Abstract
Although Paget’s disease of bone (PDB) is common in western countries, it is extremely rare in Asian ones including Japan. Recently, oral risedronate (17.5 mg once daily) was approved in Japan as a treatment of PDB besides calcitonin and etidronate. However, there are few data regarding the efficacy of this agent, dose for patients with PDB in Japan, or the durability of its effect. The purpose of this study was to evaluate the midterm outcome of oral risedronate (17.5 mg once daily) for patients with PDB in Japan. Seventeen patients with PDB were treated with risedronate (17.5 mg once daily) for 8 weeks. Efficacy and its durability were accessed based on serum total alkaline phosphatase (ALP) and symptoms. Risedronate effectively suppressed bone turnover evaluated with serum total ALP in all patients. In 8 of 10 patients with bone pain, risedronate reduced the pain. On the other hand, tinnitus and hearing loss did not disappear but somewhat improved. None of the patients suffered severe complications. Seven of 17 patients required readministration of oral bisphosphonate (risedronate, six; alendronate, one) due to elevated total ALP at 27 months (mean ranging from 9 to 39 months) after the initial administration of risedronate. Treatment of oral risedronate (17.5 mg once daily) for 8 weeks is safe and effective for patients with PDB in Japan. However, the durability of its effect is limited in some patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paget’s disease of bone (PDB) is characterized by a focal disorder of bone remodeling, bone hypertrophy, and abnormal bone structure [1]. There are great ethnic and geographical differences in its prevalence. Western and southern parts of Europe show a high prevalence of PDB [2]. Conversely, this disease is rare in Scandinavia, China, Japan, and countries in southeast Asia [3, 4].
Although the first effective treatment (calcitonin) was developed in the 1970s [5], bisphosphonate therapy is now the most commonly used treatment for PDB, normalizing biochemical markers of bone resorption and formation. The new potent bisphosphonates, such as alendronate and risedronate, have been developed for oral use. Given their much greater potency and duration of action, there is little justification for use of less effective earlier bisphosphonates such as etidronate or calcitonin [6, 7].
In Japan, until 2007, only etidronate and calcitonin were approved for the treatment of patients with PDB. However, from 2006 to 2007, a phase III, multicenter, noncomparative, clinical trial of oral risedronate (17.5 mg once daily for 8 weeks) was conducted. Due to the rarity of this disease, only 11 patients were enrolled and the efficacy was evaluated [8]. The results led to oral risedronate being approved for use in patients with PDB in Japan. However, the efficacy of oral risedronate was evaluated for only 48 weeks after administration in this clinical trial, and its durability in Japanese patients has not been clarified. In this study, we administered risedronate (17.5 mg once daily for 8 weeks) to 17 patients (pretreated with other agents or nontreated) with Paget’s disease of bone consecutively and prospectively, which is the largest such study ever conducted in Japan due to the rarity of the disease in this country. The efficacy and durability of the effect of risedronate in this population were analyzed.
Materials and methods
A phase III, multicenter, noncomparative, open-label study of risedronate (17.5 mg once daily for 8 weeks) was conducted between April 2006 and October 2007. The results of this clinical trial with a 40-week post-treatment follow-up period have been reported previously [8]. Two patients enrolled in this previous clinical trial were included in the current study. After approval of risedronate as a pharmaceutical therapeutic agent for PDB in Japan, other 15 patients with PDB were prospectively and consecutively treated with risedronate (17.5 mg once daily for 8 weeks) from August 2008 to June 2011 in three affiliated centers. A total of 17 patients were enrolled in the current study, 12 of whom had been treated in the past for PDB. Patients were not required to have increased activity of serum ALP. Four of 17 patients showed ALP levels in the normal range at the beginning of risedronate treatment after antecedent treatment.
PDB was diagnosed by typical x-ray findings [9]. In some cases, lesions were evaluated with computed tomography and/or magnetic resonance imaging. Bone scintigraphy was conducted to differentiate monostotic and polyostotic involvement.
After at least 4 weeks of washout period after previous treatment for PDB, patients were treated with 17.5 mg of oral risedronate, once daily for 8 weeks. Serum ALP activity was evaluated at every 4 weeks from the administration of risedronate until 12 weeks, and every 3 months thereafter. The criterion of risedronate readministration was based on the serum ALP value, which was above the upper limit of normal at two consecutive measurements. In case the initial serum ALP value was very high before risedronate treatment, risedronate was not readministered for the patient with the value above the upper limit during decrease of the ALP. When the ALP activity was elevated again, readministration was performed.
