Abstract
Alterations of the intracranial pressure (ICP) may be present in several conditions. The aim of this brief review is to focus on two relatively rare conditions characterized by alterations in cerebro-spinal fluid dynamics—Spontaneous Intracranial hypotension (SIH) and Idiopathic Intracranial hypertension (IIH)—in which headache is one of the key symptoms. The most relevant clinical features, the expected MRI findings, and the therapeutic options regarding both conditions are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intracranial pressure, hypotension, and hypertension: definitions
Intracranial pressure (ICP) is the pressure within the intracranial space. In the steady state, pressure within the brain parenchyma and intracranial extra-axial spaces are equal. Normal values of ICP are 5–15 mmHg (6 e 20 cm H2O) in adults in the supine position, and up to 18 mmHg (25 cm H2O) in obese patients migraine [1–3]. ICP increases with Valsalva maneuver and falls below atmospheric pressure in the standing position.
Spontaneous intracranial hypotension (SIH) is a rare disabling condition whose main clinical manifestation is orthostatic headache [3–7]. Severe cases can result in decreased level of consciousness and coma [8].
Intracranial hypertension occurs in a chronic form in a large variety of neurologic and systemic disorders [9, 10]. ICP in the range of 20–30 mmHg is considered mildly increased, whereas ICP persistently exceeding 40 mmHg is severe and life threatening. The idiopathic form of this condition (idiopathic intracranial hypertension, IIH) has been described with different definitions, and is often referred as pseudotumor cerebri [9, 10]. Symptoms of intracranial hypertension include headache, nausea and vomiting, blurred vision, and in severe cases, altered level of consciousness and death. According to the Monro-Kellie doctrine in a closed compartment, such as the intracranial and spinal canal spaces which contain nervous tissue, blood and cerebro-spinal fluid (CSF), the loss of volume of one component (CSF in our case) must be compensated by a corresponding increase in the volume of the other ones. Since the CNS is generally considered to be invariable, compensation should only occur through increase of blood volume, essentially of venous blood, because veins are more easily expansible than arteries [3].
The aim of his short review is to summarize the most important aspect of SIH and IIH, both as far as clinical data, instrumental findings and treatment options.
Spontaneous intracranial hypotension
Clinical presentation
The most common symptom in SIH is orthostatic, or postural, headache. The classic orthostatic headache commences within 15 min, but often up to several hours, after assuming a standing or upright sitting position [4–6]. Improvement or resolution typically occurs within 15–30 min of lying down. Orthostatic headache in SIH is most likely caused by downward displacement of the brain and resulting traction on the richly innervated dura. Over time, the orthostatic feature of the headache may lessen, with a pattern of chronic daily headache ensuing.
Secondary symptoms often seen in conjunction with the postural headache include posterior neck pain or stiffness, and nausea and vomiting, attributable to meningeal irritation in approximately 50% of patients, sometimes with accompanying photophobia. Less commonly, hypacusia and tinnitus, attributable to either vestibulocochlear nerve traction associated with the sagging brain, or transmission of low CSF pressure to the perilymph, are reported [4–6].
Presence of at least one of these secondary symptoms, in addition to orthostatic headache, is required for the diagnosis of headache due to SIH in the 2004 International Classification of Headache Disorders (ICHD-2) criteria [5]. We note that in a case series of 90 patients studied by our group [7], only three had a headache fullfilling IHS criteria for headache attributed to SIH. Less common symptoms include vertigo, balance disturbance, blurred vision or visual field deficits, diplopia, facial pain or numbness, facial weakness or spasm, and dysgeusia, also attributed to cranial nerve distortion or compression caused by downward displacement of the brain [6]. Although very uncommon, stupor or coma, rarely progressing to demise from tonsillar herniation and brainstem compression, can be the initial presentation in severe intracranial hypotension [8].
