Abstract
The indications for stereotactic radiosurgery are increasing for patients with both intact and resected brain metastases. Radiosurgery in a single fraction may be limited by concern for central nervous system toxicity and inferior local control, particularly for larger lesions. Hypofractionated radiosurgery, over two to five fractions, is frequently used as an alternative treatment that may improve tumor control and adverse event outcomes compared to single-fraction radiosurgery due to size and/or location. In this chapter, we review the rationale and radiobiology of hypofractionated radiosurgery for the treatment of brain metastases. We review the accumulating clinical experience thus far with various hypofractionated radiosurgery regimens and highlight areas of uncertainty and future study.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hypofractionation
- Radiation necrosis
- Brain metastases
- Radiosurgery
- Stereotactic
- Hypofractionated
- Fractionated stereotactic
- Adverse radiation effect
- Cavity
- Postresection
Introduction
Stereotactic radiosurgery (SRS), as defined by the neurosurgery and radiation oncology societies consensus statement [1], is a stereotactic irradiation in one to five fractions. Single-fraction SRS is an effective treatment option for many patients with both intact and resected brain metastases. For patients with large brain metastases who are not candidates for surgery, whole-brain radiotherapy has historically been considered the standard of care. Due to concern for poor local control and neurotoxicity associated with whole-brain radiotherapy, SRS has increasingly been explored for the treatment of these patients. However, clinicians have concern about increased toxicity with single-fraction SRS for larger targets or targets located near or within critical structures or eloquent brain, such as the brainstem, optic pathway, or motor cortex. Hypofractionated SRS over two to five fractions may be an alternative treatment that allows safe delivery of high cumulative doses to lesions suboptimally treated with single-fraction SRS due to size and/or location. There is accumulating clinical evidence showing that hypofractionated SRS can minimize risk to normal brain while maintaining acceptable local control, although the optimal dose and fractionation for this approach have yet to be determined. Other reviews have examined the outcomes of SRS versus hypofractionated SRS for benign and malignant brain tumors [2]; herein, we focus on the role and rationale of hypofractionation for brain metastases.
Limitations of Single-Fraction Radiosurgery
Single-fraction SRS dose is limited by risk of central nervous system toxicity. Adverse radiation effect (ARE), the imaging equivalent of histologically defined brain radiation necrosis, is the most common toxicity that occurs after SRS for tumors in or near the brain and can be associated with neurological deficits that can require management with steroids, bevacizumab, and, in some cases, surgical resection.
Factors that have been found to be correlated with the development of ARE include higher radiation dose , larger tumor volume, and volume of normal brain irradiated [3]. For recurrent, intact, previously irradiated primary brain tumors and brain metastases treated with escalating doses of single-fraction SRS, RTOG 90-05 found that normal brain tissue toxicity was significantly more likely to develop in patients with larger tumors. Compared to tumors smaller than 2 cm in maximum diameter, tumors with maximum diameters of 2–3 cm and 3–4 cm had, respectively, a 7.3 and 16.0 times higher risk of developing irreversible grade 3 or grade 4–5 central nervous system toxicity [3]. In addition to larger volume, increasing dose on this study was also associated with a greater risk of brain toxicity. Others have found that the risk of ARE correlates with the radio surgical volume encompassed by the 10-Gy or 12-Gy isodose line [4]. In a series of 206 patients with a total of 310 brain metastases treated with single-fraction SRS, the actuarial risk of ARE was up to 51% when the volume of receiving a dose of 12 Gy exceeded 10.9 cc [5]. Blonigen et al. similarly showed in a series of 63 patients with a total of 173 brain metastases that the risk of ARE is up to 69% when the volume of peritumoral normal brain receiving 10 and 12 Gy is greater than 14.5 and 10.8 cc, respectively [6].
For resected brain metastasis, the size of the preoperative lesion and volume of normal brain receiving 21 Gy have been found to be associated with incidence of radiation necrosis [7]. Although the addition of a margin around resection cavity improves local control [8], this also increases the volume of normal brain irradiated and, thus, can potentially increase risk of toxicity [9, 10].
In part due to the use of reduced doses to address these concerns for toxicity, larger lesions have been associated with lower control rates after single-fraction SRS. On the basis of the results of RTOG 90-05, the proposed single-fraction SRS doses for lesions with maximum diameter >2 cm, 2.1–3.0 cm, and 3.1–4.0 cm are 24 Gy, 18 Gy, and 15 Gy, respectively [3]. Using these doses, the 1-year local control rate has been reported to be only 49% and 45% for metastases 2.1–3.0 and 3.1–4.0 cm in diameter, respectively, compared with 85% for smaller lesions [11]. Similarly, Hasegawa et al. reported a 49% 1-year local control rate for tumors with a volume greater than 4 cc treated with single-fraction SRS [12]. In 153 brain metastases treated with single-fraction SRS using doses of 20 Gy or more, Chang et al. reported 1-year local control rates of 86% in tumors 1 cm or smaller in size and 56% in tumors greater than 1 cm [13]. A minimum prescribed isodose surface dose of 18 Gy and higher has been found to be associated with local control [14].
