Abstract
Purpose
This in vitro study aimed at evaluating the influence of Nd:YAG irradiation and chlorhexidine (CHX) application on immediate and long-term bond strength of a self-etching adhesive system to dentin.
Methods
Thirty fragments of dentin were randomly divided into three groups according to the treatment to be applied to the dentin surface prior to applying the self-etching adhesive system (n = 10): CHX:2% CHX application (60 s); Nd: YAG (100 mJ/20 Hz for 20 s); and NT: no treatment. The adhesive system (Clearfil SE Bond, Kuraray) was applied according to the manufacturer’s instructions, and composite resin restorations were made on the dentin. After 24 h, at 37 °C, the resin-tooth blocks were sectioned perpendicular to the adhesive interface in the form of sticks (0.8 mm2 of adhesive area), and randomly subdivided into two groups according to the microtensile bond strength (μTBS) test periods: immediately or 6 months after storage in distilled water. The data were reported in MPa and submitted to two-way ANOVA for randomized blocks, followed by Tukey’s test (α = 0.05).
Results
The group irradiated with an Nd:YAG laser presented the lowest bond strength means, regardless of the μTBS test period (24 h or 6 months) (p < 0.05). No statistical difference was observed in the μTBS means among the groups CHX and NT (p > 0.05), nor did time influence bond strength (p > 0.05).
Conclusion
Immediate and long-term bond strength was negatively affected by Nd:YAG irradiation, a condition not observed with 2% CHX solution application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bond stability of adhesive systems to dentin is directly related to hybrid layer integrity. Degradation of polymers and collagen fibrils that compose the hybrid layer can compromise bond strength in the long term, causing the restoration to fail [1]. This degradation may occur in stages [1, 2]: water is absorbed by polymers and hydrolytic degradation is initiated; resin components are extracted from the hybrid layer and/or from the adhesive layer; collagen fibrils become unprotected and susceptible to enzymatic degradation by host-derived matrix metalloproteinases (MMPs) [3] or by cysteine cathepsins [4]. Also, during the adhesive system application on dentin, the ideal situation in which dentin is demineralized and subsequently penetrated by resin monomers is not always achieved [5], irrespective of the adhesive used in the etch-and-rinse or the self-etching approach [6, 7]. As a consequence, not fully covered collagen may stay exposed and vulnerable to degradation mediated by MMPs.
MMps are secreted as inactive proenzymes, but promote the degradation of collagen fibril, elastin and extracellular matrix components when activated [6]. These enzymes can be activated at a lower pH—as occurs when dentin is conditioned by acid etching—but function the best in a neutral pH—as occurs following application of an etch-and-rinse adhesive system [6, 8]. Recently, it has been demonstrated that self-etching adhesive systems can also activate MMPs by their acidic primer [9]. In addition, the drop in pH leads to the activation of cysteine cathepsins that also seem to activate MMPs [4].
Greater knowledge concerning MMPs and cysteine cathepsin enzyme action on hybrid layer degradation has encouraged the development and evaluation of substances that may inhibit their function. Among them, chlorhexidine digluconate (CHX) solution has been evaluated especially because of its MMPs [10] and cysteine cathepsin [11] inhibiting properties. Application of CHX solution does not influence bond strength to dental substrate [10] and promotes bond durability of adhesive restorations [12,13,14,15].
On the other hand, high-power lasers—mainly the Nd:YAG laser with a 1064 nm wavelength—have been employed on dental substrates to induce morphological alterations that make them more acid-resistant [16]. Also, Nd:YAG laser irradiation promotes cavity disinfection, while does not alter bond strength of adhesive systems to dentin, when irradiated with 120-mJ energy at 20-Hz pulse repetition [17]. It has been reported that ablation with Nd:YAG potentially decreases MMP-8 levels in patients with chronic periodontal disease when applied with a 100-mJ energy at 10-Hz frequency [18]. When irradiated with a 1.5-J/cm2 fluence, Q-switched Nd:YAG laser irradiation decreased MMP-2 mRNA levels [19]. This suggests that Nd:YAG laser irradiation offers promising technology for enhancing the bond stability of adhesives to dentin because of its possible MMP-inhibition action.
