Abstract
The aim of this in vitro study was to optimise clinical parameters and the energy density of Er:YAG laser-conditioned dentin for class V fillings. Shear tests in three test series were conducted with 24 freshly extracted human third molars as samples for each series. For every sample, two orofacial and two approximal dentin surfaces were prepared. The study design included different laser energies, a thin vs a thick bond layer, the influence of adhesives as well as one-time- vs two-time treatment. The best results with Er:YAG-conditioned dentin were obtained with fluences just above the ablation threshold (5.3 J/cm2) in combination with a self-etch adhesive, a thin bond layer and when bond and composite were two-time cured. Dentin conditioned this way reached an averaged bond strength of 23.32 MPa (SD 5.3) and 24.37 MPa (SD 6.06) for two independent test surfaces while showing no statistical significance to conventional dentin adhesion and two-time treatment with averaged bond strength of 24.93 MPa (SD 11.51). Significant reduction of bond strength with Er:YAG-conditioned dentin was obtained when using either a thick bond layer, twice the laser energy (fluence 10.6 J/cm2) or with no dentin adhesive. The discussion showed clearly that in altered (sclerotic) dentin, e.g. for class V fillings of elderly patients, bond strengths in conventional dentin adhesion are constantly reduced due to the change of the responsibles, bond giving dentin structures, whereas for Er:YAG-conditioned dentin, the only way to get an optimal microretentive bond pattern is a laser fluence just above the ablation threshold of sclerotic dentin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dentin adhesives have become indispensable in modern dentistry for bonding tooth-coloured restorations. In defects of class V fillings not affected by caries but caused by erosion or abrasion, the bond strength of the restoration to the tooth is the most important factor for long-term clinical success in minimally invasive dentistry.
Sound dentin of freshly extracted third molars contains 33 vol% organic material, 20 vol% water and 47 vol% hydroxyapatite. Enamel on the other side is a highly mineral tissue, composed of 3 vol% organic material, 12 vol% water and 85 vol% hydroxyapatite. The relatively hydrophilic and complex nature of dentin created much more problems than the enamel to get a good adhesion to the hydrophobic resin composites.
Since Nakabayashi et al. [1] published their classic paper in 1982, it is known that good dentin adhesion can be achieved by formation of a hybrid layer. The mineral phase of dentin is removed by acids and the “spaghetti like” exposed collagen fibrils are infiltrated by hydrophilic monomers and cured in situ. Strong bond strength can then be achieved for resin composites [2].
Another problem in conventional dentin adhesion techniques is the formation of a smear layer, caused by diamond or carbide bur preparation. This smear layer can be removed (total etching) or partially modified (self-etching). If the smear layer is not removed (no etching), the bond strength on dentin is much lower [3, 4] than in total etch [5–7] or self-etch techniques [8].
A new technique in minimally invasive dentistry is the use of an Er:YAG laser. The laser energy at this wavelength of 2,940 nm is highly absorbed in water. The water in hydroxyapatite is rapidly vaporised and, due to its expansion, hard dental tissue will be removed by microexplosions [9–11]. When using an adequate water spray for this so-called thermomechanical ablation, thermal damages of the surrounding tissue can be avoided [12, 13]. The water spray is not primarily a cooling system but necessary for the ablation process [14, 15].
Dentin treated by Er:YAG laser creates always a microretentive pattern, when the ablation threshold is passed. The settings (energy, frequency, fluence and pulse duration) of the laser become very important, if a good adhesion is desired. And when we speak from minimally invasive dentistry, conditioning a class V defect by Er:YAG laser, we understand the lowest possible loss of health tooth substrate.
The aim of this in vitro study was to evaluate if the change of clinical parameters (with dentin adhesive vs no dentin adhesive, thin bond layer vs thick bond layer, one-time curing of bond and composite vs two-time curing) influence the bond strength of composite rods on Er:YAG-conditioned dentin surfaces when using a fluence of 5.3 J/cm2 (70 mJ, 1300 μm spot size) vs one of 10.6 J/cm2 (140 mJ, 1,300 μm spot size) [16]. The obtained forces per area, or shear strength values, were compared with those for a conventional self-etch adhesive technique.
