Abstract
We report our experience in implementing CT multiplanar reformats (MPRs) to demonstrate the trajectory of penetrating trauma. It is an easily learned tool that can be conveniently and speedily applied in the fragments injury. We describe the detailed technique of performing MPRs, depicted by various examples. Furthermore, benefits and limitations of the technique (such as numerous fragments, change in position and respiratory phase, and embolization of fragments) are presented. We conclude that MPRs in the fragments trajectory can be helpful for accurate and fast diagnosis of injury. In addition, MPRs serve as a vivid presentation of injured and spared organs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multidetector CT (MDCT) has been reported to be of the high value in diagnosis of an injury caused by penetrating trauma [1, 2] including terror bombings [3]. Increasingly more CT studies are now performed with 16 or more detectors scanners in the isotropic or nearly isotropic acquisition mode that allows performance of multiplanar reformats (MPRs). MPRs have been shown to be very useful in variety of diagnostic challenges, such as diagnosis of urinary stones [4], small bowel obstruction [5], acute appendicitis [6], and staging of rectal cancer [7]. In trauma settings, MPRs are reported to be used for diagnosing acute vertebral fractures [8], right hemidiaphragmatic rupture [9], and in the forensic investigation of penetrating projectile [10, 11] and non-projectile [12] injury.
Here, we report our experience in implementing CT MPRs to demonstrate the trajectory of penetrating trauma. We show how this technique helps in understanding the trauma mechanism, leading to a more focused evaluation of structures in the presumed proximity of the trauma trajectory.
Shrapnel or penetrating fragment injury
The word shrapnel is derived from the name of Major-General Henry Shrapnel (1761–1842), an English artillery officer, who developed a new type of artillery shell. The term originally referred only to the spherical shot or musket balls dispersed when a shrapnel shell bursts, and this is still the strict technical definition of the term. However, “shrapnel” is now commonly used to describe all types of high-velocity fragments thrown out from an explosion and does not differentiate among the processes that create them.
The shrapnel or penetrating fragment injury (technically the correct term) is a subset of a blast injury. It may be both high and low energy injury—depending on the shape, size, weight of the fragment, and distance from the explosion. The initial velocity of the fragment is up to 1,800 m/s, but it decreases rapidly due to irregular shape and lack streamlining [13].
Propagation of a fragment traveling in the body depends on the tissue resistance. Most of the fragments travel in relatively straight fashion, rarely deflecting significantly, unless they meet a bony surface [14]. As an entry and exit wound (or alternatively a retained fragment in the body) can be usually identified, MPR along the fragment trajectory can be performed.
During second Israel Lebanon war, most of the civilian injuries and large part of military casualties were caused by explosives (locally called “Katyusha” [1]) that contained numerous small lead balls (Fig. 1). As our hospital cared for most casualties during the war, we acquired a significant experience with the fragment trauma. We found that performance of MPRs in the trajectory of penetrating trauma allowed fast and accurate delineation of injured organs, in addition to vivid presentation of fragment trajectory to the treating physician.
Case series—patients and methods
This study was approved by Institutional Ethics Review Committee with a waiver of informed consent.
The cases were gathered during the days of second Israel–Lebanon war in July–August of 2006. Our hospital received both civilian and military casualties. Five hundred eleven injured patients were treated at our hospital. Of the 404 patients who underwent radiological investigation as part of their trauma workup, 173 (43%) underwent total body CT that included head, cervical spine, chest, and abdomen CT.
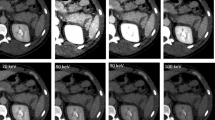
CT studies were performed on a Brilliance 16-MDCT scanner (Philips Medical Systems, Best, The Netherlands), with intravenous injection of 120 ml nonionic iodinated contrast material [Iomeron (iomeprol), 300 mg I/ml, Bracco] at a rate of 3–4 ml/s using a power injector. The CT scan was acquired with detector collimation of 16 × 0.75 mm and slice thickness reconstruction of 3 mm with 1.5 cm overlap. CT angiography studies were done to rule out arterial injury with detector collimation of 16 × 0.75 mm and slice thickness reconstruction of 2 mm with 1 cm overlap. No oral contrast was administered.
