Abstract
Phototherapy has demonstrated positive effects in the treatment of peripheral nerve injury, but there is a need to investigate the dosimetric parameters. Thus, the aim of the present study was to conduct a literature review on the effects of photobiomodulation with the use of low-level laser therapy (LLLT) on the treatment of peripheral nerve injury in experimental models. The databases of PubMed/MEDLINE, SCOPUS, and SPIE Digital Library were searched for articles on the use of LLLT in experimental models of peripheral nerve injury published in English between January 2007 and March 2016. The laser parameter variability was wavelength (632.8 to 980 nm), power (10 to 190 mW), and total energy (0.15 to 90 J) in pulsed or continuous wave and single or multiple points. Eighteen original articles demonstrating the effects of LLLT on the acceleration of functional recovery, morphological aspects as well as the modulation of the expression inflammatory cytokines, and growth factors were selected. LLLT is a viable phototherapeutic modality for the treatment of peripheral nerve injury, demonstrating positive effects on the neuromuscular repair process using either red or infrared light. The majority of studies used a power of up to 50 mW and total energy of up to 15 J administered to multiple points. The determination of these parameters is important to the standardization of a LLLT protocol to enhance the regeneration process following a peripheral nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral nerve injury (PNI) is more common than a spinal cord injury. While PNI does not pose a fatal risk, it can exert a negative impact on quality of life due to the possibility of the non-occurrence of complete regeneration, resulting in a motor disorder (paralysis) or sensory disorder (anesthesia, paresthesia, and painful neuropathy). Thus, there is considerable interest in the investigation of the most adequate form of treatment, since nerve fibers have regenerative potential [1,2,3,4,5].
After a PNI, the repair process is initiated, involving neuronal growth, reinnervation, and functional recovery. PNI is classified into three types: neuropraxia, in which no structural changes occur and there is minimal sensory or motor loss resulting from mild pressure; axonotmesis, in which Wallerian degeneration of the axon occurs distally, with no loss of Schwann cells and the maintenance of connective tissue; and neurotmesis, the complete sectioning of the nerve, which can lead to tissue fibrosis due to proximal and distal degeneration [6].
Different models of PNI are used in experimental studies, such as crushing [7], nerve compression [8, 9], laceration, and complete cross-sectioning [10, 11]. The standardization of such injuries constitutes the greatest challenge. In studies involving axonotmesis or neuropraxia, the acquisition of a standardized injury is less likely in comparison to neurotmesis, since there is no assurance of an injury with the same amount of fibers in all experiments [12, 13]. With neurotmesis, the continuity of the nerve is interrupted and the muscles innervated by the fiber in question undergo progressive deterioration due to denervation [14], followed by the insufficient replacement of the lost tissue [11]. This regenerative incapacity demonstrates the need for adequate therapy to optimize and accelerate the nerve repair process.
Low-level laser therapy (LLLT) has recently been highlighted in the literature due to its photobiomodulating effect, which can cause either the inhibition or stimulation of tissue metabolism. The mechanism of action is believed to consist of the absorption of light (photons) by photoreceptors, altering the synthesis of ATP in mitochondria through the acceleration of the electron transport chains, thereby modulating cell reactions [15, 16]. Thus, LLLT can enhance postinjury functionality [17], increase the axonal diameter [18, 19], increase the thickness of the myelin sheath [19], diminish mononuclear inflammatory infiltrate [20], increase the number of Schwann cells [21], increase neurotrophic growth factors [22], and promote the remodeling of the extracellular matrix [23].
However, there is no standardization in treatment with LLLT and different irradiation parameters have been used in different models of PNI, resulting in a diversity of photobiomodulating effects. Thus, the aim of the present study was to perform a review of the literature on the applicability of LLLT as the treatment in experimental models of peripheral nerve injury. The null hypothesis of the study was if there is no relation between the laser parameters and the effects of photobiomodulation in different models of PNI.
Methods
The databases of PubMed/MEDLINE (Medical Literature Analysis and Retrieval System Online), SCOPUS, and SPIE Digital Library were searched for original articles involving experimental models of PNI treated with LLLT published in English between January 2007 and March 2016. The search strategy involved the use of the following terms: “lasers,” “laser therapy,” “low-level laser therapy,” “low intensity laser therapy,” “irradiation,” “phototherapy,” “photobiomodulation”; “repair,” “regeneration,” “injury,” and “peripheral nerve.” The bibliographic references of the articles were also analyzed for the identification of additional studies (Fig. 1).
