Abstract
Background
Subthalamic nucleus deep brain stimulation (STN-DBS) is an effective surgical treatment for advanced Parkinson’s disease (PD). However, some patients still experience motor fluctuations or dyskinesia after STN-DBS. Safinamide is approved as add-on treatment to levodopa in fluctuating PD patients. In this study, we evaluated the effect of safinamide as adjunctive therapy in PD patients still experiencing motor fluctuations and dyskinesias after STN-DBS.
Methods
PD patients treated for at least 2 years with bilateral STN-DBST and with troublesome motor fluctuation and/or dyskinesias were examined by means of the Movement Disorders Society—Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), the quality of life questionnaire Parkinson’s Disease Questionnaire-8 (PDQ-8) and the Non-Motor Symptoms Scale (NMSS) at baseline (T0), after 1 month of treatment with safinamide 50 mg daily (T1) and after another month of treatment with safinamide 100 mg daily (T2).
Results
Twenty-nine PD patients were examined. An improvement of the MDS-UPDRS IV score (motor complications) was observed between T0 and T1, T0 and T2, and T1 and T2. The time spent in the OFF state, the functional impact and the complexity of motor fluctuations significantly improved between T0 and T1 and T0 and T2. The mean levodopa equivalent daily dose significantly decreased from T0 to T1 and from T0 to T2. Regarding non-motor symptoms, an improvement on mood and pain was observed.
Conclusions
Safinamide seems to be an effective adjunctive treatment in PD patients treated with bilateral STN-DBS, leading to an improvement of motor complications, mood and pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subthalamic nucleus deep brain stimulation (STN-DBS) is an effective surgical treatment for advanced Parkinson’s disease (PD) patients with troublesome motor complications or refractory tremor despite the optimization of medical therapy [1]. STN-DBS proved an average 60% reduction in levodopa-related motor complications [2, 3] and 40–60% improvement in quality of life (QoL) [4, 5]. Nonetheless, the clinical outcomes following DBS show a significant variability, and a notable number of patients still experience motor fluctuations or dyskinesias despite a correct lead placement and an accurate regulation of stimulation parameters [6, 7].
Safinamide is a novel dual-mechanism drug recently approved as add-on treatment to levodopa in fluctuating PD patients. Safinamide proved to be efficacious in the improvement of motor fluctuations, by increasing the on time without troublesome dyskinesia [8,9,10,11]. Moreover, an improvement of non-motor symptoms (NMS) has been reported, probably related to its dual effect on both dopaminergic and glutamatergic systems [12,13,14,15].
The aim of this study was to evaluate the effect of safinamide as adjunctive therapy in PD patients still experiencing motor fluctuations and dyskinesia notwithstanding undergoing STN-DBS, and to assess eventual further improvement of motor complications. In addition, we have also evaluated the role of safinamide in improving motor symptoms, NMS, activities of daily living (ADL) and QoL.
Methods
We recruited 29 consecutive PD patients at two experienced DBS centres: San Pio X Clinic (Milan) and Movement Disorders Clinic of the University of Turin. The inclusion criteria were:
-
diagnosis of idiopathic PD [16]
-
at least 2 years of treatment with bilateral STN-DBS
-
persistence of troublesome motor fluctuation and/or dyskinesias despite the best medical treatment (defined as the anti-parkinsonian therapy allowing the best control of symptoms with tolerable side effects; the treatment was best tailored to the individual patients and their responses), and the optimization of the stimulation parameters, defined as a score ≥ 2 at one or more of the items 4.1 (dyskinesia duration), 4.2 (functional impact of dyskinesia), 4.3 (time of waking day spent in OFF) or 4.4 (functional impact of fluctuations) of the MDS-UPDRS [17]
-
acquisition of written informed consent
The details of DBS surgery were described elsewhere [18]; position of the electrodes was verified with post-operative CT scan or MRI.
Patients were examined at baseline (T0) by means of the MDS-UPDRS. A subgroup of 10 patients (6 females, 4 males) was further investigated by means of the QoL questionnaire PDQ-8 [19] and the Non-Motor Symptoms Scale (NMSS) [20]. Levodopa equivalent daily dose (LEDD) was calculated according to the recognized standard conversion [21].
At T0, safinamide 50 mg daily was added to therapy in all patients. Patients were re-assessed after 1 month of treatment (T1) with the same scales used at T0. At this point, the dosage of safinamide was increased to 100 mg daily, and patients were re-assessed after 1 month (T2).