Radiobiology and Rationale of Hypofractionation
Hypofractionated SRS may allow the delivery of higher cumulative dose to larger targets while minimizing the risk of toxicity. Fractionation is a central tenet in radiotherapy that leverages the four Rs of classic radiation biology (repair, repopulation, reassortment, and reoxygenation) to expand the therapeutic window. Single-fraction SRS contradicts these conventional radiobiological principles but has been shown to be associated with excellent local control with acceptable toxicity for both metastatic and benign disease. A high level of precision and accuracy is required for delivering high doses of radiation to small targets. Previously, immobilization was achieved by invasively fixing the patient’s head to a frame locked to the treatment couch. However, recent advances in image guidance and robotic-based systems have allowed the evolution of noninvasive, frameless radiosurgery which can facilitate the fractionated delivery of stereotactic radiotherapy with acceptable levels of accuracy [15,16,17]. Furthermore, recent preclinical and clinical studies on the radiobiology of single fraction, high-dose SRS have uncovered mechanisms of radiation different from that of conventionally fractionated radiotherapy. In addition to DNA double-strand breaks, single-fraction high-dose SRS may cause microvascular dysfunction and cell death through endothelial cell inflammation and apoptosis via the sphingomyelin pathway [18, 19]. There is still debate over whether there is a “new biology” beyond the classic radiobiologic paradigm of fractionation or simply higher biological effective dose (BED) that accounts for the efficacy of single-fraction SRS [20].
For malignant tumors, concern exists that single-fraction SRS results in a suboptimal therapeutic ratio between tumor control and late effects. As brain metastases comprise acutely responding neoplastic cells immediately surrounded by late responding normal brain tissue, Hall and Brenner argue that fractionated radiotherapy allows for normal tissue repair/recovery and offers the potential to exploit the different biologic responses and repair mechanisms between neoplastic and normal tissues to irradiation [21, 22]. Additionally, a radioresistant subpopulation of hypoxic cells may survive after single dose of radiation [23], leading to worse tumor control. Allowing for re-oxygenation over multiple fractions may improve tumor control outcomes. Expanding the therapeutic window may not be as important for smaller volumes treated with stereotactic techniques, as there is minimal dose spill outside the target volume. For larger volumes, hypofractionated SRS may offer an approach that leverages the radiobiologic advantages of both high doses per fraction and fractionation. Modeling studies suggest that treatment over 5–10 fractions provides the most gain in normal tissue sparing for fast-growing tumor; the rate of improvement generally levels off at a large (i.e., >10 fractions) number of fractions [24].
Finally, there is emerging evidence that radiation treatment of tumors may have immune-stimulatory effects through immunogenic tumor cell death and enhanced recruitment of antitumor T cells and can be coupled with immunotherapy to improve cancer control outcomes [25, 26]. Diverse radiation regimens have been used in combination with immunotherapy, and recent data suggest that dose fractionation can determine the efficacy of combination treatment. Dewan et al. showed using breast and colon carcinoma models that while a single dose of 20 Gy was as effective as the fractionated regimens of 8 Gy × 3 and 6 Gy × 5 at controlling the growth of the irradiated tumor, only the two fractionated regimens were able to synergize with CTLA-4 blockade to induce antitumor T-cell immunity and inhibit a second palpable tumor outside the radiation field (“abscopal effect”) [27]. It may be that single-fraction SRS damages the vasculature and may impair perfusion and transport of antigens and immune cells [28]. Molecular responses of cells irradiated with fractionated radiation have also been found to differ from single-dose radiation in vitro and in vivo, and they may contribute to the observed differences in effect of fractionated versus single-fraction radiation [29].
Clinical Experience with Hypofractionated SRS
Intact Metastases
Table 10.1 summarizes published studies of hypofractionated SRS for intact brain metastases and overall shows acceptable local control rates with hypofractionated regimens despite the large tumor volumes treated in many of these series. Also, the data suggest equivalent to improved toxicity rates compared to historical outcomes with single-fraction SRS.
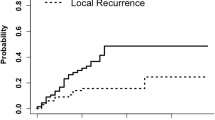
A retrospective study by Minniti et al. of 289 patients with brain metastases with maximum diameters greater than 2 cm showed superior local control using a hypofractionated SRS regimen (9 Gy × 3 fractions) compared to single-fraction SRS, with 1-year local control rates of 90% versus 77%, respectively [45]. Furthermore, there was a lower risk of ARE (9% versus 18%) with hypofractionated SRS. In contrast, Wiggenraad et al. [52] found no difference in the local control rates or toxicity between hypofractionated SRS (8 Gy × 3) and single-fraction SRS (15 Gy) for large (volume >13 cc) brain metastases. Fokas et al. also found no difference in local control between hypofractionated SRS (using either 5 Gy × 7 or 4 Gy × 10) and single-fraction SRS; however, they found that grade 1–3 toxicity was significantly higher with single-fraction SRS (14%) compared with hypofractionated SRS (6% with 5 Gy × 7 and 2% with 4 Gy × 10) [34]. Another series found that 30 Gy in five fractions was associated with better local control than 24 Gy in five fractions (1-year local control 91% vs 75%) [41]. Some series have reported potentially worse local control with hypofractionated SRS for radioresistant histologies, although this may be due to lower BED of the hypofractionated regimens used [47]. These data suggest that hypofractionated regimens are safe but that clinicians should be vigilant to maintain a high BED, equivalent to single-fraction doses, for optimal local control.