Articles were selected based on the pre-established eligibility criteria. The following were the inclusion criteria:
-
1.
Articles published between January 2007 and March 2016;
-
2.
Experimental studies with animal models of peripheral nerve injury;
-
3.
Adequate description of the dosimetric parameters (wavelength, mean output power, beam area, power density, energy density, energy per point, total energy, number of points irradiated, and radiance time per point) or sufficient information to calculate these parameters
The following were the exclusion criteria:
-
1.
Clinical trials and in vitro studies;
-
2.
Review articles;
-
3.
Absence of an untreated injury group;
-
4.
Injury models of cranial nerves;
-
5.
Radiance not performed in contact, not enabling the description of real parameters
Results
One hundred seventy-nine potentially relevant articles were identified. After the analysis of the abstracts, 139 were excluded for the following reasons: injury models involving cranial nerves (n = 13), in vitro studies (n = 4), studies involving radiotherapy (n = 2), clinical trials (n = 2), systematic reviews (n = 7), radiance performed on prosthesis (n = 1), LED radiance (n = 4), use of high-power laser (n = 8), inadequate description of parameters (n = 6), radiance not transcutaneous (n = 1), and studies duplicated in different databases (n = 113).
Eighteen articles were included in the present review for the analysis of the effects of LLLT on PNI. The vast majority of studies used the continuous application mode (n = 17). Eight studies (44.4%) used the red spectrum, five (27.8%) used the infrared spectrum, and four (22.2%) used both spectra. Only one study (5.55%) employed the pulsed mode, with the wavelength in the infrared spectrum.
Different experimental models of PNI were used: crushing (n = 9; 50%), cross-sectioning followed by neurorrhaphy or anastomosis (n = 4; 22.2%), chronic constriction (n = 3; 16.7%), and cross-sectioning followed by tubulization (n = 2; 11.1%). The sciatic nerve was used in the majority of cases (n = 16; 88.9%), the fibular nerve was used in one study (5.55%), and the ganglion of the dorsal root (L4–L5) was used in one study (5.55%). Wistar rats were used in the majority of the experimental models (n = 12; 66.7%), followed by Sprague-Dawley rats (n = 5; 27.8%) and New Zealand rabbits (n = 1; 5.55%).
Table 1 displays the details of the studies involving LLLT in the red spectrum using the continuous mode. Table 2 displays the details of the studies involving LLLT in the infrared spectrum using the continuous mode. Table 3 displays the details of the study involving LLLT in the infrared spectrum using the pulsed mode. Table 4 displays the details of the studies that compared the two laser spectra (red and infrared) using the continuous mode.
Discussion
Annually in the USA and Europe, approximately 100,000 individuals are submitted to operations for peripheral nerve recovery due to technological advances in the field of microsurgery. However, the lack of satisfactory functional recovery underscores the need for greater investigation into the repair process of this tissue [3].
Different surgeries are used for PNI, such as neurorrhaphy [24], grafting [25], and tubulization [11]. Moreover, LLLT [24], electrotherapy, and therapeutic ultrasound constitute physical stimuli aimed at modulating the reinnervation process [1]. Biological therapies are also used, such as the inoculation of cells and growth factors at the injury site [26, 27].
LLLT has demonstrated varied effects with different application parameters, such as an increase in functionality [9], better range of motion [28], the attenuation of dysesthesia [29], and the modulation of the concentration of inflammatory cytokines [30]. Thus, there is an evident need to understand the mechanisms of action involved in the modulation of the inflammatory process to achieve the desired effects.
The inadequate description of radiance parameters impeded the inclusion of many studies that report promising results. The lack of the description of the mode of application, frequency (pulsed mode), beam area, fluence, and energy as well as the onset and frequency of treatment renders the reproducibility of experiments impossible, since differences in these parameters have different effects. This failure to describe the protocol constitutes a barrier to the interpretation of the findings.
