Abstract
Background
Overexpression of tumor-associated antigens has been reported in many types of cancer and may trigger secretion of their autoantibodies. The present work was designed to test whether circulating antibody to FOXP3 protein-derived antigens was altered in early cervical cancer and cervical benign tumors.
Methods
A total of 141 patients with cervical cancer, 133 patients with cervical benign tumors and 148 healthy age-matched volunteers were recruited. The level of circulating anti-FOXP3 IgG antibody was tested using an enzyme-linked immunosorbent assay developed in-house with linear peptide antigens derived from FOXP3 protein. The linear peptide antigens were designed according to the computational prediction of HLA-II epitopes.
Results
Student’s t test showed that anti-FOXP3 IgG in the malignant tumor group and the benign tumor group was significantly higher than in the control group (t = 6.127, p < 0.001; t = 2.704, p = 0.007). In addition, patients with stage I cervical cancer (t = 2.968, p = 0.003) had a significantly higher level of FOXP3 autoantibodies than patients with benign tumors. The sensitivity against >90 % specificity was 20.6 % with an interassay deviation of 11.7 % in the cervical cancer group. Based on a cut-off value determined by the 98th percentile of the control group IgG levels, the anti-FOXP3 IgG positivity was 2.1 % in patients with cervical cancer compared to 2.0 % in the health controls (chi-squared = 0.004, p = 0.952, OR = 1.051, 95 % CI 0.209–5.295).
Conclusion
The circulating autoantibody to FOXP3 reflecting the continuous development of the cervical lesion, may be a potential biomarker with early prognostic values for cervical cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is one of the most common gynecologic malignancies seriously threatening women’s health. There are approximately 466,000 new cases of cervical cancer diagnosed annually worldwide, 80 % of which occur in developing countries, and approximately 270,000 people die of the disease [1, 2]. In China, there are approximately 10 million new cases each year, accounting for nearly 20 % of the total new cases in the world. In addition, the incidence of cervical cancer in recent years shows a regional increasing trend as the age of onset becomes earlier [2]. The prognosis of patients with cervical cancer is closely related with pathological type and clinical stage. Early diagnosis of patients with cervical cancer is necessary in order to receive proper, timely and effective treatment, to control disease progression and to improve the health and quality of life. Traditional serological tumor markers have some limitations in the early diagnosis of cervical cancer and more new serum tumor markers need to be identified to improve the early diagnostic rate.
When a tumor occurs, abnormally proliferated tumor cells will be considered by the immune system as exotic abnormal antigens to stimulate immune responses and be killed by autoantibodies against these tumor antigens, with the aim of destroying the tumor. Previous studies have shown that some autoantibodies of tumor-associated antigens (TAAs) in patients with malignant tumors exhibit some antitumor effects. Although these TAA autoantibodies vary among tumor types and among individuals, they are still potential diagnostic tumor biomarkers. In recent years, there has been much discussion regarding TAA autoantibodies as early tumor biomarkers to determine the therapeutic efficacy or evaluate disease prognosis [3, 4]. While TAA expression level is low at the early cancer stage, they cannot be accurately detected by conventional protein detection methods; however, based on antigen–antibody reaction, TAA autoantibodies could be detected with higher sensitivity. Therefore, compared with TAAs, the detection of TAA autoantibodies is more significant in early tumor diagnosis.
FOXP3 is a member of forkhead/winged helix family transcription factors. The human FOXP3 gene is located in Xp11.23 and contains 11 exons and 10 introns, and the full length of cDNA is 1869 bp. The expression level has been shown to be closely related to tumorigenesis and tumor development [5, 6]. FOXP3 is the most specific marker of regulatory T cells (Tregs). It is involved in the activation and functional regulation of Tregs [7], and is essential for dynamic regulation of immune homeostasis. Absence of FOXP3 leads to autoimmune diseases, indicating that it plays a crucial role in Treg functioning [5]. Tregs are a type of multi-immunoregulatory T cell. They can inhibit activation of other T cells, impede the body’s immune surveillance to cancer [8], and prevent TAA autoantibodies from providing effective immune responses, thus providing an immune escape environment for tumor cells and promoting tumor development. Previous studies have found that the level of peripheral CD4+CD25+ Tregs is significantly higher in patients with lung, breast, ovarian, colon and other cancers than in healthy subjects [9, 10], and is closely associated with a patient’s clinical stage and tumor-bearing state.