Materials and methods
Design of the study
There were three test series with 24 freshly extracted human third molars in each, collected within 18 days and stored immediately after extraction in 0.5 % chloramine solution for disinfection. Teeth with complete roots were embedded in epoxy resin (Struers, Birmensdorf, CH) in a cold embedding procedure. Because the curing of the resin lasted 8 h, a special mould was constructed. After that time, the samples could be removed from the mould (Fig. 1) and stored in 0.9 % sodium chloride solution at room temperature [16].
At day 19 of each test series, two orofacial and two approximal dentin surfaces a, b, c and d were prepared on every molar sample. For this purpose a special preparation unit was constructed (Fig. 2 left) consisting of the following parts:
-
Drilling and milling lathe (PROXXON, BFB 2000)
-
Crosstable (PROXXON, KT 150)
-
Bench vise (BOSCH)
Therein, the samples were fixed for the preparation of the four dentin surfaces.
The dentin surfaces a, b, c and d were prepared with a handpiece (KAVO, INTRAmatic Lux3, 25 LH, Germany), fixed in the preparation unit (Fig. 2 right), at 200,000 rpm under full water spray of 65 ml/min with a blue diamond (Jota, Rüthi, Switzerland, Ref 883 314 014) of corn size 64 to 128 μm and then polished with Sof-Lex Popon discs (3M ESPE, Ref. 2381 C, 2382 M, Neuss, Germany) with 20,000 rpm under water spray of 50 ml/min of a corn size of 10 to 40 μm. All test surfaces were purely dentin [16], contained a smear layer and were marked with a trephine of 3.5 mm inside diameter (Ustomed, Tuttlingen, Germany, Art. Nr. 67-890-035) to an area of about 10 mm2.
For our purpose of this study, the handpiece in the preparation unit was moved only vertically and the crosstable with the fixed sample could be moved in the other two directions. The laser was an Er:YAG with a wavelength of 2,940 nm (LiteTouch, Orcos Medical, Küsnacht, Switzerland). The pulse duration was very short and could not be adjusted via the user interface. For a laser energy of 100 mJ according to the user interface—and experimentally measured as 140 mJ—and a frequency of 15 Hz, the pulse duration was measured to be 142 μs. For a lower laser energy of 50 mJ on display and effectively measured as 70 mJ at a frequency of 15 Hz, a pulse duration of 180 μs was determined.
The Er:YAG-treated dentin surfaces a, b and d were uniformly, vertically irradiated during 8 s under water spray (35 ml/min) and at a common clinical distance of between 2 and 3 mm. The spot size of the sapphire was 1,300 μm and the repetition rate 15 Hz. The application of the dentin adhesive (Syntac, Ivoclar Vivadent, Schaan, Lichtenstein) exactly followed the producer’s instructions.
The parameters were a laser energy of 140 mJ and a thin bond layer in the first test series A, 70 mJ and a thick bond layer in the second test series B, and 70 mJ and a thin bond layer in the third test series C.
Thin or thick bond layer are clinical terms. A thin bond layer means that the bond was blown away by dry and oil-free air after application such that the microretentive pattern in Er:YAG-conditioned dentin was clearly visible by eye without magnifying glasses, whereas for a thick bond layer, the pattern’s visibility disappeared completely.
A composite rod in a small bead used as a mould (Gütermann Bügelperlen weiss, Germany) was then bonded perpendicularly in four-hand dentistry
-
To surface a with Er:YAG-conditioned dentin and no dentin adhesive,
-
To surfaces b and d with Er:YAG-conditioned dentin with dentin adhesive and
-
To surface c, which was conventionally conditioned, with dentin adhesive.
The inner diameter of the bead was 2.6 mm and the length 5 mm. The bead was filled up to about 3/4 of the length with composite.
The composite in the beads was always precured for 3 s before bonding to reduce polymerisation contraction stress and to avoid deformation of the bead by the holder, while fixing it. To prevent air bubbles in the composite on the side of the bead, which was bonded to the dentin surfaces, the bead was always refilled with fresh composite [16].