No standardization of parameters was found in the articles selected for the present review. Moreover, the different experimental models tested different aspects of a PNI. In chronic constriction models, there was a predominance of altered sensitivity [9, 30], whereas cross-sectioning and crushing models [19, 22] led to mixed alterations. It is therefore important to consider the experimental model chosen for the investigation of the motor and sensory aspects of a PNI. In models involving neurotmesis, Wallerian degeneration with consequent muscle atrophy is ensured, with consequent alterations in collagen distribution and muscle function [10, 31, 32]. Models involving axonotmesis have the advantage of greater standardization of the injury and no need for microsurgery training, but the rapid return to baseline conditions results in greater difficulty obtaining significant differences between the group submitted to the therapeutic protocol and the group submitted to injury alone. In contrast, regeneration is slower in neurotmesis models, which is critical for the transposition of the model to clinical trials [31].
Effects of LLLT on functionality
Functional recovery following a PNI begins after 12 days in a case of axonotmesis and 30 days in a case of neurotmesis, reaching a plateau at 28 and 120 days, respectively [31]. LLLT in both the red and infrared spectra accelerated the functional recovery process. In experimental models of axonotmesis due to crushing, Belchior et al. [33] found that red LLLT led an improvement in functionality, as demonstrated by the increase in the sciatic functional index (SFI) in the group submitted to laser therapy (660 nm, 26.3 mW, 7.6 J) for 20 consecutive days after surgery. Takhtfooladi et al. [34] found increases in both the SFI and sciatic static index after 14 and 21 consecutive days of LLLT (660 nm, 15 mW, 0.15 J) following injury. However, Barbosa et al. [17] only found an increase in the index at 14 days in the group submitted to LLLT (660 nm, 30 mW, 0.6 J) immediately after surgery for 20 consecutive days. In groups submitted to infrared radiation, an increase was found in the fibular functional index at 14 days in the study by Sousa et al. [35] with daily irradiation (830 nm, 40 mW, 2.77 J) for 28 days and the SFI in the study by Wang et al. [28] in groups irradiated (808 nm, 170 mW) with either 3 or 8 J for 20 consecutive days as well as an increase in range of motion in the group irradiated with 8 J.
With regard to chronic constriction models, Hsieh et al. [9] found an increase in functionality [motor aspect (SFI, fibular functional index, and tibial functional index) and sensitive aspect (mechanical hyperalgesia)] in groups irradiated 7 days after injury using red LLLT (660 nm, 30 mW, 7.2 J) for 7 consecutive days. Chen et al. [30] found a reduction in mechanical and thermal hyperalgesia at 4 and 8 days in groups irradiated 24 h after injury daily for 8 days using infrared LLLT (808 nm, 190 mW, 36 J). Masoumipoor et al. [29] demonstrated an increase in the thermal and mechanical thresholds of paw withdrawal in groups irradiated after injury daily for 2 weeks using red (660 nm, 100 mW, 3.4 J) and infrared (980 nm, 70 mW, 3.4 J) LLLT.
In models of neurotmesis followed by tubulization, Shen et al. [19] found an increase in the SFI, peak range of movement, and compound muscle action potential at 8 days in groups irradiated on the first day after surgery for 21 consecutive days using red LLLT (660 nm, 50 mW, 15 J). In another study by the same group [11], the same results were obtained in animals irradiated on the first day after surgery for 9 consecutive days, but after 12 weeks (660 nm, 50 mW, and 90 J immediately after surgery and 15 J over the subsequent 9 days). Medalha et al. [36] found accelerated functional recovery in models of neurotmesis followed by anastomosis in animals irradiated 24 h after surgery at a frequency of five sessions per week for 3 weeks using red LLLT (660 nm, 30 mW, 0.81 and 4.23 J), as demonstrated by the increase in the SFI at 4 months. However, using rats injured by neurotmesis followed by neurorrhaphy, Silva-Couto et al. [10] performed postoperative irradiation for 10 consecutive days as well as on alternating days for a total of 1 month using red and infrared LLLT with different energy doses (660 and 780 nm; 40 mW; 2.4, 4.8, and 9.6 J) and found no improvement in functional aspects measured using the SFI.
These findings demonstrate that different parameters alter the velocity of motor and sensory functional recovery. Thus, an irradiation protocol is needed for the optimization of this recovery.
