trials. Lick histograms were produced by dividing trial intervals into contiguous 20-ms bins. Each bin was assigned a score of 1 if the rat made contact with the spout during the time window, or 0 if the rat avoided the spout. The sequence of bin scores was aligned to the onset of the UCS, which is designated time 0 s in Fig. 1. All of the bin scores for the same stimulus condition were summed, then converted to an average lick rate by dividing by the summed bin duration (i.e., 20 ms × the number of trials).
Acquisition of conditioned suppression. The upper plot illustrates the temporal pattern of drinking for a representative rat. The conditioned response to silent safe trials (open circles) and broadband noise warning trials (BBN, filled circles) is measured during the 2.5-s interval immediately preceding the delivery of water or shocks (gray region). The lower plot shows the progressive separation of conditioned responses to sound and silence as the rat learned to avoid the spout during warning trials. Pure-tone warning trials were added when the rat reached stable performance for BBN warning trials
Lick histograms were partitioned into three segments to examine the following trial dynamics: the initial approach, conditioned responses (CR) to silence or BBN before the delivery of water or shocks, and unconditioned responses (CR + UCR) during reinforcement with water or shocks. The CS remained on for the entire trial period.
The binned lick rates in the CR segment have been converted to a global average (gray region, symbols) to estimate the magnitude of conditioned suppression in a sampling window that begins after rats have had time to reach the spout and ends before the unconditioned stimulus is delivered. Rats drink continuously when water becomes available, and not at all when shocks are delivered.
The lower panel of Fig. 1 shows the effects of training on the average CR lick rates of the rat. Session #1 is the first session that delivered shocks when the rat contacted the spout during BBN warning trials. Acquisition of the conditioned suppression task is indicated by a progressive increase in licking during silent safe trials and decline in licking during BBN warning trials.
After BBN warning trials began to produce high suppression rates (session #10), the set of warning sounds was expanded to include pure tones (frequencies = 8, 12, 16, 22 kHz; 70 dB SPL). Although the rat immediately generalized suppression behavior to this new class of warning sound, training with BBN and pure tones was extended to session #23 to increase lick rates during safe trials and to improve overall stability.
Unilateral Sound Exposure
Rats were sound exposed after they completed warning sound training. In our experience, the damaging effects of sound exposure are more consistent when the procedure is performed without anesthesia using free-field sound. The rats were caged at a calibrated location inside a sound-attenuating chamber and rotated around a horizontal axis to minimize the potential effects of location-dependent acoustic nulls. Two high-output tweeters (Pyramid TW57) delivered a continuous 16-kHz tone at a peak level of 116 dB SPL. The stimulus was gradually increased to the peak level over 60 s, and then maintained for the remainder of the 2-h exposure.
One ear was plugged to preserve hearing for subsequent behavioral testing. The foam plug (EAR, 3 M) attenuated sound frequencies above 10 kHz by approximately 55 dB (Jones and May 2017). Auditory brainstem responses (ABRs) were used to measure the magnitude and frequency of threshold shifts in the unprotected ear and verified the preservation of normal hearing in the protected ear. ABRs were collected at least 1 week after the sound exposure to minimize the effects of temporary threshold shifts.
Details of our ABR recording methods have been previously described (Ngan and May 2001; May et al. 2011). Briefly, the rats were anesthetized (ketamine 40: xylazine 10 mg/kg), fitted with subcutaneous electrodes, and placed inside an electrically shielded sound-attenuating chamber. The test ear was directed toward a speaker on the ceiling of the chamber (Fostex FT28D). The opposite ear was plugged and oriented toward the floor of the chamber.
Differential recordings were obtained with electrodes placed on the left pinna (inverting), dorsal midline of the skull (non-inverting), and the left hind leg (ground). Pure tones (5-ms duration, 0.5 ms rise/fall times) were presented at a rate of 10 pulses/s. The electrode signal was amplified, filtered from 300 to 3000 Hz, digitized, and averaged over 300 repetitions. The peak-to-peak magnitude of the ABR signal was measured in a 5-ms window that began 1 ms after stimulus onset. The peak-to-peak magnitude of the recording’s noise floor was measured in a 5-ms window that began 25 ms after stimulus onset. Threshold was defined as the stimulus level that produced an ABR magnitude 2 SDs above the noise floor.
Immediate Acoustic Intervention
The acoustic intervention began immediately after sound exposure. Based on previous acoustic measures in our high-density institutional rodent facilities (Lauer et al. 2009), we hypothesized unstructured BBN would be an effective treatment stimulus. Nine rats were placed in a sound isolation chamber where they were housed in constant BBN. The remaining nine rats were left in quiet laboratory facilities. These two groups are designated noise-treatment and quiet-treatment rats.