The possible inhibitory effect of host-derived MMPs by Nd:YAG irradiation, with consequent attenuation of hybrid layer degradation, can be indirectly measured by long-term bond strength, but this has never been reported in the literature. Thus, the aim of this study was to undertake a comparative investigation into the influence of CHX application and Nd:YAG irradiation on the immediate and long-term bond strength of a self-etching adhesive systems to human dentin. The null hypothesis tested was that neither dentin pre-treatment nor periods of water storage would exert an influence on bond strength of a self-etching adhesive to dentin.
Materials and methods
Ethical aspects
The present study was approved by the local research ethics committee (#2012/0200).
Experimental design
There are two factors under study in this vitro study:
-
I.
Dentin pre-treatment applied previously to a self-etching adhesive (Clearfil SE Bond, Kuraray), at three levels: LASER (Nd:YAG laser), 2% CHX, and control group (no treatment—NT), comparatively.
-
II.
Time points of microtensile bond strength testing: after storage in water for 24 h or for 6 months.
The quantitative outcome variable was the microtensile bond strength value, in MPa. The bond strength average of sticks from the same tooth became the value for that particular experimental unit (n = 10). The failure pattern was described in percentage terms.
The materials cited in the experimental design, as well as their composition and mode of use, are described in Table 1.
Preparation of tooth selection and dentin fragments
Thirty human third molars, extracted for reasons not related to those of the present research, and stored in thymol (0.1%, pH 7.0) after extraction, were used in this experiment. The teeth were submitted to debriding with scalpel blades and periodontal curettes. Then, they were cross-sectioned using a water-cooled diamond saw (15 HC series, Buehler Ltd., Lake Bluff, IL, USA) in a sectioning machine (IsoMet 1000 precision diamond saw, Buehler Ltd., Lake Bluff, IL, USA), which removed the occlusal third from the crown to obtain a large dentin surface in the middle third, perpendicular to the long axis of the tooth. The dentin surfaces were flattened in a water-cooled polishing machine (Politriz Aropol 2 V, Arotec, São Paulo, SP, Brazil) with decreasing granulations (#400, #600, and #1200) of water abrasive paper (Imperial Wetordry, 3 M, St. Paul, MN, USA).
Adhesive procedures
Dentin fragments were randomly divided into three groups, according to the treatment to be applied to the dentin surface: 2% CHX solution, Nd:YAG laser irradiation, or NT.
The procedure for the CHX group consisted of passively applying 20 μl of 2% CHX solution to the dentin for 60 s [20]. The dentin was then dried gently with absorbent paper.
For the LASER group, irradiation was performed with an Nd:YAG laser system (Power Laser™, ST6, Lares Research®, Chico, CA, USA), in the pulsed form, contact mode, and with 100 mJ of energy, and 20 Hz frequency. A 300-μm quartz fiber was used, thus the energy density calculated was ≅141.47 J/cm2. One irradiation of 20 s was performed per dentin fragment. One calibrated operator manually scanned the dentin surface with the optical fiber perpendicular to the dentin surface and running in the back and front direction. The irradiation protocol was similar to that proposed by Dalkilic et al. [17].
The self-etching adhesive system (Clearfil SE Bond, Kuraray, Japan) was then applied to the dentin fragments, which were restored with a microhybrid resin composite (Filtek Z250, 3 M ESPE, St. Paul, MN, USA). The final resin-dentin blocks were 4 mm high. Light polymerization was performed on both the adhesive system and the microhybrid composite, for the time recommended by the manufacturers (Table 1), using a visible light-curing unit (Ultralux EL, Dabi Atlante, Ribeirão Preto, SP, Brazil). The output of the light-curing unit was measured periodically with a radiometer (Newdent Equipamentos Ltda., Ribeirão Preto, SP, Brazil), where a minimal range of 630 mW/cm2 was observed.
