Abstract
This study aimed to comparatively assess cervical sagittal alignment, progression of ossification of the posterior longitudinal ligament (OPLL), and health-related quality of life (HRQOL) outcomes between patients who underwent cervical laminoplasty (CL) and those who underwent cervical laminectomy with fusion (LF) for cervical OPLL at more than three levels. We retrospectively evaluated consecutive 91 patients with cervical OPLL undergoing CL (n = 49) or LF (n = 42) who were followed up for at least 24 months (mean 38.6 months). We analyzed radiological measurements (C2–7 sagittal vertical axis [C2–7 SVA], C0–2 angle, C2–7 lordotic angle, T1 slope, and range of motion [ROM]), OPLL thickness, and clinical outcomes (visual analog scale [VAS], neck disability index [NDI], Short Form-36, and Japanese Orthopaedic Association [JOA] scores). Compared with preoperative levels, postoperative C2–7 SVA increased significantly increased in the LF (15.05 mm) and CL (7.86 mm) groups (P = 0.0021). Loss of cervical lordosis and ROM was significantly larger in the cervical LF group (P = 0.0296, P = 0.0004). Improvements in HRQOL, JOA recovery ratio, and VAS were similar between both groups, while NDI improved more significantly in the CL group (P = 0.0425). The postoperative neck VAS correlated positively with the change (Δ) of C2–7 SVA (P = 0.0174) and negatively with the change (Δ) of C2–7 lordotic angle (P = 0.0354). Progression of OPLL thickness in the LF (0.31 ± 0.37 mm) was significantly smaller than in the CL group (1.09 ± 0.64 mm) (P < 0.0001). CL was superior to LF in preserving cervical ROM, preoperative cervical lordosis, and minimizing neck disability. The stabilization obtained by adding instrumented fusion could suppress the progression of OPLL thickness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posterior decompression surgeries have been widely performed to adequately decompress the spinal cord, although they cannot directly remove ossification of the posterior longitudinal ligament (OPLL) [3, 14, 19, 33]. In patients with cervical myelopathy caused by OPLL in more than three segments, posterior decompression is more attractive than anterior decompression because the latter can prevent the need for an anterior route or major strut graft-related problems, such as cerebrospinal fluid leakage, pseudoarthrosis, or graft dislodgment [2, 37].
Cervical laminoplasty (CL) and laminectomy with fusion (LF) are two common posterior decompression surgeries for the treatment of cervical myelopathy with multilevel OPLL. Laminoplasty has been reported to diminish cervical lordosis postoperatively, and postoperative kyphotic deformities are considered a source of pain and disability [12, 21, 25, 31, 44]. On the other hand, cervical LF was reported to provide improvement and maintenance of cervical lordotic alignment [1, 8, 27, 42]. It has also been reported that augmentation with posterior fixations could provide stronger biomechanical strength to prevent cervical OPLL progression and to reduce postlaminectomy kyphosis and instability [8, 27]. There was no consensus in the literature concerning the superiority of CL or LF on cervical alignment and clinical outcomes in the treatment of cervical myelopathy caused by more than three segments OPLL. This controversy is perpetuated by the paucity of studies comparing laminoplasty and LF performed by a single surgeon [5, 6, 29].
We compared CL with LF to treat cervical compressive myelopathy (CCM) in patients with OPLL at more than three levels. The purpose of this study was to comparatively assess cervical sagittal alignment, OPLL progression, and clinical outcomes, including patient-reported pain and HRQOL, between patients who underwent CL and those who underwent LF.
Materials and methods
Patient demographics
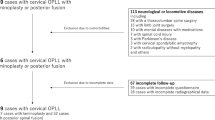
This study was approved by the local ethical committee and the institutional review board (SGPAIK 2018-05-014). This was a retrospective cohort study. From January 2013 to January 2016, we treated 494 consecutive patients with cervical spine diseases. Of these 494 patients, 110 (22.3%) had ventral cord compression with OPLL at more than three levels. Four patients who underwent anterior cervical decompression and 15 who underwent combined anteroposterior surgeries were excluded from this study.
Ninety-one patients (69 men and 22 women) with a mean age of 60.5 years (range 38–77 years) underwent posterior cervical decompression surgery such as CL or LF to treat CCM associated with OPLL at more than three levels. CCM was diagnosed using magnetic resonance imaging (MRI) with radiological confirmation, and the diagnosis was determined when there was one or more upper motor neuron domain (e.g., spasticity, hyper-reflexia, or a positive Babinski sign), based on a neurological examination [4].
We excluded patients with one- or two-level segmental OPLL, other acute traumatic cord injuries with cervical bony fractures caused by high-energy trauma, or other confirmed neurological disorders (e.g., cerebral palsy, Parkinson’s disease, multiple sclerosis, or polio). Patients with ossification of the yellow ligament and those with a history of cervical spine surgery were also excluded.
We determined whether to perform CL or LF according to radiological factors (instability, cervical curvature [lordotic, straight, kyphotic], or cord compression ratio) or patient age. The C2–C7 Cobb angle was used to define lordosis (Cobb angle < − 10°), straight (Cobb angle − 10 to 0°), and kyphosis (Cobb angle > 0°) [22]. We preferred cervical LF for cases with straight or lordotic cervical curvature and segmental instability to prevent kyphosis development and instability aggravation postoperatively. In addition, we preferred to perform LF to widely decompress the spinal cord in patients with severe cord compression caused by OPLL. If the patients were younger than 60 years, we recommended CL to preserve neck motion. The surgical procedure was selected an individual case-by-case basis.