Effects of LLLT on morphological aspects
The quantification of the morphological aspects of nerve fibers, especially myelinized fibers, is important to the investigation of the regenerative process [4]. The number and density of nerve fibers, diameter of axons and fibers, cross-sectional area of axons and fibers, perimeter of axons and fibers, and thickness of the myelin sheath are important to the analysis of the recovery [37]. After a PNI, morphological and metabolic changes are evident at the injury site, such as changes in the cell body, distal and proximal segments of the nerve injury, and the distal segment in the motor plate or sensory receptor. Injuries due to axonotmesis or neurotmesis have different regeneration rates, ranging from 3.0 to 4.4 mm/day in rats and 2.0 to 3.5 mm/day in rabbits [37].
In crushing models, Dias et al. [38] employed red LLLT (780 nm, 30 mW, 1.8 J) at 48-h intervals over a total of six sessions and found an increase in the concentration of myelin per cross-sectional area and an increase in the number of blood vessels 4 and 8 weeks after injury. Using the same parameters (780 nm, 30 mW, 1.8 J), Dias et al. [39] found an increase in the diameter of the nerve fibers 4 and 8 weeks after injury. Using infrared LLLT (808 nm, 170 mW, 11.4 and 30.4 J), Wang et al. [28] found an increase in the thickness of the myelin sheath 20 days after injury.
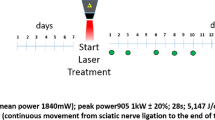
In neurotmesis models, Mohammed et al. [18] found an increase in the fiber length and the intermodal diameter of the fibular nerve at 2, 4, 6, and 8 weeks after injury in rabbits submitted to cross-sectioning and followed by neurorrhaphy, with postoperative irradiation for 10 consecutive days using infrared LLLT (901 nm, 2 mW, 1.2 J) in pulsed mode. Using red LLLT (660 nm, 50 mW, 15 J), Shen et al. [19] found an increase in the number of nerve fibers, axonal diameter, and myelin sheath in 8 weeks following cross-sectioning of the sciatic nerve of rats followed by tubulization. Shen et al. [11] performed irradiation on the first postoperative day using the same parameters (660 nm, 50 mW, 15 J) for 9 consecutive days, but with a greater energy immediately after surgery (90 J), reporting different findings, such as increases in the number of Schwann cells, neurofilaments, axonal diameter, thickness of the myelin sheath, as well as the diameter, and number of nerve cells at 12 weeks following the same injury model, demonstrating that a change in irradiation parameters can lead to different findings. In cross-sectioning models followed by anastomosis, Reis et al. [40] used red LLLT (660 nm, 26.3 mW, 7.6 J) following surgery for 20 consecutive days and found an increase in the myelin sheath at 21 days. Using red (660 nm, 30 mW, 4.23 J) and infrared (808 nm, 30 mW, 4.23 J) LLLT 24 h after surgery at a frequency of five sessions per week for 3 weeks, Medalha et al. [36] found an increase in the diameter of the axons and fibers in the irradiated groups when compared to the group submitted to injury without subsequent LLLT.
The positive photobiomodulating effects of red and infrared LLLT on morphological aspects in the studies selected for the present review underscore the need to investigate the mechanisms of action of different parameters to confirm the signaling pathways.
Effects of LLLT on expression of cytokines and growth factors
With a PNI, there is an increase in induced nitric oxide synthase (iNOS), resulting in the recruitment of inflammatory cells to the injury site, with an increase in the production and release of pro-inflammatory cytokines [22], such as those associated with neuropathic pain [tumor necrosis factor alpha (TNF-α) and interleukin 1 beta (IL-1β)] [9, 30]. The release of these cytokines can be stimulated by hypoxia-induced factor 1 alpha (HIF-1α) and the concentration increases ischemia and hypoxia during an inflammatory process [9]. Concomitantly to the relation of pro-inflammatory cytokines, neurotrophic factors are released to avoid necrosis of the nerve tissues and promote axonal regeneration. The major factors in this process are nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), and neurotrophins 3, 4, and 5 (NT3, NT4, NT5) as well as other growth factors, such as vascular endothelial growth factor (VEGF) [9, 22]. Moreover, growth-associated protein 43 (GAP-43) can be used as an indicator of nerve regeneration, since its concentration is proportional to the frequency of nerve sprouting exclusively during nerve regeneration in adult organisms [30].