While fixing the bead to the dentin surface, composite overhangs around the bead were removed by probe before curing. After having bonded the four composite rods in the bead to the dentin surfaces a–d (Fig. 3), the sample was incubated immediately for 24 h in a 37 °C water bath.
After then, the Gütermann beads, heated up by the temperature during incubation, could be removed with Furrer pliers (Aesculap, DP 752) from the composite rod very easily.
At day 21, the shear tests were executed with a Zwick universal machine (Z010, Zwick, Ulm, Germany). Given the perpendicularly bonded composite rods and the parallel surface alignments of a to c and b to d, the best physical conditions were provided to measure the shear forces. The shear bond strength was measured as the applied force per area at failure in newtons per square millimetre or megapascal.
All dentin surfaces of the first 12 sample teeth of each test series were cured one time (treatment I), and in the second 12 teeth two-time (treatment II). Table 1 illustrates the study design.
Investigated questions
The experimental outcome is described by the bond strength of each measurement, their mean and standard deviation for all four surfaces of all three test series. The data on adhesion were adjusted to a three-factor mixed linear model with the following specification:
-
Unstructured covariance
-
Fixed group factors of the test series A to C (three levels) and the treatments I and II (two levels)
-
Fixed factor repeated measures of the surfaces a to d (four levels)
In addition, the following seven questions were investigated:
-
1.
Are there differences between the surfaces b and d (averaged over all test series)?
-
2.
Are there differences between the surfaces a and c (averaged over all test series)?
-
3.
Are there differences between the surfaces b and d compared to a (averaged over all test series)?
-
4.
Are there differences between the surface c to b and d (averaged over all test series)?
-
5.
Is there a difference between conditioning with a laser energy of 70 or 140 mJ, using a thin bond layer; test series C vs A (averaged over all surfaces and treatments I and II)?
-
6.
Is there a difference between thin and thick bond layer, using a laser energy of 70 mJ; test series C vs B (averaged over all surfaces and treatments I and II)?
-
7.
Is there a difference between treatments I and II, i.e. one-time- or two-time curing of bond and composite (averaged over all laser energies and all surfaces)?
These questions were answered using linear contrasts in the statistical model. Effects were evaluated to be significant at a threshold value of p < 0.05. The calculations were performed using PROC MIXED, SAS® 9.1 (TS1M3) and the operating system Microsoft Windows XP.
Results
Evaluation of the test series
The following tables show the average measured bond strengths in megapascal of the test series A with a laser energy of 140 mJ and a thin bond layer (Table 2), of the test series B with a laser energy of 70 mJ and a thick bond layer (Table 3), and of the test series C with a laser energy of 70 mJ and a thin bond layer (Table 4).
The best average bond strengths in Er:YAG-conditioned dentin were reached with fluences just above the ablation threshold of dentin from freshly extracted teeth (5.3 J/cm2, 70 mJ, spot size 1,300 μm), using a self-etch dentin adhesive (surfaces b and d), a thin bond layer (test series C) and when bond and composite were two-time cured (treatment II in series C). They are comparable to the average bond strengths in conventional dentin adhesion. The corresponding average bond strengths for the Er:YAG-conditioned surface b are 23.32 MPa (SD 5.30) and 24.37 MPa (SD 6.06) for surface d. For the conventional treated surface c, treatment II, it is 24.93 MPa (SD 11.51).
Figure 4 shows the results of measurements from Tables 2, 3 and 4 graphically to illustrate the means and standard deviations for all three test series A, B and C. It was observed that the difference in averaged bond strength between treatment I and treatment II was much bigger for conventional adhesion (surface c) than for Er:YAG-conditioned dentin (surfaces a, b and d) in all three test series.
Significance of the model
The shear strengths of a total of 288 measured values for the three test series A to C and the four surfaces a to d were statistically analysed for significance with a threshold of 5 % (p < 0.05), using an analysis of variance (ANOVA) in a mixed linear model. The results are listed in Table 5. A clear significance between the surfaces a to d (p = 0.0003) and the test series A to C (p < 0. 0001) is apparent. Less clear, however, is a relationship between treatments I and II (p = 0.0366).