We have previously found that a variety of TAA autoantibodies are closely related to cancer. For example, the level of ABCC3 autoantibodies in patients with lung and esophageal cancers [11, 12], p16 autoantibodies in patients with esophageal cancer and non-small-cell lung cancer [13, 14], ANXA1 autoantibodies in patients with lung cancer [15] and FOXP3 autoantibodies in patients with esophageal cancer [16] are significantly higher than in healthy subjects. However, only a few studies on autoantibodies in patients with cervical cancer have been reported. Based on our recent work, the application of linear peptides and antigens may be more sensitive for enzyme-linked immunosorbent assay (ELISA) of circulating autoantibodies against some TAAs. Accordingly, the present work was undertaken to develop an in-house ELISA with human leukocyte antigen class II-restricted peptide antigens to detect circulating antibodies to FOXP3 protein.
Materials and methods
Subjects
A total of 274 female patients first diagnosed with cervical cancer, including 133 with cervical benign tumors and 141 with malignant tumors, were confirmed by radiographic examination and histological confirmation with staging information. All 274 patients had complete clinical data information and were recruited from the Second Hospital of Jilin University. Blood samples were taken prior to any anticancer treatment. 148 healthy age-matched subjects (Table 1 were also recruited as controls from local communities. International recognition on the stage III and IV cancer as advanced cervical cancer was confirmed by clinical diagnosis. In our practical work, we only had a few samples from advanced cervical cancer patients who attended the specialized gynecological clinic. Therefore, we were only able to include stage I malignant tumor group and stage II cervical cancer group in order to study the significance of FOXP3 autoantibodies in the diagnosis of early cervical cancer. We also used clinical interviews and imaging examinations to eliminate patients with any other tumors and control subjects who had a history of any tumors. We excluded patients with a history of severe autoimmune diseases, such as autoimmune thyroid disease, pernicious anemia, type I diabetes and celiac disease, multiple sclerosis, ankylosing spondylitis, systemic lupus erythematosus, rheumatoid arthritis, and inflammatory bowel disease. All patients were of Chinese Han origin and provided written informed consent to participate in this study. This work was approved by the Ethics Committee of Jilin University.
Autoantibody testing
A linear peptide antigen was designed according to the computational prediction of human leukocyte antigen class II (HLA-II)-restricted epitopes, which can be recognized by HLA-II molecules among >90 % of the Chinese population. The autoantibody specific for FOXP3 protein was measured by a relative ELISA approach as described in our recent publication [11–16]. To reduce the interference from a non-specific signal produced by passive absorption of various IgG antibodies in plasma to the surface of a 96-well microplate, a specific binding index (SBI) was used to express the levels of circulating autoantibody against FOXP3. This therefore was a relatively quantitative ELISA antibody test, and the SBI was calculated as follows:
The OD value of control antigens represents the complete non-specific binding signal, and that of FOXP3 antigens represents a combination of both specific and non-specific binding signals. Each sample was tested in duplicate. To minimize an intra-assay deviation, the ratio of the difference between duplicate sample OD values and their sum was used to assess the assay accuracy. The inter-assay deviation that reflected the reproducibility of assay was estimated using the SBI tested with pooled plasma samples, namely quality control (QC) samples that were randomly collected from >200 healthy subjects and tested on every 96-well plate.
Data analysis
The mean ± SD in SBI was used to present data. Microsoft Excel 2010 was used to construct a database with individual SBI values and to graphically analyze the distributions of individual autoantibody levels, and IBM SPSS Statistics 19.0 was applied to perform Student’s t test to compare the differences in SBI between the patient group, the benign group and the control group; to perform Pearson’s chi-squared test for the difference in antibody positivity between different groups, with calculation of odds ratio (OR) and 95 % confidence interval (CI); and to analyze receiver operating characteristic curve (ROC) analysis for calculation of the area under the ROC curve (AUC) with the ELISA sensitivity against a specificity of >90 %. The anti-FOXP3 antibody positivity was determined by a cut-off value above the 98th percentile of antibody levels in control subjects.
