Abstract
The treatment of brain metastases is changing. Many different radiotherapy options are now available and under clinical evaluation. As part of this effort, we retrospectively evaluated the efficacy and toxicity of hypofractionated stereotactic radiotherapy (HSRT) in patients with up to three brain metastases. Sixty-five patients with 81 lesions were treated with hypofractionated radiotherapy. Median dose was 24 Gy in three fractions. Median follow-up was 24.6 months. Actuarial tumour control was 75 and 45% at 9 months and 24 months after treatment, respectively. Median survival time was 7.5 months, and 32% of the patients died from brain tumour progression. Actuarial overall survival was 75% at 3 months and 25% at 12 months. Recursive partitioning analysis class was the only significant prognostic factor. Neoadjuvant whole-brain radiotherapy (in 29 patients) had no impact on survival or local control. Neurological status improved in 42 patients (65%). Adverse events were rare and usually mild. This experience suggests HSRT should be considered as an alternative approach in the treatment of one to three metastatic lesions in selected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases occur in 25% of cancer patients [1]. Treatment of brain metastases has historically included whole-brain radiotherapy (WBRT), which can produce tumour control, improve quality of life, and attenuate neurological symptoms. Life expectancy of patients treated with WBRT, however, is still disturbingly brief (2.8–5.3 months) [2], and the long-term risks of serious and permanent toxic effects resulting from WBRT are less understood [3, 4].
One of the most comprehensive retrospective meta-analyses yet to be published about single or oligo brain metastases has shown that single dose stereotactic radiosurgery (SRS) along with WBRT leads to a significantly longer overall survival compared to WBRT alone, for patients with good performance status (Karnofsky performance status (KPS) >70) and single brain metastases (level 1 evidence). Moreover, the authors pointed out that SRS, in combination with WBRT, seems to be more effective than WBRT alone in terms of local control in patients with one to four metastases and KPS >70 (level 2 evidence), and may lead to significantly longer survival in patients with two to three metastases (level 3 evidence). The authors note that the incidence of distant recurrence is lower when WBRT is added [5]. Several previous studies have reported similar results [4, 6–23]. SRS has been limited traditionally by the lesion’s dimensions and the proximity of critical structures. At the same time, the extent of late toxicity following WBRT is not well established, and so whether late toxicity is a major concern for clinicians is an open question [24].
Hypofractionated stereotactic radiotherapy (HSRT), by focusing the field of impact of the radiation, would theoretically improve the sparing of critical structures, and consequently may limit the long-term side effects of radiation therapy. In this sense, hypofractionated radiotherapy could have a primary role in the treatment of brain metastases, especially when these are close to critical structures, or have a main diameter larger than 3.5 cm.
Nevertheless, the literature lacks reports of previous experiences with hypofractionated radiotherapy for oligometastases. This retrospective review evaluates the efficacy and toxicity of hypofractionated stereotactic radiotherapy with or without WBRT in patients with three or fewer brain metastases arising from solid tumours.
Patients and methods
Patients
In the period between January 2001 and August 2005, 65 patients bearing 81 brain metastases were treated. Of these, 48 lesions were treated using a Philips SL 75/5 LINAC-based stereotactic system (Philips Medical Systems, Best, The Netherlands) with a dynamic micromultileaf collimator (DMLC) (3DLine International, Milan, Italy), and 33 lesions were treated with CyberKnife® (Accuray Incorporated, Sunnyvale, CA, USA). Patient selection criteria for stereotactic radiotherapy (SRT) at our institute were: a recursive partitioning analysis (RPA) classification I or II, one to three brain metastases, a single lesion with a diameter more than 35 mm, inoperable patients, multiple and very large lesions after WBRT (with RPA class I or II). The neurological status of the patients was prospectively classified according to the European Organization for Research and Treatment of Cancer (EORTC) scale (see Table 1) [25, 26]. Patient, lesion, and treatment characteristics are summarized in Table 1. Forty-eight patients (74%) had a solitary and 17 (26%) had multiple metastases; 36% of the lesions were subtentorial. Mean tumour volume was 8.0 cc (range, 0.3–48.2 cc). Twenty-six patients (40%) belonged to RPA class I and 39 patients (60%) to RPA class II. All 81 lesions were treated radiosurgically. Twenty-nine patients (44.5%) received neoadjuvant WBRT. Sixty-five percent of the patients initially presented with motor, speech, or cerebellar impairments; a minority had seizures without focal deficit (16%), or experienced headaches (9%). Ten percent of the patients were asymptomatic. Mean neurological score before treatment was two.