During the whole duration of the study, LEDD adjustments were allowed based on clinical assessment. The stimulation parameters remained unchanged; the mean voltage was 3.6 ± 0.9 V, the mean frequency was 115.7 ± 23.4 Hz and the mean pulse width was 60.3 ± 0.7 µs.
The primary outcome was the assessment of the improvement of motor complications, as per the changes of the MDS-UPDRS part IV score (and related sub-scores) at two different time points: 1 month after starting treatment with safinamide 50 mg (T1) and 1 month after starting treatment with safinamide 100 mg (T2).
The secondary outcome measures were:
-
motor symptoms, as per the changes at the MDS-UPDRS part III at T0, T1 and T2 in the Stimulation On-Medication On condition
-
ADL, as per the changes at the MDS-UPDRS part II at T0, T1 and T2
-
LEDD changes at T0, T1 and T2
-
NMS, as per the changes at the MDS-UPDRS part I (all patients), and at the NMSS at T0, T1 and T2 (10 patients)
-
QoL improvement, as per the PDQ-8 questionnaire (10 patients).
The statistical analysis was performed by the Wilcoxon signed-rank test for non-parametric data with Bonferroni’s correction for multiple comparisons, using the IBM-SPSS Statistics software version 25. It was considered significant a p level > 0.05.
All patients gave their informed consent for genetic testing and participation in the study. The study was performed in agreement with the principles of the Declaration of Helsinki and was approved by the local ethics committee.
Results
Twenty-nine PD patients, 13 females and 16 males, were included in the study.
The demographic and clinical features of patients are listed in Table 1 section A.
The demographic and clinical features of 10 patients who were assessed also for NMS and QoL are listed in Table 1 section B, showing no significant differences compared to the whole group of patients for age, disease duration, DBS duration, LEDD and MDS-UPDRS IV score.
Side effects
The therapy was well tolerated, also after the increase of dose. No side effects were reported.
Motor fluctuations and dyskinesias
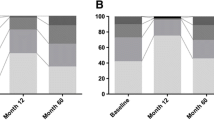
A significant improvement of the MDS-UPDRS IV score was observed between T0 and T1 (36.1 %; p < 0.001), T0 and T2 (66.3 %; p = 0.001), and T1 and T2 (47.2 %; p < 0.001) (Table 2).
Regarding MDS-UPDRS part IV sub-scores (Table 2), the main significant improvements were observed for the time spent in the OFF state (50.0% between T0 and T1 and 70.0% between T0 and T2; p < 0.001), for the functional impact of fluctuations (45.5% between T0 and T1 and 72.7% between T0 and T2; p < 0.001) and for the complexity of motor fluctuations (31.3% between T0 and T1 and 56.3% between T0 and T2; p = 0.002 and p = 0.001, respectively). A significant improvement was also observed for the functional impact of dyskinesias, with an improvement of 27.3% between T0 and T1 (p = 0.035) and an improvement of 54.5% between T1 and T2 (p = 0.031). The time spent with dyskinesias decreased from T0 to T1 and even more to T2, but the difference was not significant. The painful off-state dystonia score remained almost unchanged.
There were no significant differences between males and females.
Motor symptoms and ADL
Both the MDS-UPDRS II-III scores in the Stimulation On-Medication On condition significantly improved from T0 to T1 (p = 0.001) and from T0 and T2 (p = 0.006), whereas no significant differences were observed between T1 and T2 (Table 2).
There were no significant differences between males and females.
LEDD
In more than 50% of patients (16/29), LEDD was lowered after safinamide treatment and the mean LEDD value decreased significantly from T0 to T1 (p < 0.001) and from T0 to T2 (p = 0.003), while no significant differences between T1 and T2 were observed (Table 2).
There were no significant differences between males and females.
Non-motor symptoms
The MDS-UPDRS I score significantly decreased from T0 to T1 (p = 0.009), with no further changes at T2 (Table 2). A slight improvement was observed for depression comparing T0 and T1, and also T0 and T2 (p = 0.025). In addition, the score relative to pain and other sensations significantly improved at T1 (p = 0.020) and T2 (p = 0.015). A trend of improvement was also observed for the scores relative to cognitive impairment, hallucinations and psychosis, apathy, and fatigue.
In the subgroup of 10 patients, the NMSS evaluation (Table 3) showed that the mood/cognition score was significantly improved at T1 and T2 (p = 0.042). The sleep/fatigue and the attention/memory scores also improved at T1 and T2 but without reaching a significant difference as well as the urinary score; the gastrointestinal tract function assessment showed a mild, not significant worsening. The miscellaneous score was unchanged comparing T0 and T1, while the comparison between T0 and T2 showed a slight, not significant, improvement.
