Abstract
The present scoping review assessed knowledge updates in tinnitus management. We included randomized trials, non-randomized studies, systematic reviews, meta-analyses, and observational studies in last 5 years on patients with tinnitus using Population, Concept, and Context mnemonic. We excluded studies on tinnitus epidemiology, technique-specific comparative studies for tinnitus assessment, review articles, or case reports. We used an artificial intelligence-powered tool MaiA for overall workflow management. Data charting elements included study identifiers, study design, population, interventions used, their outcomes on tinnitus scales, and treatment recommendations if any. Charted data from selected sources of evidence was presented using tables and a concept map. We also identified five evidence-based clinical practice guidelines (CPGs) [from the United States, Europe, and Japan regions] in our review of total 506 results, 205 underwent screening based on eligibility criteria and 38 were included for the final charting. We found three major categories of interventions in our review: Medical technology therapies; Behavioural/habituation therapies; and Pharmacological, herbal/complementary, and alternative medicine therapies. Although evidence-based guidelines on tinnitus therapy did not recommend stimulation therapies, majority of the tinnitus research to date is focused on stimulation. It is highly recommended that clinicians consider CPGs when making treatment recommendations and make the distinction between established management approaches with good evidence and emerging treatment approaches for tinnitus management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tinnitus is an intricate field in otorhinolaryngology and has remained debatable due to equivocal evidence on therapy. It can have several consequences including resulting in anxiety, depression, irritability, sleep cycle disturbances, poor concentration, pain and ultimately reducing the quality of life (QoL) [1]. In extreme conditions, suicidal ideations have also been reported by individuals with tinnitus. Tinnitus may manifest as a symptom of underlying neurological, infectious, or cardiovascular diseases apart from being a side-effect of drugs with reported ototoxicity [2]. However, unidentifiable causative mechanism and poor understanding of the pathophysiology result in unclear treatment options [3].
To date, two clinical practice guidelines (CPG) for tinnitus management (Tunkel DE et al. [4] and RFF Cima et al. [5]) are found with favorable recommendations for cognitive behavioral therapy (CBT) and sound therapy in tinnitus. There have been some studies on other experimental therapies from pharmacological, medical technology therapies (MedTech), or herbal arena with inconclusive evidence. In 2014, several systematic reviews (SLRs) [6,7,8,9,10,11,12,13,14,15,16,17,18,19] have been published with no actionable insights on existing therapeutic options for tinnitus due to poor quality or unavailability of data from randomized controlled trials (RCTs). Additionally, several scoping reviews (ScRs) [20,21,22] were conducted between 2014 and 2021. But their objective focused on standalone therapies and not a holistic analysis of the therapeutic landscape. This motivated us to undertake comprehensive research.
The objective of our ScR was to study prevalent therapies and evidence-based CPGs for tinnitus management. The specific objectives were:
-
1.
What are prevalent options for tinnitus treatment and management to date?
-
2.
What is the status of global evidence-based guidelines on tinnitus care?
-
3.
What are the evidence-based therapies recommended in those guidelines?
Method
We followed Joanna Briggs Institute’s (JBI) methodological guidance for ScR [23] and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-ScR checklist for this report.
Protocol
We registered this study protocol on Open Science Framework (OSF) after consultation with global subject matter experts (SMEs) in the field of audiology and ear, nose, and throat (ENT) with experience with tinnitus care. This is available on OSF Platform; DOI:https://doi.org/10.17605/OSF.IO/R8D39.
Eligibility Criteria and Information Sources
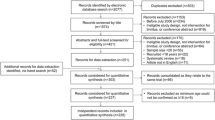
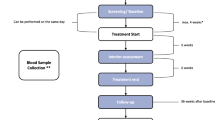
Eligible studies for our review were SLRs, meta-analyses (MAs), RCTs, and observational studies. We referred to per Population, Concept, and Context (PCC) framework (Fig. 1) for study selection. Additional filters for our literature search included publication language “English”, species “human”, “free full text”, and timeframe “last 5 years”. We excluded review articles, conference abstracts, blogs, and technical articles. The detailed study selection process is described in the PRISMA-ScR flow diagram (Fig. 2).