While randomized studies comparing hypofractionated SRS over other techniques are lacking, the clinical experience so far suggests that hypofractionated SRS may represent a better treatment option for larger metastatic brain tumors or those in close proximity to eloquent areas such as the brainstem or optic chiasm [44].
Resection Cavities
Surgery alone after resection of brain metastases is inadequate for local control [53,54,55]. Compared to postresection whole-brain radiotherapy, postresection SRS to the resection cavity results in improved cognition with no detriment to overall survival and has now become a standard of care treatment [56]. Numerous studies have reported outcomes of single-fraction SRS to small resection cavities with 1-year local control rates ranging from around 70% to 90% [8, 55, 57, 58]. As with intact lesions treated with SRS, cavities from large preoperative metastases (maximum diameter of 3 cm or greater) are more likely to recur locally after cavity SRS [59]. Increasing cavity volume is also associated with increased toxicity [7, 60]. Delaying SRS does not help reduce target volumes as there is minimal cavity shrinkage seen between the immediate postoperative scan to within a month following resection [61], and delay may be associated with inferior local control [62]. Hypofractionated SRS to the resection cavity has been shown to offer excellent local control rates, even for large brain metastases. Minniti et al. reported 1- and 2-year local control rates of 93% and 84%, respectively, and symptomatic radiation necrosis rate of only 5% with 9 Gy × 3 to the resection cavity [60]. Table 10.2 summarizes published studies of hypofractionated SRS for resected brain metastases.
Optimal Hypofractionated SRS Regimen
The optimal dose and fractionation schedule for hypofractionated SRS remain to be determined. Although the reliability of the linear–quadratic (LQ) model has been questioned for SRS [75], BED based on the LQ model is most widely used clinically to compare the effects of various fractionation schedules. Local control has been associated with peripheral BED10 (using an alpha/beta ratio of 10 for tumor): one series found that the 1-year local control rate was 97% for BED10 greater than 80 Gy versus 90% for BED10 less than 80 Gy [43]. A recently published systematic review of SRS for brain metastases compared the BEDs of different SRS treatment schedules using an alpha/beta value of 12 Gy and found that a BED12 of at least 40 Gy (which corresponds to 25.5 Gy in three fractions or 20 Gy in single fraction) is necessary to obtain a 1-year local control >70% [52]. Similarly, in the postoperative setting, multisession SRS using BED10 ≥48 Gy to the resection cavity has been associated with improved local control. Surgical cavities treated with a BED10 ≥48 Gy (30 Gy in five fractions or 27 Gy in three fractions) had a 1-year local control of 100% compared to 33% for cavities treated with a lower BED10 [69].
Overall treatment time also needs to be explored in the setting of high doses per fraction. Studies in other organ sites have shown improved efficacy, toxicity, and quality of life with every other day dosing [76,77,78]. Radiobiologic studies suggest that the repair halftime for brain necrosis may be relatively long, with the potential of unrepaired damage still present after a 24-hour interval [79]. Reoxygenation may similarly require a longer time interval as hypoxia has been detected in lung tumors at 24–48 hours after a single fraction of radiation to the lung [80]. Increasing the interval of time between radiation fractions by delivering treatment on nonconsecutive days can allow for reassortment of remaining tumor cells into G2-M phase of the cell cycle and improved oxygenation and radiation sensitivity for subsequent fractions, thereby maximizing efficacy of the radiation. There is also time for repair and repopulation of normal cells in between the treatment sessions, thereby minimizing the risk of treatment. For patients with brain metastases not amenable to single-fraction SRS because of location or tumor size, Narayana et al. reported 1-year local control of 70% and steroid dependency in 15% of patients treated with 30 Gy in five fractions at two fractions per week [46]. However, other studies have found no benefit with every other day treatment compared to daily treatment [81].
A further extension of this concept is staged SRS treatment, in which fractions are separated by an even longer interval of at least few weeks. Staged SRS distributes high cumulative doses over time and allows for potentially smaller targets at subsequent treatment sessions. Higuchi et al. published the first report of staged SRS, in which patients with brain metastases of volume larger than 10 cc were treated with a total dose of 30 Gy over three staged fractions separated by 2-week interfraction intervals [35]. Overall tumor shrinkage was observed in 91% of the tumors, with tumor volumes decreasing by 19% and 40% at the second and third sessions. This approach resulted in 1-year local control rates of 76%, with only one patient developing grade 3 toxicity that required surgery. Other series have since been subsequently reported, showing similarly successful treatment of large brain metastases using staged SRS of 20–33 Gy over two sessions with minimal treatment-related morbidity [82,83,84]. Angelov et al. used a 30-day interfraction interval in order to allow for 10 half-lives for repair, assuming the repair half-time for late radiation effects in the brain is as long as 76 hours [79]. In their series of brain metastases greater than 2 cm treated with a median of 30 Gy in two sessions, they reported a 6-month local control rate of 88% and 6% of symptomatic radiation necrosis [83].