Patient age, sex, duration of symptoms, medical conditions, and radiographic findings were investigated. The presence of OPLL was confirmed with X-ray or three-dimensional computed tomography (3D CT). All patients underwent high-resolution MRI using a 1.5T Avanto unit (Siemens Medical System, Erlangen, Germany) imaging unit prior to surgery. We defined complications as events that occurred within 1 month postoperatively. We analyzed neurological recovery in patients who completed at least 24 months of follow-up.
Operative technique
The patients were placed in the prone position under general anesthesia. A standard posterior midline approach was used. CL was performed based on the neurological symptoms and the extent of cord compressed levels, including the most narrowed side on images. Unilateral or bilateral gutters were made using a high-speed drill in the area between the facet joints and laminae, and the spinous processes were split sagittally with a high-speed burr. The spinal canal was enlarged by opening the split laminae unilaterally or bilaterally with a spreader. Posterior cervical titanium miniplates (Centerpiece®, Medtronic Sofamor Danek, Memphis, TN, USA) or hydroxyapatite spacers (Apacerum®, Asahi Optical Co., Ltd., Tokyo, Japan) were used to keep the “door” open.
We performed cervical LF using a posterior screw-rod system for OPLL patients with straight, lordotic cervical curvature, or segmental instability to prevent local kyphosis after decompression. Following complete decompression of the neural elements, lateral mass or pedicle screw and rod instrumentation (Vertex®, Medtronic Sofamor Danek, Memphis, TN, USA) was performed. During fixation, we cut the rod into an appropriate length to fit each patient and bent it to fit the lordotic curve. After lordotic rods were applied, locking nuts were tightened firmly. The perizygapophysial joints were filled with autologous bone fragments from the excised lamina. Postoperatively, all patients were required to wear Miami neck collars or Philadelphia braces for approximately 3 months. The patients were followed clinically with plain and dynamic radiography at 1, 3, and 6 months and then every 6 months postoperatively.
Radiographic assessment
Cervical spine radiological measurements were made by assessing the following parameters: (1) C2–7 sagittal vertical axis (C2–7 SVA), (2) C0–2 angle, (3) C2–7 lordotic angle, (4) T1 slope, and (5) total range of motion (ROM). The C2–7 SVA was defined as the distance between the posterosuperior corner of C7 and a vertical line from the center of the C2 body. The C0–2 angle was measured using a Cobb angle between the McGregor line and the C2 lower end plate. Cervical lordosis was assessed with the C2–7 lordotic angle. The C2–7 lordotic angle was defined as the Cobb angle formed by the inferior endplate of C2 and C7 on a standing lateral radiograph. The T1 slope was measured as the angle between a horizontal line and the superior endplate of T1 (Fig. 1). The total ROM of the cervical spine was defined as the summation of alignment during flexion and extension on radiographs. Changes in the cervical alignment were defined as the difference between the pre- and postoperative cervical sagittal parameters [15, 29]. CT scanning was performed preoperatively for all patients. The occupying ratio of the spinal canal was measured on a CT sagittal view (Fig. 2). The thickness of the OPLL was measured as the thickest part of the OPLL by sagittal thin cut CT images [35]. The progression of OPLL thickness was defined as the subtraction between pre- and postoperative OPLL thickness. We also assessed signal intensity changes on MRI T2-weighted images. All the surgeries enrolled in this study were performed by a single surgeon (JJS). Radiographic measurement data were collected and reviewed by two surgeons (YH and JJS).
Radiological parameters. The C2–7 sagittal vertical axis (the distance from the posterosuperior corner of C7 and a vertical line from the center of the C2 body), C0–2 angle (a Cobb angle between the McGregor line and the C2 lower end plate), C2–7 lordotic angle (Cobb angle between the inferior endplate of C2 and C7), and T1 slope (the angle between a horizontal line and the superior endplate of T1) were measured on neutral lateral radiographs
Clinical outcome assessment
The clinical outcomes were assessed using the patient-reported visual analog scale for neck pain (VAS-N) and arm pain (VAS-A), neck disability index (NDI), Short Form-36 health survey questionnaire (SF-36), and the Japanese Orthopaedic Association (JOA) score. These data were obtained for all patients preoperatively and for at least 2 years postoperatively. The neurological outcomes were evaluated according to the JOA scale for cervical myelopathy [15]. The postoperative recovery rates were calculated using the following formula:
Statistical analysis
All values are expressed as mean ± standard deviation or percentage. Normally distributed data were compared using Student’s t test or the chi-squared test, as appropriate for the data set. Data with a non-normal distribution were evaluated using a nonparametric analysis, and the Mann-Whitney U test was used to evaluate differences between the two groups. Pearson’s correlation analysis was used to evaluate the relationships between the JOA recovery ratio and age, cervical spine parameters, occupying ratio of the spinal canal, and pre- and postoperative VAS-N, VAS-A, NDI, SF-36, and JOA scores. All statistical analyses were performed using MedCalc version 18.11.6 (MedCalc, Mariakerke, Belgium), and a P value < 0.05 was considered statistically significant.