Search Strategy
We performed this ScR using an artificial intelligence (AI)-powered evidence synthesis tool – MaiA using two electronic biomedical literature databases - PubMed and Google Scholar. Two authors (VC and DP) referred to key articles in ENT/audiology domain and consulted senior librarians and SMEs to develop the list of relevant search terms. This list included medical subject headings (MeSH), text words, and indexed terms in abstracts from the articles found during the preliminary search. The relevant records were retrieved using key terms “tinnitus”, “therap*”, “management”, “treatment*”, and “outcome*” and boolean operators AND and OR. The search strategy is provided in online supplementary material 1. We also handpicked several articles from the bibliography of eligible articles and google search engine (first 20 pages).
Selection of Source(s) of Evidence
Two independent reviewers (DP and VC) performed the screening and selection of retrieved records using MaiA. Any discrepancy regarding screening and/or inclusion was resolved through consultation with the third reviewer (KK).
Data Charting
A Microsoft (MS)-Excel-based data charting instrument was prepared using JBI ScR data extraction template. This instrument was vetted and piloted on five random articles from the included articles (VC). Following necessary modifications based on the pilot, DP and FS performed the charting. KK and VC crossverified the charted data with the help of source records. Data discrepancies were resolved by mutual discussion and/or further adjudication from the third reviewer (VM) if needed.
The data charting elements included study type, sample size, patient characteristics (age, gender, region, type of tinnitus), tinnitus management (pharmacological, non-pharmacological), study objective (primary and secondary if available), study outcome(s) [effect on tinnitus perception, severity, loudness, hearing loss, QoL, adverse events (AEs)], and conclusion remarks/recommendations from the study author(s) as applicable. The verified, charted data was analyzed and presented using concept map(s) and charts.
Results
Report Characteristics
We retrieved a total of 506 records. After de-duplication and screening based on title/abstract, 205 records underwent eligibility-based screening. During the first- and second-level screening, 167 records were excluded based on various reasons (84 studies due to no free-full text availability, and 83 based on the mismatch with PCC), yielding 38 full-length studies for inclusion in our review. Further, we included five evidence-based guidelines on tinnitus treatment and/or management from a dedicated literature search in the google search engine.
The 38 included studies comprised of 11 SLR/MAs, 21 interventional clinical trials, 5 observational studies, and 01 ScR (Fig. 3).
Of 38, 25 studies were based on MedTech or digital interventions [6, 7, 10, 12, 13, 18, 19, 24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41], 4 studies on behavioral/habituation therapies [15, 42,43,44], and 9 studies assessed pharmacological, herbal, and multimodal therapies [45,46,47,48,49,50,51,52,53]. Detailed distribution on the types of interventions is shown in Fig. 4.
Two authors (DP and FS) performed data charting from the selected source of evidence focusing on the following characteristics: participants, sample size, interventions, study origin, type of study, tinnitus measurement tool, and efficacy, safety, and/or QoL outcomes.
Key Findings
Population
Our review considered studies with adult patients suffering from tinnitus.
Concept
MedTech Therapies
We found ten studies on non-invasive stimulation therapies comprised of transcranial direct current stimulation (tDCS), repetitive transcranial magnetic stimulation (rTMS), trans-electrical nerve stimulation (TENS), and/or vagus nerve stimulation (VNS). Of them, six studies [6, 7, 12, 13, 24, 28] assessed the effect of r-TMS. Active r-TMS was amongst the few effective treatment options compared to sham r-TMS with immediate short-term effects. However, none of the studies demonstrated the superiority of any of the r-TMS techniques (including variants such as neuronavigation and theta-burst) on long-term clinical benefits as per self-reported tinnitus severity and depression scores. Amongst r-TMS variants studied in a network MA, superior results were shown for the tinnitus patients who received r-TMS priming compared to those who did not receive it [10]. Four [27, 29, 30, 32] studies on electrical stimulation showed significant benefits in both acute (TENS) and chronic tinnitus management (trans-tympanic electrical stimulation and VNS). One study considered photobimodulation therapy as a comparator [37]. All stimulation therapies showed efficacy and safety in tinnitus patients on a short-term basis, however, none of the stimulation therapies showed improvement on a long-term basis.