The MPRs were performed by the board-certified radiologist and the resident in the last year of training according to flow chart (Fig. 2). The MPR injury depiction value was graded 1–5 (Table 1), 1 adding no value and 5 contributing excellent value, in two profiles—diagnostic and demonstrative. For the diagnostic grading, 1 meant no additive diagnostic value of MPR due to superficial injury, or when injury occurred in axial plane, blast injury, and numerous fragments. Grade 3 was given when injury tract was in two planes and was reasonably well depicted at axial planes, but there was some additive diagnostic value of MPR images. Grade 5 was given when the injury occurred in three planes, was a deep injury, and included numerous organs. For the demonstrative profile, grade 1 was given when no additive presentation value was acquired from MPR images; grade 3 showed the mechanism of injury, but may be not inclusive of all damage; grade 4 was given when MPR shows well the mechanism of injury, but may be difficult to understand due to unfamiliar imaging plane; and grade 5 represented “one image demonstrate all injury” with clear depiction of the mechanism of injury.
Case series—results
Twenty-seven patients had penetrating torso trauma out of 173 patients that underwent total body CT (Table 2). These cases were identified through the review of CT reports of all trauma patients scanned during the time period of the war. In ten cases (37%), a single fragment was identified, and in 17 (63%) cases, multiple fragments were seen. In ten cases (37%), MPRs along the injury trajectory were found to add information about the mechanism of injury, its exact trajectory, and injured or spared organs, and in six cases (22%), MPRs were found to provide the treating physician a vivid and intuitive demonstration of the injury. The cases in which MPRs were found to be less contributive included cases with superficial injury, mostly muscle and subcutaneous tissue injury, multiple fragments, and injury occurring in the axial plane. Some of the cases are presented in Figs. 3, 4, 5, 6, 7, 8, and 9).
A 23-year-old soldier (patient 26 of the study list) wounded during active duty. Axial CT slice (a) shows piece of shrapnel at right lateral chest wall. There are no clues as to where the shrapnel came from. MPR image (b) shows that the same piece caused fracture of the scapula body, thus pointing to a point of entry that is posterior and lateral, far from the big vessels and other vital structures
A 20-year-old soldier (patient 9 of the study list) with extensive injury to his right chest. Axial CT image (a) shows extensive lung contusion, minimal pneumothorax with chest tube in pleural cavity, numerous fractured ribs, and large subcutaneous emphysema with small bits of shrapnel both in the chest wall and possibly in the lung. The imaging findings are consistent with both blast and penetrating injuries. Such devastating penetrating injury would have caused serious injury at the point of entry. An MPR image (b) easily identifies the point of entry and extent of injury. Another MPR image (c), slightly off the trajectory site, identifies the subclavian artery, which was uninjured, even though it is surrounded by numerous bits of shrapnel
A 36-year-old injured soldier (patient 19 of the study list). Axial CT slice (a) shows large piece of shrapnel medial and posterior to right kidney. An MPR image (b) shows the shrapnel trajectory through subcutaneous tissues of the right lateral chest wall, costophrenic angle of right lung, liver, and upper pole of right kidney. Note the unaligned trajectory lines for liver and kidney due to the different respiratory phases during injury and CT scanning
A 45-year-old civilian (patient 25 of the study list) injured by a falling rocket while driving his car. Scout view shows a small piece of shrapnel medial to spine in right upper abdomen (a). Axial CT image (b) shows an irregular bit of shrapnel just lateral to the aorta. An MPR image (c) shows the exact details of the trajectory: subcutaneous tissues of the right lateral chest wall, possibly right costophrenic sinus, liver, right adrenal, and right diaphragmatic crus
This 40-year-old civilian (patient 24 of the study list) was wounded by rockets at his workplace. The patient suffered multiple shrapnel injuries, mostly in his left chest. In addition, another piece of shrapnel was located at the right lung apex (a). It was vastly important to identify the origin of this shrapnel in order to rule out its passage through the mediastinum and possible injury to great vessels. An MPR image (b) shows that the shrapnel came through the posterior lower neck and caused some hematoma and subcutaneous emphysema, rib fracture, and lung contusion