Results
Ninety-one patients (69 men and 22 women) were evaluated. Forty-two patients who had multilevel cervical OPLL were surgically treated with cervical LF. Forty-nine patients were treated with CL, which is unilateral open-door laminoplasty with titanium miniplates (40) or bilateral double-door laminoplasty with spacers (9). The average follow-up period was 38.6 months (range 27.8–46.2; 37.51 for cervical LF patients and 39.61 for CL patients). The mean age at the time of surgery was 60.5 years (range 38–77). There were more male than female patients.
The mixed type of OPLL was the most prevalent in patients who underwent surgery. The average number of operated-upon levels was 3.12 in the LF group and 3.04 in the CL group (P = 0.1917). OPLL in the upper cervical (C2) or cervicothoracic area (C7) was more frequently observed in LF (8/42, 19.05%) than in the CL group (4/49, 8.16%). The preoperative occupying ratio was higher in the CL group than that in the LF group, while the prevalence of preoperative signal intensity changes on T2-weighted MRIs was higher in the CL group than that in the LF group. However, there were no statistically significant differences between the two groups. There was no significant difference regarding the operation time (P = 0.1242) and the amount of bleeding (P = 0.7950) between the two groups. The demographic characteristics of the patients in this study are summarized in Table 1.
Radiological results
The mean preoperative C2–7 lordotic angles were 15.40 ± 6.27° in LF and 12.75 ± 7.82° in CL (P = 0.0807). There were no patients with kyphotic angles in the preoperative phase. In addition, there were no statistically significant differences in other cervical radiological parameters on the preoperative phase between the cervical LF and CL groups (Table 2). After posterior decompression, the C2–7 lordotic angle was reduced, ROM was restricted, and the C0–2 lordotic angle was increased compared with the preoperative cervical radiological parameters. Postoperatively, cervical alignment in patients in the cervical LF group tilted forward compared with that of patients in the CL group. The mean C2–7 SVA in the LF group significantly increased from 19.34 ± 8.51 mm at the preoperative phase to 24.89 ± 8.56 mm at 6 months postoperatively, 30.98 ± 8.42 mm at 12 months postoperatively, and 34.39 ± 15.04 mm at the last follow-up examination. On the other hand, C2–7 SVA increased from 19.53 ± 9.18 to 21.76 ± 9.17 mm at 6 months postoperatively, 24.13 ± 9.18 mm at 12 months postoperatively, and 27.40 ± 11.30 mm at the last follow-up in the CL group (Table 2) (Fig. 3). The change (Δ) in the C2–7 SVA was significantly different between the LF (15.05 ± 13.87 mm) and CL (7.86 ± 7.14 mm) groups (P = 0.0021). The mean C2–7 lordotic angle in the LF group significantly decreased from 15.40 ± 6.27° preoperatively to 8.20 ± 6.43° at the last follow-up examination, while it decreased from 12.75 ± 7.82 to 9.00 ± 7.17° in the CL group (Fig. 3). The change (Δ) in the C2–7 lordotic angle was significantly different between the LF (− 7.20 ± 8.53°) and CL groups (− 3.75 ± 6.35°) (P = 0.0296). However, the changes (Δ) in the C0–2 angle were not significantly different between the LF and CL groups. The change (Δ) in T1 slope was larger in LF than in the CL group at 12 months postoperatively (P < 0.0001), but not significantly different at the last follow-up (P = 0.0560) (Table 2).
Changes in the radiological parameters. a The change in cervical lordosis at the time point of measurement. The mean C2–7 lordotic angle of LF significantly decreased compared with that of CL. The mean cervical lordosis of LF decreased from 15.40 ± 6.27° in the preoperative phase to 12.78 ± 6.23° at 6 months postoperatively, 10.89 ± 6.13° at 12 months postoperatively, and 8.20 ± 6.43° at the last follow-up. The mean cervical lordosis of CL decreased from 12.75 ± 7.82 to 10.94 ± 7.76° at 6 months postoperatively, 9.97 ± 7.97° at 12 months postoperatively, and 9.00 ± 7.17° at the last follow-up. b The change in C2–7 SVA at the time point of measurement. The mean C2–7 SVA in the LF group significantly increased compared with that of CL. The mean C2–7 SVA of LF increased from 19.34 ± 8.51 mm at the preoperative phase to 24.89 ± 8.56 mm at 6 months postoperatively, 30.98 ± 8.42 mm at 12 months postoperatively, and 34.39 ± 15.04 mm at the last follow-up examination. The mean C2–7 SVA of CL increased from 19.53 ± 9.18 to 21.76 ± 9.17 mm at 6 months postoperatively, 24.13 ± 9.18 mm at 12 months postoperatively, and 27.40 ± 11.30 mm at the last follow-up. c The change in global ROM at the time point of measurement. The mean global ROM of LF significantly increased compared with that of CL. The mean global ROM of LF increased from 40.13 ± 9.06° at the preoperative phase to 32.80 ± 9.22° at 6 months postoperatively, 21.63 ± 11.49° at 12 months postoperatively, and 18.55 ± 9.58° at the last follow-up examination. The mean global ROM of CL increased from 37.85 ± 9.14 to 35.82 ± 9.40° at 6 months postoperatively, 32.60 ± 9.83° at 12 months postoperatively, and 29.21 ± 11.02° at the last follow-up. C2-7 SVA C2-7 sagittal vertical axis, ROM range of motion, LF laminectomy with fusion, CL cervical laminoplasty, Preop preoperative, 6 M 6 months postoperative, 12 M 12 months postoperative, 24 M 24 months postoperative
The incidence of the loss of cervical lordosis after decompression surgery was 74.73% (68/91), and 85.71% of the patients (36/42) in the LF group and 65.31% (32/49) of the patients in the CL group lost cervical lordosis postoperatively. The percentage of patients who lost cervical lordosis postoperatively in the LF group was significantly higher than that of patients in the CL group (P = 0.0264).