Indications for Surgery (Versus Radiosurgery) for Larger Lesions
For larger lesions, hypofractionated SRS has been shown as an effective primary treatment modality for large brain metastases that cannot be resected. While large brain metastases (those measuring greater than 2–3 cm in maximum diameter) are typically treated with resection followed by adjuvant radiation, surgical resection is sometimes not appropriate due to factors such as patients’ performance status and comorbidities or extent of disease. In fact, a secondary analysis of EORTC 22952-26001 found that in patients with one to two brain metastases with a diameter of no greater than 4 cm, SRS was associated with improved early local control compared to surgical resection [85]. However, surgical resection is necessary in the following scenarios:
-
Pathologic proof of metastatic disease is needed.
-
Symptoms of edema/mass effect do not resolve with steroids.
-
Symptoms that resolve with steroids but concern that the patient would be steroid dependent for weeks/months until the tumor shrinks (i.e., surgery would allow for more rapid resolution of edema/mass effect than with SRS alone).
Future Directions and Conclusions
Hypofractionated radiosurgery is a promising strategy for maximizing local control while minimizing toxicity, particularly for larger lesions or lesions in critical locations. While there is a wide range of acceptable fractionation regimens reported in the literature, maintaining a high BED (i.e., BED10 ≥48 Gy, equivalent to 27 Gy in three fractions) is important for optimal local control [52, 69]. Areas of uncertainty include how hypofractionated SRS compares with surgery for the treatment of larger brain metastases and how hypofractionated SRS compares with single-fraction SRS for the treatment of small brain metastases. Additional work is warranted in determining the optimal interfraction time interval and investigating novel approaches such as staged SRS.
Key Points
-
For intact metastases and resection cavities greater than 2 cm in maximum diameter, data suggest improved tumor control and/or treatment-related toxicity with hypofractionated SRS over 2–5 days compared to single-fraction SRS.
-
Maintain high BED equivalent to single-fraction doses for optimal local control with hypofractionation (i.e., BED10 ≥48 Gy, equivalent to 27 Gy in three fractions). Recommended radiosurgery doses for intact brain metastases and resection cavities are listed in Table 10.3.
Case Vignettes
Case 1: Postresection Cavity Hypofractionated SRS due to Size Along with Single-Fraction SRS for Small Intact Metastases
A 59-year-old woman with metastatic ovarian cancer presented with headaches, confusion, and visual disturbance due to a hemorrhagic brain metastasis measuring 4.8 × 4.9 cm in the left parieto-occipital lobe, with trace rim enhancement and surrounding vasogenic edema. She was started on antiseizure medication and steroids, which resulted in complete resolution of her symptoms. She underwent craniotomy for resection the hemorrhagic portion of her metastases followed by radiosurgery treatment 1 week later. On her radiosurgery planning MRI, the left parieto-occipital lesion measured 2.7 × 1.5 cm. Two additional lesions were seen in the left precentral gyrus (7 × 5 mm) and right frontal lobe (2 mm). The left parieto-occipital lesion was treated without margin to 27 Gy in three fractions with dose prescribed to the 72% isodose line (Fig. 10.1a). In a separate plan, the other two lesions were each treated together to 24 Gy in one fraction with dose prescribed to the 72% isodose line (Fig. 10.1b, c). She remains locally controlled at 1 year following radiosurgery, without neurological symptoms.
Postresection cavity hypofractionated SRS due to size along with single-fraction SRS for small intact metastases. (a) Left parieto-occipital lesion (2.7 × 1.5 cm), status postresection of hemorrhagic portion, treated to 27 Gy in three fractions prescribed to the 72% isodose line (green 27 Gy, light blue 13.5 Gy, dark blue 6.75 Gy). (b and c) Left precentral gyrus lesion (7 × 5 mm) and right frontal lobe lesion (2 mm) treated in a separate plan to 24 Gy in one fraction prescribed to the 72% isodose line (green 24 Gy, light blue 12 Gy, dark blue 6 Gy)
Case 2: Postresection Cavity Hypofractionated SRS over 5 Days due to Large Size
A 64-year-old woman with metastatic hormone-positive breast cancer presented with forgetfulness and abnormal behavior and was found to have a large cystic and solid right frontal mass measuring 5.5 cm with associated edema, subfalcine herniation, and midline shift. She underwent a gross total resection which revealed metastatic breast carcinoma. She was not able to undergo adjuvant radiosurgery until 2 months after her resection. At the time of her treatment planning, there was a thick rim of enhancement of the resection cavity margins, concerning for recurrent tumor. She underwent radiosurgery to the resection cavity with 2-mm margin to 25 Gy in five fractions. She developed nodular leptomeningeal progression 3 months following radiosurgery for which she completed whole-brain radiotherapy (Fig. 10.2).
Axial and sagittal views of right frontal resection cavity with 2-mm margin treated with 25 Gy in five fractions prescribed to the 72% isodose line. The preoperative MRI was fused with the postoperative images to aid in contouring the target volume. The preoperative extent rather than entire surgical tract was covered
Case 3: Hypofractionated SRS over 3 Days due to Large Size and Location
A 65-year-old woman with metastatic ovarian carcinoma, previously treated with SRS 6 months ago for four brain metastases, presented with mild diplopia on far lateral gaze. MRI revealed a 2.7 × 2.7 cm metastasis in the pons. She received 24 Gy in three consecutive daily fractions to the 72% isodose line. Follow-up MRI 9 months later revealed continued shrinkage of the tumor with no adverse radiation effect (Fig. 10.3).