Ambient noise levels in the two treatment environments are shown in Fig. 2. The BBN treatment waveform was produced with an analog noise generator (50-kHz bandwidth), amplified, and delivered to a wide-range tweeter on the ceiling of the noise chamber (Fostex FT28D). The output of the speaker was calibrated by placing the microphone of a sound level meter in the empty housing cage. Peak spectrum levels (30–35 dB SPL/Hz) were recorded at frequencies between 3 and 10 kHz. Spectrum levels remained above 20 dB SPL for frequencies up to 20 kHz, which was the upper frequency limit of our meter. Given the neural thresholds that we routinely observe in Sprague-Dawley rats (Cai et al. 2009; Ropp et al. 2014; Li et al. 2015), the high-frequency components of the treatment stimulus were expected to be clearly audible in the protected ear, but not distressingly loud. Previous studies have shown that long-term exposure to similar sound levels do not damage the organ of Corti (Canlon and Fransson 1995) or elevate ABR thresholds (Norena and Eggermont 2006; Tanaka et al. 2009; Zhou and Merzenich 2012; Ngodup et al. 2015).
Ambient noise levels for quiet treatment were approximately 25 dB below levels for constant BBN treatment at frequencies where Sprague-Dawley rats show sensitive hearing (Kelly and Masterton 1977). The noise levels in our quiet facilities are strongly biased toward low frequencies by the sound of moving air in the room’s ventilation system. Because our laboratory houses a relatively small number of animals, the air exchange rate is lower and therefore much quieter than what is observed in high-density institutional rodent facilities.
Safe Sound Training
Safe sound training began the day after sound exposure. This training was simply a reinstatement of the initial training protocol with silent safe trials and BBN warning trials. Training with the pure-tone warning sounds was stopped.
While previously learned stimulus-response relationships remained unchanged in rats that did not develop tinnitus, rats with tinnitus were required to learn a new class of “safe sound” behavior because they experienced the sound of their own tinnitus during silent safe trials. The basic assumption of our tinnitus test is that the subject’s tendency to drink in the presence of tinnitus will generalize to objective sounds that share salient perceptual features.
Tinnitus Test
The effects of safe sound training on conditioned suppression were evaluated by re-introducing pure tones as generalization probes (frequencies = 8, 12, 16, 22 kHz; 70 dB SPL). Tinnitus-positive rats were expected to classify some probes as safe sounds because they shared pitch properties of the tinnitus percept. Consequently, safe sound classification is revealed by a frequency-dependent loss of conditioned suppression. Tinnitus-negative rats were expected to maintain suppression behavior at all probe frequencies.
The tinnitus test was designed to measure the combined effects of initial warning sound training and post-exposure safe sound training without modifying those previously learned classifications. Like the CS training stimuli, test tone probes remained on throughout the trial period, but the responses elicited by these stimuli were neither rewarded with water nor suppressed with shocks during the UCR interval. Silent safe trials and BBN warning trials retained their previous contingencies of reinforcement. These maintenance trials were presented with higher probability than probe trials to enforce suppression behavior.
Tinnitus tests were repeated no more than once a week as another method to minimize the effects of testing on training. Training sessions with silent safe trials and BBN warning trials were conducted on the remaining days. Rats that showed behavioral indications of tinnitus were assigned a tinnitus-positive status and removed from behavioral testing. Rats that failed to show tinnitus behavior were tested for at least 2 months before being assigned a tinnitus-negative status.
The behavioral performances of a representative rat from each treatment group are compared in Fig. 3. The plots are identical to Fig. 1, except that the unreinforced responses to pure-tone probes are now presented (gray region, red symbols).
Examples of tinnitus tests in the quiet-treatment and noise-treatment groups. Symbols indicate the conditioned response to BBN warning trials, silent safe trials, and unreinforced probe trials. Numerical labels indicate probe frequency (8, 12, 16, 22 kHz). Rats were assigned a positive tinnitus status when a probe elicited lick rates that approximated responses to silent safe trials (rat 127, 16 kHz)
When tested with 8-, 12-, and 22-kHz probes, the quiet-treatment rat (upper panel) exhibited suppression effects that were equivalent to those observed during BBN warning trials. These responses suggest that the warning sound classification was not altered during safe sound training. When tested with 16-kHz probes, the rat showed lick rates that were more closely associated with responses to silent safe trials. This frequency-dependent loss of suppression indicates a positive tinnitus test. Moreover, we can infer that the rat was experiencing a tone-like tinnitus with a pitch near 16 kHz. The noise-treatment rat (lower panel) exhibited strong suppression for all probe frequencies, indicating a negative tinnitus test.
RESULTS
Effects of Sound Exposure on ABR Thresholds
Figure 4 shows representative click-evoked ABRs for quiet-treatment and noise-treatment rats. For this comparison, rats with matching hearing loss have been selected to remove the effects of threshold from the waveforms. The protected ears of the two rats produced thresholds of 30.6 (quiet) and 33.1 (noise) dB SPL. The exposed ears produced thresholds of 42.3 and 40.1 dB SPL. When threshold differences are removed in this manner, the acoustic intervention had no discernable effects on waveform magnitude, latency, and shape. Further analyses of the input/output functions of discrete ABR waves (e.g., comparisons of changes in waves 1 to 5) may reveal important insights into the auditory structures that contribute to the therapeutic effects of background noise. Unfortunately, our ABR measures are too strongly biased toward near-threshold sound levels to support a systematic analysis of functional changes over the dynamic range of hearing.