Results
The levels of circulating IgG to FOXP3 in the cervical cancer, benign tumor and control groups
We analyzed the expression of autoantibody to FOXP3 in the malignant tumor, benign tumor and control groups, and the results are shown in Table 2. As shown in Table 2, the level of autoantibody to FOXP3 in both the malignant tumor group and the benign tumor group were significantly higher than in controls (t = 6.127, p < 0.001; t = 2.704, p = 0.007). The level of autoantibody to FOXP3 in the malignant tumor group was significantly higher than in the benign tumor group (t = 2.775, p = 0.006). The expression of autoantibody to FOXP3 in the control, benign tumor and malignant tumor groups showed an increasing trend. Based on a cut-off value determined by the 98th percentile of the control group IgG levels, the anti-FOXP3 IgG positivity was 2.1 % in patients with cervical cancer and 6.8 % in patients with benign tumors compared to 2.0 % in the health controls (chi-squared = 0.004, p = 0.952, OR = 1.051, 95 % CI 0.209–5.295; chi-squared = 3.85, p = 0.05, OR = 3.508, 95 % CI 0.929–13.244), as shown in Table 3. The percentages of anti-FOXP3 IgG positivity in patients with stage I cervical cancer and in patients with stage II cervical cancer were 1.7 and 2.4 % (Table 3).
The levels of circulating IgG to FOXP3 in different stage of cervical cancer
The patients in our study had stage I and stage II cervical cancer. First, we found that the level of autoantibody to FOXP3 in the stage I and stage II groups was statistically significantly higher than in the healthy controls (t = 5.595, p < 0.001; t = 4.344, p < 0.001), as shown in Table 2. We also reviewed stage I and II groups with the benign tumor group as shown in Table 2. Patients with stage I cervical cancer had a significantly higher level of FOXP3 autoantibodies than patients with benign tumors (t = 2.968, p = 0.003), while patients with stage II cervical cancer showed no difference compared with the benign tumor group (t = 1.569, p = 0.118). Furthermore, there was no significant difference in the level of FOXP3 autoantibodies between patients with stage I and II cervical cancer (t = 1.758, p = 0.081).
ROC analysis
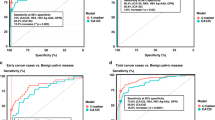
We used the ROC curve to assess the diagnostic value between the malignant tumor group and the healthy control group; the results show that IgG to FOXP3 in the malignant tumor group had an AUC of 0.703 (SE = 0.031,95 % CI 0.643–0.763) (Fig. 1; Table 4), and the ELISA test had a sensitivity of 20.6 % against 90.0 % specificity for FOXP3 autoantibody. IgG to FOXP3 in the stage I cervical cancer group showed the highest positivity with a sensitivity of 25.4 % against 90.0 % specificity, and ROC analysis showed an AUC of 0.741 SE = 0.037, 95 % CI 0.668–0.814) (Fig. 1; Table 4). In the stage II cervical cancer group, ROC analysis gave an AUC of 0.676 (SE = 0.036, 95 % CI 0.606–0.747) (Fig. 1; Table 4), and a sensitivity of 17.1 % against 90.0 % specificity for FOXP3 autoantibody. Meanwhile in the benign tumor group, ROC analysis showed an AUC of 0.570 SE = 0.034,95 % CI 0.503–0.637) (Fig. 1; Table 4), and a sensitivity of 15.0 % against 90.0 % specificity.
Discussion
Immune surveillance is one of the most basic functions of the immune system; it can identify, destroy, kill or inhibit mutant cells and prevent tumorigenesis. The theory also provides a way for the early detection of cancer [17]. When patients have not presented any symptoms and their TAAs are at low level, the immune system is able to monitor the presence of TAAs and cause immune responses, producing large amounts of autoantibodies to clear carcinomic antigens. Thus, serum autoantibodies are sensitive biomarkers for cancer detection [18]. For immune response between TAAs and autoantibodies present in cancer patients, the detection of serum autoantibodies can be used to distinguish between cancer patients and healthy subjects [19, 20].
Many studies on lung, stomach and colon cancers have confirmed that TAAs and TAA autoantibodies can be used as tools for early diagnosis of cancer and indicators of therapeutic efficacy. Combined detection of p53, c-myc, cyclin-B1 and other TAA autoantibodies with conventional tumor markers can significantly improve the diagnostic specificity and sensitivity [5, 21–23]. We have previously demonstrated that expression of TAA autoantibody is increased in patients with other cancers. Currently, only a few studies on TAA autoantibody in patients with cervical cancer have been reported. In this study, we selected several TAA autoantibodies in plasma and found that FOXP3 autoantibody expression level was significantly different among cervical cancer, benign tumor and healthy control groups.
An increased proportion of CD4+CD25+ Tregs in peripheral lymphocytes and tumor-infiltrating lymphocytes was first demonstrated in patients with breast, ovarian, and pancreatic cancers and skin squamous cell carcinoma [24–28].