Preoperatively, the average cervical ROMs in patients in the LF and CL groups were 40.13 ± 9.06° and 37.85 ± 9.14°, respectively. At the last follow-up examination, patients in the LF group experienced a significant reduction in ROM compared with those in the CL group (Fig. 3). The mean reduction of ROM was 46.96% of the preoperative ROM in the LF group and 84.86% of the preoperative ROM in the CL group. The magnitude of lost ROM was much larger in the LF group than that in the CL group.
At last follow-up, cervical 3D CT scan was performed on 26 of 42 patients who underwent LF and 24 of 49 patients who underwent CL. The mean time of last follow-up cervical CT was 36.94 ± 16.90 months in the LF group and 43.59 ± 21.23 months in CL, and the difference was not statistically significant (P = 0.1400). The thickness of OPLL in the preoperative phase was 5.35 ± 1.37 mm in LF and 5.00 ± 1.28 mm in CL (P = 0.3638). At last follow-up, the thickness of the OPLL was 5.66 ± 1.33 mm in LF and 6.09 ± 1.37 mm in CL (P = 0.2618). Progression of the thickness of the OPLL in the LF group (0.31 ± 0.37 mm) was significantly smaller than in the CL group (1.09 ± 0.64 mm) (P < 0.0001) (Fig. 4). The decrease in OPLL thickness was more frequently observed in the LF than in the CL groups. Six (23.08%) of the 26 participants who underwent LF experienced a suppression of preoperative OPLL thickness, while 1 (4.17%) of the 24 participants who underwent CL experienced a suppression of OPLL thickness.
Progression of OPLL thickness. The OPLL thickness was compared between LF and CL groups using sagittal views of three-dimensional computed tomography pre- and postoperatively. Progression of OPLL thickness in LF (0.31 ± 0.37 mm) was significantly smaller than in the CL group (1.09 ± 0.64 mm, P < 0.0001). OPLL ossification of posterior longitudinal ligament, LF laminectomy with fusion, CL cervical laminoplasty
Clinical results
All clinical parameters were significantly improved at least 24 months postoperatively. The postoperative VAS-A scores and HRQOL were similar between the two groups (Table 3). The postoperative VAS-N scores (LF 3.05 ± 1.31 vs. CL 1.88 ± 1.11) and NDI (LF 16.40 ± 7.66 vs. CL 11.82 ± 5.02) were significantly higher in the LF than in the CL group (P < 0.0001 and P = 0.0029). The mean improvement of VAS-N scores from preoperative to the last follow-up was not significantly higher in the CL group (2.29 ± 1.91) compared to the LF group (1.86 ± 2.24) (P = 0.3409). On the other hand, the CL group had a significantly greater mean improvement in NDI from preoperative to the last follow-up compared to the LF group (P = 0.0425). The JOA recovery ratio was improved in the LF (47.81 ± 23.97%) and CL groups (55.31 ± 17.99%), but significant differences were not seen (P = 0.1394) (Table 3). The overall change (Δ) in the C2–7 SVA correlated positively with neck VAS at the final follow-up (R2, 0.0619; P = 0.0174). The change (Δ) in the C2–7 lordotic angle correlated negatively with neck VAS at the final follow-up (R2, 0.0487; P = 0.0354).
Complications
Surgery-related complications occurred in 9 patients (9.89%) with C5 nerve palsy 6 (14.29%, 6/42) in the LF group and 3 in the CL group (6.12%, 3/49). Most of the patients recovered within 3 months, but one patient had sustained, unilateral C5 nerve palsy. Furthermore, one patient who underwent CL had a hematoma that developed 3 h postoperatively. We immediately removed the hematoma, but C5 nerve palsy remained on the patient’s right side. Superficial wound infections occurred in 5 patients, but no additional surgery was required to remove instrumentation.
Discussion
CL has some disadvantages including postoperative kyphosis and the potential development of worsening or new onset axial neck pain postoperatively [21, 25, 31, 44]. Such concerns can be treated by alternative posterior techniques such as LF. Cervical LF has been reported to prevent postoperative loss of lordosis and decrease axial neck pain and disability [8, 27]. We compared clinical outcomes including SF-36, neck pain, and disability, and radiological outcomes after laminoplasty versus LF for multilevel cervical OPLL. This study elucidated that compared to LF, CL improved clinical outcomes, such as VAS neck pain and NDI scores, and it did not aggravate patient-reported neck pain. CL preserved preoperative cervical alignment and ROM more than that by cervical LF. Cervical sagittal malalignment, such as increase in C2–7 SVA and loss of lordosis, was associated with axial neck pain postoperatively. The stabilization obtained by the addition of instrumented fusion could suppress the progression of OPLL.