The primary endpoint was the changes in total ALP. Positive response was defined as normalization of serum ALP activity or a reduction of at least 75 % of the ALP value above the upper limit of normal. The second endpoint was the mitigation of symptoms attributed to PDB, such as bone pain, arthritic pain, and tinnitus/hearing loss. The third endpoint was readministration of risedronate due to elevation of serum total ALP and/or worsening of symptoms. Adverse events were recorded throughout the follow-up period. The study was approved by the ethics committee of our institution.
Numerical data were summarized as mean and standard deviation (SD). Categorical data (gender, monostotic vs polyostotic, with or without antecedent treatment) were compared by the chi-square test or Fisher’s exact tests. The difference between the values at baseline and post-treatment in the same patient was examined by paired Student’s t test for paired samples. We determined differences between the readministration of risedronate (+) group and (−) group in nonnormally distributed data (age, duration from risedronate treatment to the latest follow-up) using the Mann–Whitney U test. Results were considered as significant for P < 0.05. All analyses were performed using SPSS 17.0 for Windows software.
Results
Since 1994, a total of 25 patients were diagnosed with PDB by X-ray examination and/or bone biopsy. Seventeen of them were treated with 17.5 mg of risedronate once daily for 8 weeks. Nine of them were male, and eight were female, with a mean age of 61 ± 12 years (range, 44–81 years). Mean follow-up duration after the treatment with risedronate was 32 ± 15 months (range, 4–65 months) (Table 1). All of the patients were Japanese. There was no family history of PDB in this cohort. Nine showed monostotic involvement and eight, polyostotic. The pelvic bone was involved in 10 patients, femur in 7, skull in 6, humerus in 4, spine in 2, and other sites in one each. Ten patients suffered bone and/or arthritic pain, and two had hearing loss and tinnitus. Four patients underwent bone biopsy to confirm the histological diagnosis. Twelve patients were pharmaceutically treated in advance of the treatment with risedronate, including calcitonin in 5, etidronate in 10, alendronate in 6, and 2.5 mg of risedronate in 3. Total ALP concentration at presentation to our institutions was 1,147 ± 1,106 IU/L (range, 401–4,319; normal range, 115–359), and that at the beginning of treatment with 17.5 mg of risedronate was 799 ± 877 IU/L (range, 190–4,031). Serum ALP concentration was normalized in 4 (24 %) of 17 patients with antecedent drugs, 2 patients with alendronate, 1 with etidronate, and 1 with 2.5 mg risedronate daily.
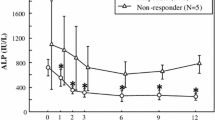
Oral risedronate effectively reduced the serum ALP concentration in a time-dependent manner (Table 2). Because of slight differences in the normal range of serum total ALP values among the three institutions, percent changes from the beginning of risedronate treatment in total ALP were shown in Fig. 1. Total ALP concentration was elevated by above 100 % in two cases, although ALP activity in these cases was well controlled in advance of risedronate treatment with preceding alendronate administration. At 12 weeks, 11 (65 %) of 17 patients had a normal ALP concentration. Three patients had a reduction of at least 75 % in the ALP excess. Response rate at 12 weeks was 82 %. In 8 (80 %) of 10 patients with bone and/or arthritic pain, the symptoms disappeared with treatment of risedronate by no later than 12 weeks. Of note, persistent pain in two patients seemed to originate from arthritic pain of the hip and lateral bowing of the femur in one each. Bone pain itself was thought to be improved with risedronate treatment. Clinical symptoms did not worsen in any case even when the serum ALP value was elevated again. The hearing loss and/or tinnitus in two patients did not disappear, but improved slightly.
There were no severe adverse effects associated with risedronate use. One patient had transient hypocalcemia at 8 weeks, which returned to normal at 10 weeks. Another complained of mild nausea in the early phase of risedronate administration, which soon resolved.