Other MedTech therapies of non-stimulatory nature in our review included sound and music therapies [18, 26, 34, 39, 40], and smartphone applications [41] delivering the acoustic therapies, and facilitating capture and signal processing of electroencephalogram. No substantial improvement in tinnitus was reported after acoustic therapies and the studies provide inconclusive evidence.
Behavioral/Habituation Therapies
Major behavioral/habituation therapies reported in this study were CBT [15, 43, 44] and tinnitus retraining therapy (TRT) [42]. Apart from conventional CBT, mobile-based CBT and internet-based CBT were innovative interventions.
CBT was effective with significant results on tinnitus intrusiveness and tinnitus severity. It was also effective in improving depression-related and mood symptoms of tinnitus, insomnia, hearing disability, and hyperacusis. Imputed visual analog scale (VAS) score values demonstrated significant improvement after CBT unlike those with actual VAS scores. No AEs were reported in an audiologist-based trial using CBT on tinnitus patients [43].
TRT did not show significant improvement in any of the tinnitus severity scales [tinnitus questionnaire (TQ), tinnitus functional index (TFI), or tinnitus handicap inventory (THI)]. However, significant results were observed on a long-term basis [42].
Pharmacological, Herbal, and Complementary and Alternative Medicine (CAM) Interventions
We found nine studies on pharmacological (n = 5), herbal (n = 3), and CAM therapies (n = 1) [45,46,47,48,49,50,51,52,53].
The pharmacological interventions included OTO-313, dexamethasone, AUT00063, transdermal lidocaine, and nitrous oxide gas. Of these, OTO-313 and intratympanic dexamethasone showed significant improvement in mean TFI (P < 0.05) at week 4 and 8 and THI at six months (P = 0.037). Similarly, after one month post-treatment with transdermal lidocaine in a pilot study, significant reduction from pre-treatment TFI at 1 month and 3 months was seen (P < 0.05) [47]. However, no significant efficacy findings were found in the study assessing effect of nitrous oxide [52] or AUT00063 [53].
Herbal products reported in three studies to reduce oxidative stress due to tinnitus were Ginkgo Biloba (GB) extract, antioxidant supplementation (multivitamin, multimineral, phytochemicals, alpha-lipoic acid), and açaí extract. GB demonstrated significant improvement in tinnitus loudness (P = 0.0021) and annoyance (P = 0.0002). It also reduced anxiety with significant reduction in the Hospital Anxiety and Depression Scale (HADS) anxiety score from the baseline abnormal score (P = 0.005). Antioxidant supplementation significantly decreased tinnitus loudness and maximum masking limit (MML) from baseline to post-measure (P < 0.001) [46]. Similarly, it also significantly reduced THI (P = 0.015) and TFI scores from baseline values (P = 0.410) [45].
All of the above interventions were well-tolerated with several AEs. However, none of them resulted in any serious adverse event, demonstrating a good safety profile.
Figure 5 summarizes the therapeutic potential from individual therapies included based on the strength of evidence.
Digital Therapies
Two studies were on internet-based interventions and both demonstrated the therapeutic potential of CBT delivered with added benefits when done under the expert guidance of an audiologist [25, 33]. Also, a recent trial reported Virtual Reality as an aiding factor to CBT’s effectiveness with a reported reduction in tinnitus distress [31].
Evidence-Based Clinical Practice Guidelines on Tinnitus Treatment and Management
Five evidence-based guidelines were included based on our targeted search [4, 5, 54,55,56]. Key evidence-based therapies included CBT, sound therapy, family physician counselling, personalized amplification device, and digital approaches to implement CBT. Our review did not find any studies exclusively focusing on the therapies (such as antidepressants, anticonvulsants, and anxiolytics) or therapies which are not recommended in the guidelines. However, the majority of studies focused on rTMS -indicating a dire need to educate MedTech researchers working in the tinnitus space (see Table 1).