The resin-dentin blocks were kept in relative humidity at 37 °C for 24 h, and sectioned perpendicular to the bonding surface into 0.9-mm thick slabs, using a water-cooled diamond saw. Multiple beam-shaped sticks were obtained by rotating samples 90° and sectioning them again lengthwise, each with a cross-sectional surface area of 0.8mm2. Half of the sticks from the same resin-dentin block were submitted to microtensile bond strength (μTBS) testing after 24 h. The other half were kept in distilled water, which was changed every 2 days and kept in a bacteriological oven for 6 months.
Microtensile bond strength testing
The specimens were attached to a μTBS testing device, with cyanoacrylate adhesive (Super Bonder Gel, Henkel Ltda., Itapevi, SP, Brazil). They were subjected to tensile stress on a universal testing machine, at a crosshead speed of 0.5 mm/min and a 50 N load cell until fracture. The bond strength values were expressed in kilogram-force/square centimeter, and converted to megapascal after measuring the cross-sectional area at the fracture site, with a digital caliper (Mitutoyo, Tokyo, Japan). The comparison was made using the average value of each tooth (n = 10).
After bond strength testing, the failure pattern of each stick was analyzed under a stereomicroscope (EK3ST, CQA, São Paulo, SP, Brazil) at ×30 magnification to assess the failure modes, classified as adhesive (lack of adhesion), cohesive in dentin (failure of the dental substrate), cohesive in composite resin (failure of the resin composite), or mixed (adhesive and cohesive failures).
Statistical analysis
Based on the normal distribution of the data, split-plot-factorial analysis of variance (ANOVA) and Tukey’s test were applied. Statistical calculations were performed with SAS* (SAS Institute Inc., Cary, NC, USA, Release 9.2, 2010). The significance level was set at 5%, and the failure pattern was described with descriptive statistics (percentage terms).
Results
As shown in Table 2, the LASER group presented the lowest mean bond strength, which was statistically different from that observed in the CHX and the NT groups, regardless of the time point for the microtensile bond strength evaluation (p < 0.05). CHX and NT groups presented statistically similar mean bond strength among the groups (p > 0.05). The time point for the microtensile bond strength evaluation (24 h or 6 months) did not statistically influence the mean bond strength (p > 0.05).
As for the failure modes (Fig. 1), most of the failures in the group that received no treatment (NT–control group) were cohesive in resin (57.9% for the 24-h and 40.0% for the 6-month time points), followed by the adhesive type (28.9% for the 24-h and 35.0% for the 6-month time points). In the group receiving the CHX application, a predominance of cohesive in resin failures (44.7%) was observed for the specimens tested after 24 h, and a predominance of adhesive (30.8%) followed by mixed failures (28.2%), for the specimens tested after 6 months. In terms of the Nd:YAG laser group, a predominance of adhesive type failures was observed after the 24-h (54.5%) and the 6-month (72.7%) time points.
Discussion
Considering the effect of MMPs on the degradation of the collagen exposed in the hybrid layer [3], the search for substances that inhibit the action of these enzymes has intensified [10, 12, 13, 20]. Thus, the aim of this in vitro study was to evaluate the effects of dentin pre-treatments that affect MMP activity—2% CHX digluconate and Nd:YAG irradiation—on the immediate and long-term bond strength of a self-etching adhesive to dentin.