There were no significant differences between males and females.
Quality of life
The PDQ-8 was administrated to the subgroup of 10 patients (Table 3). A significant improvement was observed for the depression score at T2 (p = 0.046), while the improvement at T1 was not significant. The communication and the pain scores progressively improved from T0 to T1 and T2, but no significant differences were observed. The other items of the PDQ-8 remained unchanged, apart from the “getting around in public” score that slightly worsened at T2.
There were no significant differences between males and females.
Discussion
The main challenge of advanced PD treatment is represented by the motor complications related to the progression of the disease and to the chronic administration of levodopa [22]. Bilateral STN-DBS is an effective and safe treatment [2, 3]; however, some patients may still show motor fluctuations and dyskinesia after surgery with a clinically negative impact [6, 7].
Safinamide is an aminoamide derivative with a dopaminergic and non-dopaminergic mechanism of action [23]. The dopaminergic properties derive from its powerful, reversible and highly selective inhibition of the monoamine oxidase B (MAO-B), while the non-dopaminergic activity is related to the reduction of the sodium channels activity through a state- and use-dependent blockade, and to the inhibition of the glutamate release by N-type calcium channels [24].
Preclinical studies showed potential role of safinamide in PD by maintaining sustained dopamine levels and balancing the impaired dopaminergic-glutaminergic neurotransmission: safinamide has shown to potentiate levodopa-mediated increase in dopamine levels in dopamine-depleted mice, and to improve motor complications in levodopa treated 6-hydroxydopamine (6-OHDA)-treated rats [24]. Moreover, in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-lesioned dyskinetic macaque monkey, safinamide reduced levodopa-induced dyskinesias while increasing the duration of the antiparkinsonian response of levodopa [25].
In addition, preclinical studies have suggested that safinamide might have neuroprotective and neuro-rescuing effects in the mouse MPTP model, in the rat kainic acid model and in the gerbil ischemia model, although this has not been confirmed in humans [24].
Based on these preclinical findings, the beneficial role of safinamide has been tested in clinical trials for PD [26]. Borgohain et al. showed the efficacy of safinamide 50 or 100 mg daily in the reduction of off time together with the improvement of motor complications with the dosage of 100 mg daily [8]. Furthermore, an improvement of motor fluctuations without a worsening of dyskinesias was also observed [9, 10] suggesting that the modulation by safinamide 100 mg daily of glutamate receptors could play a specific role for the improvement of dyskinesias [27]; the same mechanism has been proposed for the improvement of NMS [15].
Our findings showed a significant improvement of motor complications with safinamide at both 50 and 100 mg daily dosage. The main effect was related to the reduction of the time spent in off and to the impact and complexity of motor fluctuations, mainly with the 100 mg daily dosage. A significant improvement was also observed in the functional impact of dyskinesias, while the on time with dyskinesias decreased for a lesser extent; in both cases, the improvement was greater for the 100 mg daily dosage. The efficacy of safinamide as add-on therapy in reducing off time has been clearly demonstrated [8,9,10], while its effect on dyskinesias is still debated. An increase in on time without troublesome dyskinesia has been reported, probably related to the glutamatergic inhibition [24], but a role of the reduction of levodopa dosage cannot be excluded. Our findings showed an improvement of dyskinesias scores at T1 (safinamide 50 mg daily) with a concomitant 13% reduction of LEDD; at T2 (safinamide 100 mg daily), dyskinesias further improved while LEDD was substantially unchanged (3% increase respect to T1). Probably, the LEDD reduction played a role at T1 while the further improvement at T2 was probably related to the specific glutamatergic inhibitory effect of safinamide [27].
NMS are one of the major determinants of quality of life in PD patients [28], and they are related to dopaminergic and non-dopaminergic neurotransmission [29]. We observed a slight but significant improvement of MDS-UPDRS I score both with safinamide 50 and 100 mg daily, with no differences between the two dosages. The main differences were observed in mood and pain scores for both dosages, although the effect was greater with 100 mg daily. Other non-motor aspects, as cognition and hallucinations, showed a trend towards an improvement.
Among NMS, we have also observed a significant improvement in mood and cognition with safinamide 100 mg daily, as well as a positive trend for sleep/fatigue and other items, including pain evaluation. Notably, depression showed a significant improvement with safinamide 100 mg daily.
A positive effect of safinamide on mood has been already reported [13, 15] possibly related to its glutamatergic mechanism of action [30, 31].