In chronic constriction models, Hsieh et al. [9] demonstrated that red LLLT (660 nm, 30 mW, 7.2 J) increased the concentration of VEGF and NGF as well as diminished the expression of HIF-1α, TNF-α, and IL-1β. Chen et al. [30] found that infrared LLLT (808 nm, 190 mW, 36 J) diminished the gene and tissue expression of TNF-α 3 days after injury as well as diminished the gene expression of both GAP-43 and IL-1β. However, the tissue concentration of GAP-43 was increased.
In crushing models, Wang et al. [28] used infrared LLLT (808 nm, 170 mW, 11.4 and 30.4 J) and found an increase in the concentration of GAP-43 at 20 days following injury. Gomes et al. [22] used red LLLT (632.8 nm, 5 mW, 1 J) and found a reduction in the gene expression of iNOS at 21 days as well as an increase in the gene expression of both BDNF and NGF at 14 and 21 days after injury, but no change in the gene expression of NT3 was found at any evaluation time. Alcântara et al. [23] found that red LLLT (660 nm, 40 mW, 4.8 J) led to an increase in the concentration of TNF-α.
In general, the findings demonstrate the positive effects of photobiomodulation with LLLT. However, the divergent results confirm the need to establish ideal parameters. While the aim of LLLT is to diminish pro-inflammatory cytokines and increase growth factors, this therapeutic modality can lead to an increase in the concentration of TNF-α, demonstrating a modulating effect on nerve tissue, as reported in the study by Alcântara et al. [23]. Thus, further investigations into the mechanisms of action of LLLT are needed.
Conclusion
LLLT is a viable phototherapeutic modality for the treatment of peripheral nerve injury, demonstrating positive effects on the neuromuscular repair process using either red or infrared light, with improvements in the functional indices, morphological aspects, and expression of both cytokines and growth factors. The majority of studies used a power of up to 50 mW and total energy of up to 15 J administered to multiple points. The determination of these parameters is important to the standardization of a low-level laser therapeutic protocol to enhance the regeneration process following a peripheral nerve injury.
Funding
This work was supported by UNINOVE and the Brazilian fostering agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (www.cnpq.br; process number: 305739/2014 RAMF); Coordenação de Aperfeiçoamento de Pessoal do Nível Superior (www.capes.gov.br; process numbers: 1550120 LADS; 1183510 LADS; 1510536 BGR); Fundação de Amparo à Pesquisa do Estado de São Paulo (www.fapesp.br; process number: 2014/12381-1 RAMF, 2013/07502-1 KPSF).
References
Kim JR, Oh SH, Kwon GB, Namgung U, Song KS, Jeon BH, Lee JH (2013) Acceleration of peripheral nerve regeneration through asymmetrically porous nerve guide conduit applied with biological/physical stimulation. Tissue Eng Part A 19:2674–2685
Li R, Liu Z, Pan Y, Chen L, Zhang Z, Lu L (2014) Peripheral nerve injuries treatment: a systematic review. Cell Biochem Biophys 68:449–454
Martínez de Albornos P, Delgado PJ, Forriol F, Maffulli N (2011) Non-surgical therapies for peripheral nerve injury. Br Med Bull 100:73–100
Raimondo S, Fornaro M, Di Scipio F, Ronchi G, Giacobini-Robecchi MG, Geuna S (2009) Chapter 5: Methods and protocols in peripheral nerve regeneration experimental research: part II—morphological techniques. Int Rev Neurobiol 87:81–103
Xiao L, Tsutsui T (2013) Human dental mesenchymal stem cells and neural regeneration. Hum Cell 26:91–96
Seddon HS (1975) Surgical disorders of the peripheral nerves, 2nd edn. Churchill Livingstone, Edinburgh
Bobinski F, Ferreira TA, Córdova MM, Dombroski PA, da Cunha C, Santo CC, Poli A, Pires RG, Martins-Silva C, Sluka KA, Santos AR (2015) Role of brainstem serotonin in analgesia produced by low-intensity exercise on neuropathic pain after sciatic nerve injury in mice. Pain 156:2595–2606