Click-evoked auditory brainstem responses (ABRs) for representative rats in the quiet-treatment and noise-treatment groups. The rats have been matched in terms of thresholds in the protected ear (left panel) and unprotected ear (right panel). For illustrative purposes, signal levels have been selected to show the full dynamic range of responses
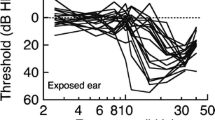
Figure 5 presents the post-exposure audiograms of quiet-treatment and noise-treatment rats. Hearing loss was calculated by comparing the absolute ABR threshold at multiple tone frequencies to the average ABR threshold of our large sample of unexposed Sprague-Dawley rats (N = 174). The audiograms from protected ears show thresholds that remained within 20 dB of normal hearing levels (lower panels). These results confirm that our ear plugging procedure preserved hearing for post-exposure behavioral testing. In addition, they reveal no adverse effects of the acoustic intervention on the protected ears of noise-treated rats (Norena and Eggermont 2006; Tanaka et al. 2009; Zhou and Merzenich 2012).
Auditory brainstem response (ABR) audiograms of unilaterally sound-exposed rats. Audiograms plot absolute thresholds at each frequency relative to the average threshold of 174 unexposed ears. Results from the quiet-treatment group (N = 9) and noise-treatment group (N = 9) are compared in the left and right columns. Exposed and protected ears are compared in the upper and lower panels
The audiograms from exposed ears (upper panels) were marked by a sharp transition from normal to impaired thresholds. A striking difference between the two treatment groups was the magnitude and frequency location of hearing loss. Quiet-treatment rats showed considerable variation in both metrics. Noise-treatment rats showed remarkable consistency.
Figure 6 presents a quantitative analysis of exposed-ear audiograms. The transition from normal to impaired thresholds is defined as the EDGE frequency of hearing loss (Ropp et al. 2014), which is the midpoint between the two adjacent frequencies that produced the maximum negative slope in the audiogram. Box plots of the distribution of EDGE frequencies (upper panel) reveal an expanded representation of high-frequency sounds among quiet-treatment rats. The difference in the log-transformed EDGE frequency between treatment groups was statistically significant (MATLAB t test for unknown and unequal variances, t(12.6) = 2.21, P = 0.047.
Box plots comparing the distribution of EDGE frequencies (upper panel) and maximum threshold shifts (lower panel) for the exposed ears of rats in the quiet-treatment and noise-treatment groups. The upper and lower limits of the boxes indicate the interquartile range of the distribution (1–3 quartile range). The line bisecting the box indicates the median. Error bars (“whiskers”) represent the highest and lowest values that fall within the ± 1.5 interquartile range. Outliers are plotted as individual symbols
Boxplots of maximum threshold shifts (lower panel) suggest that noise treatment was associated with reduced hearing sensitivity. Most of the rats in the noise-treatment group showed maximum threshold shifts that were greater than 60 dB, which is near the limits of measurable hearing loss in the exposed ear of unilaterally deafened animals. Louder stimulus levels evoke responses from the more sensitive protected ear even when it is plugged. Most of the rats in the quiet-treatment group showed maximum threshold shifts that were less than 60 dB, with some rats producing thresholds within 40 dB of normal baselines. The difference in maximum threshold shift between groups was statistically significant (MATLAB t test for unknown and unequal variances, t(10.48) = 2.60, P = 0.025).
Effects of Acoustic Intervention on Tinnitus Behavior
The presence of a tinnitus percept was inferred when rats generalized safe sound behavior to a subset of pure-tone probes. This frequency-dependent loss of suppression was quantified by converting CR lick rates to a tinnitus score. The calculation is described by Eq. 1, where CRprobe is the conditioned response to the probe, CRwarning is the conditioned response to BBN warning trials, and CRsafe is the conditioned response to silent safe trials.
Tinnitus scores approach 1 when responses to a probe equal responses to safe trials. Tinnitus scores remain near 0 when responses to a probe equal responses to warning trials. Therefore, a high tinnitus score indicates the loss of conditioned suppression during post-exposure training. Table 1 summarizes the post-exposure tinnitus scores of all rats in the two treatment groups.
Figure 7 describes the magnitude and frequency selectivity of tinnitus scores in the two treatment groups. The peak tinnitus score (upper panel) is the highest score produced by each rat regardless of probe frequency. This behavioral correlate of tinnitus magnitude was significantly lower in the noise-treatment group (t(14.00) = 2.69, P = 0.018).
Peak tinnitus scores in the quiet-treatment group were often elicited by 16-kHz probes (Table 1, shaded cells). This selectivity is graphically depicted by the frequency profiles in Fig. 7 (lower panel). The profiles relate the mean tinnitus scores (± 95 % confidence intervals) of the two treatment groups to probe frequency. Rats in the quiet-treatment group produced a profile with a prominent peak at 16 kHz. Rats in the noise-treatment group produced a featureless profile. The effect of probe frequency was statistically significant (repeated measures ANOVA, F(3) = 5.98, P = 0.002), as was the interaction between frequency and treatment (F(3) = 4.08, P = 0.012).