Axial and sagittal views of pontine metastasis treated with 24 Gy (green isodose line) in three consecutive daily fractions to the 72% isodose line (a and b). Also shown is the 50% dose line in cyan (12 Gy isodose line). Follow-up MRI 9 months later (c and d) revealed continued shrinkage of the tumor with no adverse radiation effect
References
Barnett GH, Linskey ME, Adler JR, Cozzens JW, Friedman WA, Heilbrun MP, et al. Stereotactic radiosurgery—an organized neurosurgery-sanctioned definition. J Neurosurg. 2007;106(1):1–5.
Kirkpatrick JP, Soltys SG, Lo SS, Beal K, Shrieve DC, Brown PD. The radiosurgery fractionation quandary: single fraction or hypofractionation? Neuro Oncol. 2017;19(suppl_2):ii38–49.
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, et al. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys. 2000;47(2):291–8.
Korytko T, Radivoyevitch T, Colussi V, Wessels BW, Pillai K, Maciunas RJ, et al. 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int J Radiat Oncol Biol Phys. 2006;64(2):419–24.
Minniti G, Clarke E, Lanzetta G, Osti MF, Trasimeni G, Bozzao A, et al. Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol Lond Engl. 2011;6:48.
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC. Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2010;77(4):996–1001.
Doré M, Martin S, Delpon G, Clément K, Campion L, Thillays F. Stereotactic radiotherapy following surgery for brain metastasis: predictive factors for local control and radionecrosis. Cancer Radiother. 2017;21(1):4–9.
Choi CYH, Chang SD, Gibbs IC, Adler JR, Harsh GR, Lieberson RE, et al. Stereotactic radiosurgery of the postoperative resection cavity for brain metastases: prospective evaluation of target margin on tumor control. Int J Radiat Oncol Biol Phys. 2012;84(2):336–42.
Kirkpatrick JP, Wang Z, Sampson JH, McSherry F, Herndon JE, Allen KJ, et al. Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: results of a randomized trial. Int J Radiat Oncol Biol Phys. 2015;91(1):100–8.
Nataf F, Schlienger M, Liu Z, Foulquier JN, Grès B, Orthuon A, et al. Radiosurgery with or without a 2-mm margin for 93 single brain metastases. Int J Radiat Oncol Biol Phys. 2008;70(3):766–72.
Vogelbaum MA, Angelov L, Lee S-Y, Li L, Barnett GH, Suh JH. Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg. 2006;104(6):907–12.
Hasegawa T, Kondziolka D, Flickinger JC, Germanwala A, Lunsford LD. Brain metastases treated with radiosurgery alone: an alternative to whole brain radiotherapy? Neurosurgery. 2003;52(6):1318–26.
Chang EL, Hassenbusch SJ, Shiu AS, Lang FF, Allen PK, Sawaya R, et al. The role of tumor size in the radiosurgical management of patients with ambiguous brain metastases. Neurosurgery. 2003;53(2):272–81.
Shiau C-Y, Sneed PK, Shu H-KG, Lamborn KR, McDermott MW, Chang S, et al. Radiosurgery for brain metastases: relationship of dose and pattern of enhancement to local control. Int J Radiat Oncol Biol Phys. 1997;37(2):375–83.
Adler JR Jr, Chang SD, Murphy MJ, Doty J, Geis P, Hancock SL. The Cyberknife: a frameless robotic system for radiosurgery. Stereotact Funct Neurosurg. 1997;69(1–4):124–8.
Fuss M, Salter BJ, Cheek D, Sadeghi A, Hevezi JM, Herman TS. Repositioning accuracy of a commercially available thermoplastic mask system. Radiother Oncol. 2004;71(3):339–45.
Li G, Ballangrud A, Chan M, Ma R, Beal K, Yamada Y, et al. Clinical experience with two frameless stereotactic radiosurgery (fSRS) systems using optical surface imaging for motion monitoring. J Appl Clin Med Phys. 2015;16(4):149–62.
Paris F, Fuks Z, Kang A, Capodieci P, Juan G, Ehleiter D, et al. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science. 2001;293(5528):293–7.
Ch’ang H-J, Maj JG, Paris F, Xing HR, Zhang J, Truman J-P, et al. ATM regulates target switching to escalating doses of radiation in the intestines. Nat Med. 2005;11(5):484–90.
Brown JM, Koong AC. High-dose single-fraction radiotherapy: exploiting a new biology? Int J Radiat Oncol Biol Phys. 2008;71(2):324–5.
Brenner DJ, Martel MK, Hall EJ. Fractionated regimens for stereotactic radiotherapy of recurrent tumors in the brain. Int J Radiat Oncol Biol Phys. 1991;21(3):819–24.
Hall EJ, Brenner DJ. The radiobiology of radiosurgery: rationale for different treatment regimes for AVMs and malignancies. Int J Radiat Oncol Biol Phys. 1993;25(2):381–5.
Brown JM, Diehn M, Loo BW. Stereotactic ablative radiotherapy should be combined with a hypoxic cell radiosensitizer. Int J Radiat Oncol Biol Phys. 2010;78(2):323–7.