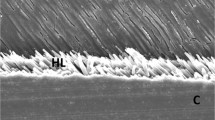
The results of this research demonstrated that the use of CHX did not affect the immediate bond strength, compared with the group that did not receive pre-treatment (control group), a result consistent with previous studies [2, 14, 17, 20, 21]. However, dentin irradiation with Nd:YAG negatively affected immediate and long-term bond strength to dentin. Thus, the null hypothesis was rejected. Similar results were obtained by Lise et al. [16], who observed that the microtensile bond strength of adhesive materials to Nd:YAG-irradiated dentin was lower than to non-irradiated dentin. It has been reported that Nd:YAG laser irradiation promotes the overheating of dental structures followed by their recrystallization [22]. This process results in an acid-resistant, melted dentin surface [23, 24] that can impair resin bond infiltration [22]. This can explain the fractures in the laser-irradiated group, which were predominantly of the adhesive type (Fig. 1). Although scanning electronic microscopy (SEM) images were not provided, the literature has confirmed morphological alterations in Nd:YAG-irradiated dentin [25], even when applied after adhesive polymerization [26].
The irradiation parameters may have a relevant influence on morphological alterations to dentin. The literature has shown that, in comparison with the parameters applied in the present study, Nd:YAG irradiation at a lower power, energy, and frequency favored bond strength [17] and decreased the microleakage [27] of the Clearfil SE Bond two-step self-etching adhesive to dentin. Another possible application of Nd:YAG was demonstrated by Marimoto et al. [28], that irradiated dentin over adhesives, before their polymerization, suggesting that this procedure creates a new bonding layer by dentin-adhesive melting. Future studies should look into alternative laser parameters and protocols of laser application that reduce morphological changes and favor dentin bond strength, while keeping inhibitory effects over MMPs and cathepsin proteases.
The Clearfil SE Bond adhesive system uses the self-etching approach, in which dentin demineralization and monomer infiltration occur simultaneously, unlike the etch-and-rinse approach, which requires the application of phosphoric acid, and which demineralizes dentin more deeply [5]. By using the etch-and-rinse approach, it has been demonstrated that Nd:YAG irradiation does not alter bond strength to dentin [29, 30]. This suggests that acid conditioning may be important for adhesion in Nd:YAG irradiated tissues. In fact, Gan et al. [31] stated that Nd:YAG irradiation (100 mJ/10 Hz) removed collagen fibrils in lased-dentin surface; thus, the resin composite infiltrated the micropores of hidroxyapatite created by acid etching instead of demineralized collagen matrices. As a result, dentin-resin bond interface was more stable over time and not vulnerable to the biodegradation [17].
Another observation is related to the fact that the Clearfil SE Bond self-etching adhesive system contains 10-methacryloxy decile dihydrogen phosphate (monomer 10-MDP), which promotes a strong ionic bond with calcium [5]. However, Nd:YAG irradiation reduces the percentage of calcium and phosphate in the dentin structure, causing changes in the organic composition of hydroxyapatite [32]. With this in mind, the chemical bonding capacity of 10-MDP to dentin calcium may have been lower after Nd:YAG irradiation.
At both periods (24 h and 6 months) of water storage, the bond strength values were statistically similar, regardless of the dentin pre-treatment. Accordingly, no beneficial effect was found for the CHX application, considering that the control group (without dentin pre-treatment) also showed bond stability. This stability can be attributed to the adhesive system, which not only promotes micromechanical retention, but also provides a chemical bond with calcium [5]. This stability may also have contributed to their having no significant decrease in bond strength after 6 months, in any of the groups, except the Nd:YAG laser group, in which the bond strength values constantly presented lower values. In addition, although the present study did not consider the evaluation of hybrid layer under SEM, it is hypothesized that the 6-month water storage period may have induced hydrolytic degradation at a microscopic level, but not enough to statistically alter bond strength values, even considering that the small size of the microtensile bond strength sticks may have facilitated water diffusion. To this effect, it can be suggested that prolonged water storage procedures would make degradative effects more evident in terms of altering bond strength to dentin [33].
Conclusion
Within the limitations of this in vitro study, it can be concluded that Nd:YAG laser application to dentin as a pre-treatment before applying a MDP-containing self-etching adhesive is contraindicated, because it negatively affected immediate and long-term bond strength to dentin, a result not observed with the application of 2% CHX.
