Abstract
Introduction
To analyze how K-line is related to change in sagittal cervical curvature and laminoplasty outcomes in patients with cervical ossification of the posterior longitudinal ligament (OPLL).
Materials and methods
The study retrospectively analyzed 81 patients with OPLL who had undergone posterior cervical single-door laminoplasty and arch plate fixation between June 2011 and June 2017. Fifty-five were K-line positive (K[+]) and 26 were K-line negative (K[−]). Clinical and radiological results were compared between the groups. Patients were followed up for at least 2 years.
Results
Before the operation, Japanese Orthopedic Association (JOA) score, visual analogue scale (VAS) score, neck disability index (NDI), and short-form-36 (SF-36) quality of life score did not differ significantly between the groups. Neurological function was improved in both groups after the procedure. At last follow-up, JOA score, VAS score, NDI, SF-36 score, and JOA score improvement rate differed significantly between the groups. Before the operation, at the 3-month and final follow-ups, C2–7 Cobb angle, T1 slope, and C2–7 SVA differed significantly between the groups. The changes were more marked in the K(−) group than in the K(+) group. The incidence of cervical kyphosis differed significantly between the groups (P < 0.05), as well as between patients with lordosis < 7° and those with lordosis ≥ 7°.
Conclusions
K-line negativity and lordosis < 7° may predict kyphosis after laminoplasty in patients with OPLL. The cervical curvature in patients with OPLL tends towards kyphosis and anteversion after laminoplasty, which contributes to the reduced clinical effect of the procedure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a progressive disease of the cervical spine [1] that is one of the main causes of cervical spondylosis [2, 3]. It is a multifactorial disease that may be related to genetics, diabetes, obesity, and other factors [4,5,6]. The incidence of OPLL among East Asians is relatively high. In Japan, Fujimori et al. [7] found that the incidence of the disease is 6.3%, while Nouri et al. found that 10% of patients with cervical spondylotic myelopathy had OPLL [8]. The surgical outcomes of OPLL are similar to those of other cervical spondylotic myelopathies, but the risk of perioperative complications is higher [9]. In this regard, Fujiyoshi et al. [10] proposed that the K-line is a predictor of the clinical effect of posterior cervical decompression in patients with OPLL. On a standard lateral X-ray of the cervical spine, the K-line is a straight line that joins the midpoints of the spinal canal at C2 and C7. Patients are said to be K-line positive when their OPLL does not extend beyond the K-line, while they are K-line negative when it does. Cervical curvature and spinal cord signal changes may also be important factors affecting OPLL prognosis [11, 12]. Kim et al. [13] suggested that the degree of loss of cervical lordosis after laminoplasty was related to T1 slope. However, it is unclear whether K-line is related to change in sagittal cervical curvature, or whether the change in cervical curvature is related to clinical effect.
The present retrospective analysis of medical records aimed to (1) analyze how K-line is related to change in sagittal cervical curvature and kyphosis after laminoplasty, (2) analyze the correlation between change in sagittal cervical curvature and clinical efficacy of laminoplasty in patients with OPLL, and (3) explore the predictive factors of kyphosis after laminoplasty in patients with OPLL.
Materials and methods
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) diagnosis of OPLL and involving 2 or more vertebrae; (2) progressive neurological damage requiring surgical intervention, (3) available computed tomography (CT) to identify the presence and type of OPLL before surgery, (4) magnetic resonance imaging (MRI) showing obvious compression of the spinal cord, and (5) main outcome measures that included improvement in nerve function and change in sagittal curvature.
The exclusion criteria were as follows: (1) history of cervical surgery, (2) severe internal diseases that contraindicated surgery, (3) cervical trauma, spinal cord injury, or tumor, (4) kyphosis before the operation, (5) mental illness that prevented treatment and follow-up.