Woo et al. [10] first reported that the proportion of FOXP3+ Tregs is enhanced in non-small-cell lung cancer cells. The underlying mechanism may be that the population of Tregs is higher in cancer patients than in healthy subjects because Tregs are involved in functional regulation of immune suppression and cancer patients are in an immunosuppressed state, and as FOXP3 is a specific marker of Tregs, it is therefore highly expressed in Tregs. Since then, many researchers have found the expression level of FOXP3+ Tregs is also increased in peripheral lymphocytes and tumor-infiltrating lymphocytes of patients with various malignant tumors such as epithelial malignant lesions, head and neck cancer, hepatocellular carcinoma, pancreatic cancer and breast cancer [25–30], suggesting that the expression level of FOXP3+ Tregs is closely related with tumor occurrence, development and prognosis. Upregulation of FOXP3+ Tregs in vivo is a common phenomenon in patients with malignant tumors.
Further studies have confirmed that FOXP3 expression is significantly higher in breast cancer cells, and detection of FOXP3 mRNA and protein expression has significant guidance for diagnosis and prognosis of breast cancer. Researchers believe that FOXP3 expression is an independent risk factor for breast cancer metastasis [30, 31]. In a study of FOXP3 gene and cervical cancer, Hou et al. [32] showed that an imbalance of the immune system was present in patients with cervical cancer, which led to T cells differentiating towards FOXP3+ T cells. Therefore, the population of FOXP3+ T cells was significantly higher in patients with cervical cancer than in healthy subjects. Jaafar et al. [33] found that in animal models, cytokine overexpression in cervical cancer contributed to the accumulation of FOXP3+ T cells. Further studies reported that FOXP3 expression was changed in benign and malignant cervical lesions. Loddenkemper et al. [34] found that the FOXP3+ Treg population was significantly higher in cervical intraepithelial neoplasia and cervical carcinoma. Scott et al. [35] found that FOXP3 was expressed both in cervical cancer and CIN epithelium. In addition, the expression of FOXP3 mRNA is closely related to the grade of cervical lesions, i.e., the higher the CIN grade the higher the expression of FOXP3 mRNA. Zeng et al. [36] also confirmed the findings of Scott et al. regarding FOXP3 mRNA expression being closely related to cancer progress and positively correlated with the stage of cervical cancer. As FOXP3 is closely associated with the development of cervical cancer, it has become an important candidate gene for cancer research. Whether FOXP3 autoantibody could become a new biomarker of cervical cancer has become an important part of our research.
In our study, we found that the expression of FOXP3 autoantibody is significantly different among patients with malignant tumors, benign tumors and healthy subjects. FOXP3 autoantibody expression is highest in patients with malignant cancers, followed in turn by patients with benign tumors and healthy subjects. These results are in agreement with a previous study showing that FOXP3 expression is elevated as the grade of cervical lesion increases [35]. Our previous results showing that expression of FOXP3 autoantibody is enhanced in patients with esophageal cancer [16], indicate that FOXP3 autoantibody could reflect the changes of cervical lesions to some extent. To our knowledge, this is the first report on FOXP3 autoantibody in cervical cancer. The results indicate that the expression level of FOXP3 autoantibody is significantly higher in patients with stage I and II cervical cancer than in healthy subjects. In addition, patients with stage I cervical cancer, but not patients with stage II cervical cancer, have significantly higher levels of FOXP3 autoantibody than patients with benign tumors, and there is no significant difference in level of FOXP3 autoantibody between patients with stage I and II cervical cancer. These results are similar to our previous results showing that the levels of FOXP3 [16] and p16 [14] autoantibody are highest in patients with stage I esophageal cancer; however, they differ from another report showing that expression of p16 autoantibody is highest in patients with stage IV lung cancer [13]. The mechanisms for the significantly increased expression of FOXP3 autoantibody in patients with early cervical cancer are unclear. Some researchers suggest that it is associated with host response to TAAs and the process of abnormal immune gene regulation during tumorigenesis, while others suggest that it is due to antigen stimulation resulted from destruction of tumor cells [37]. Because of the value of FOXP3 autoantibody in the early diagnosis of cervical cancer and the difficulties in case collection of patients with advanced cervical cancer at first diagnosis, we only tested the expression level of FOXP3 autoantibody in patients with stage I and II cervical cancer. Interestingly, we found that the expression level of FOXP3 autoantibody is higher in patients with stage I cervical cancer than in patients with stage II cervical cancer. Although this difference is not statistically significant, its expression trend is similar to that in patients with esophageal cancer. The changes in the expression level of FOXP3 autoantibody as it gradually reduced as the stage of cancer progressed further demonstrate the value of FOXP3 autoantibody in the early diagnosis of cancer. Overall, the level of FOXP3 autoantibody in patients with stage I cervical cancer is not only the highest, but also has the highest sensitivity of 25.4 % against 90.0 % specificity. Thus, FOXP3 autoantibody may be a biomarker for the early diagnosis of cervical cancer, although this needs to be further confirmed by large-scale sample analysis.