Dubový P, Brázda V, Klusáková I, Hradilová-Svíženská I (2013) Bilateral elevation of interleukin-6 protein and mRNA in both lumbar and cervical dorsal root ganglia following unilateral chronic compression injury of the sciatic nerve. J Neuroinflammation 10:55
Hsieh YL, Chou LW, Chang PL, Yang CC, Kao MJ, Hong CZ (2012) Low-level laser therapy alleviates neuropathic pain and promotes function recovery in rats with chronic constriction injury: possible involvements in hypoxia-inducible factor 1α (HIF-1α). J Comp Neurol 520:2903–2916
Silva-Couto MA, Gigo-Benato D, Tim CR, Parizotto NA, Salvini TF, Russo TL (2012) Effects of low-level laser therapy after nerve reconstruction in rat denervated soleus muscle adaptation. Rev Bras Fisioter 16:320–327
Shen CC, Yang YC, Huang TB, Chan SC, Liu BS (2013) Neural regeneration in a novel nerve conduit across a large gap of the transected sciatic nerve in rats with low-level laser phototherapy. J Biomed Mater Res A 101:2763–2777
Ijkema-Paassen J, Jansen K, Gramsbergen A, Meek MF (2004) Transection of peripheral nerves, bridging strategies and effect evaluation. Biomaterials 25:1583–1592
Pachioni CAS, Mazzer N, Barbieri CH, Fazan VP, Padovani CR, Moro CA, da Silva CA (2006) Rats’ ischiatic nerve injury caused by smashing: a vascularization study. Acta Ortop Bras 14:203–207
Rochkind S, Geuna S, Shainberg A (2009) Chapter 25: Phototherapy in peripheral nerve injury: effects on muscle preservation and nerve regeneration. Int Rev Neurobiol 87:445–464
Passarella S, Karu T (2014) Absorption of monochromatic and narrow band radiation in the visible and near IR by both mitochondrial and non-mitochondrial photoacceptors results in photobiomodulation. J Photochem Photobiol B 140:344–358
Karu TI (2008) Mitochondrial signaling in mammalian cells activated by red and near-IR radiation. Photochem Photobiol 84:1091–1099
Barbosa RI, Marcolino AM, de Jesus Guirro RR, Mazzer N, Barbieri CH, de Cássia Registro Fonseca M (2010) Comparative effects of wavelengths of low-power laser in regeneration of sciatic nerve in rats following crushing lesion. Lasers Med Sci 25:423–430
Mohammed IFR, Al-Mustawfi N, Kaka LN (2007) Promotion of regenerative processes in injured peripheral nerve induced by low-level laser therapy. Photomed Laser Surg 25:107–111
Shen CC, Yang YC, Liu BS (2011) Large-area irradiated low-level laser effect in a biodegradable nerve guide conduit on neural regeneration of peripheral nerve injury in rats. Injury 42:803–813
Akgul T, Gulsoy M, Gulcur HO (2014) Effects of early and delayed laser application on nerve regeneration. Lasers Med Sci 29:351–357
Câmara CN, Brito MV, Silveira EL, Silva DS, Simões VR, Pontes RW (2011) Histological analysis of low-intensity laser therapy effects in peripheral nerve regeneration in Wistar rats. Acta Cir Bras 26:12–18
Gomes LEA, Dalmarco EM, André ES (2012) The brain-derived neurotrophic factor, nerve growth factor, neurotrophin-3, and induced nitric oxide synthase expression after low-level laser therapy in an axonotmesis experimental model. Photomed Laser Surg 11:642–647
Alcântara CC, Gigo-Benato D, Salvini TF, Oliveira AL, Anders JJ, Russo TL (2013) Effect of low-level laser therapy (LLLT) on acute neural recovery and inflammation-related gene expression after crush injury in rat sciatic nerve. Lasers Surg Med 45:246–252
Anders JJ, Moges H, Wu X, Erbele ID, Alberico SL, Saidu EK, Smith JT, Pryor BA (2014) In vitro and in vivo optimization of infrared laser treatment for injured peripheral nerves. Lasers Surg Med 46:34–45
Moges H, Wu X, McCoy J, Vasconcelos OM, Bryant H, Grunberg NE, Andes JJ (2011) Effect of 810 nm light on nerve regeneration after autograft repair of severely injured rat median nerve. Lasers Surg Med 43:901–906
Pan HC, Yang DY, Chiu YT, Lai SZ, Wang YC, Chang MH, Cheng FC (2006) Enhanced regeneration in injured sciatic nerve by human amniotic mesenchymal stem cell. J Clin Neurosci 13:570–575