Epidemiolgy
SIH occurs more often in women, with a female:male ratio of 3:2. Peak incidence is at approximately 40 years of age, with most cases presenting in the 40- to 60-year age range. Although the prevalence and incidence of SIH are unknown, one study reported an estimated annual incidence of 5/1,000, based on the frequency of this diagnosis in an emergency department setting [4]. The observation that reported incidences of SIH have increased in the past decade implies that the condition is likely still underdiagnosed, because the condition has only recently been recognized [4, 6].
Neuroimaging
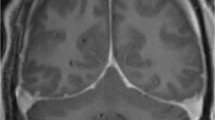
Despite the considerable variability of the clinical spectrum, neuroradiological studies reveal more constant and characteristic features. Brain MRI findings include intracranial pachymeningeal thickening and post-contrast enhancement, subdural fluid collections, and downward displacement or “sagging” of the brain. Spinal MRI findings include collapse of the dural sac with a festooned appearance, intense epidural enhancement owing to dilatation of the epidural venous plexus, and possible epidural fluid collections [6].
Treatment
Although recognition of SIH has increased in the past decade because of the increased sensitivity of MR imaging, SIH continues to be frequently misdiagnosed. A 2003 study reported that 17 of 18 consecutive patients referred to a surgical practice for the treatment of SIH with a documented CSF leak were initially misdiagnosed by a physician despite typical symptoms [11]. A 2007 study showed that, in a 3-year period, 11 patients who presented to an urban emergency room with SIH were all initially incorrectly diagnosed. [12].
Most cases of SIH resolve spontaneously; thus conservative treatment consisting in bedrest and hydration to treat symptoms. Once the diagnosis of SIH is made, epidural blood patch is recommended, according to our experience, if conservative treatments fail to reduce headache symptoms within 2 months.
The epidural blood patch is performed by administering autologous blood into the epidural space, usually at a lumbar level typically, 5–30 mL of blood and fibrin glue [13]. How this mainstay treatment of SIH works is not entirely clear. Two mechanisms have been proposed for the efficacy of epidural blood patch. The first is that the blood may increase ICP, by increasing the volume of the epidural space [14], and the second is that the clot tamponades the site of CSF leakage, sealing off the leakage [13]. These two mechanisms are likely to be complementary: headache relief is often immediate following blood patch, this would not be possible if the leak were simply sealed by a patch, because the formation of CSF is only 0.35 mL/min. In fact, according to our hypothesis [14] this syndrome may not be necessarily caused by a real leakage, but by CSF aspiration from the subarachnoid into the epidural space - and then into the venous system (inferior vena cava system), due to the low epidural pressure created by the presence of the large one-way valve collector veins in constitutionally predisposed individuals, such as those with constitutional weakness of dura or those with multiple subarachnoidal microdiverticula. We think that the dural tear, even when clearly identified, may be not the cause of the disease but the effect of the epidural hypotension maintained by the inferior cava vein outflow to the heart. This hypothesis could explain even those cases in which there is no neuroradiological evidence of a definite CSF leakage area or of spinal radicular cysts.
Idiopathic intracranial hypertension
Secondary intracranial hypertension can occur in chronic or acute forms in a large variety of neurologic and systemic disorders, including intracranial mass lesions such as tumor or abscess, traumatic brain injury, ischemic or hemorrhagic stroke, dural venous sinus thrombosis, dural arteriovenous fistula, hydrocephalus, or diffuse cerebral edema such as in liver failure [9, 10, 18].
A diagnosis of IIH is, therefore, a diagnosis of exclusion, which is made in the setting of chronic elevated ICP when a specific cause cannot be defined. Normal values of ICP in adults are in the range of 5–15 mmHg (6 e 20 mm H2O) [1]. ICP in the range of 20–30 mmHg is mildly increased and may need treatment, whereas ICP persistently exceeding 40 mmHg is a severe and life-threatening condition, which deserves appropriate treatment interventions.
Clinical presentation
Acute, abnormal increase of ICP results in headache, nausea and vomiting, blurred vision, and, in severe cases, reflex bradycardia and altered level of consciousness or death caused by cerebral hypoperfusion and/or brain herniation. In IIH, characterized by mild to intermediate chronic increase of ICP, the most common presenting symptom is chronic daily headache [9, 10, 15, 16].