Recent studies have shown that combined detection of a variety of TAA autoantibodies can increase detection sensitivity and specificity [21]. Currently, the first kit in the world based on the theory of TAA autoantibodies, EARLY CDT kit, is now available in Europe and North America. The kit includes 7 TAA autoantibodies and has sensitivity as high as 50 % [38]. In the future, we will screen more TAA autoantibodies, and further evaluate the value of combined detection of multiple TAA autoantibodies.
References
Parkin DM, Bray F, Ferlay J et al (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Yanan Wu (2009) The screening methods of cervical carcinoma at early stage. J Liaoning University Traditional Chin Med 11(6):65–67
Anderson KS, LaBaer J (2005) The sentinel within: exploiting the immune system for cancer biomarkers. J Proteome Res 4(4):1123–1133
Zaenker P, Ziman MR (2013) Serologic autoantibodies as diagnostic cancer biomarkers—a review. Cancer Epidemiol Biomarkers Prev 22(12):2161–2181
Coffer PJ, Burgering BM (2004) Forkhead-box transcription factors and their role in the immune system. Nat Rev Immunol 4(11):889–899
Fontenot JD, Rasmussen JP, Williams LM et al (2005) Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity 22(3):329–341
Hori S, Nomura T, Sakaguchi S (2003) Control of regulatory T cell development by the transcription factor Foxp3. Science 299(5609):1057–1061
Whiteside TL (2014) Regulatory T cell subsets in human cancer: are they regulating for or against tumor progression? Cancer Immunol Immunother 63(1):67–72
Wolf AM, Wolf D, Steurer M et al (2003) Increase of regulatory T cells in the peripheral blood of cancer patients. Clin Cancer Res 9(2):606–612
Woo EY, Chu CS, Goletz TJ et al (2001) Regulatory CD4(+)CD25(+) T cells in tumors from patients with early-stage non-small cell lung cancer and late-stage ovarian cancer. Cancer Res 61(12):4766–4772
Liu L, Liu N, Liu B et al (2012) Are circulating autoantibodies to ABCC3 transporter a potential biomarker for lung cancer? J Cancer Res Clin Oncol 138(10):1737–1742
Cheng Y, Xu J, Guo J et al (2013) Circulating autoantibody to ABCC3 may be a potential biomarker for esophageal squamous cell carcinoma. Clin Transl Oncol 15(5):398–402
Zhang C, Ye L, Guan S et al (2014) Autoantibodies against p16 protein-derived peptides may be a potential biomarker for non-small cell lung cancer. Tumour Biol 35(3):2047–2051
Jin Y, Guan S, Liu L et al (2014) Anti-p16 autoantibodies may be a useful biomarker for early diagnosis of esophageal cancer. Asia Pac J Clin Oncol. doi:10.1111/ajco.12198
Wang W, Guan S, Sun S et al (2014) Detection of circulating antibodies to linear peptide antigens derived from ANXA1 and DDX53 in lung cancer. Tumor Biol 35(5):4901–4905
Ye L, Guan S, Zhang C et al (2013) Circulating autoantibody to FOXP3 may be a potential biomarker for esophageal squamous cell carcinoma. Tumour Biol 34(3):1873–1877
Cunha LL, Morari EC, Nonogaki S et al (2012) Foxp3 expression is associated with aggressiveness in differentiated thyroid carcinomas. Clinics (Sao Paulo) 67(5):483–488
Tan EM, Zhang J (2008) Autoantibodies to tumor-associated antigens: reporters from the immune system. Immunol Rev 222:328–340
Wang LH, Su L, Wang JT (2010) Correlation between elevated FOXP3 expression and increased lymph node metastasis of gastric cancer. Chin Med J (Engl) 123(24):3545–3549
Niu J, Jiang C, Li C et al (2011) Foxp3 expression in melanoma cells as a possible mechanism of resistance to immune destruction. Cancer Immunol Immunother 60(8):1109–1118
Tan HT, Low J, Lim SG et al (2009) Serum autoantibodies as biomarkers for early cancer detection. FEBS J 276(23):6880–6904