CL caused regional malalignment and loss of lordotic curvature of the cervical spine in the literature [26, 40]. The loss of cervical lordosis or kyphotic deformity after CL was variously reported to occur in 33 to 70.7% of cases [26, 31, 40]. Postoperative kyphosis and kyphotic change were associated with poor clinical outcomes and progressive kyphosis lead to late neurological deterioration in a long-term follow-up study [21, 31, 37, 40, 44]. Sakai et al. announced that the C2–7 SVA increased after CL [37], which was not suitable for cervical myelopathy patients with preoperative cervical sagittal imbalance. Tang et al. reported that larger C2-C7 SVA negatively affected HRQOL scores, and the severity of disability increased with positive sagittal malalignment [40]. It has been known that the increase of C2–7 SVA and loss of C2–7 Cobb angle have been regarded as negative indicators for clinical outcome after surgery [36, 40]. In contrast, some researchers reported that postoperative malalignment or kyphotic change was not associated with poor clinical outcomes [22, 24, 27]. In general, for patients with significant preoperative kyphosis or a high risk of developing kyphosis, CL should be avoided because of postoperative kyphotic deformity and aggravation of neurological deficits [20]. To avoid these drawbacks, it has been reported that augmentation with posterior fixations could provide stronger biomechanical strength and reduce postlaminectomy kyphosis and instability [1, 27]. Therefore, some surgeons insisted that posterior screw augmentation after laminectomy could prevent postoperative kyphotic deformities, axial pain, and instability [1, 20]. Furthermore, LF could provide improvement and maintenance in cervical lordosis for cases with the OPLL than CL [27]. In the present study, the loss of cervical lordosis developed in 74.73% of the patients after posterior decompression, which was 85.71% in the LF group and 65.31% in the CL group. Contrary to previous reports, the incidence of postoperative kyphosis was larger in LF than in laminoplasty. After LF, patients experienced neck tilting forward, that is increased C2–7 SVA, but not in CL. Based on the above results, supplementation with screw fixation after posterior decompression did not allow us to maintain the preoperative cervical alignment.
Traditionally, it has been known that cervical laminectomy and instrumented fusion significantly improved neck pain [6], while laminoplasty has been associated with shoulder and neck pain [6, 7]. However, in the present study, CL yielded a slightly improvement in postoperative neck pain (VAS-N) than LF. The neck disability was more severe after cervical LF than after laminoplasty. The explanations are as follows. Posterior decompression surgeries, such as CL and LF, cause inevitable damage to the posterior muscular-ligament complex and disrupt the original cervical alignment. When cervical LF is performed, the posterior neck muscles should be dissected extensively to confirm the screw’s entry point, compared with the muscle exposure procedure used in CL. As the level of surgical invasion of the posterior muscular-ligament complex increases, cervical sagittal balance decreases [26]. Despite the use of posterior screw augmentation to stabilize the bony and joint structures, the compensatory mechanism did not work after the musculo-ligamentous complex was damaged. In the present study, the increase of T1 slope tended to be larger in LF than in laminoplasty to maintain the lordotic curve, but that was not significant enough to compensate the malalignment. As a result, invasion of the posterior muscular-ligament complex and regional malalignment, such as loss of cervical lordosis and anterior neck tilt, increased energy expenditure in relation to the head’s position and horizontal gaze. These factors could explain why patients experienced axial neck pain and neck disability after undergoing posterior decompression surgery, particularly those who underwent the cervical LF technique. Consequentially, sagittal imbalance after posterior decompression surgery of the cervical spine would be related to the clinical outcome, particularly postoperative axial neck pain and neck disability.
Some authors have introduced surgical techniques to reduce postoperative neck pain and maintain regional alignment [12, 17, 22, 37]. Kim et al. reported myoarchitectonic spinolaminoplasty without damaging the attachments of the semispinalis cervicis, multifidus, interspinales, and rotator muscles, which could prevent postoperative instability, decrease the incidence of postoperative kyphosis, and preserve the ROM of the C2–7 angle at 1 year after surgery [10, 14]. In addition, Nolan et al. reported that maintaining the paraspinal musculature at C2 and C7 was important during a posterior cervical operation because involvement of the C2 and C7 vertebrae might affect the postoperative cervical sagittal balance [34]. If OPLL was involved in the cervico-thoracic junction, Lapsiwala et al. insisted that long fusions should be extended to traverse the junction in order to prevent pseudoarthrosis or iatrogenic kyphotic deformity in the area [20]. The extended fixation of the upper thoracic spine is to prevent postoperative kyphosis and potential risk of additional cord injury by reducing dynamic factors [30, 43].
OPLL size
In addition to sagittal alignment, radiographs were used to assess the thickness of OPLL. OPLL growth has been reported to be observed more frequently by laminoplasty than by LF [13, 23, 35]. The present study showed that supplementation with screw fixation after posterior decompression suppressed thickening of the OPLL as well as decreased the thickness of the OPLL. Koda et al. reported spontaneous reduction of the thickness of the thoracic OPLL after posterior decompression with fusion [17, 18]. Miyashita et al. explained that the decrease in dural pulsation after posterior stabilization might cause the reduction in thickness of the thoracic OPLL [32]. Posterior stabilization with screw fixation may remove the mechanical stimulus for cervical OPLL and suppress its progression through a similar mechanism [35]. In three-dimensional OPLL volume studies [11, 13, 23], posterior instrumented fusion has the effect of reducing OPLL growth rate compared with motion-preserving CL.