General information
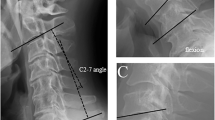
Between June 2011 and June 2017, 128 patients with OPLL underwent posterior cervical single-door laminoplasty and arch plate fixation at our hospital. Ninety-six were eligible to participate in the study according to the above inclusion and exclusion criteria; of these, 81 were included in the present study and finished the 2-year follow-up: 54 men and 27 women, with an average age of 58.012 ± 10.687 years (range 32–80 years), and with an average disease course of 15.617 ± 10.655 months (range 6–60 months). Based on the position of the OPLL in relation to the K-line (Fig. 1), the patients were divided into the K-line positive K(+) group (55 patients: 37 men, 18 women) and the K-line negative K(−) group (26 patients: 17 men, 9 women). There were no significant differences in the baseline data between the groups (P > 0.05; Table 1), indicating that the groups were comparable. The clinical research plan was approved by the medical ethics committee, and all the patients signed the informed consent document.
a Schematic diagram for the measurement of the sagittal curvature of the cervical spine. K-line (red), C2–7 Cobb angle (yellow), T1 slope (black) and C2–7 SVA (blue) were measured on the standard lateral X-ray film of the cervical spine; b Schematic diagram for the measurement of percentage of spinal canal occupation by ossified mass. The thickness of the ossification block (a, blue line) and the anteroposterior diameter of the spinal canal (b, yellow line) were measured on the axial CT section of the highest point of the ossification block. The percentage of spinal canal occupation by the ossification block = a/b × 100%
Operative method
The patients were placed in the prone position under general anesthesia. A standard posterior midline exposure was performed for all procedures, the supraspinous ligaments entirely preserved. We usually decided symptomatic or severely compressed side as the open side. A high-speed grinding drill or an ultrasonic bone knife was used to cut grooves along the junction of the lamina and facet articular process on both sides. The inner lamina was retained on the side of the door shaft, and the whole lamina was cut off on the side of the door opening. The lamina was elevated from the open side toward the hinge side stabilized with miniplates and screws. The hormone was administered when decompressing, and 0.5 g of methylprednisolone was added to 100 mL of normal saline for rapid intravenous drip. With their necks protected and supported by a neck bracket, the patients resumed active neck flexion and extension 2 weeks after the operation, and they started exercising the posterior neck muscles.
Outcome measures and measurement method
All patients were followed up for 24–72 months, with a mean follow-up period of 42.20 ± 14.75 months. All patients underwent X-ray, CT, and MRI before the operation and were reexamined 3 months after the operation. At the last follow-up appointment, routine X-ray, CT, or MRI was performed. Japanese Orthopedic Association (JOA) score, visual analogue scale (VAS), neck disability index (NDI), and short form-36 (SF-36) quality of life score were recorded before the operation, 3 months after the operation, and at the last follow-up. The improvement rate of JOA score was calculated ([postoperative JOA score − preoperative JOA score]/[17 − preoperative JOA score] × 100%) [14]. The C2–7 Cobb angle, T1 slope, C2–7 sagittal vertical axis (SVA), and spinal canal occupation rate of the ossified mass were measured. A C2–7 Cobb angle ≥ 0° was defined as lordosis, while a C2–7 Cobb angle < 0° was defined as kyphosis; on this basis, the incidence of postoperative kyphosis was evaluated. Changes in cervical curvature and complications were recorded. The following parameters were measured: (1) C2–7 Cobb angle, defined as the angle between two intersecting vertical lines parallel to the extension of the C2 and C7 lower endplates on the cervical lateral radiograph; (2) T1 slope, defined as the angle between the extension line of the end plate on T1 and the horizontal plane [15]; (3) C2–7 SVA, defined as the vertical distance between the C2 center and the upper rear corner of C7 [13]; (4) K-line measurements were performed on standing lateral X-ray of the cervical spine, the K-line is a straight line that joins the midpoints of the spinal canal at C2 and C7; (5) ratio of the occupation rate of the ossified block spinal canal, calculated as the ratio between the thickness of the ossification block and the diameter of the anterior and posterior spinal canal (Fig. 1). Two independent clinical research assistants, who were not involved with the study and blinded to all clinical information, performed radiological measurements. Radiological parameters were measured twice at 1-week intervals, and the average values of both observers were used in this study. In the study, we investigated the reliability of the measurement techniques and found good to excellent intra- and inter-observer agreement for each parameter.
Statistical analysis
SPSS 22.0 statistical software was used for all statistical analysis. Continuous data with normal distribution were compared using the t test. The Wilcoxon rank-sum test was used for data with non-normal distribution. Categorical data were compared using the chi-square test. However, when the sample size was < 40, Fisher’s exact test was used. A P value of < 0.05 was considered statistically significant.