Chen H, Werner S, Tao S et al (2014) Blood autoantibodies against tumor-associated antigens as biomarkers in early detection of colorectal cancer. Cancer Lett 346(2):178–187
Werner S, Chen H, Tao S et al (2014) Systematic review: serum autoantibodies in the early detection of gastric cancer. Int J Cancer. doi:10.1002/ijc.28807
Erfani N, Hamedi-Shahraki M, Rezaeifard S et al (2014) FoxP3+ regulatory T cells in peripheral blood of patients with epithelial ovarian cancer. Iran J Immunol 11(2):105–112
Hanakawa H, Orita Y, Sato Y et al (2014) Regulatory T-cell infiltration in tongue squamous cell carcinoma. Acta Otolaryngol 134(8):859–864
Azzimonti B, Zavattaro E, Provasi M et al (2015) Intense Foxp3+ CD25+ regulatory T cell infiltration is associated with high-grade cutaneous squamous cell carcinoma and counterbalanced by CD8+ /Foxp3+ CD25+ ratio. Br J Dermatol 172(1):64–73
Shibuya KC, Goel VK, Xiong W et al (2014) Pancreatic ductal adenocarcinoma contains an effector and regulatory immune cell infiltrate that is altered by multimodal neoadjuvant treatment. PLoS One 9(5):e96565
Kim S, Lee A, Lim W et al (2014) Zonal difference and prognostic significance of FOXP3 regulatory T cell infiltration in breast cancer. J Breast Cancer 17(1):8–17
Raghavan S, Quiding-Järbrink M (2011) Regulatory T cells in gastrointestinal tumors. Expert Rev Gastroenterol Hepatol 5(4):489–501
Merlo A, Casalini P, Carcangiu ML et al (2009) FOXP3 expression and overall survival in breast cancer. J Clin Oncol 27(11):1746–1752
Wolf AM, Rumpold H, Wolf D et al (2007) Role of forkhead box protein 3 expression in invasive breast cancer. J Clin Oncol 25(28):4499–4500
Hou F, Li Z, Ma D et al (2012) Distribution of Th17 cells and Foxp3-expressing T cells in tumor-infiltrating lymphocytes in patients with uterine cervical cancer. Clin Chim Acta 413(23–24):1848–1854
Jaafar F, Righi E, Lindstrom V et al (2009) Correlation of CXCL12 expression and FoxP3+ cell infiltration with human papillomavirus infection and clinicopathological progression of cervical cancer. Am J Pathol 175(4):1525–1535
Loddenkemper C, Hoffmann C, Stanke J et al (2009) Regulatory (FOXP3+) T cells as target for immune therapy of cervical intraepithelial neoplasia and cervical cancer. Cancer Sci 100(6):1112–1117
Scott ME, Ma Y, Kuzmich L et al (2009) Diminished IFN-gamma and IL-10 and elevated FOXP3 mRNA expression in the cervix are associated with CIN 2 or 3. Int J Cancer 124(6):1379–1383
Zeng C, Yao Y, Jie W et al (2013) Up-regulation of Foxp3 participates in progression of cervical cancer. Cancer Immunol Immunother 62(3):481–487
Caron M, Choquet-Kastylevsky G, Joubert-Caron R (2007) Cancer immunomics using autoantibody signatures for biomarker discovery. Mol Cell Proteomics 6(7):1115–1122
Chapman CJ, Healey GF, Murray A et al (2012) Early CDT®-Lung test: improved clinical utility through additional autoantibody assays. Tumour Biol 33(5):1319–1326
Acknowledgments
This study was supported by Jilin Pharmaceutical Industry Development Special Fund Project (No. 130701YY01066802). We would like to acknowledge Dr. Cui Manhua and colleagues for their help and support with serum sample processing.
Conflict of interest
All the authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
About this article
Cite this article
Xu, S., Huangfu, M., Jia, X. et al. FOXP3 autoantibody as a potential early prognostic serum biomarker in patients with cervical cancer . Int J Clin Oncol 20, 982–988 (2015). https://doi.org/10.1007/s10147-015-0797-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0797-4