Examination of the investigated questions
The seven questions of clinical interest that were identified in section Material and Methods were statistically analysed. Table 6 shows the results.
Er:YAG-conditioned dentin surfaces generate significantly better average bond strengths when using a dentin adhesive (surfaces b and d) than without using one (surface a) (question 3). Conventional dentin adhesion shows significant better average bond strengths than Er:YAG-conditioned dentin without dentin adhesive (question 2). A laser energy of 70 mJ with a fluence of 5.3 J/cm2 creates significantly better average values than an energy of 140 mJ and a fluence of 10.6 J/cm2 (question 5).
A thick bond layer reduces the average bond strength significantly and for all surfaces a to d (question 6). Small advantages are seen when bond and composite are cured in two times instead of in one time (question 7).
No significance was shown between conventional dentin adhesion and Er:YAG-conditioned dentin with dentin adhesive (question 4) and the identical, Er:YAG-treated surfaces b and d (question 1). Table 7 shows the average bond strengths of each effect in megapascal (newtons per square millimetre) and reflects the statistical significances obtained from Table 6. Additionally, there was no significance (p = 0.7534, F = 0.10, NDF = 1, DDF = 67) between the average bond strengths of orofacial and approximal surfaces.
Discussion
The literature generally confirms that Er:YAG-conditioned dentin surfaces without application of a dentin adhesive show the lowest bond strengths. The reason is probably the fact that the hydrophobic nature of the bonding layer does not allow to wet and therefore to penetrate the laser-generated microretentive pattern of the hydrophilic dentin very well [17–21].
A thick bonding layer significantly reduces the bond strength for all surfaces due to its high polymerisation contraction of more than 10 %. We know that in conventional dentin adhesion, bond strengths are generated by formation of a hybrid layer in the intertubular dentin and via the formation of dentin tags in the dentin tubules [1, 5–8, 22–28].
The intertubular dentin in freshly extracted teeth, not affected by caries, is rich in collagen fibres, which are demineralised by acids. The “spaghetti-like”, exposed collagen fibres are infiltrated by hydrophilic polymerisable monomers and are bonded in situ by curing. The hydrophobic bond reacts chemically with the hydrophilic monomer to form a hybrid layer which can react with the hydrophobic composite restorative material.
We must assume that a classical hybrid layer formation in Er:YAG-conditioned dentin is not possible due to the optical and physical properties at this wavelength [10, 11, 14, 29]. The water-containing collagen fibres absorb the laser energy and are consequently denatured to a depth of about 15 to 20 μm. A hybridisation is therefore not probable [18–21].
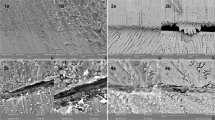
The dentin adhesion after Er:YAG laser conditioning is generated by formation of a microretentive pattern according to the transversal electromagnetic mode of this wavelength. (TEM31). It reflects nothing but the transversal distribution of the laser energy in the direction of propagation of the laser beam. The bond strength after Er:YAG laser irradiation in dentin is therefore generated by a huge magnification of the dentin surface and by dentin tags in the opened tubules. The dentin adhesive hydrophobises the Er:YAG laser-generated microretentive pattern in the intertubular dentin and the opened tubules.
It is known that, when class V defects must be restored, dentin will be altered due to grinding, pressing, attrition, decay, bur traumata or amalgam fillings without underlayer. These dentin alterations can show the following characteristics [30–32]:
-
Replacement of collagen-rich intertubular dentin by highly mineralized peritubular dentin.
-
Formation of acid-resistant (also phosphoric acid), highly mineralized areas
-
Denaturation of collagen fibres due to bur traumata or amalgam infiltration
-
Formation of crystallites in dentin tubules
All these above-mentioned sclerotisations in aged dentin are responsible for reduction of conventional dentin adhesion due to bonding mechanisms and are therefore responsible for clinical failures in restorative dentistry like microleakage and loss of class V fillings [33].
Er:YAG laser-generated dentin adhesion due to dentin alterations is in this sense only affected in that the optical properties of sclerotic dentin have changed because of lost water. The consequence therefore is an augmentation of the energy density to pass the ablation threshold of sclerotic dentin safely and to generate microretentive pattern.