Discussion
We performed a ScR to broadly explore the treatment landscape for tinnitus patients especially in the last five years using an automation tool for synthesizing the tinnitus evidence to date. ScR is an emerging research method to assess the evidence gaps and to obtain a bird eye view on any specific topic. Although several ScRs are available on tinnitus, they either focused on individual therapy or had different objective(s)/population. To date, there has been only one ScR providing an overview about the broader treatment and management landscape for tinnitus [22]. However, it contained a focused search strategy towards behavioral and habit-oriented interventions, limiting the scope of evidence synthesis. This limitation was overcome by our broad, informed search strategy.
Our preliminary literature search identified five evidence-based treatment and/or management guidelines for tinnitus from Europe (EU), the United States of America (USA), and Japan regions [4, 5, 54,55,56]. However, the only ScR exploring tinnitus therapy as a whole did not include any of these guidelines. Also, the ScR did not refer to any standard reporting checklists to ascertain the quality of reporting [22]. Our ScR is the first of its kind with AI-powered workflow and alignment with evidence-based guidelines to date. It was in concordance with the PRISMA-ScR checklist 2020. For recency of data purposes, we kept the timeframe for our literature search from 2017 to 2021 (search date: 1 Apr 2022). Being a ScR with broad concepts regarding study designs, we included SLR and SLR-MA, RCTs, non-RCTs, and observational studies. However, we did not consider case reports and review articles due to their low level of evidence. We limited our search to free- full-text articles only to promote public accessibility of research. ScR by Makar et al. described the interventions with intended cognitive effects on tinnitus, including counselling, tinnitus masking, TRT, CBT, relaxation, and attention diversion in tinnitus patients [22]. Our study provided further updates on interventions with broader scope and search strategy, aligning our intended purpose and methodology with standard ScR guidelines from the JBI.
We included 38 studies and five evidence-based guidelines for the treatment and/or management of tinnitus. Our ScR found several new therapies than those mentioned in included guidelines, indicating recent strides in tinnitus research. Collectively, none of the therapies except for CBT was found with significant findings with strong recommendations, demonstrating a scope of evaluating methodological inconsistencies for the interventions other than CBT.
Compared with guidelines by Tunkel 2014 [4], there were six new therapy modalities found in EU guidelines, reflecting the evolution in tinnitus research over the period of time. Contradictorily, we found majority of studies focusing on interventions related to stimulation therapies and acoustic therapies despite no strong recommendations for such therapies in both evidence-based guidelines, pointing towards the plateaued phase of tinnitus research.
Out of 12 therapy modalities considered in the EU guideline, seven presented no recommendation owing to the lack of safety, efficacy, or both data. This shows an unmet research need and warrants well-designed studies for reforming current practice models.
All the included studies were found similar with an assessment of tinnitus severity as a primary objective. Also, the tools used for the assessment of tinnitus severity and associated QoL were found to be consistently used across all the studies.
Unfortunately, we could not extract any actionable insights from available studies assessing pharmacological, CAM, or similar interventions for tinnitus. The possible reason as experienced by many tinnitus researchers could be the inherent disease complexity. Given the increasing use of AI in proteomics and metabolomics for lead identification, we encourage tinnitus researchers to decipher complex tinnitus mechanisms and explore new drugs with AI-induced target identification or AI-induced frequency modulation. We noticed a huge evidence gap in terms of reporting secondary outcomes i.e., depression, anxiety, and QoL. Only ten studies reported improvement/no improvement in QoL, rendering the dearth on similar aspects for the rest of the interventions.
Although none of the guidelines provides in-depth information on the use of digital means to deliver interventions for treating or managing tinnitus, our ScR analyzed four studies using internet-based or mobile applications-based solutions for delivering CBT with promising outcomes, informing the future cost-effective tinnitus research especially post-coronavirus pandemic.
Study Limitations
We did not consider studies evaluating technical parameters for MedTech interventions due to the lack of relevant expertise. Secondly, we found no study from the Asia-Pacific region, which hampered our findings’ generalizability to the Indian context. Thus, the future scope may include a modified search strategy with the inclusion of surgical therapies and technical parameters of MedTech and primary studies on tinnitus research from the Asia-Pacific region for deeper insights.