The frequency profiles of the quiet-treatment group show large variability at the 16-kHz peak response. This variation implies that the rats did not experience a uniform tinnitus magnitude. In Fig. 8, the individual profiles of all subjects in both treatment groups have been assigned to the three most common patterns of generalization behavior by a statistical cluster analysis of the tinnitus scores at each probe frequency and overall peak magnitude (MATLAB, linkage and dendrogram functions).
Summary of tinnitus testing in individual rats. Frequency profiles were interpreted as a positive (upper panel), ambiguous (middle panel), or negative test (lower panel) based on the peak tinnitus score. Dashed lines indicate the criteria for classification. Legends report the number of rats in each treatment group that received the classification
One prototype was characterized by profiles with a prominent peak at 16 kHz and peak scores that exceeded 0.55 (upper panel). This pattern is interpreted as a positive test for a tinnitus pitch near 16 kHz. Most rats in the quiet-treatment group (5/9) produced a profile that was assigned to the tinnitus-positive prototype. None of the rats in the noise-treatment group met the criteria for this classification.
A second prototype was defined by featureless profiles and peak scores that fell below 0.26 (lower panel). The perseveration of suppression at all probe frequencies is interpreted as a negative tinnitus test. Most rats in the noise-treatment group (6/9) produced profiles that were classified as tinnitus-negative prototypes. Relatively few of the rats in the quiet-treatment group (2/9) were assigned to this classification.
The third prototype displayed a mix of profile shapes and intermediate tinnitus scores (middle panel). The absence of a consistent peak score makes it impossible to assign a uniform tinnitus pitch or magnitude to this classification. Ambiguous profiles were produced by a minority of rats in both treatment groups.
DISCUSSION
The essential finding of our study is that noise treatment prevented the onset of tinnitus behavior in sound-exposed rats. The environmental manipulation began immediately after sound exposure and continued without interruption for 2 months of behavioral testing. The persistence of the therapeutic effect, optimum conditions of acoustic stimulation, and most efficient schedule of treatment remain to be determined.
Our acoustic intervention also altered patterns of hearing loss. These results suggest that injury-induced changes of central auditory gain may be responsible for tinnitus-related hyperactivity, as well as the recovery of hearing sensitivity after acoustic trauma. The role of homeostatic plasticity as a mechanism for tinnitus-related hyperactivity has been previously proposed by neurophysiological modeling studies (Schaette and Kempter 2006; Norena 2011). Similar mechanisms have been invoked to explain modifications of central processing in deaf individuals (Irvine and Rajan 1996; Norena and Eggermont 2005; Eggermont 2017). The dissociation of tinnitus (quiet-treatment rats) and increased hearing loss (noise-treatment rats) is evidence for the discrete nature of the two pathologies and their potential treatment with sound therapy.
The Neurophysiology of Tinnitus
Because the disordered outputs of a damaged cochlea terminate in the cochlear nucleus (Perkins and Morest 1975; Brown and Ledwith 3rd 1990), its ascending projections represent a primary conduit for the injury-induced changes in central auditory processing that have been associated with tinnitus. Tinnitus-related hyperactivity was first recorded in the dorsal subdivision of the nucleus (DCN)(Kaltenbach and McCaslin 1996), then isolated to its projection neurons (Brozoski et al. 2002). Subsequent studies have shown that peripheral damage to the auditory system also evokes hyperactivity in the ventral subdivisions of the cochlear nucleus (VCN)(Kraus et al. 2011; Vogler et al. 2011).
Surgical ablations have established the importance of DCN hyperactivity for the induction of tinnitus, but not necessarily the maintenance of an existing tinnitus condition. If the ascending projections of the DCN are destroyed before the cochlea is damaged, behavioral indications of tinnitus fail to develop (Brozoski et al. 2012). If the procedure is performed on animals that already exhibit tinnitus, the behaviors persist (Brozoski and Bauer 2005). These outcomes predict that acoustic interventions will be most effective if they target the DCN and begin before local pathologies advance to a global hyperactive state.
The major physiological response types of the auditory brainstem are defined by their distinctive responses to variations in stimulus frequency, level, and bandwidth (Young et al. 1988). These properties can be exploited to amplify or attenuate the effects of acoustic intervention on particular subdivisions or cellular populations of the cochlear nucleus. For example, narrowband sounds excite the projection neurons of the ventral subdivision but inhibit the projection neurons of the dorsal subdivision (Young and Brownell 1976). The failure of an intervention with pure tones would implicate the dorsal subdivision as an important generator site. Alternatively, BBN excites all of the major cellular populations in the cochlear nucleus (Young et al. 1988), making it an ideal stimulus for maximizing the success of treatment.
A comparison of our treatment conditions (Fig. 2) and exposed ear audiograms (Fig. 5) raises the question: Was the intervention loud enough to evoke noise-driven activity in the cochlear nucleus of the exposed ear? A direct comparison of these two metrics is somewhat misleading because single-unit thresholds tend to be lower than ABR thresholds (Ngan and May 2001), and noise-driven thresholds can differ substantially from tone-driven thresholds, especially when spectral integration properties are expanded by trauma (Ma and Young 2006; Cai et al. 2009). Nevertheless, it is intriguing to speculate that the benefits of sound therapy may have been achieved in the damaged DCN through its rich sources of descending input (Winter et al. 1989; Shore et al. 1991; Oertel and Young 2004), or in the damaged VCN through its commissural connections (Doucet et al. 2009). Unilateral sound exposure is an excellent paradigm for exploring these alternate pathways.