Treatment plan and delivery
Thirty-six patients were treated with a 6-MV, LINAC-based stereotactic system using a DMLC with a 4-mm leaf thickness at isocentre. Twenty-nine patients were treated with CyberKnife, a robotic LINAC-based (6-MV photons) system that employs an image-guided localization system to track the target position, and to aim the radiation beams with a large number of possible angles. Because fixed stereotactic frames were not necessary with either system, each patient was positioned comfortably with an individually fitted thermo-shell headrest attached to a mouthpiece assembly, and a non-invasive immobilization frame in the case of the Philips Linac treatment. Patients underwent contrast-enhanced CT and MR imaging of the entire brain using a slice thickness of 1.25–2 mm. These images were fused with automatic image fusion software based on surface matching using Ergo++ (Elekta AB, Stockholm, Sweden), and with a mutual information algorithm using CyrisTM (Accuray) to define the gross tumour volume (GTV) that was taken to be identical to the clinical target volume (CTV). The planning target volume (PTV) was defined to encompass the CTV plus a 2-mm margin in all directions [10]. Accuracy of the entire system was evaluated to be under 1 mm in the CyberKnife system and 2 mm in the 3DLine system. Median dose was 24 Gy in three fractions to a median isodose line of 78% for the CyberKnife system, and 80% for the LINAC-based system. The selected dose could be considered equivalent to 15 Gy in a single fraction [27]. Pre-SRT conventional WBRT (30 Gy in 3 Gy/fraction) was administered to 29 patients.
Quality criteria
The prescription isodose line included at least 95% of the PTV. For each plan, the dose–volume histogram (DVH) was calculated for the PTV and the organs at risk (OAR). Ergo++ and the CyberKnife On-TargetTM Treatment Planning System (Accuray) were used for dose calculation, and to input the contours defining the target volumes and the OAR on CT-MR fused images. For each plan, the conformity index (CI), as described by Paddick [28], and the homogeneity index (HI), which is the ratio of the maximum dose to the prescription dose (MDPD), were evaluated. Cerebral V15 was 5% or lesser.
Follow-up and statistics
All patients were evaluated with clinical and radiological follow-up using MRI after 2 months and every 3 months thereafter. Median follow-up was 24.6 months. End points were local tumour control rate, survival rate, functional neurological status at the end of treatment, and toxicity. In this evaluation, we defined complete response (CR) as >50% decrease, partial response (PR) as 25–49% decrease, stable disease (SD) as 0–25% decrease, and progressive disease (PD) as >25% increase in the size of the lesion on MRI [29]. When patients had more than one lesion, local response of each metastasis was reported individually. The functional neurological status was evaluated every 2 months. Survival was defined as the time period between the beginning of the therapy and the last follow-up or death. Death was assumed to be brain-related unless it was confirmed to be attributable to extracranial causes. Patients whose deaths were due to neither neurologic reasons nor systemic progression were classified as unknown.
Overall survival and local control curves were calculated by the Kaplan–Meier method. Univariate analyses were performed using the log-rank test, and stepwise forward conditional multivariate analyses were conducted using the Cox regression model to calculate the prognostic value of different variables related to survival and local tumour control (see Tables 2 and 3). The variables with p < 0.15 in the univariate analysis were included in the multivariate analysis.
Toxicity was evaluated according to the central nervous system toxicity criteria of the RTOG/EORTC late radiation morbidity scoring schema [30].