Ma L, Sahgal A, Descovich M, Cho Y-B, Chuang C, Huang K, et al. Equivalence in dose fall-off for isocentric and nonisocentric intracranial treatment modalities and its impact on dose fractionation schemes. Int J Radiat Oncol Biol Phys. 2010;76(3):943–8.
Demaria S, Golden EB, Formenti SC. Role of local radiation therapy in cancer immunotherapy. JAMA Oncol. 2015;1(9):1325.
Demaria S, Bhardwaj N, McBride WH, Formenti SC. Combining radiotherapy and immunotherapy: a revived partnership. Int J Radiat Oncol Biol Phys. 2005;63(3):655–66.
Dewan MZ, Galloway AE, Kawashima N, Dewyngaert JK, Babb JS, Formenti SC, et al. Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody. Clin Cancer Res. 2009;15(17):5379–88.
Park HJ, Griffin RJ, Hui S, Levitt SH, Song CW. Radiation-induced vascular damage in tumors: implications of vascular damage in ablative hypofractionated radiotherapy (SBRT and SRS). Radiat Res. 2012;177(3):311–27.
Tsai M-H, Cook JA, Chandramouli GVR, DeGraff W, Yan H, Zhao S, et al. Gene expression profiling of breast, prostate, and glioma cells following single versus fractionated doses of radiation. Cancer Res. 2007;67(8):3845–52.
Aoki M, Abe Y, Hatayama Y, Kondo H, Basaki K. Clinical outcome of hypofractionated conventional conformation radiotherapy for patients with single and no more than three metastatic brain tumors, with noninvasive fixation of the skull without whole brain irradiation. Int J Radiat Oncol Biol Phys. 2006;64(2):414–8.
Aoyama H, Shirato H, Onimaru R, Kagei K, Ikeda J, Ishii N, et al. Hypofractionated stereotactic radiotherapy alone without whole-brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys. 2003;56(3):793–800.
Ernst-Stecken A, Ganslandt O, Lambrecht U, Sauer R, Grabenbauer G. Phase II trial of hypofractionated stereotactic radiotherapy for brain metastases: results and toxicity. Radiother Oncol. 2006;81(1):18–24.
Fahrig A, Ganslandt O, Lambrecht U, Grabenbauer G, Kleinert G, Sauer R, et al. Hypofractionated stereotactic radiotherapy for brain metastases: results from three different dose concepts. Strahlenther Onkol. 2007;183(11):625–30.
Fokas E, Henzel M, Surber G, Kleinert G, Hamm K, Engenhart-Cabillic R. Stereotactic radiosurgery and fractionated stereotactic radiotherapy: comparison of efficacy and toxicity in 260 patients with brain metastases. J Neuro-Oncol. 2012;109(1):91–8.
Higuchi Y, Serizawa T, Nagano O, Matsuda S, Ono J, Sato M, et al. Three-staged stereotactic radiotherapy without whole brain irradiation for large metastatic brain tumors. Int J Radiat Oncol Biol Phys. 2009;74(5):1543–8.
Kim Y-J, Cho KH, Kim J-Y, Lim YK, Min HS, Lee SH, et al. Single-dose versus fractionated stereotactic radiotherapy for brain metastases. Int J Radiat Oncol Biol Phys. 2011;81(2):483–9.
Kwon AK, DiBiase SJ, Wang B, Hughes SL, Milcarek B, Zhu Y. Hypofractionated stereotactic radiotherapy for the treatment of brain metastases. Cancer. 2009;115(4):890–8.
Lindvall P, Bergström P, Löfroth P-O, Tommy Bergenheim A. A comparison between surgical resection in combination with WBRT or hypofractionated stereotactic irradiation in the treatment of solitary brain metastases. Acta Neurochir. 2009;151(9):1053–9.
Lockney NA, Wang DG, Gutin PH, Brennan C, Tabar V, Ballangrud A, et al. Clinical outcomes of patients with limited brain metastases treated with hypofractionated (5 × 6 Gy) conformal radiotherapy. Radiother Oncol. 2017;123(2):203–8.
Manning MA, Cardinale RM, Benedict SH, Kavanagh BD, Zwicker RD, Amir C, et al. Hypofractionated stereotactic radiotherapy as an alternative to radiosurgery for the treatment of patients with brain metastases. Int J Radiat Oncol Biol Phys. 2000;47(3):603–8.
Marcrom SR, McDonald AM, Thompson JW, Popple RA, Riley KO, Markert JM, et al. Fractionated stereotactic radiation therapy for intact brain metastases. Adv Radiat Oncol. 2017;2(4):564–71.
Märtens B, Janssen S, Werner M, Frühauf J, Christiansen H, Bremer M, et al. Hypofractionated stereotactic radiotherapy of limited brain metastases: a single-centre individualized treatment approach. BMC Cancer. 2012;12:497.
Matsuyama T, Kogo K, Oya N. Clinical outcomes of biological effective dose-based fractionated stereotactic radiation therapy for metastatic brain tumors from non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2013;85(4):984–90.
Minniti G, D’Angelillo RM, Scaringi C, Trodella LE, Clarke E, Matteucci P, et al. Fractionated stereotactic radiosurgery for patients with brain metastases. J Neuro-Oncol. 2014;117(2):295–301.