Conclusion
Our ScR is the first of its kind in the domain of tinnitus research. It provided holistic insights about available therapies for tinnitus treatment and management since the release of evidence-based guidelines in the US and thereafter. Considering the evidence gap between low and middle-income countries, otorhinolaryngology professionals and acoustics professionals from countries like India are encouraged to undertake the large-scale burden of disease studies and interventional research on various therapies recommended in global CPGs. Given the lack of high-quality efficacy and safety data, it would be worthwhile to promote primary research with meticulous methods of acoustic technologies and stimulation therapies especially those of lesser harm. Implementation research focusing on the effectiveness of a multidisciplinary approach is highly recommended over the assessment of the therapeutic potential of individual therapies. Digital interventions for CBT delivery may provide newer insights in tinnitus treatment and management, however, requiring robust evidence for health system integration.
References
De Ridder D, Vanneste S, Weisz N et al (2014) An integrative model of auditory phantom perception: Tinnitus as a unified percept of interacting separable subnetworks. Neurosci Biobehav Rev 44:16–32. https://doi.org/10.1016/j.neubiorev.2013.03.021
Bisht M, Bist SS (2011) Ototoxicity: the hidden menace. Indian J Otolaryngol Head Neck Surg 63:255–259. https://doi.org/10.1007/s12070-011-0151-8
Haider HF, Bojić T, Ribeiro SF, Paço J, Hall DA, Szczepek AJ (2018) Pathophysiology of subjective Tinnitus: triggers and maintenance. Front Neurosci 12:866. https://doi.org/10.3389/fnins.2018.00866
Tunkel DE, Bauer CA, Sun GH et al (2014) Clinical practice Guideline. Otolaryngol Neck Surg 151:S1–S40. https://doi.org/10.1177/0194599814545325
Cima RFF, Mazurek B, Haider H et al (2019) A multidisciplinary european guideline for tinnitus: diagnostics, assessment, and treatment. HNO 67:10–42. https://doi.org/10.1007/s00106-019-0633-7
Yin L, Chen X, Lu X, An Y, Zhang T, Yan J (2021) An updated meta-analysis: repetitive transcranial magnetic stimulation for treating tinnitus. J Int Med Res 49:030006052199954. https://doi.org/10.1177/0300060521999549
Liang Z, Yang H, Cheng G, Huang L, Zhang T, Jia H (2020) Repetitive transcranial magnetic stimulation on chronic tinnitus: a systematic review and meta-analysis. BMC Psychiatry 20:547. https://doi.org/10.1186/s12888-020-02947-9
Hall DA, Wegner I, Smit AL, McFerran D, Stegeman I (2018) Betahistine for tinnitus. Cochrane Database Syst Rev 12(12):CD013093. https://doi.org/10.1002/14651858.cd013093.pub2
Liu H, Zhang J, Yang S et al (2021) Efficacy of sound therapy interventions for tinnitus management. Med (Baltim) 100:e27509. https://doi.org/10.1097/md.0000000000027509
Lefebvre-Demers M, Doyon N, Fecteau S (2021) Non-invasive neuromodulation for tinnitus: a meta-analysis and modeling studies. Brain Stimul 14:113–128. https://doi.org/10.1016/j.brs.2020.11.014
Stegeman I, Velde HM, Robe PAJT, Stokroos RJ, Smit AL (2021) Tinnitus treatment by vagus nerve stimulation: A systematic review. Michiels S, editor. PLoS One 16:e0247221. https://doi.org/10.1371/journal.pone.0247221
Chen J-J, Zeng B-S, Wu C-N et al (2020) Association of Central Noninvasive Brain Stimulation Interventions with Efficacy and Safety in Tinnitus Management. JAMA Otolaryngol Neck Surg 146:801. https://doi.org/10.1001/jamaoto.2020.1497