Other common presenting symptoms in IIH are pulsatile tinnitus (60%) and transient visual obscurations (75%) [10, 16], the latter consisting of episodes of transient monocular or binocular vision loss that may occur with changes in head position. Diplopia caused by sixth nerve palsy has also been reported.
Patients may also present with more sustained, sometimes irreversible, vision impairment caused by longstanding untreated papilledema.
Epidemiology
The overall annual incidence of IIH is 1–2 per 100,000, although the incidence in women in the 20- to 44-year age range who are more than 20% heavier than ideal body weight is as much as 20 times higher [16].
Pathophysiology
IIH is characterized by chronically increased ICP in the absence of a specific known cause. Modified Dandy criteria for IIH [15], include increased opening pressure on lumbar puncture, with normal CSF composition and no known specific cause of increased ICP. IIH is likely heterogeneous as far as predisposing causes and risk factors, given its association with numerous clinical features. In addition to obesity, these also include dural venous sinus thrombosis, sleep apnea, vitamin A toxicity, and withdrawal from steroid medications [16]. Idiopathic intracranial hypertension is consistently associated with venous outflow disturbances. Sinus venous stenosis are found at magnetic resonance venography in the large majority of IIH patients and may have various conformations, ranging from functional smooth narrowings of sinus segments associated or not with definite flow gaps, to segmental hypoplasia or aplasia of one or more central venous collectors. Stenosis are currently believed to be a consequence of a primary altered CSF pressure since it may normalize after CSF subtraction with lumbar puncture or shunting procedures. A ‘‘self-sustained venous collapse’’ has been proposed as a crucial causative mechanism in predisposed subjects, leading to a self-sustained intracranial hypertension in presence of a wide range of triggering factors [17].
Diagnosis
An increased CSF opening pressure is the essential diagnostic criterion for IIH; imaging studies may be normal despite markedly increased ICP. In contrast, in SIH, CSF pressures can be within the normal range and imaging tests frequently play a key and decisive role in both diagnosis and treatment. IIH is suspected when opening pressure is in excess of 20 cm H2O (10 cm H2O in young children, and 25 cm H2O in obese patients) [2]. Asymptomatic presentations of IIH are common, e.g., when papilledema is noted during routine ophthalmologic examination.
IIH was included in the in the 2004 International Classification of Headache Disorders (ICHD-2), with rather detailed diagnostic criteria which include clinical presentation (daily headache; diffuse/non-pulsating pain; aggravation bt coughing or straining), demonstration of increased CSF pressure, as well as the presence of any of four different visual symptoms (papilloedema, enlarged blind spot, visual field defect, or sixth nerve palsy) [5].
Neuroimaging
Severe increase in ICP of any cause can result in diffuse effacement of sulci, small or slitlike ventricles, and/or brain herniation. Downward cerebral herniation is manifested as compressed or completely effaced basal cisterns, and subfalcine herniation is manifested as displacement of midline structures. Critically serious abnormalities include brainstem compression; compression of the posterior cerebral artery near the incisura, with resulting infarction; obstructive hydrocephalus secondary to compression of the foramen of Monro; anterior cerebral artery infarction secondary to subfalcine herniation; and cerebellar tonsillar and upward transtentorial cerebellar herniation. If cerebral perfusion pressure falls below 50 mmHg, as in severely increased ICP without a corresponding increase in mean arterial pressure, a reduction in cerebral blood flow may result in large-territory or global ischemia or infarction [19].
Imaging studies in patients with more modest increases of ICP, both acute and chronic, are often normal. In moderate elevation of ICP, as can occur in IIH, small sulci and/or small ventricles, dural venous sinus stenosis or occlusion of the dural venous sinus increases ICP, and is believed to be a cause for chronically increased ICP. However, dural venous sinus stenosis and occlusion may be a consequence rather than a cause of IIH [20].