The ablation threshold in dentin of freshly extracted teeth not affected by caries is at about at a fluence of 4 J/cm2 when using very short laser pulses between 100 and 200 μs. The ablation threshold in sclerotic dentin depends on the degree of sclerotisation (lost water) in sclerotic dentin; it is between a fluence of 5 and 6 J/cm2 at the pulse duration range just mentioned.
If the ablation threshold in sclerotic dentin is not reached, no microexplosions will occur and no microretentive pattern will be created, but the applied laser energy will be transferred as heat by conduction towards the pulp which can be damaged.
The fluence for optimal dentin adhesion is 5.3 J/cm2 according to our investigations. This value is slightly above the ablation threshold of dentin of freshly extracted teeth. Similarly, the energy density to generate an efficient microretentive pattern in altered dentin with optimal dentin adhesion must be just above the ablation threshold of the sclerotic dentin and can be reached with fluences between 6 and 10 J/cm2. Therefore, the therapeutic window to generate optimal Er:YAG-conditioned dentin adhesion is small.
Some studies mention that they obtained bond strength values comparable to those for conventional dentin adhesion at high energies and energy densities between 30.86 and 72.6 J/cm2 [34–37]. However, at such high fluences, the risk is very real of opening the pulp by removing too much healthy tooth substrate too quickly; one should then not speak of minimal invasiveness. Such laser settings would be more suitable to measure the preparation speed. Other authors have reported significantly lower bond strength values for laser-conditioned dentin and dentin adhesive than for conventional dentin adhesion when using lower fluences between 15.9 and 23 J/cm2 [18–20]. The suggested arguments for these findings are subsurface damages due to laser irradiation like scale of detached dentin, fissure building and denaturation of collagen fibrils in the areas where hybridization normally occurs. All studies concentrated on freshly extracted human premolars or third molars unaffected by caries where the best conditions exist for conventional dentin adhesion.
It is obvious that fluences between 15.9 and 23 J/cm2 exceed the ablation threshold of fresh dentin by multiple times compared to our own study and formation of scale, weakly joined to healthy dentin, at the mentioned energy densities is possible. Additionally, longer pulse durations of 250 μs were used. When the pulse duration of a laser pulse is shortened, the peak power is increased and the fluence to reach the ablation threshold is decreased. As a consequence, the thermal side effects when conditioning a dentin surface are decreased [14]. These are positive effects reducing or even eliminating subsurface damages resulting in better bond strengths [15, 38, 39].
Finally, conventional dentin adhesion demands for hybridisable intertubular dentin and non-crystallised tubules for clinical successful operations. These are two factors that are present in absolute perfection in almost all studies where freshly extracted human premolars or third molars are used. In clinical reality such dentin is often found to be very sensitive in younger patients with primary caries lesions, to include masticatory erosions due to pathologic reflux or bulimia, or to contain fractures of incisors. The formation of smear layers by diamond or carbide bur preparation, where smear plugs in the tubules are used in self-etch techniques as bonding substrates, can create very high bond strengths and can prevent postoperative pains [8, 40].
The exposed dentin in elderly patients is mostly non-sensitive with eroded incisal edges, amalgam-infiltrated or devital, or including alterations of any kind. Such dentin should be preferably conditioned by Er:YAG laser with fluences short above the ablation threshold of the irradiated tissue. The generated microretentive pattern is not sensitive to moisture, very user-friendly and not dependent on the age of the patient.
It becomes clear that dentin of older patients is altered through sclerotisation and the formation of hypermineralised areas and crystallites in the tubules. The volume of peritubular dentin is increasing, and that of intertubular dentin decreasing. The collagen fibres in the reduced intertubular area can be damaged by bur traumata or chemical influences. As a consequence, reduced bond strength must be expected by conventional dentin adhesion [30–32]. The advantage of treating sclerotic dentin with less water content than dentin of freshly extracted teeth by Er:YAG laser is that the only adaption needed is a higher fluence to get the ablation threshold. Hence, the Er:YAG laser conditioning of such altered dentin generates a microretentive pattern TEM 31 like in freshly extracted teeth. Therefore, the bond strengths must be, according to our investigation, comparable to conventional dentin adhesion under best conditions. As a logical consequence, traditional self-etch dentin adhesion in younger patients with high dentin sensitivities and laser-generated microretention in elderly patients successfully complement each other in clinics.