Askari N, Yaghoobi MM, Shamsara M, Esmaeili-Mahani S (2015) Tetracycline-regulated expression of OLIG2 gene in human dental pulp stem cells lead to mouse sciatic nerve regeneration upon transplantation. Neurosci 305:197–208
Wang CZ, Chen YJ, Wang YH, Yeh ML, Huang MH, Ho ML, Liang JI, Chen CH (2014) Low-level laser irradiation improves functional recovery and nerve regeneration in sciatic nerve crush rat injury model. PLoS One 9:e103348
Masoumipoor M, Jameie SB, Janzadeh A, Nasirinezhad F, Soleimani M, Kerdary M (2014) Effects of 660- and 980-nm low-level laser therapy on neuropathic pain relief following chronic constriction injury in rat sciatic nerve. Lasers Med Sci 29:1593–1598
Chen YJ, Wang YH, Wang CZ, Ho ML, Kuo PL, Huang MH, Chen CH (2014) Effect of low level laser therapy on chronic compression of the dorsal root ganglion. PLoS One 9:e89894
Tos P, Ronchi G, Papalia I, Sallen V, Legagneus J, Geuna S, Giacobini-Robecchi MG (2009) Chapter 4: Methods and protocols in peripheral nerve regeneration experimental research: part I—experimental models. Int Rev Neurobiol 87:47–79
Rochkind S, Geuna S, Shainberg A (2013) Phototherapy and nerve injury: focus on muscle response. Int Rev Neurobiol 109:99–109
Belchior ACG, dos Reis FA, Nicolau RA, Silva IS, Pereira DM, de Carvalho PT (2009) Influence of laser (660 nm) on functional recovery of the sciatic nerve in rats following crushing lesion. Lasers Med Sci 24:893–899
Takhtfooladi MA, Jahanbakhsh F, Takhtfooladi HA, Yousefi K, Allahverdi A (2015) Effect of low-level laser therapy (685 nm, 3 J/cm2) on functional recovery of the sciatic nerve in rats following crushing lesion. Lasers Med Sci 30:1047–1052
Sousa FF, Andraus RA, Barbieri CH, Mazzer N (2009) Influence of laser radiation in nerve regeneration in different treatments sites. Acta Ortop Bras 17:331–335
Medalha CC, Di Gangi GC, Barbosa CB, Fernandes M, Aguiar O, Faloppa F, Leite VM, Rennó AC (2012) Low-level laser therapy improves repair following complete resection of the sciatic nerve in rats. Lasers Med Sci 27:629–635
Geuna S, Raimondo S, Ronchi G, Di Scipio F, Tos P, Fornaro M (2009) Chapter 3: Histology of the peripheral nerve and chances occurring during nerve regeneration. Int Rev Neurobiol 87:27–46
Dias FJ, Issa JP, Iyomassa MM, Coutinho-Netto J, Calzzani RA, Iyomassa DM, Sousa LG, Almeida SR, Cury DP, Watanabe IS (2013) Application of a low-level laser therapy and the purified protein from natural latex (Hevea brasiliensis) in the controlled crush injury of the sciatic nerve of rats: a morphological, quantitative, and ultrastructural study. Biomed Res Int 2013:597863
Dias FJ, Issa JP, Coutinho-Netto J, Fazan VP, Sousa LG, Iyomassa MM, Papa CP, Watanabe IS (2015) Morphometric and high resolution scanning electron microscopy analysis of low-level laser therapy and latex protein (Hevea brasiliensis) administration following a crush injury of the sciatic nerve in rats. J Neurol Sci 349:129–137
dos Reis FA, Belchior AC, de Carvalho PT, da Silva BA, Pereira DM, Silva IS, Nicolau RA (2009) Effect of laser therapy (660 nm) on recovery of the sciatic nerve in rats after injury through neurotmesis followed by epineural anastomosis. Lasers Med Sci 24:741–747
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study received approval from the Ethics Committee on Animal Experimentation of Universidade Nove de Julho under process 2/2016.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The informed consent was not necessary for this study.
Rights and permissions
About this article
Cite this article
Andreo, L., Soldera, C.B., Ribeiro, B.G. et al. Effects of photobiomodulation on experimental models of peripheral nerve injury. Lasers Med Sci 32, 2155–2165 (2017). https://doi.org/10.1007/s10103-017-2359-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2359-7