ROM
ROM of the cervical spine was reported to be restricted by posterior decompression surgeries such as CL or LF [9, 29]. Several reports have described reductions in ROM of 30 to 70% of the preoperative ROM after CL [9, 29]. Blizzard et al. reported that the ROM was reduced by up to 27.11% of the preoperative ROM after cervical LF [3]. In the present study, patients who underwent cervical LF experienced a significant reduction in ROM compared with those who underwent CL. CL is advantageous because it can preserve the cervical spine’s motions compared with multilevel LF.
Clinical outcomes
Previous studies have addressed the relationship between cervical sagittal alignment and HRQOL [40]. In the present study, decompression surgeries including cervical LF and CL were associated with similar improvements in QOL scores such as the SF-36 and JOA scores.
Kimura et al. reported that laminoplasty worsened or created new onset axial neck pain postoperatively [16, 39, 41]. In the present study, we compared neck pain and disability after laminoplasty versus LF for multilevel cervical OPLL. VAS neck pain scores significantly decreased in the CL than in the LF group at 2 years postoperative, but the difference in the neck VAS improvement from preoperative to the last follow-up was not statistically different between two groups. Neck disability was significantly improved by CL rather than LF. Although the difference in NDI improvement could be assessed as minimal clinically significant differences, the NDI actually decreased more in the CL than in the LF group. Because there were baseline differences in VAS neck pain scores and NDI between LF and CL groups, our results do not imply the clinical superiority of one technique versus another in all OPLL patients who underwent posterior decompression. Based on our results, laminoplasty improved clinical outcomes, such as VAS-N and NDI scores rather than LF, and does not at least aggravate patient-reported neck pain.
Shou et al. performed a meta-analysis that focused on the prevalence of C5 nerve root palsy postoperatively and demonstrated that cervical LF was associated with a high prevalence of C5 nerve root palsy (11.0%) [38]. The findings of the current study are consistent with those of previous studies [28, 34], reporting that there was a higher prevalence of C5 nerve root palsy after cervical LF (14.29%) than there was after CL (6.12%).
Limitations
This study has several limitations. First, the study was a retrospective, consecutive patient series, and inequalities between the groups inevitably existed. This study has an inherent patient selection bias when comparing surgical procedures because indications for expansive laminoplasty and cervical LF tend to be different. We preferred cervical LF for cases with straight or lordotic cervical curvature and segmental instability to prevent kyphosis development and instability aggravation postoperatively. On the other hand, we recommended CL for patients who were younger than 60 years because of its ability to preserve neck motion with less substantial alteration to the natural biomechanics of the cervical spine. Therefore, future prospective studies or randomized trials are warranted to address these drawbacks. Another limitation of this study is the small number of patients, with a retrospective case series based on a single surgeon’s experience. Second, the radiographical analysis period was relatively short (mean 38.6 months), and a longer follow-up period will be required to determine the durability of these study findings. Third, measurement of neck muscles mass was not evaluated in this study. It is necessary to assess the relationship between loss of neck muscle mass and spinal malalignment. Fourth, this study used two-dimensional images to measure OPLL growth; so, it was difficult to determine three-dimensional OPLL volume change accurately. Fifth, the whole-spine sagittal alignment, which was affected by cervical alignment postoperatively, was not included in the analysis. Further studies are needed to determine whether patients will have whole-spine sagittal imbalance in the long term. A prospective, randomized study would likely result in higher quality comparisons.
Recommendations
When evaluating the above results, postoperative kyphosis was associated with postoperative neck pain after posterior decompression, particularly cervical LF. For patients with the risk of developing kyphosis, CL with minimal damage of musculo-ligamentous complex would be recommended for the treatment of multilevel cervical OPLL. Because supplementation with screw fixation suppressed the progression of OPLL, cervical LF would likely be considered in large size OPLL cases even if it has a high prevalence of C5 nerve palsy. Surgeons using cervical LF should be aware of insufficiency to maintain the preoperative cervical alignment and should consider traversing the cervico-thoracic junction to prevent kyphotic deformity, as suggested by previous studies [20, 30, 43].
Conclusion
CL and LF were effective surgical techniques to improve the patient-reported outcomes and HRQOL of patients with OPLL at more than three levels. CL preserved cervical lordosis and ROM and improved neck disability, more than LF. Cervical regional malalignment after posterior decompression was related to the clinical outcome, particularly axial neck pain. The stabilization obtained by addition of instrumented fusion could suppress the progression of OPLL.
Study design
Retrospective cohort study.