Results
Overall survival
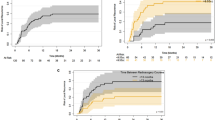
Median overall survival was 7.5 months (confidence interval, 5.9–9.2 months) with a median follow-up of 24.6 months. Patients who received WBRT had a median survival of 6.7 months (CI: 4.6–8.7 months). We found no difference in survival between patients who received SRT as primary therapy, and patients who received SRT after WBRT (p = 0.39). Survival curves for the two groups did not differ according to the log-rank test (Fig. 1).
Actuarial overall survival was 61 and 25% at 6 and 12 months, respectively (Fig. 2). The 23 patients in RPA class 1 had a median survival of 11.4 months (CI: 6.8–16.0 months), whereas the median survival time for the 37 patients in RPA class 2 was 5.0 months (CI: 3.5–6.4 months, P = 0.015) (Fig. 3).
Death was attributed to systemic disease progression in 21 patients (40.4%), to intracerebral progression in 24 patients (46.1%) of which 15 were sub-tentorial, and to unknown causes in 7 patients (13.5%).
Local control
Two patients failed to follow-up at the first follow-up scan at 2 months, and 79 lesions were evaluated (96%). MR scans at 6 months were available in all surviving patients with a total of 42 lesions. The 2-month local control rate was 90%. After 6 months, CR was achieved with seven metastases (16.7%), PR in 10 metastases (23.8%), and SD in 21 metastases (50%). Four lesions (9.5%) progressed. Actuarial local control was 79, 58.6, and 45% at 6, 12, and 24 months, respectively (Fig. 4). Twenty-six patients (40%) developed new cerebral metastases (distant brain failure, DBF). Median time to DBF was 4.7 months (range, 3–18 months). Patients who received WBRT along with SRT had a 6-month actuarial DBF rate of 20% compared with the 65% DBF rate in the same interval among patients who received SRT alone (p = 0.003).
Prognostic factors
Results of the univariate and multivariate analyses for prognostic factors regarding survival are shown in Table 2. The RPA class was found to be the only statistically significant prognostic factor, with patients in the RPA class 2 having a worse prognosis than those in the RPA class 1 (p < 0.001). All other analyzed variables failed to demonstrate any significant correlation with local control (Table 3). Tumours such as melanoma and clear cell carcinoma that are considered radioresistant appeared well controlled with SRT with a 1-year actuarial local control of 58%.
Neurological status
Sixty-five percent of the evaluable patients had an improvement of functional neurological status 2 months after SRT, compared with three patients reporting deterioration, and the remaining patients maintaining stable function. At day 7 after therapy, all the patients with stable or improved neurological status reduced the steroids intake, progressively, until it was suspended completely.
Toxicity
Treatment-related complications were observed in three patients during the early follow-up period (<3 months). These complications consisted of oedema, which did not cause major neurological complications. The condition was reversed through long-term high-dose steroid therapy. One patient underwent surgery due to a persistent drug-refractory oedema. The histologic work-up following the surgery pointed to radiation necrosis.
Dosimetry
Mean PTV volume corresponded to tumour volume plus a 2-mm margin. Mean cerebral V15 Gy was 5%. This data confirms the sharp fall-off in dose gradient with either system, including while treating larger lesions.
The collected data indicated a more favourable target coverage with the CyberKnife system using similar CI for both systems. The CI for the CyberKnife system was a mean 0.73 (range 0.56–0.86) compared with the CI for the LINAC system of 0.55 (0.48–0.70). Both systems produced a good HI, calculated as MDPD: a mean of 1.30 in the case of CyberKnife (range 1.19–1.47) and 1.24 with the LINAC system (range 1.06–1.33).
Discussion
This study retrospectively analyzed outcomes of 69 patients who had received HSRT with or without WBRT for one to three metastatic lesions. A total dose of 24 Gy in three fractions was delivered to the 80% isodose line. In 29 patients, the treatment was preceded by a standard regimen of WBRT, consisting of 30 Gy delivered in 3-Gy fractions.
The results of this analysis are in general agreement with earlier reports on HSRT. Actuarial local tumour control rates at 1 year have been reported as 64–91% [21, 23, 31]. In our study, the actuarial local control was 79% at 6 months and 59% at 12 months; in longer-term survivors, the actuarial local control rate at 24 months reached 45%.