Dong C, Chen C, Wang T et al (2020) Low-frequency repetitive transcranial magnetic stimulation for the treatment of chronic Tinnitus: a systematic review and Meta-analysis of Randomized controlled trials. Biomed Res Int 2020:1–9. https://doi.org/10.1155/2020/3141278
Mehdi M, Stach M, Riha C et al (2020) Smartphone and Mobile Health apps for Tinnitus: systematic identification, analysis, and Assessment. JMIR mHealth uHealth 8:e21767. https://doi.org/10.2196/21767
Fuller T, Cima R, Langguth B, Mazurek B, Vlaeyen JW, Hoare DJ (2020) Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev 1(1):CD012614. https://doi.org/10.1002/14651858.cd012614.pub2
Schoisswohl S, Agrawal K, Simoes J et al (2019) RTMS parameters in tinnitus trials: a systematic review. Sci Rep 9:12190. https://doi.org/10.1038/s41598-019-48750-9
Beukes EW, Manchaiah V, Allen PM, Baguley DM, Andersson G (2019) Internet-based interventions for adults with hearing loss, Tinnitus, and vestibular Disorders: a systematic review and Meta-analysis. Trends Hear 23:233121651985174. https://doi.org/10.1177/2331216519851749
Sereda M, Xia J, El Refaie A, Hall DA, Hoare DJ (2018) Sound therapy (using amplification devices and/or sound generators) for tinnitus. Cochrane Database Syst Rev 12(12):CD013094. https://doi.org/10.1002/14651858.cd013094.pub2
Santos A, HM, Santos APS, Santos HS, Silva AC (2018) da The use of tDCS as a therapeutic option for tinnitus: a systematic review. Braz J Otorhinolaryngol 84:653–659. https://doi.org/10.1016/j.bjorl.2018.02.003
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 169:467–473
Tricco AC, Lillie E, Zarin W et al (2016) A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 16:15. https://doi.org/10.1186/s12874-016-0116-4
Makar SK, Mukundan G, Gore G (2017) Treatment of Tinnitus: a scoping review. Int Tinnitus J 21(2):144–156. https://doi.org/10.5935/0946-5448.20170027
Peters M, Godfrey C, McInerney P, Munn Z, Trico A, Khalil H (2020) Chap. 11: Scoping Reviews (2020 version) In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis, JBI. https://doi.org/10.46658/JBIMES-20-12
Hong S-M, Kim S-K, Seo M-Y, Kang S-Y (2021) Multiple daily Rounds of Theta-Burst Stimulation for Tinnitus: preliminary results. Med (B Aires) 57(8):743. https://doi.org/10.3390/medicina57080743
Beukes W, Andersson E, Fagelson G, Manchaiah M V (2022) Internet-based audiologist-guided cognitive behavioral therapy for Tinnitus: Randomized Controlled Trial. J Med Internet Res 24:e27584. https://doi.org/10.2196/27584
Atipas S, Therdphaothai J, Suvansit K, Prakairungthong S, Thongyai K, Limviriyakul S (2021) A Randomized, Controlled Trial of Notched Music Therapy for Tinnitus Patients. J Int Adv Otol 17:221–227. https://doi.org/10.5152/iao.2021.9385
Conlon B, Hamilton C, Meade E et al (2022) Different bimodal neuromodulation settings reduce tinnitus symptoms in a large randomized trial. Sci Rep 12:10845. https://doi.org/10.1038/s41598-022-13875-x
Sahlsten H, Holm A, Rauhala E et al (2019) Neuronavigated Versus non-navigated repetitive transcranial magnetic stimulation for chronic Tinnitus: a randomized study. Trends Hear 23:233121651882219. https://doi.org/10.1177/2331216518822198
Li L, Shi H, Wang M (2019) A pilot randomized controlled trial of Transcutaneous Electrical nerve stimulation for patients with Acute Tinnitus. Med (Baltim) 98:e13793. https://doi.org/10.1097/md.0000000000013793
Choi WS, Kim SJ, Chang DS, Lee HY (2018) Characteristics of stimulus intensity in Transcutaneous Vagus nerve stimulation for chronic Tinnitus. J Int Adv Otol 14:267–272. https://doi.org/10.5152/iao.2018.3977