Moreover, it has been suggested that the positive effect of safinamide on pain [12, 14] could be related to the action at the voltage-gated sodium channels which are involved in the pathophysiology of chronic inflammation and neuropathic pain [32, 33], as well as to the modulation of the glutamatergic system [34, 35]. The efficacy of safinamide on pain has been already reported with a consistent effect mainly related to a direct drug effect rather than to an indirect effect mediated by motor or mood improvement [12].
In conclusion, our findings confirm the efficacy of safinamide on fluctuating PD patients with some limitations mainly due to the small size of our sample and to the short follow-up. Moreover, the PD patients assessed in our study have some specific features: indeed, they are patients in the advanced phase of the disease, with motor fluctuations and dyskinesia not completely controlled by a highly effective therapy such as STN-DBS. The efficacy of safinamide showed in these selected and severely affected patients further support the improvement of motor complications observed in patients with a less severe disease.
Finally, albeit in a small cohort of patients with a short follow-up, our study suggests that safinamide, mostly at the dosage of 100 mg daily, is an effective adjunctive treatment in PD patients treated with bilateral STN-DBS with residual motor fluctuations that leads to an improvement of motor complications with a concurrent positive effect on mood and pain. Further studies, in larger cohorts and with longer follow-up, are needed to confirm our findings.
Availability of data and material
Data is available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Antonini A, Moro E, Godeiro C, Reichmann H (2018) Medical and surgical management of advanced Parkinson’s disease. Mov Disord 33(6):900–908
Rizzone MG, Fasano A, Daniele A, Zibetti M, Merola A, Rizzi L, Piano C, Piccininni C, Romito LM, Lopiano L et al (2014) Long-term outcome of subthalamic nucleus DBS in Parkinson’s disease: from the advanced phase towards the late stage of the disease? Parkinsonism Relat Disord 20(4):376–381
Zibetti M, Merola A, Rizzi L, Ricchi V, Angrisano S, Azzaro C, Artusi CA, Arduino N, Marchisio A, Lanotte M et al (2011) Beyond nine years of continuous subthalamic nucleus deep brain stimulation in Parkinson’s disease. Mov Disord 26(13):2327–2334
Diamond A, Jankovic J (2005) The effect of deep brain stimulation on quality of life in movement disorders. J Neurol Neurosurg Psychiatry 76(9):1188–1193
Kurtis MM, Rajah T, Delgado LF, Dafsari HS (2017) The effect of deep brain stimulation on the non-motor symptoms of Parkinson’s disease: a critical review of the current evidence. NPJ Parkinsons Dis 3:16024
Buhmann C, Huckhagel T, Engel K, Gulberti A, Hidding U, Poetter-Nerger M, Goerendt I, Ludewig P, Braass H, Choe CU et al (2017) Adverse events in deep brain stimulation: a retrospective long-term analysis of neurological, psychiatric and other occurrences. PLoS One 12(7):e0178984
Limousin P, Foltynie T (2019) Long-term outcomes of deep brain stimulation in Parkinson disease. Nat Rev Neurol 15(4):234–242
Borgohain R, Szasz J, Stanzione P, Meshram C, Bhatt M, Chirilineau D, Stocchi F, Lucini V, Giuliani R, Forrest E et al (2014) Randomized trial of safinamide add-on to levodopa in Parkinson’s disease with motor fluctuations. Mov Disord 29(2):229–237
Borgohain R, Szasz J, Stanzione P, Meshram C, Bhatt MH, Chirilineau D, Stocchi F, Lucini V, Giuliani R, Forrest E et al (2014) Two-year, randomized, controlled study of safinamide as add-on to levodopa in mid to late Parkinson’s disease. Mov Disord 29(10):1273–1280
Schapira AH, Fox SH, Hauser RA, Jankovic J, Jost WH, Kenney C, Kulisevsky J, Pahwa R, Poewe W, Anand R (2017) Assessment of safety and efficacy of safinamide as a levodopa adjunct in patients with Parkinson disease and motor fluctuations: a randomized clinical trial. JAMA Neurol 74(2):216–224
Mancini F, Di Fonzo A, Lazzeri G, Borellini L, Silani V, Lacerenza M, Comi C (2018) Real life evaluation of safinamide effectiveness in Parkinson’s disease. Neurological sci 39(4):733–739