Implications for Existing Animal Models
Tinnitus investigators with limited experience in animal behavior must rely on screening procedures that have been independently validated by established behavioral laboratories. The lengthy process of behavioral validation usually involves a detailed examination of individual animals that are extensively trained and repeatedly tested (Klump et al. 1995). These valuable subjects are invariably maintained in restricted facilities with low ambient noise levels. The effects of our acoustic intervention suggest that quiet housing may be a subtle but critical factor for the success of the tinnitus models that are promoted by behavioral laboratories. Investigators seeking the successful implementation of those protocols should pay close attention not only to experimental methodology but also environmental context. The informal observations that prompted this study suggest that ambient noise levels in high-density rodent facilities are sufficient to invalidate current tinnitus models (Lauer et al. 2009; Gourevitch et al. 2014; Eggermont 2017).
Behavioral screening remains a major obstacle for the advancement of tinnitus research (Fournier and Hebert 2013; Jones and May 2017). Even the most rigorously tested animal models remain controversial or difficult to translate to the high-throughput demands of contemporary tinnitus research (Jastreboff and Sasaki 1994; Turner 2007a; Brozoski and Bauer 2016). At present, a behavioral analysis cannot be avoided because the success of induction is indeterminate. Environmental manipulations could reduce this uncertainty by introducing an intentional bias toward positive or negative yields. For example, the likelihood of successful induction was negligible for rats in our noise-treatment group. Rats housed in a silent environment might exhibit an even higher percentage of successful outcomes than rats in our quiet-treatment group. If environmentally enhanced induction methods produce only positive or negative outcomes, there is no longer a need for behavioral screening.
Clinical Implications
Our findings raise the possibility that prophylactic sound therapy may be able to prevent tinnitus or reduce its severity in individuals who have suffered a recent acoustic injury. While prolonged exposure to less extreme noise levels is the more common clinical condition, the severe acute acoustic injury used in the present study represents a significant health issue, particularly among military personnel (Yankaskas 2013; Yong and Wang 2015). These injuries are often incurred by young individuals with no prior history of hearing loss, making them excellent candidates for treatment.
It is unlikely that audiological patients would tolerate months of uninterrupted exposure to loud levels of acoustic stimulation. Additional laboratory studies are needed to optimize the stimulus conditions and schedule of our intervention. The robust approach used in the present study may prove to be excessive in terms of loudness and length of daily exposure. It is also important to ascertain: How long can treatment be delayed, is periodic treatment effective, and do benefits persist when treatment is terminated? Beyond clinical practicality, a better understanding of the critical periods for intervention may provide new insights into how the induction process is linked to specific events in the cascade of neurophysiological events that follow acoustic injury.
The transition from laboratory study to clinical practice may not be that challenging. It is already well established that the emotional response to an existing tinnitus condition can be managed through sound therapy (Jastreboff 2015), or the restoration of auditory function with hearing aids, sound generators, or cochlear implants (Tunkel et al. 2014). Our results suggest that similar methods could be used to deliver acoustic stimulation to individuals who have experienced a recent acoustic injury. For these patients, the goal of sound therapy is to prevent the disorder, not make it more manageable.
An unexpected consequence of our acoustic intervention was an increase in the magnitude and range of ABR threshold shifts in noise-treated rats. This expanded hearing loss appears to link tinnitus induction to the mechanisms that restore the gain of central auditory processing after acoustic injury (Salvi et al. 2000; Eggermont 2017). As a result, the benefits of sound therapy may be offset by deficits in the recovery of hearing sensitivity. An alternative, but equally troubling interpretation, is that prolonged treatment with broadband noise exacerbated the damaging effects of the sound exposure. In either instance, refinements of the stimulus conditions or timing of the intervention should be explored to minimize potential adverse effects.
Rats in the quiet-treatment group presumably showed less hearing loss than rats in the noise-treatment group because central auditory neurons increased their gain to compensate a weakened cochlear input. In addition to tinnitus-related hyperactivity, this enhanced excitability may lead to disturbances of loudness perception (Phillips and Carr 1998; May et al. 2009; Brotherton et al. 2015). Individuals that suffer from hyperacusis and misophonia become so sensitive to sounds that they are unable to tolerate everyday acoustic experience (Schwartz et al. 2011; Wallen et al. 2012). Like tinnitus, loudness perception disorders are treated with desensitization procedures that often involve prolonged exposure to therapeutic sounds (Vernon 1987; Aazh et al. 2014). If the disorders share a common underlying neuropathology, as hypothesized, acoustic interventions to prevent tinnitus may also reduce the occurrence of equally debilitating loudness disorders if they are introduced before the onset of overt perceptual disabilities.