Results
Improvement in nerve function
There were no significant differences in JOA score, VAS score, NDI, or SF-36 score between the groups before the operation (P > 0.05). Neurological function in both groups was significantly improved after the operation (P < 0.05). There were no significant differences in JOA score, VAS score, NDI, SF-36 score, or JOA improvement rate 3 months after the operation (P > 0.05). However, at the last follow-up, there were significant differences in JOA score, VAS score, NDI, SF-36 score, and JOA improvement rate (P < 0.05; Table 2). There was no significant difference in the incidence of complications between the groups (P > 0.05; Table 3).
Changes in cervical curvature
There were significant differences in C2–7 Cobb angle, T1 slope, and C2–7 SVA between the two groups before the operation (P < 0.05; Table 2). In the K(+) group, the C2–7 Cobb angle was larger, the T1 slope larger, the C2–7 SVA smaller, and the cervical lordosis larger than in the K(−) group.
The C2–7 Cobb angle decreased in both groups after surgery, and the change was greater in the K(−) group (P < 0.05). The T1 slope decreased in both groups, with the change being greater in the K(−) group (P < 0.05). C2–7 SVA increased in both groups; the change was greater in the K(−) group (P < 0.05; Table 2; Fig. 2).
A 46-year-old woman with OPLL and negative K-line. a Standard preoperative lateral X-ray film of the cervical spine showing that the highest point of ossification mass of the posterior longitudinal ligament is beyond the K-line and lordosis > 7°. b Preoperative sagittal CT showing that the range of ossification of the posterior longitudinal ligament is C2–C5. c Preoperative MRI showing obvious compression in front of the cervical spinal cord. d Lateral X-ray performed 3 months after surgery showing that the C2–C7 Cobb angle decreased, the T1 slope decreased, the C2–7SVA increased, and the cervical lordosis decreased. e Lateral X-ray performed 3 years after surgery showing good internal fixation position, reduction of cervical lordosis, but did not develop into kyphosis. f MRI performed 3 years after surgery showing that the anteroposterior diameter of the spinal canal increased significantly and that the spinal cord compression reduced significantly
The incidence of kyphosis was 3.64% (2/55) in the K(+) group and 30.77% (8/26) in the K(−) group, constituting a significant difference (P < 0.05). Among patients with lordosis ≥ 7°, there was no significant difference in the incidence of kyphosis between the two groups (P > 0.05). However, among patients with lordosis < 7°, the incidence of kyphosis was greater in the K(−) group (P < 0.05). Patients with lordosis < 7° had a significantly greater incidence of kyphosis than patients with lordosis ≥ 7° (P < 0.05; Table 3; Fig. 3).
A 51-year-old man with OPLL and negative K-line. a Standard preoperative lateral X-ray film of the cervical spine showing that the highest point of ossification mass of the posterior longitudinal ligament is beyond the K-line and lordosis < 7°. b Preoperative sagittal CT showing that the range of ossification of the posterior longitudinal ligament is C3–C5. c Preoperative MRI showing obvious compression in front of the cervical spinal cord. d Lateral X-ray performed 3 months after surgery showing that the C2–C7 Cobb angle decreased, the T1 slope decreased, the C2–7SVA increased, and the cervical lordosis decreased. e Lateral X-ray performed 2 years after surgery showing good internal fixation position, reduction of cervical lordosis, develop into kyphosis. f MRI performed 2 years after surgery showing that the anteroposterior diameter of the spinal canal increased significantly and that the spinal cord compression reduced significantly
Discussion
Correlation between K-line and change in sagittal cervical curvature
According to Ames [16] sagittal alignment of the cervical spine (C2–7 SVA and kyphosis) is related to T1 slope. Bronson et al. [17, 18] found that larger T1 slopes are associated with larger C2–C7 Cobb angle. Liu et al. [19] asserted that laminoplasty destroys the structure behind the spine, leading to cervical instability, or kyphosis. In the present study, the C2–7 Cobb angle decreased, the T1 slope decreased, and the C2–7 SVA increased in both groups. These outcomes may be related to the destruction of cervical muscles and ligaments after the operation, which accelerates the change in cervical curvature, leading to reduced cervical lordosis and increased cervical anteversion. To achieve sagittal balance, patients with cervical spondylosis must move the center of gravity of their cervical spine backward and decrease the T1 slope. This change in cervical curvature is more marked in patients with K-line negative OPLL.