Park DH, Han SS, Han M et al (2022) A clinical trial of a patient-customized virtual reality intervention for tinnitus. Sci Rep 12:12441. https://doi.org/10.1038/s41598-022-16764-5
Marinelli JP, Anzalone CL, Prummer CM et al (2022) Electrical stimulation of the cochlea for treatment of chronic disabling tinnitus: an open-label trial towards the development of an implantable device. J Transl Med 20:56. https://doi.org/10.1186/s12967-022-03271-4
Beukes EW, Andersson G, Allen PM, Manchaiah V, Baguley DM (2018) Effectiveness of guided internet-based cognitive behavioral therapy vs face-to-face Clinical Care for treatment of Tinnitus. JAMA Otolaryngol Neck Surg 144:1126. https://doi.org/10.1001/jamaoto.2018.2238
Cuesta M, Cobo P (2020) Broadband Sound equalized by the hearing loss curves as an improved stimulus for Tinnitus Retraining Therapy-A Pilot, Non-Controlled Observational Study. J Int Adv Otol 16:207–212. https://doi.org/10.5152/iao.2020.7834
Güntensperger D, Thüring C, Kleinjung T, Neff P, Meyer M (2019) Investigating the Efficacy of an Individualized Alpha/Delta Neurofeedback Protocol in the Treatment of Chronic Tinnitus. Neural Plast 1–15. https://doi.org/10.1155/2019/3540898
Kreuzer PM, Poeppl TB, Rupprecht R et al (2019) Daily high-frequency transcranial random noise stimulation of bilateral temporal cortex in chronic tinnitus – a pilot study. Sci Rep 9:12274. https://doi.org/10.1038/s41598-019-48686-0
Eladl HM, Elkholi SM, Eid MM, Abdelbasset WK, Ali ZA, Bahey El-Deen HA (2022) Effect of adding a supervised physical therapy exercise program to photobiomodulation therapy in the treatment of cervicogenic somatosensory tinnitus: a randomized controlled study. Med (Baltim) 101(31):e29946. https://doi.org/10.1097/md.0000000000029946
Kubota Y, Takahashi K, Nonomura Y et al (2022) Effects of sound source localization of masking sound on perception level of simulated tinnitus. Sci Rep 12:1452. https://doi.org/10.1038/s41598-022-05535-x
Peng F, Xiang Y, Xu H, Yin Q, Li J, Zou Y (2021) Systematic review and meta-analysis of extended high-frequency audiometry in tinnitus patients. Ann Palliat Med 10:12129–12139. https://doi.org/10.21037/apm-21-3060
Tutaj L, Hoare DJ, Sereda M (2018) Combined amplification and sound generation for Tinnitus: a scoping review. Ear Hear 39:412–422. https://doi.org/10.1097/aud.0000000000000516
Mehdi M, Riha C, Neff P et al (2020) Smartphone apps in the context of Tinnitus. Syst Rev Sens 20:1725. https://doi.org/10.3390/s20061725
Scherer RW, Formby C (2019) Effect of Tinnitus Retraining Therapy vs Standard of Care on Tinnitus-Related Quality of Life. JAMA Otolaryngol Neck Surg 145:597. https://doi.org/10.1001/jamaoto.2019.0821
Beukes EW, Andersson G, Fagelson M, Manchaiah V (2021) Audiologist-supported internet-based cognitive behavioral therapy for Tinnitus in the United States: a pilot trial. Am J Audiol 30:717–729. https://doi.org/10.1044/2021_aja-20-00222
Oron Y, Ben David BM, Doron G (2022) Brief cognitive-behavioral training for tinnitus relief using a mobile application: a pilot open trial. Health Inf J 28:146045822210834. https://doi.org/10.1177/14604582221083483
Petridou AI, Zagora ET, Petridis P et al (2019) The effect of antioxidant supplementation in patients with Tinnitus and Normal hearing or hearing loss: a Randomized, Double-Blind, Placebo Controlled Trial. Nutrients 11:3037. https://doi.org/10.3390/nu11123037
Procházková K, Šejna I, Skutil J, Hahn A (2018) Ginkgo biloba extract EGb 761® versus pentoxifylline in chronic tinnitus: a randomized, double-blind clinical trial. Int J Clin Pharm 40:1335–1341. https://doi.org/10.1007/s11096-018-0654-4