References
Aazh H, McFerran D, Salvi R, Prasher D, Jastreboff M, Jastreboff P (2014) Insights from the First International Conference on hyperacusis: causes, evaluation, diagnosis and treatment. Noise Health 16(69):123–126. https://doi.org/10.4103/1463-1741.132100
Brotherton H, Plack CJ, Maslin M, Schaette R, Munro KJ (2015) Pump up the volume: could excessive neural gain explain tinnitus and hyperacusis? Audiol Neurootol 20(4):273–282. https://doi.org/10.1159/000430459
Brown MC, Ledwith JV 3rd (1990) Projections of thin (type-II) and thick (type-I) auditory-nerve fibers into the cochlear nucleus of the mouse. Hear Res 49(1-3):105–118. https://doi.org/10.1016/0378-5955(90)90098-A
Brozoski TJ, Bauer CA (2005) The effect of dorsal cochlear nucleus ablation on tinnitus in rats. Hear Res 206(1-2):227–236. https://doi.org/10.1016/j.heares.2004.12.013
Brozoski TJ, Bauer CA (2016) Animal models of tinnitus. Hear Res 338:88–97. https://doi.org/10.1016/j.heares.2015.10.011
Brozoski TJ, Bauer CA, Caspary DM (2002) Elevated fusiform cell activity in the dorsal cochlear nucleus of chinchillas with psychophysical evidence of tinnitus. J Neurosci 22(6):2383–2390
Brozoski TJ, Wisner KW, Sybert LT, Bauer CA (2012) Bilateral dorsal cochlear nucleus lesions prevent acoustic-trauma induced tinnitus in an animal model. J Assoc Res Otolaryngol 13(1):55–66. https://doi.org/10.1007/s10162-011-0290-3
Cai S, Ma WL, Young ED (2009) Encoding intensity in ventral cochlear nucleus following acoustic trauma: implications for loudness recruitment. J Assoc Res Otolaryngol 10(1):5–22. https://doi.org/10.1007/s10162-008-0142-y
Canlon B, Fransson A (1995) Morphological and functional preservation of the outer hair cells from noise trauma by sound conditioning. Hear Res 84(1-2):112–124. https://doi.org/10.1016/0378-5955(95)00020-5
Caspary DM, Llano DA (2017) Auditory thalamic circuits and GABAA receptor function: putative mechanisms in tinnitus pathology. Hear Res 349:197–207
Doucet JR, Lenihan NM, May BJ (2009) Commissural neurons in the rat ventral cochlear nucleus. J Assoc Res Otolaryngol 10(2):269–280. https://doi.org/10.1007/s10162-008-0155-6
Eggermont JJ (2017) Effects of long-term non-traumatic noise exposure on the adult central auditory system. Hearing problems without hearing loss. Hear Res 352:12–22
Eggermont JJ (2017) Acquired hearing loss and brain plasticity. Hear Res 343:176–190. https://doi.org/10.1016/j.heares.2016.05.008
Fournier P, Hebert S (2013) Gap detection deficits in humans with tinnitus as assessed with the acoustic startle paradigm: does tinnitus fill in the gap? Hear Res 295:16–23. https://doi.org/10.1016/j.heares.2012.05.011
Gourevitch B, Edeline JM, Occelli F, Eggermont JJ (2014) Is the din really harmless? Long-term effects of non-traumatic noise on the adult auditory system. Nat Rev Neurosci 15(7):483–491. https://doi.org/10.1038/nrn3744
Heeringa AN, van Dijk P (2016) The immediate effects of acoustic trauma on excitation and inhibition in the inferior colliculus: a Wiener-kernel analysis. Hear Res 331:47–56. https://doi.org/10.1016/j.heares.2015.10.007
Heffner HE, Harrington IA (2002) Tinnitus in hamsters following exposure to intense sound. Hear Res 170(1-2):83–95. https://doi.org/10.1016/S0378-5955(02)00343-X
Irvine DR, Rajan R (1996) Injury- and use-related plasticity in the primary sensory cortex of adult mammals: possible relationship to perceptual learning. Clin Exp Pharmacol Physiol 23(10-11):939–947. https://doi.org/10.1111/j.1440-1681.1996.tb01146.x
Jastreboff PJ (2015) 25 years of tinnitus retraining therapy. HNO 63(4):307–311. https://doi.org/10.1007/s00106-014-2979-1
Jastreboff PJ, Sasaki CT (1994) An animal model of tinnitus: a decade of development. Am J Otol 15(1):19–27
Jones A, May BJ (2017) Improving the reliability of tinnitus screening in laboratory animals. J Assoc Res Otolaryngol 18(1):183–195. https://doi.org/10.1007/s10162-016-0597-1
Kaltenbach JA, Godfrey DA (2008) Dorsal cochlear nucleus hyperactivity and tinnitus: are they related? Am J Audiol 17(2):S148–S161. https://doi.org/10.1044/1059-0889(2008/08-0004)
Kaltenbach JA, McCaslin DL (1996) Increases in spontaneous activity in the dorsal cochlear nucleus following exposure to high intensity sound: a possible neural correlate of tinnitus. Aud Neurosci 3(1):57–78
Kaltenbach JA, Zacharek MA, Zhang J, Frederick S (2004) Activity in the dorsal cochlear nucleus of hamsters previously tested for tinnitus following intense tone exposure. Neurosci Lett 355(1-2):121–125. https://doi.org/10.1016/j.neulet.2003.10.038