More investigation is needed to find out the optimal therapeutic windows for classical dentin adhesion and for Er:YAG-generated microretentive patterns in order to practise a safe minimal invasive dentistry.
References
Nakabayashi N, Kojima K, Masuhara E (1982) The promotion of adhesion by the infiltration of monomers into tooth substances. J Biomed Mater Res 16:265–273
Nakabayashi N, Pashley DH (1998) Hybridization of dental hard tissues. Quintessence, Chicago
Kramer IRH, McLean JW (1952) Alterations in the staining reaction of dentine resulting from a constituent of a new self-polymerising resin. Brit Dent J 92:150–153
Brudevold F, Buonocore M, Wileman W (1956) A report on a resin composition capable of bonding to human dentin surfaces. J Dent Res 35:846–851
Fusuyama T (1980) New concepts in operative dentistry. Quintessence, Chicago
Kanca J (1996) Improved bond strength through acid etching of dentin and bonding to wet dentin surfaces. J Am Dent Assoc 123:35–43
Kanca J (1996) Wet bonding: effect of drying time and distance. Am J Dent 9:273–276
Watanabe I, Nakabayashi N, Pashley DH (1994) Bonding to ground dentin by a phenyl-P self-etching primer. J Dent Res 73:1212–1220
Seka WD, Featherstone JD, Fried D, Visuri SR, Walsh JT (1996) Laser ablation of dental hard tissue: from explosive ablation to plasma-mediated ablation. Proc. SPIE 2672 Laser in Dentistry II, 144–158
Keller U, Hibst R (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances: II. Light microscopic and SEM investigations. Lasers Surg Med 9:345–351
Hibst R, Keller U (1993) Mechanism of Er:YAG laser-induced ablation of dental hard substances. Proc SPIE 1880:156–162
Fried D, Zuerlein M, Featherstone JDB, Seka W, Duhn C, McCormack SM (1998) IR laser ablation of dental enamel: mechanistic dependence on the primary absorber. Appl Surf Sci 127–129:852–856
Fried D, Ragadio J, Champion A (2001) Residual heat deposition in dental enamel during IR laser ablation at 2.79, 2.94, 9.6, and 10.6 microm. Lasers Surg Med 29:221–229
Gutknecht, N (ed) (2007). Proceedings of the 1st International Workshop of Evidence Based Dentistry on Lasers in Dentistry: Workshop in Vaals, the Netherlands; Feb. 2006. Quintessenz Verlags-GmbH, Berlin
Gutknecht N (2007) Kariologie und Kavitätenpräparation mit dem Er:YAG-Laser. LaserZahnheilkunde 2:75–83
Gisler G (2011) Untersuchungen zur Verbundfestigkeit von Komposit an Dentin bei Präparation der Dentinoberfläche mit einem Erbium-YAG Laser unter verschiedenen Bedingungen im Vergleich zu konventioneller, adhäsiver Technik. Master Thesis, RWTH Aachen
Delme KI, Deman PJ, De Moor RJ (2005) Microleakage of class V resin composite restorations after conventional and Er:YAG laser preparation. J Oral Rehabil 32:676–685
De Munck J, Van Meerbeek B, Yudhira R, Lambrechts P, Vanherle G (2002) Micro-tensile bond strength of two adhesives to erbium:YAG-lased vs. bur-cut enamel and dentin. Eur J Oral Sci 110:322–329
Ceballo L, Toledano M, Osorio R, Tay FR, Marshall GW (2002) Bonding to Er-YAG-laser-treated dentin. J Dent Res 81:119–122
Martínez-Insua A, Da Silva DL, Rivera FG, Santana-Penín UA (2000) Differences in bonding to acid-etched or Er:YAG-laser-treated enamel and dentin surfaces. J Prosthet Dent 84:280–288
Brulat N, Rocca JP, Leforestier E, Fiorucci G, Nammour S, Bertrand MF (2009) Shear bond strength of self-etching adhesive systems to Er:YAG-laser-prepared dentin. Lasers Med Sci 24:53–57