After using a potent bisphosphonate, it is crucial to clarify the duration of the effects. Of 17 patients treated with risedronate (17.5 mg, daily), 6 required readministration of risedronate, and 1 was treated with alendronate due to an elevated serum ALP concentration. Excluding cases in which serum ALP concentration was normalized (four patients) with antecedent drugs, daily risedronate (17.5 mg) treatment could stabilize ALP level until 48 weeks in all cases; however, ALP level of one case increased at 72 weeks. Patients were divided into two groups: with or without readministration of bisphosphonate. Factors associated with the readministration were analyzed. Long duration from the administration of risedronate to the latest follow-up was significantly associated (P = 0.043; readministration (+), 42 ± 14 months; readministration (−), 25 ± 14 months) with the necessity of readministration. Existence of antecedent treatment was correlated with the requirement of readministration (P = 0.044, Table 3). Age, gender, location of lesions, and monostotic or polyostotic involvement were not correlated with the necessity of readministration.
Discussion
This prospective study revealed the midterm outcome of oral risedronate administration to patients with PDB in the central part of Japan. A previous phase III clinical trial for 11 patients in Japan demonstrated the efficacy of this drug in regulating several biochemical markers, including serum ALP, bone-specific ALP, urinary deoxypyridinoline, and urinary cross-linked N-telopeptide of type I collagen. Risedronate also reduced symptoms, particularly bone pain. However, improvement of biomarkers was accessed for 48 weeks, namely less than 1 year [8]. The durability of the effect of this agent has not been clarified in patients in Japan at a dose of 17.5 mg daily. In western countries, risedronate proved to be a highly effective therapy superior to alendronate in that a 30-mg daily dose for only 2 months produced a similar suppression of disease activity as 6 months of alendronate. The suppression of bone turnover by risedronate persisted for about 1 year [10]. Considering the difference in stature and pharmacokinetics between westerners and Japanese, evaluation of the midterm outcome of this agent (17.5 mg once daily for 8 weeks) should provide useful information for clinical practice in Japan and other Asian countries. Duration of the effectiveness of this agent is the dominant focus of this study as compared with the previous study [8].
Risedronate treatment effectively reduced serum ALP concentrations in the current study. A previous Japanese study analyzed various biomarkers of bone turnover [8]. Specialized markers of bone turnover other than ALP are marginally more sensitive, although costs are greater, but no evidence suggests that specialized markers offer any major clinical benefit over total ALP [11]. In clinical practice, total ALP concentration is sufficient to evaluate the efficacy of drugs. Paget disease is associated with a variety of symptoms [12]. Other than bone or arthritic pain, in patients with skull involvement, hearing loss is the most common complication [13], but tinnitus might also occur [14]. Symptoms of PDB were well suppressed by risedronate treatment, particularly bone and/or arthritic pain. Although hearing loss and/or tinnitus did not disappear, they were alleviated with risedronate.
The necessity for readministration was determined by the elevation of serum ALP activity. A total of seven patients required reexposure to risedronate or alendronate. None of these seven patients complained of worsened bone and/or arthritic pain at the time of serum ALP elevation, although the pain might recur without reexposure to risedronate due to the elevated serum ALP activity. Two factors are statistically correlated with the need for readministration, prior treatment (calcitonin, etidronate, alendronate) and duration from the administration of risedronate treatment. The reasons why antecedent drugs have an adverse impact on risedronate efficacy are obscure. One possible explanation is that the earlier bisphosphonate administration may not have sufficiently suppressed the abnormal bone turnover in PDB, despite which residual old bisphosphonate might be enough to interfere with the action of 17.5 mg of risedronate in bone. One of the most important findings in the current study is the latter factor, namely that long duration from risedronate treatment was significantly associated with the requirement for readministration of bisphosphonate. On the other hand, according to the results of the current study that 17.5mg risedronate (daily) treatment could stabilize ALP level until 48 weeks in all cases, routine measurement of ALP level will not be necessary from the beginning of risedronate treatment to 48 weeks. Sites of involvement, monostotic or polyostotic status, age, and gender did not influence the duration of effectiveness. Clinicians that see patients with PDB in Japan should know information regarding the durability of this agent.
In the current study, the necessity for readministration was determined based on the serum ALP concentration, not on the symptoms. The possibility of giving prophylactic treatment to prevent complications is of interest. However, the evidence base is virtually nonexistent, as recent clinical guidelines have emphasized [9]. Considering that strict control of rheumatoid arthritis improves functional impairment compared with conventional therapy [15], such a study would shed light on the possibility of novel potent bisphosphonates for control of ALP concentration as disease activity, leading to clinical benefit for patients with PDB.