Kelly JB, Masterton B (1977) Auditory sensitivity of the albino rat. J Comp Physiol Psychol 91(4):930–936. https://doi.org/10.1037/h0077356
Klump GM, Dooling RJ, Fay RR, Stebbins WC (eds) (1995) Methods in comparative acoustics. Birkhauser Verlag, Basel
Kraus KS, Ding D, Jiang H, Lobarinas E, Sun W, Salvi RJ (2011) Relationship between noise-induced hearing-loss, persistent tinnitus and growth-associated protein-43 expression in the rat cochlear nucleus: does synaptic plasticity in ventral cochlear nucleus suppress tinnitus? Neuroscience 194:309–325. https://doi.org/10.1016/j.neuroscience.2011.07.056
Lauer AM, May BJ, Hao ZJ, Watson J (2009) Analysis of environmental sound levels in modern rodent housing rooms. Lab Anim (NY) 38(5):154–160. https://doi.org/10.1038/laban0509-154
Li Y, Ropp TJ, May BJ, Young ED (2015) Dorsal Cochlear nucleus of the rat: representation of complex sounds in ears damaged by acoustic trauma. J Assoc Res Otolaryngol 16(4):487–505. https://doi.org/10.1007/s10162-015-0522-z
Ma WL, Hidaka H, May BJ (2006) Spontaneous activity in the inferior colliculus of CBA/J mice after manipulations that induce tinnitus. Hear Res 212(1-2):9–21. https://doi.org/10.1016/j.heares.2005.10.003
Ma WL, Young ED (2006) Dorsal cochlear nucleus response properties following acoustic trauma: response maps and spontaneous activity. Hear Res 216-217:176–188. https://doi.org/10.1016/j.heares.2006.03.011
May BJ, Lauer AM, Roos MJ (2011) Impairments of the medial olivocochlear system increase the risk of noise-induced auditory neuropathy in laboratory mice. Otol Neurotol 32(9):1568–1578. https://doi.org/10.1097/MAO.0b013e31823389a1
May BJ, Little N, Saylor S (2009) Loudness perception in the domestic cat: reaction time estimates of equal loudness contours and recruitment effects. J Assoc Res Otolaryngol 10(2):295–308. https://doi.org/10.1007/s10162-009-0157-z
Middleton JW, Kiritani T, Pedersen C, Turner JG, Shepherd GM, Tzounopoulos T (2011) Mice with behavioral evidence of tinnitus exhibit dorsal cochlear nucleus hyperactivity because of decreased GABAergic inhibition. Proc Natl Acad Sci U S A 108(18):7601–7606. https://doi.org/10.1073/pnas.1100223108
Munguia R, Pienkowski M, Eggermont JJ (2013) Spontaneous firing rate changes in cat primary auditory cortex following long-term exposure to non-traumatic noise: tinnitus without hearing loss? Neurosci Lett 546:46–50. https://doi.org/10.1016/j.neulet.2013.04.048
Ngan EM, May BJ (2001) Relationship between the auditory brainstem response and auditory nerve thresholds in cats with hearing loss. Hear Res 156(1-2):44–52. https://doi.org/10.1016/S0378-5955(01)00264-7
Ngodup T, Goetz JA, McGuire BC, Sun W, Lauer AM, Xu-Friedman MA (2015) Activity-dependent, homeostatic regulation of neurotransmitter release from auditory nerve fibers. Proc Natl Acad Sci U S A 112(20):6479–6484. https://doi.org/10.1073/pnas.1420885112
Norena AJ (2011) An integrative model of tinnitus based on a central gain controlling neural sensitivity. Neurosci Biobehav Rev 35(5):1089–1109. https://doi.org/10.1016/j.neubiorev.2010.11.003
Norena AJ, Eggermont JJ (2005) Enriched acoustic environment after noise trauma reduces hearing loss and prevents cortical map reorganization. J Neurosci 25(3):699–705. https://doi.org/10.1523/JNEUROSCI.2226-04.2005
Norena AJ, Eggermont JJ (2006) Enriched acoustic environment after noise trauma abolishes neural signs of tinnitus. Neuroreport 17(6):559–563
Oertel D, Young ED (2004) What’s a cerebellar circuit doing in the auditory system? Trends Neurosci 27(2):104–110. https://doi.org/10.1016/j.tins.2003.12.001
Perkins RE, Morest DK (1975) A study of cochlear innervation patterns in cats and rats with the Golgi method and Nomarkski Optics. J Comp Neurol 163(2):129–158. https://doi.org/10.1002/cne.901630202
Phillips DP, Carr MM (1998) Disturbances of loudness perception. J Am Acad Audiol 9:371–379
Rabinowitz PM (2012) The public health significance of noise-induced hearing loss. In: Le Prell CG, Henderson D, Fay RR, Popper AN (eds) Noise-induced hearing loss: scientific advances. Springer, New York, pp 13–26. https://doi.org/10.1007/978-1-4419-9523-0_2
Robertson D, Bester C, Vogler D, Mulders WH (2013) Spontaneous hyperactivity in the auditory midbrain: relationship to afferent input. Hear Res 295:124–129. https://doi.org/10.1016/j.heares.2012.02.002