A 24-year-old soldier (patient 17 of the study list) with severe multiple injuries. A large piece of shrapnel was identified in the left part of the pelvis with retroperitoneal air and a little fluid (a). A subcutaneous hematoma was surprisingly seen in the right buttock (arrow). A MPR (e) from three oblique planes (b–d) was performed to show the shrapnel trajectory, indicating the origin of the retroperitoneal air—rectum injury. Another severe injury in this case was an internal iliac AV fistula, which was not apparent at the presentation, even though the MPR images do suggest this possibility in retrospect
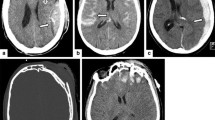
A 45-year-old civilian (patient 8 of the study list) injured by a rocket during the first days of the war. Shrapnel is seen in the left lower lobe of lung (a). Traumatic pneumatoceles (b) along the course of the shrapnel could be followed up to the lung apex, where the first rib fracture was identified (c). Delineating the shrapnel trajectory in this case could be tricky and lengthy, whereas MPR (d) clearly shows the point of entry and the end point of the shrapnel. The entire trajectory does not lie exactly on the same line due to differences in breathing and postural position between time of injury and CT scanning. An additional MPR (e), therefore, completes the picture
Technique—an isotropic dataset
As prerequisite for diagnostically acceptable MPRs, a CT study should be acquired in an isotropic manner, meaning that an image voxel has equal and sufficiently small width, height, and depth [15–17], thus producing MPR images without artifacts. In our hospital, at the time of the second Israel–Lebanon war, we had a 16-slice CT. Trauma studies were acquired with the above-described technique, which produced voxel size of 1.5 × 0.78 × 0.78 mm for regular trauma studies and voxel size of 1 × 0.78 × 0.78 mm for CT angiography studies. Even though both datasets are not fully isotropic, we have found that it was possible to produce diagnostic MPRs with minimal artifact. With the widely available 64-slice CT machines, acquiring isotropic data is a routine, thus allowing better performance with MPR.
Technique—identification of entry point
A thorough search should be undertaken to identify all entry points, which are usually smaller than the exit wound [10]. When a fragment passes through the bone, identifying the direction of injury is easier as it will cause beveling in the direction of travel (Fig. 7b), meaning that the entry site is sharp edged, while the exit side shows large inward-sloped bevel [18]. It is important to use a wide window level (soft tissue or lung window) to identify interruptions of the skin and soft tissues (Fig. 4b), findings that may point to the entry site. In many cases, the entry area will be obvious due to the significant disturbance of the tissue, but the exact entry point needed to perform accurate reconstructions of the shrapnel trajectory will be difficult to locate.
It has been shown previously that fragmentation of high velocity bullets creates a “snowstorm” appearance on the radiograph (Fig. 4b), meaning that the area over which fragments are deposited widens as the distance from the entry site increases [19–21]. This pattern produces conical distribution of lead fragments with the cone apex pointing toward the entry site. This sign, which was first described on the conventional X-rays, can be used with CT, especially on MPR images to identify the entry point.
Technique—identifying exit wound or fragment in the body
When a fragment has low velocity or meets high resistance, it will stop in the body at some point of its trajectory. It is easily identified—with a high-density structure, usually with streak artifact due to its lead content and irregular when it consists of shrapnel (Fig. 5b) or regular when it comes from lead balls of the Katyusha’s payload (Fig. 6a). For the fast search of a retained fragment, a CT topogram (Fig. 6a) or plain radiograph can be used. It is particularly useful when there is only one fragment involved. However, when a number of fragments had inflicted the injury, a thorough search for multiple exit wounds should be done with a technique identical to the search of entry wound—using wide windows to detect interruption of the skin and attenuation changes in the soft tissues.
When no fragment is identified throughout the body, a search for exit wound should be performed. The exit wound is usually larger than the entry wound and show everted edges [22]. The typical outward beveling of the bone can be seen at the skull wounds [23]. Similar findings can be seen at times in the soft tissues. Furthermore, when there is a shower of fragments in the same direction, one can assume a common path to all of them, and then there is no need to track each separately.
Technique—fragment trajectory
The next step is to perform MPRs along the presumed course of the projectile using an imaginary line connecting the two previously identified points: entry and exit wounds. When the trajectory of injury is identified, every structure in the presumed field of injury should be scrutinized for signs of the injury: slight irregularity in the vessel wall, signs of active bleeding, lacerations of solid organs, etc.