References
Anakwenze OA, Auerbach JD, Buck DW, Garg S, Simon SL, Sutton LN, Sponseller PD, Dormans JP (2011) The role of concurrent fusion to prevent spinal deformity after intramedullary spinal cord tumor excision in children. J Pediatr Orthop 31:475–479
Arvind V, Kim JS, Oermann EK, Kaji D, Cho SK (2018) Predicting surgical complications in adult patients undergoing anterior cervical discectomy and fusion using machine learning. Neurospine 15:329–337
Blizzard DJ, Caputo AM, Sheets CZ, Klement MR, Michael KW, Isaacs RE, Brown CR (2017) Laminoplasty versus laminectomy with fusion for the treatment of spondylotic cervical myelopathy: short-term follow-up. Eur Spine J 26:85–93
Cho YE, Shin JJ, Kim KS, Chin DK, Kuh SU, Lee JH, Cho WH (2011) The relevance of intramedullary high signal intensity and gadolinium (Gd-DTPA) enhancement to the clinical outcome in cervical compressive myelopathy. Eur Spine J 20:2267–2274
Heller JG, Edwards CC 2nd, Murakami H, Rodts GE (2001) Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine (Phila Pa 1976) 26:1330–1336
Highsmith JM, Dhall SS, Haid RW Jr, Rodts GE Jr, Mummaneni PV (2011) Treatment of cervical stenotic myelopathy: a cost and outcome comparison of laminoplasty versus laminectomy and lateral mass fusion. J Neurosurg Spine 14:619–625
Hosono N, Yonenobu K, Ono K (1996) Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976) 21:1969–1973
Huang RC, Girardi FP, Poynton AR, Cammisa FP Jr (2003) Treatment of multilevel cervical spondylotic myeloradiculopathy with posterior decompression and fusion with lateral mass plate fixation and local bone graft. J Spinal Disord Tech 16:123–129
Hyun SJ, Riew KD, Rhim SC (2013) Range of motion loss after cervical laminoplasty: a prospective study with minimum 5-year follow-up data. Spine J 13:384–390
Itoki K, Kurokawa R, Shingo T, Kim P (2018) Effect of myoarchitectonic spinolaminoplasty on concurrent hypertension in patients with cervical spondylotic myelopathy. Neurospine 15:77–85
Izumi T, Hirano T, Watanabe K, Sano A, Ito T, Endo N (2013) Three-dimensional evaluation of volume change in ossification of the posterior longitudinal ligament of the cervical spine using computed tomography. Eur Spine J 22:2569–2574
Kato Y, Iwasaki M, Fuji T, Yonenobu K, Ochi T (1998) Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg 89:217–223
Katsumi K, Izumi T, Ito T, Hirano T, Watanabe K, Ohashi M (2016) Posterior instrumented fusion suppresses the progression of ossification of the posterior longitudinal ligament: a comparison of laminoplasty with and without instrumented fusion by three-dimensional analysis. Eur Spine J 25:1634–1640
Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T (2007) Myoarchitectonic spinolaminoplasty: efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine 7:293–304
Kim TH, Ha Y, Shin JJ, Cho YE, Lee JH, Cho WH (2016) Signal intensity ratio on magnetic resonance imaging as a prognostic factor in patients with cervical compressive myelopathy. Medicine (Baltimore) 95:e4649. https://doi.org/10.1097/MD.0000000000004649
Kimura A, Endo T, Inoue H, Seichi A, Takeshita K (2015) Impact of axial neck pain on quality of life after laminoplasty. Spine (Phila Pa 1976) 40:E1292–E1298
Kimura H, Fujibayashi S, Takemoto M, Otsuki B, Matsuda S (2014) Spontaneous reduction in ossification of the posterior longitudinal ligament of the thoracic spine after posterior spinal fusion without decompression: a case report. Spine (Phila Pa 1976) 39:E417–E419
Koda M, Furuya T, Okawa A, Aramomi M, Inada T, Kamiya K, Ota M, Maki S, Ikeda O, Takahashi K, Mannoji C, Yamazaki M (2015) Bone union and remodelling of the non-ossified segment in thoracic ossification of the posterior longitudinal ligament after posterior decompression and fusion surgery. Eur Spine J 24:2555–2559
Kwon SY, Shin JJ, Lee JH, Cho WH (2015) Prognostic factors for surgical outcome in spinal cord injury associated with ossification of the posterior longitudinal ligament (OPLL). J Orthop Surg Res 10:94
Lapsiwala S, Benzel E (2006) Surgical management of cervical myelopathy dealing with the cervical-thoracic junction. The spine journal : official journal of the North American Spine Society 6:268S–273S
Lee CH, Jahng TA, Hyun SJ, Kim KJ, Kim HJ (2016) Expansive laminoplasty versus laminectomy alone versus laminectomy and fusion for cervical ossification of the posterior longitudinal ligament: is there a difference in the clinical outcome and sagittal alignment? Clin Spine Surg 29:E9–E15
Lee CK, Shin DA, Yi S, Kim KN, Shin HC, Yoon DH, Ha Y (2016) Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine 24:100–107
Lee JJ, Shin DA, Yi S, Kim KN, Yoon DH, Shin HC, Ha Y (2018) Effect of posterior instrumented fusion on three-dimensional volumetric growth of cervical ossification of the posterior longitudinal ligament: a multiple regression analysis. The spine journal : official journal of the North American Spine Society 18:1779–1786
Lee SE, Chung CK, Jahng TA, Kim HJ (2013) Long-term outcome of laminectomy for cervical ossification of the posterior longitudinal ligament. J Neurosurg Spine 18:465–471
Lee SH, Son DW, Lee JS, Kim DH, Sung SK, Lee SW, Song GS (2018) Differences in cervical sagittal alignment changes in patients undergoing laminoplasty and anterior cervical discectomy and fusion. Neurospine 15:91–100
Lin S, Zhou F, Sun Y, Chen Z, Zhang F, Pan S (2015) The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J 24:127–135