Aita et al. [20] observed that, although the cervical spine of patients with OPLL showed lordosis before laminoplasty, this was decreased after surgery so that the cervical spine was straightened. According to Kim et al. [13], patients with larger T1 slope also had larger cervical lordosis, as well as larger loss of lordosis. However, the same authors found no obvious postoperative kyphosis. In the present study, we found that the preoperative T1 slope was larger in the K(+) group, while the C2–7 Cobb angle was larger, the C2–7 SVA smaller, and the cervical lordosis more marked. Furthermore, postoperative T1 slope, C2–7 Cobb angle, and C2–7 SVA were all changed in the K(+) group, but not markedly so; no remarkable loss of lordosis occurred, and few patients developed kyphosis. In the K(−) group, the T1 slope was smaller, the C2–7 Cobb angle smaller, the C2–7 SVA larger, and the cervical lordosis unremarkable. Moreover, T1 slope, C2–7 Cobb angle, C2–7 SVA, and anteversion showed marked changes; the loss of lordosis was remarkable, and kyphosis formed easily.
Studies by Machino et al. [21] have found that patients with cervical spondylotic myelopathy involving cervical lordosis of less than 7° are more likely to develop kyphosis after laminoplasty. In the present study, we found that patients in the K(−) group were more prone to kyphosis (8/26) than those in the K(+) group (2/55; P < 0.05). Moreover, patients with lordosis < 7° were more likely to have kyphosis than those with lordosis ≥ 7° (P < 0.05). Therefore, we believe that K-line negativity and lordosis < 7° could be used as predictors of kyphosis in patients with OPLL.
Correlation between change in sagittal curvature of the cervical spine and clinical effect after laminoplasty
In the present study, JOA score, VAS score, NDI, SF-36 score, and JOA improvement rate were significantly better in the K(+) group than in the K(−) group at the last follow-up (P < 0.05), perhaps because there was marked change in cervical curvature in the K-line (−) group and because posterior spinal cord movement was limited after decompression.
Similar to other studies, Sugrue [22] found that laminoplasty is suitable for patients with preoperative cervical lordosis and OPLL whose spinal canal occupation rate is less than 60%. In fact, Suk et al. [23] believed that lordosis is a prerequisite for laminoplasty, and that postoperative maintenance of cervical lordosis is important for postoperative efficacy. When cervical lordosis remains unchanged, the cervical spinal cord moves backwards after laminoplasty, allowing good decompression. Sakai et al. reasoned that the spinal cord could not be effectively displaced backward after laminoplasty in patients who have kyphosis before the operation, resulting in poor decompression [24]. Miyazaki et al. [25] believed that, although cervical curvature is related to T1 slope, clinical symptoms are significantly improved after laminoplasty regardless of preoperative T1 slope. Cho et al. [26] found that the balance of the sagittal position of the cervical spine was damaged after laminoplasty, but that this effect was not related to preoperative T1 slope. Moreover, one study showed that preoperative cervical lordosis is not related to clinical effect after laminoplasty [27]. Lee et al. [28] stated that the sagittal position of the cervical spine often showed kyphosis after laminoplasty, but that the relationship between the changes in sagittal curvature of the cervical spine and clinical results is still unclear. In contrast, we found that the change in sagittal curvature of cervical spine was connected to clinical results, especially in patients with K-line negative OPLL, who showed marked change in cervical spine curvature after the operation and poorer clinical effect at last follow-up than patients with K-line positive OPLL (P < 0.05). Yoshii et al. [29] found that the spinal cord could bear more compression during neck flexion when the OPLL occupancy rate of patients was higher, even though most patients showed increased spinal cord compression during neck extension. Ito et al. [30] showed that, in the kyphosis and K(−) groups, the spinal canal narrowed in the flexion position, and that cervical flexion may lead to greater compression of the spinal cord. Koda et al. [31] found that laminoplasty is not suitable for the treatment of patients with K-line negative OPLL. In the K(−) group of the present study, we found that cervical lordosis was smaller; after surgery, lordosis had decreased significantly, with some patients even developing kyphosis, and spinal cord compression increased, affecting postoperative outcomes.