In many cases, the trajectory will not constitute a straight line between these two points due to various reasons explained further. Clues to the accurate fragment trajectory come from alteration in the tissue attenuation due to local hemorrhage, gas, and fragments that are left along the track with their concentration highest along the axis of the injury.
Limitations
Change in body position
Patient may not be in the same position when injured and imaged. Body CT is performed with the patient in supine position with arms elevated—unnatural position for civilians in their daily activities or running from explosion or for soldiers during active fighting. This may result in a false curved or truncated appearance of the fragment trajectory at the CT.
Change in inspiratory phase
Patient can be in different inspiratory phase when injured and imaged. Body, especially chest imaging, aspired to be performed in the end of inspiration [24]. Not every patient will cooperate: Unconscious patient or patient in pain will not be able to control respiration as needed. Therefore, it is hard to predict the respiratory phase of the trauma patient during imaging. Similarly, the patient can be at any respiratory phase when injured. Therefore, it is impossible to image the patient at the same respiratory phase. This will cause truncations and false alterations of the fragment trajectory (Fig. 5b). This effect is most accentuated in the organs that move extensively during respiration—chest and upper abdomen.
Change of fragment direction
The course of a fragment within the tissues may be irregular due to tumbling effect or ricochet [25]. In the cases presented herein, these effects were negligible: The lead balls that filled Katyusha’s missile were round and regular and thus had relatively straight trajectory. Nevertheless, these effects can be more pronounced in the fragments injury.
Small and numerous fragments may ricochet one from another, inducing additional injury in the tract itself. Some of them will be deflected from the original trajectory direction.
Another cause of the change in the fragment direction is ricochet from the bony surface in the body. All these changes in injury trajectory can be identified and followed through alterations in the tissue attenuation, keeping in mind the above-mentioned mechanisms of the ricochet.
Embolization of fragment
There are a number of reports about embolization of fragments through a vascular structure [26, 27]. The prerequisite for such situation is a small fragment that acquires an anatomical access to the vein or artery. The fragment will be found at the some distal point of the vessel, after a movement along the direction of the vessel. If a vein is involved, then the fragment may be found in the heart chambers or even in pulmonary arteries. If an artery is involved, then the fragment can be found in the peripheral artery. We have not encountered such case in the current case series, but this rare entity should be kept in mind when injury tract cannot be aligned with the fragment.
Multiple fragments
The biggest challenge constitutes cases with multiple fragments. It can be very hard and virtually impossible to recognize the entry point and direction of each and every fragment. Intersecting and comingling paths were found to be a major limitation for the recognition of the gunshot wound direction in the virtual autopsy series [11]. Still, the general direction of the injury can usually be outlined, in a similar way as for lone fragment.
Benefits
For radiologist
Trauma CT reading can be very time consuming as well as challenging and complicated. Usually, rapid reading is needed as critically injured patients should be treated and in the scenario of multiple casualties. Understanding the exact mechanism of injury is a prerequisite for timely and accurate diagnosis of the traumatic injury. MPR is an easily learned tool that can be conveniently and speedily applied in the fragment injury.
This technique has been used increasingly lately, as it becomes widely available and easy and fast to use. It should be noted, however, that the radiologist performing MPRs for injury trajectory should not neglect regular reading of the entire CT dataset, scrutinizing all organs for injury.
For clinician
MPR serves as an immediate and intuitive explanation of the injury to the treating physician, both depicting injured organs and mechanism of the injury. MPRs provide three-dimensional depiction of the injury, similar to the operating field, making the planning of surgery more efficient. In addition, given the time constraints of managing trauma patients, everything that helps to provide prompt diagnosis and thus prompt treatment is of high value.
For patient
The most important end point is that MPR helps to direct the surgeon to operate when needed and to avoid deep surgical exploration when not needed.
Conclusion
Protocol of MPR performance is presented herein. MPRs in the fragment trajectory can be helpful for accurate and fast diagnosis of injury. In addition, MPRs serve as vivid presentation of injured and spared organs to the treating physician.