WBRT did not influence local control or overall survival, but it has been shown to reduce DBF. The question of whether the use of WBRT as a pre-treatment option would improve the chances of survival of patients treated with SRS was recently analysed by Lindsey et al. (2010). The authors report a non-significant difference between using SRS alone and SRS plus WBRT in terms of overall survival, but at the same time they point out to a degree of a tendency towards a lower incidence of distant recurrence following WBRT [5].
Many questions remain unanswered regarding HSRT. Lindvall et al. [22] have compared the benefits of hypofractionated conformal stereotactic radiotherapy (HCSRT) with those of WBRT followed by a boost of SRS in treatment of cerebral metastases. Even though they did not observe a statistical difference between the two groups in local tumour control, they did observe that eight patients (25%) in the group treated with HCSRT had only developed new metastases in areas not covered by the irradiation. In contrast none of the patients treated with WBRT and SRS boost had developed new metastases (p = 0.0005). Despite this finding, they argued that “neoadjuvant treatment of the whole brain in patients with a short life expentancy was not necessary, as most patients would not live long enough to experience a new brain metastasis.” Moreover, a recent review by Schlienger et al. [32] has provided the most comprehensive examination on HSRT, and conceded that inclusion of WBRT could be a “confusing parameter.”
In the current study, patients who did not receive WBRT had the same probability of survival as those who did. There was also no evidence of better local tumour control among patients who received the combination therapy.
Another topic of debate remains the identification of relevant prognostic factors both for survival and local control. In the present study, the only statistically significant factor was identified as the RPA class. We would like to emphasize that in our series, we did not include any patients belonging to the RPA III class. Based on the RPA class, there was no survival difference between the two subgroups who did and did not receive neoadjuvant WBRT (p = 0.33, hazard ratio = 1.09). However Chidel et al. (2000), through their multivariate analysis, were able to show that the RPA class (p = 0.023) was in fact an independent predictor of overall survival [33].
Previous investigators have demonstrated that lesion volume is a prognostic factor for local tumour control and toxicity. However, again, we did not observe this relationship among treatment groups when stratified by tumour volume. This could be attributed to the patient selection criteria, which in this study included patients with tumours as large as 8 cc. Other researchers studied significantly smaller volumes [34].
In terms of local control, the histology of the disease also did not appear to be statistically significant, as long as sufficiently high doses are employed to overcome the relative resistance of histologies such as melanoma or clear-cell carcinoma. In fact the 1-year actuarial local control of these pathologies reached 58%, a percentage not dissimilar to that of breast cancer, a pathology that is considered radiosensitive..
This together with some of the statistical results of the current study could be limited by the small sample size of certain sub-groups but, in our opinion, this finding stresses the contribution of individual response variability to radiotherapy treatment above other factors.
With respect to toxicity, the present regimen of HSRT was well tolerated with similar results reported by several others [32, 34–37, 38]. Five percent of the patients showed moderate acute toxicity in the form of oedema, and one patient required surgical intervention. This could be related to the extremely conformal distribution of the dose and the sharp fall-off that allowed more efficient sparing of the surrounding normal brain tissues. In the present study, only the 5% of the normal brain received 15 Gy or more.
Because of the difficulty of collecting data relating to either neurological or radiological status during follow-up in patients with short life expectancy, few reports provide an accurate analysis of functional and morphological outcome of the patients. In the present series, more than half of the patients experienced an improvement of neurological status as evaluated at 2 months after treatment.
Conclusions
In conclusion, HSRT, with or without WBRT, provides reasonable and comparable tumour control and survival in patients with up to three metastatic lesions in their brain, even in the case of larger tumours. The neurological toxicity rate was low, and because of the non-invasive nature of the adopted restraints, the patient compliance is very high. These results suggest HSRT should be considered as an alternative approach in the treatment of one to three metastatic lesions in selected patients instead of the standard WBRT or in addition to it. Although a specific schedule for HSRT has not yet been established, the high target coverage with CyberKnife or IMRT may allow a dose escalation study to that end.