Minniti G, Scaringi C, Paolini S, Lanzetta G, Romano A, Cicone F, et al. Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (>2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys. 2016;95(4):1142–8.
Narayana A, Chang J, Yenice K, Chan K, Lymberis S, Brennan C, et al. Hypofractionated stereotactic radiotherapy using intensity-modulated radiotherapy in patients with one or two brain metastases. Stereotact Funct Neurosurg. 2007;85(2–3):82–7.
Oermann EK, Kress M-AS, Todd JV, Collins BT, Hoffman R, Chaudhry H, et al. The impact of radiosurgery fractionation and tumor radiobiology on the local control of brain metastases: clinical article. J Neurosurg. 2013;119(5):1131–8.
Ogura K, Mizowaki T, Ogura M, Sakanaka K, Arakawa Y, Miyamoto S, et al. Outcomes of hypofractionated stereotactic radiotherapy for metastatic brain tumors with high risk factors. J Neuro-Oncol. 2012;109(2):425–32.
Rajakesari S, Arvold ND, Jimenez RB, Christianson LW, Horvath MC, Claus EB, et al. Local control after fractionated stereotactic radiation therapy for brain metastases. J Neuro-Oncol. 2014;120(2):339–46.
Saitoh J, Saito Y, Kazumoto T, Kudo S, Ichikawa A, Hayase N, et al. Therapeutic effect of Linac-based stereotactic radiotherapy with a micro-multileaf collimator for the treatment of patients with brain metastases from lung cancer. Jpn J Clin Oncol. 2010;40(2):119–24.
Tokuuye K, Akine Y, Sumi M, Kagami Y, Murayama S, Nakayama H, et al. Fractionated stereotactic radiotherapy of small intracranial malignancies. Int J Radiat Oncol Biol Phys. 1998;42(5):989–94.
Wiggenraad R, Kanter AV, Kal HB, Taphoorn M, Vissers T, Struikmans H. Dose-effect relation in stereotactic radiotherapy for brain metastases. A systematic review. Radiother Oncol. 2011;98(3):292–7.
Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998;280(17):1485–9.
Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011;29(2):134–41.
Mahajan A, Ahmed S, McAleer MF, Weinberg JS, Li J, Brown P, et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18(8):1040–8.
Brown PD, Ballman KV, Cerhan JH, Anderson SK, Carrero XW, Whitton AC, et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18(8):1049–60.
Soltys SG, Adler JR, Lipani JD, Jackson PS, Choi CYH, Puataweepong P, et al. Stereotactic radiosurgery of the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys. 2008;70(1):187–93.
Brennan C, Yang TJ, Hilden P, Zhang Z, Chan K, Yamada Y, et al. A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys. 2014;88(1):130–6.
Ojerholm E, Miller D, Geiger GA, Lustig RA. Stereotactic radiosurgery to the resection bed for intracranial metastases and risk of leptomeningeal carcinomatosis. J Neurosurg. 2014;121:9.
Minniti G, Esposito V, Clarke E, Scaringi C, Lanzetta G, Salvati M, et al. Multidose stereotactic radiosurgery (9 Gy × 3) of the postoperative resection cavity for treatment of large brain metastases. Int J Radiat Oncol Biol Phys. 2013;86(4):623–9.
Atalar B, Choi CYH, Harsh GR, Chang SD, Gibbs IC, Adler JR, et al. Cavity volume dynamics after resection of brain metastases and timing of postresection cavity stereotactic radiosurgery. Neurosurgery. 2013;72(2):180–5.
Iorio-Morin C, Ezahr Y. Early Gamma Knife stereotactic radiosurgery to the tumor bed of resected brain metastasis for improved local control. J Neurosurg. 2014;121:6.
Abuodeh Y, Ahmed KA, Naghavi AO, Venkat PS, Sarangkasiri S, Johnstone PAS, et al. Postoperative stereotactic radiosurgery using 5-Gy × 5 sessions in the management of brain metastases. World Neurosurg. 2016;90:58–65.
Ahmed KA, Freilich JM, Abuodeh Y, Figura N, Patel N, Sarangkasiri S, et al. Fractionated stereotactic radiotherapy to the post-operative cavity for radioresistant and radiosensitive brain metastases. J Neuro-Oncol. 2014;118(1):179–86.
Ammirati M, Kshettry VR, Lamki T, Wei L, Grecula JC. A prospective phase II trial of fractionated stereotactic intensity modulated radiotherapy with or without surgery in the treatment of patients with 1 to 3 newly diagnosed symptomatic brain metastases. Neurosurgery. 2014;74(6):586–94.
Connolly EP, Mathew M, Tam M, King JV, Kunnakkat SD, Parker EC, et al. Involved field radiation therapy after surgical resection of solitary brain metastases—mature results. Neuro Oncol. 2013;15(5):589–94.
Do L, Pezner R, Radany E, Liu A, Staud C, Badie B. Resection followed by stereotactic radiosurgery to resection cavity for intracranial metastases. Int J Radiat Oncol Biol Phys. 2009;73(2):486–91.
Keller A, Doré M, Cebula H, Thillays F, Proust F, Darié I, et al. Hypofractionated stereotactic radiation therapy to the resection bed for intracranial metastases. Int J Radiat Oncol Biol Phys. 2017;99(5):1179–89.