References
Amaral FL, Colucci V, Palma-Dibb RG, Corona SA (2007) Assessment of in vitro methods used to promote adhesive interface degradation: a critical review. J Esthet Restor Dent 19:340–353
Sanabe ME, Costa CA, Hebling J (2011) Exposed collagen in aged resin-dentin bonds produced on sound and caries-affected dentin in the presence of chlorhexidine. J Adhes Dent 13:117–124
Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, Ito S (2004) Collagen degradation by host-derived enzymes during aging. J Dent Res 83:216–221
Nascimento FD, Minciotti CL, Geraldeli S, Carrilho MR, Pashley DH, Tay FR, Nader HB, Salo T, Tjäderhane L, Tersariol IL (2011) Cysteine cathepsins in human carious dentin. J Dent Res 90:506–511
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G (2003) Buonocore memorial lecture adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol IL, Geraldeli S, Tezvergil-Mutluay A, Carrilho M, Carvalho RM, Tay FR, Pashley DH (2013) Strategies to prevent hydrolytic degradation of the hybrid layer—a review. Dent Mater 29:999–1011
Mazzoni A, Tjäderhane L, Checchi V, Di Lenarda R, Salo T, Tay FR, Pashley DH, Breschi L (2015) Role of dentin MMPs in caries progression and bond stability. J Dent Res 94:241–251
Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjäderhane L, Toledano M, Pashley EL, Tay FR (2006) Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials 27:4470–4476
Mazzoni A, Scaffa P, Carrilho M, Tjäderhane L, Di Lenarda R, Polimeni A, Tezvergil-Mutluay A, Tay FR, Pashley DH, Breschi L (2013) Effects of etch-and-rinse and self-etch adhesives on dentin MMP-2 and MMP-9. J Dent Res 92:82–86
Erhardt MC, Osorio R, Toledano M (2008) Dentin treatment with MMPs inhibitors does not alter bond strengths to caries-affected dentin. J Dent 36:1068–1073
Scaffa PM, Vidal CM, Barros N, Gesteira TF, Carmona AK, Breschi L, Pashley DH, Tjäderhane L, Tersariol IL, Nascimento FD, Carrilho MR (2012) Chlorhexidine inhibits the activity of dental cysteine cathepsins. J Dent Res 91:420–425
Hebling J, Pashley DH, Tjäderhane L, Tay FR (2005) Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res 84:741–746
Carrilho MR, Geraldeli S, Tay F, de Goes MF, Carvalho RM, Tjäderhane L, Reis AF, Hebling J, Mazzoni A, Breschi L, Pashley D (2007) In vivo preservation of the hybrid layer by chlorhexidine. J Dent Res 86:529–533
Komori PC, Pashley DH, Tjäderhane L, Breschi L, Mazzoni A, de Goes MF, Wang L, Carrilho MR (2009) Effect of 2% chlorhexidine digluconate on the bond strength to normal versus caries-affected dentin. Oper Dent 34:157–165
Ricci HA, Sanabe ME, de Souza Costa CA, Pashley DH, Hebling J (2010) Chlorhexidine increases the longevity of in vivo resin-dentin bonds. Eur J Oral Sci 118:411–416
Lise AA, Guiggi PC, Larcondes ML, Jr Burnett LH, Spohr AM (2012) Nd:YAG laser influence on bond strength of adhesive resins to dentin. Stomatos 18:29–39
Dalkilic EE, Arisu HD, Kivanc BH, Uctasli MB, Omurlu H (2012) Effect of different disinfectant methods on the initial microtensile bond strength of a self-etch adhesive to dentin. Lasers Med Sci 27:819–825
Eltas A, Orbak R (2012) Effect of 1,064-nm Nd:YAG laser therapy on GCF IL-1β and MMP-8 levels in patients with chronic periodontitis. Lasers Med Sci 27:543–550
Ye X, Wang L, Dang Y, Liu B, Zhao D (2012) Investigation of the 1064 nm Q-switched Nd:YAG laser on collagen expression in an animal model. Photomed Laser Surg 30:604–609