Eye findings may also be present on brain imaging studies in a minority of cases of both chronic and acute intracranial hypertension [20, 21]. Flattening of the posterior sclera at the lamina cribrosa, dilated, fluid-filled optic nerve sheaths and enlargement and tortuosity of the superior ophthalmic veins are infrequent but specific imaging findings of increased ICP of any cause.
Treatment
Imaging is useful in excluding some treatable causes of intracranial hypertension. Conservative treatment of IIH includes weight reduction, acetazolamide, topiramate, and furosemide [16, 18]. The major long-term complication of IIH is irreversible partial or complete vision loss. Therefore, for those failing conservative treatment measures, optic nerve sheath fenestration and CSF shunting are sometimes performed.
References
Steiner LA, Andrews PJ (2006) Monitoring the injured brain: ICP and CBF. Br J Anaesth 97(1):26–38
Rangel-Castilla L, Gopinath S, Robertson CS (2008) Management of intracranial hypertension. Neurol Clin 26(2):521–541
Mokri B (2001) The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology 56(12):1746–1748
Schievink WI (2008) Spontaneous spinal cerebrospinal fluid leaks. Cephalalgia 28(12):1357–1360
Headache Classification Subcommittee of the International Headache Society (2004) International classification of headache disorders, 2nd edition. Cephalalgia 24
Schievink WI (2006) Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA 295(19):2286–2296
Mea E, Chiapparini L, Savoiardo M, Franzini A, Grimaldi D, Bussone G, Leone M (2009) Application of IHS criteria to headache attributed to spontaneous intracranial hypotension in a large population. Cephalalgia 29(4):418–422
Pleasure SJ, Abosch A, Friedman J et al (1998) Spontaneous intracranial hypotension resulting in stupor caused by diencephalic compression. Neurology 50(6):1854–1857
Radhakrishnan K, Ahlskog JE, Garrity JA et al (1994) Idiopathic intracranial hypertension. Mayo Clin Proc 69(2):169–180
Wall M (1991) Idiopathic intracranial hypertension. Neurol Clin 9(1):593–617
Schievink WI (2003) Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol 60(12):1713e8
Schievink WI, Maya MM, Moser F et al (2007) Frequency of spontaneous intracranial hypotension in the emergency department. J Headache Pain 8(6):325e8
Szeinfeld M, Ihmeidan IH, Moser MM et al (1986) Epidural blood patch: evaluation of the volume and spread of blood injected into the epidural space. Anesthesiology 64(6):820e2
Franzini A, Messina G, Nazzi V, Mea E, Leone M, Chiapparini L, Broggi G, Bussone G (2010) Spontaneous intracranial hypotension syndrome: a novel speculative physiopathological hypothesis and a novel patch method in a series of 28 consecutive patients. J Neurosurg 112(2):300–306
Friedman DI, Jacobson DM (2002) Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59(10):1492–1495
Randhawa S, Van Stavern GP (2008) Idiopathic intracranial hypertension (pseudotumor cerebri). Curr Opin Ophthalmol 19(6):445–453
De Simone R, Ranieri A, Bonavita V (2010) Advancement in idiopathic intracranial hypertension pathogenesis: focus on sinus venous stenosis. Neurol Sci 31(Suppl 1):S33–S39
Wall M (2008) Idiopathic intracranial hypertension (pseudotumor cerebri). Curr Neurol Neurosci Rep 8(2):87–93
Parizel PM, Makkat S, Jorens PG et al (2002) Brainstem hemorrhage in descending transtentorial herniation (Duret hemorrhage). Intensive Care Med 28(1):85e8
Agid R, Farb RI (2006) Neuroimaging in the diagnosis of idiopathic intracranial hypertension. Minerva Med 97(4):365–370
Brodsky MC, Vaphiades M (1998) Magnetic resonance imaging in pseudotumor cerebri. Ophthalmology 105(9):1686–1693
Conflict of interest
The author declares that he has no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mea, E., Franzini, A., D’Amico, D. et al. Treatment of alterations in CSF dynamics. Neurol Sci 32 (Suppl 1), 117–120 (2011). https://doi.org/10.1007/s10072-011-0559-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0559-7