References
Posner JB, Chernik NL (1978) Intracranial metastases from systemic cancer. Adv Neurol 19:579–592
Khuntia D, Brown P, Li J, Mehta MP (2006) Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol 24:1295–1304
DeAngelis LM, Delattre JY, Posner JB (1989) Radiation induced dementia in patients cured of brain metastases. Neurology 39:789–796
Soffietti R, Rudà R, Trevisan E (2008) Brain metastases: current management and new developments. Curr Opin Oncol 20(6):676–684
Lindsey ME, Andrews DW, Asher AL, Burris SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN (2010) The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96(1):45–68
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs. stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Gaudy-Marqueste C, Regis JM, Muracciole X, Laurans R, Richard MA, Bonerandi JJ, Grob JJ (2006) Gamma-Knife radiosurgery in the management of melanoma patients with brain metastases: a series of 106 patients without whole-brain radiotherapy. Int J Radiat Oncol Biol Phys 809–816
Hasegawa T, Kondziolka D, Flickinger JC, Germanwala A, Lunsford LD (2003) Brain metastases treated with radiosurgery alone: an alternative to whole brain radiotherapy? Neurosurgery 52:1318–1326
Shirato H, Takamura A, Tomita M, Suzuki K, Nishioka T, Isu T, Kato T, Sawamura Y, Miyamachi K, Abe H, Miyasaka K (1997) Stereotactic irradiation without whole-brain irradiation for single brain metastasis. Int J Radiat Oncol Biol Phys 37:385–391
Sneed PK, Suh JH, Goetsch SJ, Sanghavi SN, Chappell R, Buatti JM, Regine WF, Weltman E, King VJ, Breneman JC, Sperduto PW, Mehta MP (2002) A multi-institutional review of radiosurgery alone vs. radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 53:519–526
Aoyama H, Shirato H, Onimaru R, Kagei K, Ikeda J, Ishii N, Sawamura Y, Miyasaka K (2003) Hypofractionated stereotactic radiotherapy alone without whole-brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys 56:793–800
Lederman G, Wronski M, Fine M (2001) Fractionated radiosurgery for brain metastases in 43 patients with breast carcinoma. Breast Cancer Res Treat 65:145–154
Muacevic A, Kreth FW, Mack A Tonn JC, B Wowra (2004) Stereotactic radiosurgery without radiation therapy providing high local tumor control of multiple brain metastases from renal cell carcinoma. Minim Invasive Neurosurg 47:203–208
Schoeggl A, Kitz K, Reddy M (2002) Stereotactic radiosurgery for brain metastases from colorectal cancer. Int J Colorectal Dis 17:150–155
Schomas DA, Roeske JC, MacDonald RL, Sweeney PJ, Mehta N, Mundt AJ (2005) Predictors of tumor control in patients treated with linac-based stereotactic radiosurgery for metastatic disease to the brain. Am J Clin Oncol 28:180–187
Selek U, Chang EL, Hassenbusch SJ 3rd, Shiu AS, Lang FF, Allen P, Weinberg J, Sawaya R, Maor MH (2004) Stereotactic radiosurgical treatment in 103 patients for 153 cerebral melanoma metastases. Int J Radiat Oncol Biol Phys 59:1097–1106
Serizawa T, Saeki N, Higuchi Y, Ono J, Iuchi T, Nagano O, Yamaura A (2005) Gamma knife surgery for brain metastases: indications for and limitations of a local treatment protocol. Acta Neurochir (Wien) 147:721–726
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Kocher M, Maarouf M, Bendel M, Voges J, Müller RP, Sturm V (2004) Linac radiosurgery versus whole brain radiotherapy for brain metastases: a survival comparison based on the RTOG recursive partitioning analysis. Strahlenther Onkol 180:263–267
Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD (2005) Radiosurgery with or without whole-brain radiotherapy for brain metastases: the patients’ perspective regarding complications. Am J Clin Oncol 28:173–179
Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45:427–434