Liu X, Chen Y, Yang H, Li T, Xu B, Chen D (2017) Expansive open-door laminoplasty versus laminectomy and instrumented fusion for cases with cervical ossification of the posterior longitudinal ligament and straight lordosis. Eur Spine J 26:1173–1180
Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S, Morita D, Kato F (2012) Cervical alignment and range of motion after laminoplasty: radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature. Spine (Phila Pa 1976) 37:E1243–E1250
Manzano GR, Casella G, Wang MY, Vanni S, Levi AD (2012) A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery 70:264–277
Matsumoto M, Chiba K, Toyama Y, Takeshita K, Seichi A, Nakamura K, Arimizu J, Fujibayashi S, Hirabayashi S, Hirano T, Iwasaki M, Kaneoka K, Kawaguchi Y, Ijiri K, Maeda T, Matsuyama Y, Mikami Y, Murakami H, Nagashima H, Nagata K, Nakahara S, Nohara Y, Oka S, Sakamoto K, Saruhashi Y, Sasao Y, Shimizu K, Taguchi T, Takahashi M, Tanaka Y, Tani T, Tokuhashi Y, Uchida K, Yamamoto K, Yamazaki M, Yokoyama T, Yoshida M, Nishiwaki Y (2008) Surgical results and related factors for ossification of posterior longitudinal ligament of the thoracic spine: a multi-institutional retrospective study. Spine (Phila Pa 1976) 33:1034–1041
Matsunaga S, Sakou T, Nakanisi K (1999) Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord 37:20–24
Miyashita T, Ataka H, Tanno T (2013) Spontaneous reduction of a floated ossification of the ligamentum flavum after posterior thoracic decompression (floating method); report of a case (abridged translation of a primary publication). Spine J 13:e7–e9
Moon BJ, Kim D, Shin DA, Yi S, Kim KN, Yoon DH, Ha Y (2019) Patterns of short-term and long-term surgical outcomes and prognostic factors for cervical ossification of the posterior longitudinal ligament between anterior cervical corpectomy and fusion and posterior laminoplasty. Neurosurg Rev. https://doi.org/10.1007/s10143-018-01069-x
Nolan JP Jr, Sherk HH (1988) Biomechanical evaluation of the extensor musculature of the cervical spine. Spine (Phila Pa 1976) 13:9–11
Ota M, Furuya T, Maki S, Inada T, Kamiya K, Ijima Y, Saito J, Takahashi K, Yamazaki M, Aramomi M, Mannoji C, Koda M (2016) Addition of instrumented fusion after posterior decompression surgery suppresses thickening of ossification of the posterior longitudinal ligament of the cervical spine. J Clin Neurosci 34:162–165
Roguski M, Benzel EC, Curran JN, Magge SN, Bisson EF, Krishnaney AA, Steinmetz MP, Butler WE, Heary RF, Ghogawala Z (2014) Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 39:2070–2077
Sakai K, Yoshii T, Hirai T, Arai Y, Shinomiya K, Okawa A (2017) Impact of the surgical treatment for degenerative cervical myelopathy on the preoperative cervical sagittal balance: a review of prospective comparative cohort between anterior decompression with fusion and laminoplasty. Eur Spine J 26:104–112
Shou F, Li Z, Wang H, Yan C, Liu Q, Xiao C (2015) Prevalence of C5 nerve root palsy after cervical decompressive surgery: a meta-analysis. Eur Spine J 24:2724–2734
Stephens BF, Rhee JM, Neustein TM, Arceo R (2017) Laminoplasty does not lead to worsening axial neck pain in the properly selected patient with cervical myelopathy: a comparison with laminectomy and fusion. Spine (Phila Pa 1976) 42:1844–1850
Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, Lafage V, Shaffrey CI, Schwab F, Ames CP (2015) The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 76(Suppl 1):S14–S21 discussion S21
Wang M, Luo XJ, Deng QX, Li JH, Wang N (2016) Prevalence of axial symptoms after posterior cervical decompression: a meta-analysis. Eur Spine J 25:2302–2310
Wu JC, Chen YC, Huang WC (2018) Ossification of the posterior longitudinal ligament in cervical spine: prevalence, management, and prognosis. Neurospine 15:33–41
Yamazaki M, Mochizuki M, Ikeda Y, Sodeyama T, Okawa A, Koda M, Moriya H (2006) Clinical results of surgery for thoracic myelopathy caused by ossification of the posterior longitudinal ligament: operative indication of posterior decompression with instrumented fusion. Spine (Phila Pa 1976) 31:1452–1460
Zhang JT, Li JQ, Niu RJ, Liu Z, Tong T, Shen Y (2017) Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J 26:1205–1210
Acknowledgments
The authors wish to thank Hyun Kyung Park, PhD, for her contributions in drafting the manuscript and revising it for important intellectual content.
Funding
This work was supported by the 2018 Inje University research grant.
Author information
Authors and Affiliations
Contributions
JJS analyzed the data and drafted the manuscript. YH revised the manuscript critically for important intellectual content and approved the final version to be submitted. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
This study was approved by the local ethical committee and the institutional review board (SGPAIK 2018-05-014).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent from each patient is not required; instead, an ethical approval has been made by the regional ethics board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ha, Y., Shin, J.J. Comparison of clinical and radiological outcomes in cervical laminoplasty versus laminectomy with fusion in patients with ossification of the posterior longitudinal ligament. Neurosurg Rev 43, 1409–1421 (2020). https://doi.org/10.1007/s10143-019-01174-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01174-5