We also found that, in patients with OPLL, the change in cervical curvature after laminoplasty tended towards kyphosis and anteversion, regardless of K-line state (positive or negative) and degree of cervical lordosis. However, patients with K-line positive OPLL tended to have larger cervical lordosis before the operation, which buffered the changes in cervical lordosis after the operation. Based on the bowstring effect, the clinical effect was better after surgery in these patients. Moreover, the change in curvature of the cervical spine was not remarkable after the operation, so it had little effect on postoperative outcome. However, in patients with K-line negative OPLL, preoperative cervical lordosis was often smaller, with less buffering effect on the development of postoperative cervical kyphosis; as such, the postoperative change in cervical curvature was more marked, with cervical kyphosis forming easily. For this reason, the cervical spinal curvature had a greater postoperative effect in these patients, leading to worse clinical outcomes. Therefore, we believe that the loss of cervical lordosis after laminoplasty, as well as the tendency towards kyphosis and anteversion, may decrease the curative effect of this procedure in patients with OPLL.
The present study had several limitations. For example, it was carried out in a single center and was retrospective. During the case selection, we only included patients who had received single-door laminoplasty arch titanium plate internal fixation. Moreover, patients with both OPLL and cervical kyphosis were not included in the study. Only a small number of patients were included, so selective bias may have occurred, leading to errors in the results. Finally, the follow-up time of the study was relatively short.
Conclusion
To sum up, neurological function was improved in both groups after the operation. The clinical effect in the K(+) group was better than that in the K(−) group at last follow-up. In the K(+) group, cervical curvature changed little, while in the K(−) group, it changed markedly and kyphosis occurred easily. In patients with OPLL involving lordosis < 7°, kyphosis occurs easily. Therefore, K-line negativity and lordosis < 7° could be used as predictors of kyphosis after laminoplasty in patients with OPLL. The cervical curvature in patients with OPLL tends towards kyphosis and anteversion, which is an important factor in the reduced clinical effect of laminoplasty. Because the present study was limited by its small sample size, future studies should be carried out that involve larger sample size, perform long-term follow-up, and analyze the prognosis of different surgical methods.
References
Tsuyama N (1984) Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res 184:71–84
Fargen KM, Cox JB, Hoh DJ (2012) Does ossification of the posterior longitudinal ligament progress afterlaminoplasty? Radiographic and clinical evidence of ossification of the posterior longitudinal ligament lesion growth and the risk factors for lateneurologic deterioration. J Neurosurg Spine 17(6):512–524
Matsunaga S, Nakamura K, Seichi A et al (2008) Radiographic predictors forthe development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine (Phila Pa 1976) 33(24):2648–2650
Ikeda Y, Nakajima A, Aiba A et al (2011) Association between serum leptin and bone metabolic markers, and the development of heterotopic ossification of the spinal ligament in femalepatients with ossification of the posterior longitudinal ligament. Eur Spine J 20(9):1450–1458
Matsunaga S, Sakou T (2012) Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976) 37(5):E309-314
Kobashi G, Washio M, Okamoto K et al (2004) High body mass index after age 20 and diabetes mellitus are independent risk factors for ossification of the posterior longitudinal ligament of the spine in Japanese subjects: a case–control study in multiple hospitals. Spine (Phila Pa 1976) 29(9):1006–1010
Fujimori T, Watabe T, Iwamoto Y et al (2016) Prevalence, concomitance, and distribution of ossification of the spinalligaments: results of whole spine CT scans in 1500 Japanese patients. Spine (Phila Pa 1976) 41(21):1668–1676
Nouri A, Martin AR, Tetreault L et al (2017) MRI analysis of the combined prospectively collected AOSpine North America and International Data: the prevalence and spectrum of pathologies in a global cohort of patients with degenerative cervical myelopathy. Spine (Phila Pa 1976) 42(14):1058–1067