References
Múnera F, Morales C, Soto JA et al (2004) Gunshot wounds of abdomen: evaluation of stable patients with triple-contrast helical CT. Radiology 231:399–405
Salim A, Sangthong B, Martin M et al (2006) Use of computed tomography in anterior abdominal stab wounds: results of a prospective study. Arch Surg 141:745–750
Benjaminov O, Sklair-Levy M, Rivkind A, Cohen M, Bar-Tal G, Stein M (2006) Role of radiology in evaluation of terror attack victims. Am J Roentgenol 187:609–616
Lin WC, Uppot RN, Li CS, Hahn PF, Sahani DV (2007) Value of automated coronal reformations from 64-section multidetector row computerized tomography in the diagnosis of urinary stone disease. J Urol 178:907–911
Filippone A, Cianci R, Grassedonio E, Di Fabio F, Storto ML (2007) Four-section multidetector computed tomographic imaging of bowel obstruction: usefulness of axial and coronal plane combined reading. J Comput Assist Tomogr 31:499–507
Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC (2005) Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology 235:879–885
Sinha R, Verma R, Rajesh A, Richards CJ (2006) Diagnostic value of multidetector row CT in rectal cancer staging: comparison of multiplanar and axial images with histopathology. Clin Radiol 61:924–931
Begemann PGC, Kemper J, Gatzka C, Stork A, Nolte-Ernsting C, Adam G (2004) Value of multiplanar reformations (MPR) in multidetector CT (MDCT) of acute vertebral fractures. J Comput Assist Tomogr 28:572–580
Rees O, Mirvis SE, Shanmuganathan K (2005) Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clin Radiol 60:1280–1289
Harcke HT, Levy AD, Getz JM, Robinson SR (2008) MDCT analysis of projectile injury in forensic investigation. Am J Roentgenol 190:W106–W111
Levy AD, Abbott RM, Mallak CT et al (2006) Virtual autopsy: preliminary experience in high-velocity gunshot wound victims. Radiology 240:522–528
Thali MJ, Schwab CM, Tairi K, Dirnhofer R, Vock P (2002) Forensic radiology with cross-section modalities: spiral CT evaluation of a knife wound to the aorta. J Forensic Sci 47:1041–1045
Covey DC (2002) Blast and fragment injuries of the musculoskeletal system. J Bone Joint Surg Am 84-A(7):1221–1234
Hollerman JJ, Fackler ML, Coldwell DM, Ben-Menachem Y (1990) Gunshot wounds: 1. Bullets, ballistics, and mechanisms of injury. Am J Roentgenol 155:685–690
Kalender WA (1995) Thin-section three-dimensional spiral CT: is isotropic imaging possible? Radiology 197:578–580
Mahesh M (2002) Search for isotropic resolution in CT from conventional through multiple-row detector. Radiographics 22:949–962
Parrish FJ (2007) Volume CT: state-of-the-art reporting. Am J Roentgenol 189:528–534
Klepinger LL (2006) Fundamentals of forensic anthropology. Wiley, Hoboken, pp 110
Molina DK, Wood LE, DiMaio VJ (2007) Shotgun wounds: a review of range and location as pertaining to manner of death. Am J Forensic Med Pathol 28:99–102
Wilson AJ (1999) Gunshot injuries: what does a radiologist need to know? Radiographics 19:1358–1368
Phillips CD (1992) Emergent radiologic evaluation of the gunshot wound victim. Radiol Clin North Am 30:307–324
Guharaj PV (2003) Forensic medicine. Orient Blackswan, Andhra Pradesh, pp 123
Smith OC, Berryman HE, Lahren CH (1987) Cranial fracture patterns and estimate of direction from low velocity gunshot wounds. J Forensic Sci 32:1416–1421
Bankier AA, O’Donnell CR, Boiselle PM (2008) Quality initiatives. Respiratory instructions for CT examinations of the lungs: a hands-on guide. Radiographics 28:919–931
Haag LC (2007) Wound production by ricocheted and destabilized bullets. Am J Forensic Med Pathol 28:4–12
Patel KR, Cortes LE, Semel L, Sharma PV, Clauss RH (1989) Bullet embolism. J Cardiovasc Surg (Torino) 30:584–590
Chen JJ, Mirvis SE, Shanmuganathan K (2007) MDCT diagnosis and endovascular management of bullet embolization to the heart. Emerg Radiol 14:127–130
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brook, O.R., Eran, A. & Engel, A. CT multiplanar reconstructions (MPR) for shrapnel injury trajectory. Emerg Radiol 19, 43–51 (2012). https://doi.org/10.1007/s10140-011-0988-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-011-0988-x