O’Brien DC, Robinson AD, Wang N, Diaz R (2019) Transdermal lidocaine as treatment for chronic subjective tinnitus: a pilot study. Am J Otolaryngol 40:413–417. https://doi.org/10.1016/j.amjoto.2019.03.009
Oppitz SJ, Garcia MV, Bruno RS et al (2022) Supplementation with açaí (Euterpe Oleracea Martius) for the treatment of chronic tinnitus: effects on perception, anxiety levels and oxidative metabolism biomarkers. Codas 34(4):e20210076. https://doi.org/10.1590/2317-1782/20212021076
Maxwell KS, Robinson JM, Hoffmann I et al (2021) Intratympanic Administration of OTO-313 reduces Tinnitus in patients with moderate to severe, persistent Tinnitus: a phase 1/2 study. Otol Neurotol 42:e1625–e1633. https://doi.org/10.1097/mao.0000000000003369
Yener HM, Sari E, Aslan M, Yollu U, Gozen ED, Inci E (2020) The efficacy of Intratympanic Steroid Injection in Tinnitus cases unresponsive to Medical Treatment. J Int Adv Otol 16:197–200. https://doi.org/10.5152/iao.2020.7588
Li Y, Sang D, Wu Z, Cao X (2022) Systematic Evaluation of the Efficacy of Acupuncture Associated with Physical and Mental Intervention when Treating Idiopathic Tinnitus and the Improvement of Tinnitus Symptoms. Tang M, editor. Comput Math Methods Med 022:6764909. https://doi.org/10.1155/2022/6764909
Hong HY, Karadaghy O, Kallogjeri D et al (2018) Effect of Nitrous Oxide as a treatment for subjective, idiopathic, nonpulsatile Bothersome Tinnitus. JAMA Otolaryngol Neck Surg 144(9):781–787. https://doi.org/10.1001/jamaoto.2018.1278
Hall DA, Ray J, Watson J et al (2019) A balanced randomised placebo controlled blinded phase IIa multi-centre study to investigate the efficacy and safety of AUT00063 versus placebo in subjective tinnitus: the QUIET-1 trial. Hear Res 377:153–166. https://doi.org/10.1016/j.heares.2019.03.018
Ogawa K, Sato H, Takahashi M et al (2020) Clinical practice guidelines for diagnosis and treatment of chronic tinnitus in Japan. Auris Nasus Larynx 47(1):1–6. https://doi.org/10.1016/j.anl.2019.09.007
Tinnitus : assessment and management | Guidance | NICE. https://www.nice.org.uk/guidance/ng155. Accessed 20 January 2023
Wu V, Cooke B, Eitutis S, Simpson MTW, Beyea JA (2018) Approach to tinnitus management. Can Fam Physician 64(7):491–495. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc6042678/
Acknowledgements
The author team would like to thank the global experts who provided valuable inputs that led to modification in the previous version of the registered protocol with stronger scientific rigor.
Authors would like to acknowledge Ms. Shwetha Kumar for her editorial support.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Concept and Design – VC, KK. Data Acquisition – DP, VC. Screening and Data Charting – DP, FS. Analysis and Interpretation – VM. Manuscript Drafting – DP, FS, VC. Editorial Review and Finalization – VM, KK.
Corresponding author
Ethics declarations
Conflict of interest
VC, DP, FS, VM, KK declare that they have no CoI.
Research involving Human Participants and/or Animals
Not applicable as our study was based on secondary data (published literature).
Informed Consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chhaya, V., Patel, D., Shethia, F. et al. Current Therapeutic Trends for Tinnitus Cure and Control: A Scoping Review. Indian J Otolaryngol Head Neck Surg 75, 4158–4166 (2023). https://doi.org/10.1007/s12070-023-03910-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03910-2