Nakashima H, Tetreault L, Nagoshi N et al (2016) Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy: results from the prospective, multicenter AOSpine CSM-international study of 479 patients. J Bone Jt Surg Am 98(5):370–378
Fujiyoshi T, Yamazaki M, Kawabe J et al (2008) A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976) 33(26):E990-993
Maruo K, Moriyama T, Tachibana T et al (2014) The impact of dynamic factors on surgical outcomes after double-doorlaminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 21(6):938–943
Vedantam A, Jonathan A, Rajshekhar V (2011) Association of magnetic resonance imaging signal changes and outcome prediction after surgery for cervical spondylotic myelopathy. J Neurosurg Spine 15(6):660–666
Kim B, Yoon DH, Ha Y et al (2016) Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J 16(2):219–225
Matsuoka T, Yamaura I, Kurosa Y et al (2001) Long-term results of the anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 26(3):241–248
Kim TH, Lee SY, Kim YC et al (2013) T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 38(16):E992-997
Ames CP, Blondel B, Scheer JK et al (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 38:S149-160
Bronson WH, Moses MJ, Protopsaltis TS (2018) Correction of dropped head deformity through combined anterior and posterior osteotomies to restore horizontal gaze and improve sagittal alignment. Eur Spine J 27(8):1992–1999
Patwardhan AG, Khayatzadeh S, Havey RM et al (2018) Cervical sagittal balance: a biomechanical perspective can help clinicalpractice. Eur Spine J 27(Suppl 1):25–38
Liu X, Chen Y, Yang H et al (2017) Expansive open-door laminoplasty versus laminectomy and instrumentedfusion for cases with cervical ossification of the posterior longitudinal ligamentand straight lordosis. Eur Spine J 26(4):1173–1180
Aita I, Wadano Y, Yabuki T (2000) Curvature and range of motion of the cervical spine after laminaplasty. J Bone Jt Surg Am 82(12):1743–1748
Machino M, Ando K, Kobayashi K et al (2020) Postoperative kyphosis in cervical spondylotic myelopathy: cut-off preoperative angle for predicting the post-laminoplasty kyphosis. Spine (Phila Pa 1976) 45(10):641–648
Sugrue PA, McClendon J Jr, Halpin RJ et al (2011) Surgical management of cervical ossification ofthe posterior longitudinalligament: natural history and the role of surgical decompression and stabilization. Neurosurg Focus 30(3):E3
Suk KS, Kim KT, Lee JH et al (2007) Sagittal alignment of the cervical spine after the laminoplasty. Spine (Phila Pa 1976) 32(23):E656-660
Sakai K, Okawa A, Takahashi M et al (2012) Five-year follow-up evaluation of surgical treatment for cervical myelopathycaused by ossification of the posteriorlongitudinalligament: a prospectivecomparative study of anterior decompression and fusion with floating methodversus laminoplasty. Spine (Phila Pa 1976) 37(5):367–376
Miyazaki M, Ishihara T, Notani N et al (2018) Relationship of T1 slope with loss of lordosis and surgical outcomes after laminoplasty for cervical ossification of the posterior longitudinal ligament. Clin Neurol Neurosurg 164:19–24
Cho JH, Ha JK, Kim DG et al (2014) Does preoperative T1 slope affect radiological and functional outcomes aftercervical laminoplasty? Spine (Phila Pa 1976) 39(26):E1575-1581
Kim SW, Hai DM, Sundaram S et al (2013) Is cervical lordosis relevant in laminoplasty? Spine J 13(8):914–921
Lee CK, Shin DA, Yi S et al (2016) Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine 24(1):100–107
Yoshii T, Yamada T, Hirai T et al (2014) Dynamic changes in spinal cord compression by cervical ossification of the posterior longitudinal ligament evaluated by kinematic computed tomographymyelography. Spine (Phila Pa 1976) 39(2):113–119
Ito K, Yukawa Y, Ito K et al (2015) Dynamic changes in the spinal cord cross-sectional area in patients with myelopathy due to cervical ossification of posterior longitudinal ligament. Spine J 15(3):461–466
Koda M, Mochizuki M, Konishi H et al (2016) Comparison of clinical outcomes between laminoplasty, posterior decompression with instrumented fusion, and anterior decompression with fusion for K-line (−) cervical ossification of the posterior longitudinal ligament. Eur Spine J 25(7):2294–2301
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, C., Zha, G., Yang, Z. et al. K-line in patients with cervical ossification of the posterior longitudinal ligament: relationship with change in sagittal cervical curvature and laminoplasty outcomes. Arch Orthop Trauma Surg 142, 1743–1751 (2022). https://doi.org/10.1007/s00402-020-03741-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03741-8