Ropp TJ, Tiedemann KL, Young ED, May BJ (2014) Effects of unilateral acoustic trauma on tinnitus-related spontaneous activity in the inferior colliculus. J Assoc Res Otolaryngol 15(6):1007–1022. https://doi.org/10.1007/s10162-014-0488-2
Salvi RJ, Wang J, Ding D (2000) Auditory plasticity and hyperactivity following cochlear damage. Hear Res 147(1-2):261–274. https://doi.org/10.1016/S0378-5955(00)00136-2
Schaette R, Kempter R (2006) Development of tinnitus-related neuronal hyperactivity through homeostatic plasticity after hearing loss: a computational model. Eur J Neurosci 23(11):3124–3138. https://doi.org/10.1111/j.1460-9568.2006.04774.x
Schwartz P, Leyendecker J, Conlon M (2011) Hyperacusis and misophonia: the lesser-known siblings of tinnitus. Minn Med 94(11):42–43
Shore SE, Helfert RH, Bledsoe SC Jr, Altschuler RA, Godfrey DA (1991) Descending projections to the dorsal and ventral divisions of the cochlear nucleus in guinea pig. Hear Res 52(1):255–268. https://doi.org/10.1016/0378-5955(91)90205-N
Szczepaniak WS, Moller AR (1996) Effects of (-)-baclofen, clonazepam, and diazepam on tone exposure-induced hyperexcitability of the inferior colliculus in the rat: possible therapeutic implications for pharmacological management of tinnitus and hyperacusis. Hear Res 97(1-2):46–53
Tanaka C, Chen GD, Hu BH, Chi LH, Li M, Zheng G, Bielefeld EC, Jamesdaniel S, Coling D, Henderson D (2009) The effects of acoustic environment after traumatic noise exposure on hearing and outer hair cells. Hear Res 250(1-2):10–18. https://doi.org/10.1016/j.heares.2008.12.010
Tunkel DE et al (2014) Clinical practice guideline: tinnitus executive summary. Otolaryngol Head Neck Surg 151(4):533–541
Turner JG (2007a) Behavioral measures of tinnitus in laboratory animals. Prog Brain Res 166:147–156. https://doi.org/10.1016/S0079-6123(07)66013-0
Turner JG (2007b) Behavioral measures of tinnitus in laboratory animals. Prog Brain Res 166:147–549. https://doi.org/10.1016/S0079-6123(07)66013-0
Vernon JA (1987) Pathophysiology of tinnitus: a special case—hyperacusis and a proposed treatment. Am J Otol 8(3):201–202
Vogler DP, Robertson D, Mulders WH (2011) Hyperactivity in the ventral cochlear nucleus after cochlear trauma. J Neurosci 31(18):6639–6645. https://doi.org/10.1523/JNEUROSCI.6538-10.2011
Wallen MB, Hasson D, Theorell T, Canlon B (2012) The correlation between the hyperacusis questionnaire and uncomfortable loudness levels is dependent on emotional exhaustion. Int J Audiol 51(10):722–729. https://doi.org/10.3109/14992027.2012.695874
Winter IM, Robertson D, Cole KS (1989) Descending projections from auditory brainstem nuclei to the cochlea and cochlear nucleus of the guinea pig. J Comp Neurol 280(1):143–157. https://doi.org/10.1002/cne.902800110
Yankaskas K (2013) Prelude: noise-induced tinnitus and hearing loss in the military. Hear Res 295:3–8. https://doi.org/10.1016/j.heares.2012.04.016
Yong JS, Wang DY (2015) Impact of noise on hearing in the military. Mil Med Res 2(1):6. https://doi.org/10.1186/s40779-015-0034-5
Young ED, Brownell WE (1976) Responses to tones and noise of single cells in dorsal cochlear nucleus of unanesthetized cats. J Neurophysiol 39(2):282–300. https://doi.org/10.1152/jn.1976.39.2.282
Young ED, Shofner WP, White JA, Robert JM, Voigt HF (1988) Response properties of cochlear nucleus neurons in relationship to physiological mechanisms. In: Edelman GM, Gall WE, Cowan WM (eds) Auditory function: neurobiological bases of hearing. John Wiley & Sons, New York, pp 277–312
Zhang JS, Kaltenbach JA (1998) Increases in spontaneous activity in the dorsal cochlear nucleus of the rat following exposure to high-intensity sound. Neurosci Lett 250(3):197–200. https://doi.org/10.1016/S0304-3940(98)00482-0
Zhou X, Merzenich MM (2012) Environmental noise exposure degrades normal listening processes. Nat Commun 3:843. https://doi.org/10.1038/ncomms1849
Acknowledgments
Support for this research was provided by the Tinnitus Research Consortium, Action on Hearing Loss, and NIDCD grant P30 DC005211. The authors thank ED Young and AM Lauer for their comments on a preliminary version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were reviewed and approved by the Institutional Animal Care and Use Committee of The Johns Hopkins University School of Medicine.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jones, A., May, B.J. Effects of Acoustic Environment on Tinnitus Behavior in Sound-Exposed Rats. JARO 19, 133–146 (2018). https://doi.org/10.1007/s10162-017-0651-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10162-017-0651-7