Monteiro TMA, Basting RT, Turssi CP, França FMG, Amaral FLB (2013) Influence of natural and synthetic metalloproteinase inhibitors on bonding durability of an etch-and-rinse adhesive to dentin. Int J Adhes Adhes 47:83–88
Stape TH, Menezes MS, Barreto BC, Aguiar FH, Martins LR, Quagliatto PS (2012) Influence of matrix metalloproteinase synthetic inhibitors on dentin microtensile bond strength of resin cements. Oper Dent 37:386–396
Laxman KV, Ghosh S, Dhingra K, Patil R (2015) Effect of Er: YAG or Nd:YAG laser exposure on fluorosed and non-fluorosed root surfaces: an in vitro study. Laser Ther 31:93–101
Kinney JH, Haupt DL, Balooch M, White JM, Bell WL, Marshall SJ, Marshall GW Jr (1996) The threshold effects of Nd and Ho: YAG laser-induced surface modification on demineralization of dentin surfaces. J Dent Res 75:1388–1395
Sazak H, Türkmen C, Günday M (2001) Effects of Nd: YAG laser, air-abrasion and acid-etching on human enamel and dentin. Oper Dent 26:476–481
Anić I, Segović S, Katanec D, Prskalo K, Najzar-Fleger D (1998) Scanning electron microscopic study of dentin lased with argon, CO2, and Nd:YAG laser. J Endod 24:77–81
Ferreira LS, Ferreira LS, Francci C, Navarro RS, Calheiros FC, Eduardo Cde P (2009) Effects of Nd:YAG laser irradiation on the hybrid layer of different adhesive systems. J Adhes Dent 11:117–125
Savadi OS, Alizadeh OP, Jafari NE, Ahmad AA, Pournaghi AF, Rikhtegaran S, Amini M (2013) Comparison of the effect of Nd:YAG and diode lasers and photodynamic therapy on microleakage of class V composite resin restorations. J Dent Res Dent Clin Dent Prospects 7:74–80
Marimoto AK, Cunha LA, Yui KC, Huhtala MF, Barcellos DC, Prakki A, Gonçalves SE (2013) Influence of Nd:YAG laser on the bond strength of self-etching and conventional adhesive systems to dental hard tissues. Oper Dent 38:447–455
Ribeiro CF, Gonçalves SE, Yui KC, Borges AB, Barcellos DC, Brayner R (2013) Dentin bond strength: influence of Er:YAG and Nd:YAG lasers. Int J Periodontics Restorative Dent 33:373–377
Silva TM, Gonçalves LL, Fonseca BM, Esteves SR, Barcellos DC, Damião AJ, Gonçalves SE (2016) Influence of Nd:YAG laser on intrapulpal temperature and bond strength of human dentin under simulated pulpal pressure. Lasers Med Sci 31:49–56
Gan J, Liu S, Zhou L, Wang Y, Guo J, Huang C (2017) Effect of Nd:YAG laser irradiation pretreatment on the long-term bond strength of etch-and-rinse adhesive to dentin. Oper Dent 42:62–72
Malkoç MA, Sevimay M (2012) Evaluation of mineral content of dentin treated with desensitizing agents and neodymium yttrium-aluminium-garnet (Nd:YAG) laser. Lasers Med Sci 27:743–748
Breschi l, Mazzoni A, Nato F, Carrilho M, Visintini E, Tjäderhane L, Ruggeri A Jr, Tay FR, Dorigo Ede S, Pashley DH (2010) Chlorhexidine stabilizes the adhesive interface: a 2-year in vitro study. Dent Mater 26:320–325
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by CNPq (National Council for Scientific and Technological Development) [grant number 126120/2014-5].
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Menezello, S.A., França, F.M.G., Basting, R.T. et al. Effect of chlorhexidine application or Nd:YAG laser irradiation on long-term bond strength of a self-etching adhesive system to dentin. Laser Dent Sci 1, 41–46 (2017). https://doi.org/10.1007/s41547-017-0005-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-017-0005-0