Lutz F, Krejci I, Schüpbach P (1993) Adhäsivsysteme für zahnfarbene Restaurationen. Schweiz Monatsschrift Zahnmed 103:537–549
Haller B (2000) Recent developments in dentin bonding. Am J Dent 13:44–50
Spencer P, Wang Y, Walker MP, Swafford JR (2001) Molecular structure of acid-etched dentin smear layers—in situ study. J Dent Res 80:1802–1807
Pashley DH, Ciucchi B, Sano H, Carvalho RM, Russell CM (1995) Bond strength versus dentine structure: a modelling approach. Arch Oral Biol 40:1109–1118
Gwinnett AJ, Tay FR, Pang KM, Wei SH (1996) Quantitative contribution of the collagen network in dentin hybridization. Am J Dent 9:140–144
Nakabayashi N, Takarada K (1992) Effect of HEMA on bonding to dentin. Dent Mater 8:125–130
Van Meerbeek B, Inokoshi S, Braem M, Lambrechts P, Vanherle G (1992) Morphological aspects of the resin–dentin interdiffusion zone with different dentin adhesive systems. J Dent Res 71:1530–1540
Hoke JA, Burkes EJ Jr, Gomes ED, Wolbarsht ML (1990) Erbium:YAG (2.94 mum) laser effects on dental tissues. J Laser Appl 2:61–65
Mendis BR, Darling AI (1979) Distribution with age and attrition of peritubular dentine in the crowns of human teeth. Arch Oral Biol 24:131–139
Duke ES, Lindemuth J (1991) Variability of clinical dentin substrates. Am J Dent 4:241–246
Tay FR, Pashley DH (2004) Resin bonding to cervical sclerotic dentin: a review. J of Dentistry 32:173–196
Davidson CL, de Gee AJ, Feilzer A (1984) The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res 63:1396–1399
Bertrand MF, Semez G, Leforestier E, Muller-Bolla M, Nammour S, Rocca JP (2006) Er:YAG laser cavity preparation and composite resin bonding with a single-component adhesive system: relationship between shear bond strength and microleakage. Lasers Surg Med 38:615–623
Celik EU, Ergücü Z, Türkün LS, Türkün M (2006) Shear bond strength of different adhesives to Er:YAG laser-prepared dentin. J Adhes Dent 8:319–325
Armengol V, Jean A, Weiss P, Hamel H (1999) Comparative in vitro study of the bond strength of composite to enamel and dentine obtained with laser irradiation or acid-etch. Lasers Med Sci 14:207–215
Visuri SR, Gilbert JL, Wright DD, Wigdor HA, Walsh JT Jr (1996) Shear strength of composite bonded to Er:YAG laser-prepared dentin. J Dent Res 75:599–605
Staninec M, Gardner AK, Le CQ, Sarma AV, Fried D (2006) Adhesion of composite to enamel and dentin surfaces by IR laser pulses of 0.5–35micros duration. J Biomed Mater Res B Appl Biomater 79:193–201
Burkes EJ, Hoke J, Gomes E, Wolbarsht M (1992) Wet versus dry enamel ablation by Er:YAG laser. J Prosthet Dent 67:847–51
Unemori M, Matsuya Y, Akashi A, Goto Y, Akamine A (2001) Composite resin restoration and postoperative sensitivity: clinical follow-up in an undergraduate program. J Dent 29:7–12W
Acknowledgments
The authors wish to thank Monika Vogt and Sonja Huber for their endurance in lending their hands to our four-hand dentistry needed to fix the rods to the samples for series I and for series II/III, respectively. Further, Franz Jungwirth of the University Hospital of Aachen was of great assistance in bond strength testing for all test series.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gisler, G., Gutknecht, N. The influence of the energy density and other clinical parameters on bond strength of Er:YAG-conditioned dentin compared to conventional dentin adhesion. Lasers Med Sci 29, 77–84 (2014). https://doi.org/10.1007/s10103-012-1243-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-012-1243-8