Lindvall P, Bergstrom P, Lofroth PO (2005) Hypofractionated conformal stereotactic radiotherapy alone or in combination with whole-brain radiotherapy in patients with cerebral metastases. Int J Radiat Oncol Biol Phys 61:1460–1466
Pirzkall A, Debus J, Lohr F, Fuss M, Rhein B, Engenhart-Cabillic R, Wannenmacher M (1998) Radiosurgery alone or in combination with whole-brain radiotherapy for brain metastases. J Clin Oncol 16:3563–3569
Murray KJ, Scott C, Zachariah B, Michalski JM, Demas W, Vora NL, Whitton A, Movsas B (2000) Importance of the mini-mental status examination in the treatment of patients with brain metastases: a report from the Radiation Therapy Oncology Group protocol 91–04. Int J Radiat Oncol Biol Phys 48:59–64
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Gaspar LE, Scott C, Murray K, Curran W (2000) Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiat Oncol Biol Phys 47:1001–1006
Yuan J, Wang JZ, Lo S, Grecula JC, Ammirati M, Montebello JF, Zhang H, Gupta N, Yuh WT, Mayr NA (2008) Hypofractionation regimens for stereotactic radiotherapy for large brain tumors. Int J Radiat Oncol Biol Phys 1:72(2): 390–397
Paddick I. (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 93(Suppl 3):219–222
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:1277–1280
Radiation Therapy Oncology Group (1999) RTOG/EORTC Late radiation morbidity scoring schema. http://www.rtog.org/members/toxicity/late.html. Accessed June 15
Rades D, Bohlen G, Pluemer A, Veninga T, Hanssens P, Dunst J, Schild SE (2007) Stereotactic radiosurgery alone versus resection plus whole-brain radiotherapy for 1 or 2 brain metastases in recursive partitioning analysis class 1 and 2 patients. Cancer 15:109(12):2515–2521
Schlienger M, Nataf F, Huguet F, Pene F, Foulquier JN, Orthuon A, Roux FX, Touboul E (2010) Hypofractionated stereotactic radiotherapy for brain metastases. Cancer Radiother 14(2):119–127
Chidel MA, Suh JH, Reddy CA, Chao ST, Lundbeck MF, Barnett GH (2000) Application of recursive partitioning analysis and evaluation of the use of whole brain radiation among patients treated with stereotactic radiosurgery for newly diagnosed brain metastases. Int J Radiat Oncol Biol Phys 47:993–999
Kwon AK, Dibiase SJ, Wang B, Hughes SL, Milcarek B, Zhu Y (2009) Hypofractionated stereotactic radiotherapy for the treatment of brain metastases. Cancer 15:115(4):890–898
Giubilei C, Ingrosso G, D’Andrea M, Benassi M, Santoni R (2009) Hypofractionated stereotactic radiotherapy in combination with whole brain radiotherapy for brain metastases. J Neurooncol 91(2):207–212
Hara W, Tran P, Li G, Su Z, Puataweepong P, Adler JR Jr, Soltys SG, Chang SD, Gibbs IC (2009) Cyberknife for brain metastases of malignant melanoma and renal cell carcinoma. Neurosurgery 64(2 Suppl):A26–A32
Manning MA, Cardinale RM, Benedict SH, Kavanagh BD, Zwicker RD, Amir C, Broaddus WC (2000) Hypofractionated stereotactic radiotherapy as an alternative to radiosurgery for the treatment of patients with brain metastases. Int J Radiat Oncol Biol Phys 47:603–608
Scorsetti M, Facoetti A, Navarria P, Bignardi M, De Santis M, Ninone SA, Lattuada P, Urso G, Vigorito S, Mancosu P, Del Vecchio M (2009) Hypofractionated stereotactic radiotherapy and radiosurgery for the treatment of patients with radioresistant brain metastases. Anticancer Res 29(10):4259–4263
Acknowledgment
The authors wish to thank Dr. David W. Schaal and Dr. Mikail Gezginci, Accuray Incorporated, for technical and editorial assistance.
Conflict of interest
The authors have no financial interest in the instruments presented in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marchetti, M., Milanesi, I., Falcone, C. et al. Hypofractionated stereotactic radiotherapy for oligometastases in the brain: a single-institution experience. Neurol Sci 32, 393–399 (2011). https://doi.org/10.1007/s10072-010-0473-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-010-0473-4