Kumar AMS, Miller J, Hoffer SA, Mansur DB, Coffey M, Lo SS, et al. Postoperative hypofractionated stereotactic brain radiation (HSRT) for resected brain metastases: improved local control with higher BED10. J Neuro-Oncol. 2018;139(2):449–54.
Ling DC, Vargo JA, Wegner RE, Flickinger JC, Burton SA, Engh J, et al. Postoperative stereotactic radiosurgery to the resection cavity for large brain metastases: clinical outcomes, predictors of intracranial failure, and implications for optimal patient selection. Neurosurgery. 2015;76(2):150–7.
Pessina F, Navarria P, Cozzi L, Ascolese AM, Maggi G, Riva M, et al. Outcome evaluation of oligometastatic patients treated with surgical resection followed by hypofractionated stereotactic radiosurgery (HSRS) on the tumor bed, for single, large brain metastases. Sherman JH, editor. PLoS One. 2016;11(6):e0157869.
Steinmann D, Maertens B, Janssen S, Werner M, Frühauf J, Nakamura M, et al. Hypofractionated stereotactic radiotherapy (hfSRT) after tumour resection of a single brain metastasis: report of a single-centre individualized treatment approach. J Cancer Res Clin Oncol. 2012;138(9):1523–9.
Vogel J, Ojerholm E, Hollander A, Briola C, Mooij R, Bieda M, et al. Intracranial control after Cyberknife radiosurgery to the resection bed for large brain metastases. Radiat Oncol. 2015;10(1):221. Available from: http://www.ro-journal.com/content/10/1/221.
Wang C-C, Floyd SR, Chang C-H, Warnke PC, Chio C-C, Kasper EM, et al. Cyberknife hypofractionated stereotactic radiosurgery (HSRS) of resection cavity after excision of large cerebral metastasis: efficacy and safety of an 800 cGy × 3 daily fractions regimen. J Neurooncol. 2012;106(3):601–10.
Park C, Papiez L, Zhang S, Story M, Timmerman RD. Universal survival curve and single fraction equivalent dose: useful tools in understanding potency of ablative radiotherapy. Int J Radiat Oncol Biol Phys. 2008;70(3):847–52.
Quon HC, Ong A, Cheung P, Chu W, Chung HT, Vesprini D, et al. Once-weekly versus every-other-day stereotactic body radiotherapy in patients with prostate cancer (PATRIOT): a phase 2 randomized trial. Radiother Oncol. 2018;127(2):206–12.
Alite F, Stang K, Balasubramanian N, Adams W, Shaikh MP, Small C, et al. Local control dependence on consecutive vs. nonconsecutive fractionation in lung stereotactic body radiation therapy. Radiother Oncol. 2016;121(1):9–14.
Jain S, Poon I, Soliman H, Keller B, Kim A, Lochray F, et al. Lung stereotactic body radiation therapy (SBRT) delivered over 4 or 11 days: a comparison of acute toxicity and quality of life. Radiother Oncol. 2013;108(2):320–5.
Bender ET. Brain necrosis after fractionated radiation therapy: is the halftime for repair longer than we thought? Med Phys. 2012;39(11):7055–61.
Kelada OJ, Decker RH, Nath SK, Johung KL, Zheng M-Q, Huang Y, et al. High single doses of radiation may induce elevated levels of hypoxia in early-stage non-small cell lung cancer tumors. Int J Radiat Oncol Biol Phys. 2018;102(1):174–83.
Samson P, Rehman S, Juloori A, DeWees T, Roach M, Bradley J, et al. Local control for clinical stage I non-small cell lung cancer treated with 5-fraction stereotactic body radiation therapy is not associated with treatment schedule. Pract Radiat Oncol. 2018;8(6):404–13.
Yomo S, Hayashi M, Nicholson C. A prospective pilot study of two-session Gamma Knife surgery for large metastatic brain tumors. J Neuro-Oncol. 2012;109(1):159–65.
Angelov L, Mohammadi AM, Bennett EE, Abbassy M, Elson P, Chao ST, et al. Impact of 2-staged stereotactic radiosurgery for treatment of brain metastases ≥ 2 cm. J Neurosurg. 2018;129:366–82.
Yomo S, Hayashi M. A minimally invasive treatment option for large metastatic brain tumors: long-term results of two-session Gamma Knife stereotactic radiosurgery. Radiat Oncol Lond Engl. 2014;9:132.
Churilla TM, Chowdhury IH, Handorf E, Collette L, Collette S, Dong Y, et al. Comparison of local control of brain metastases with stereotactic radiosurgery vs surgical resection: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2019;5(2):243–7. Available from: https://jamanetwork.com/journals/jamaoncology/fullarticle/2713842.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pollom, E.L., Shi, S., Soltys, S.G. (2020). Hypofractionated Stereotactic Radiosurgery for Intact and Resected Brain Metastases. In: Yamada, Y., Chang, E., Fiveash, J., Knisely, J. (eds) Radiotherapy in Managing Brain Metastases. Springer, Cham. https://doi.org/10.1007/978-3-030-43740-4_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-43740-4_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43739-8
Online ISBN: 978-3-030-43740-4
eBook Packages: MedicineMedicine (R0)