Cattaneo C, Barone P, Bonizzoni E (2017) Sardina M (2017) Effects of safinamide on pain in fluctuating Parkinson’s disease patients: a post-hoc analysis. J Parkinson dis 7(1):95–101
Cattaneo C, Muller T, Bonizzoni E, Lazzeri G, Kottakis I, Keywood C (2017) Long-term effects of safinamide on mood fluctuations in Parkinson’s disease. J Parkinson dis 7(4):629–634
Cattaneo C, Kulisevsky J, Tubazio V, Castellani P (2018) Long-term efficacy of safinamide on Parkinson’s disease chronic pain. Adv ther 35(4):515–522
Bianchi MLE, Riboldazzi G, Mauri M, Versino M (2019) Efficacy of safinamide on non-motor symptoms in a cohort of patients affected by idiopathic Parkinson’s disease. Neurological sci 40(2):275–279
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R et al (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170
Zibetti M, Romagnolo A, Crobeddu E, Fornaro R, Merola A, Rizzone MG, Lopiano L, Lanotte M (2014) Does intraoperative microrecording really increase the risk of hemorrhagic complications in deep brain stimulation? Brain Stimul 7(6):911–912
Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N (1997) The PDQ-8: development and validation of a short-form Parkinson’s disease questionnaire. Psychology Health 12(6):805–814
Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P, Ondo W, Abe K, Macphee G, Macmahon D et al (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22(13):1901–1911
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Ray Chaudhuri K, Poewe W, Brooks D (2018) Motor and nonmotor complications of levodopa: phenomenology, risk factors, and imaging features. Mov Disord 33(6):909–919
Fariello RG (2007) Safinamide. Neurotherapeutics 4(1):110–116
Caccia C, Maj R, Calabresi M, Maestroni S, Faravelli L, Curatolo L, Salvati P, Fariello RG (2006) Safinamide: from molecular targets to a new anti-Parkinson drug. Neurology 67:S18-23
Grégoire L, Jourdain VA, Townsend M, Roach A, Di Paolo T (2013) Safinamide reduces dyskinesias and prolongs L-DOPA antiparkinsonian effect in parkinsonian monkeys. Parkinsonism Relat Disord 19(5):508–514. https://doi.org/10.1016/j.parkreldis.2013.01.009
Muller T (2018) Safinamide: an add-on treatment for managing Parkinson’s disease. Clin pharmacol 10:31–41
Gregoire L, Jourdain VA, Townsend M, Roach A, Di Paolo T (2013) Safinamide reduces dyskinesias and prolongs L-DOPA antiparkinsonian effect in parkinsonian monkeys. Parkinsonism Relat Disord 19(5):508–514
Park A, Stacy M (2009) Non-motor symptoms in Parkinson’s disease. J Neurol 256(3):293–298
Fox SH (2013) Non-dopaminergic treatments for motor control in Parkinson’s disease. Drugs 73(13):1405–1415
Machado-Vieira R, Manji HK, Zarate CA (2009) The role of the tripartite glutamatergic synapse in the pathophysiology and therapeutics of mood disorders. Neuroscientist 15(5):525–539
Zarate C Jr, Machado-Vieira R, Henter I, Ibrahim L, Diazgranados N, Salvadore G (2010) Glutamatergic modulators: the future of treating mood disorders? Harv Rev Psychiatry 18(5):293–303
Salvati P, Maj R, Caccia C, Cervini MA, Fornaretto MG, Lamberti E, Pevarello P, Skeen GA, White HS, Wolf HH et al (1999) Biochemical and electrophysiological studies on the mechanism of action of PNU-151774E, a novel antiepileptic compound. J pharmacol exp ther 288(3):1151–1159
Miladinovic T, Nashed MG, Singh G (2015) Overview of glutamatergic dysregulation in central pathologies. Biomolecules 5(4):3112–3141
Bleakman D, Alt A, Nisenbaum ES (2006) Glutamate receptors and pain. Semin Cell Dev Biol 17(5):592–604
Juri C, Rodriguez-Oroz M, Obeso JA (2010) The pathophysiological basis of sensory disturbances in Parkinson’s disease. J Neurol Sci 289(1–2):60–65
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the local ethics committee and complies to the Declaration of Helsinki.
Consent to participate
All patients gave their informed consent to participate to the study.
Consent for publication
All patients gave their consent to publication of anonymised data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rizzone, M.G., Mancini, F., Artusi, C.A. et al. Efficacy of safinamide as add-on therapy after subthalamic nucleus deep brain stimulation in Parkinson disease. Neurol Sci 43, 3187–3193 (2022). https://doi.org/10.1007/s10072-021-05730-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05730-0