A limitation of the current study was the small number of cases enrolled. However, the number of patients comprising this study was higher than that of the previous phase III clinical trial in Japan [8]. Long-term outcome in future studies may provide different information from that of this study. Moreover, the effects of a more potent intravenous bisphosphonate, zoledronate, should be examined for patients with PDB in Japan as well as denosumab, an inhibitor of receptor activator for nuclear factor—kB (RANK) ligand. In a randomized, double-blind clinical trial of treatment for PDB, a single 15-min infusion of 5 mg zoledronate was compared with standard oral risedronate treatment of 30 mg daily for 2 months. The results demonstrated the superiority of zoledronate over risedronate [6], and the efficacy was also confirmed by a follow-up study [16]. However, under the present condition in Japan, zoledronate and denosumab have not been approved for use in patients with PDB. Possible use of these agents should be evaluated in the future.
In conclusion, 17 consecutive patients with PDB were prospectively treated with oral risedronate (17.5 mg once daily for 8 weeks) in the central part of Japan. Risedronate effectively reduced the serum ALP concentration and symptoms, particularly bone and/or arthritic pain. Longer duration from risedronate treatment may diminish its effects, and reexposure is justified.
References
Siris ES (1998) Paget’s disease of bone. J Bone Miner Res 13(7):1061–1065. doi:10.1359/jbmr.1998.13.7.1061
Detheridge FM, Guyer PB, Barker DJ (1982) European distribution of Paget’s disease of bone. Br Med J (Clin Res Ed) 285(6347):1005–1008
Joshi SR, Ambhore S, Butala N, Patwardhan M, Kulkarni M, Pai B, Karne R (2006) Paget’s disease from Western India. J Assoc Phys India 54:535–538
Takata S, Hashimoto J, Nakatsuka K, Yoshimura N, Yoh K, Ohno I, Yabe H, Abe S, Fukunaga M, Terada M, Zamma M, Ralston SH, Morii H, Yoshikawa H (2006) Guidelines for diagnosis and management of Paget’s disease of bone in Japan. J Bone Miner Metab 24(5):359–367. doi:10.1007/s00774-006-0696-x
Sturtridge WC, Harrison JE, Wilson DR (1977) Long-term treatment of Paget’s disease of bone with salmon calcitonin. Can Med Assoc J 117(9):1031–1034
Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, Mesenbrink P, Su G, Pak J, Zelenakas K, Luchi M, Richardson P, Hosking D (2005) Comparison of a single infusion of zoledronic acid with risedronate for Paget’s disease. N Engl J Med 353(9):898–908. doi:10.1056/NEJMoa044241
Reid IR, Nicholson GC, Weinstein RS, Hosking DJ, Cundy T, Kotowicz MA, Murphy WA Jr, Yeap S, Dufresne S, Lombardi A, Musliner TA, Thompson DE, Yates AJ (1996) Biochemical and radiologic improvement in Paget’s disease of bone treated with alendronate: a randomized, placebo-controlled trial. Am J Med 101(4):341–348
Yoh K, Takata S, Yoshimura N, Hashimoto J (2010) Efficacy, tolerability, and safety of risedronate in Japanese patients with Paget’s disease of bone. J Bone Miner Metab 28(4):468–476. doi:10.1007/s00774-009-0152-9
Selby PL, Davie MW, Ralston SH, Stone MD (2002) Guidelines on the management of Paget’s disease of bone. Bone 31(3):366–373
Siris ES, Chines AA, Altman RD, Brown JP, Johnston CC Jr, Lang R, McClung MR, Mallette LE, Miller PD, Ryan WG, Singer FR, Tucci JR, Eusebio RA, Bekker PJ (1998) Risedronate in the treatment of Paget’s disease of bone: an open label, multicenter study. J Bone Miner Res 13(6):1032–1038. doi:10.1359/jbmr.1998.13.6.1032
Reid IR, Davidson JS, Wattie D, Wu F, Lucas J, Gamble GD, Rutland MD, Cundy T (2004) Comparative responses of bone turnover markers to bisphosphonate therapy in Paget’s disease of bone. Bone 35(1):224–230. doi:10.1016/j.bone.2004.03.023
Cundy T, Bolland M (2008) Paget disease of bone. Trends Endocrinol Metab 19(7):246–253. doi:10.1016/j.tem.2008.06.001
Wermers RA, Tiegs RD, Atkinson EJ, Achenbach SJ, Melton LJ 3rd (2008) Morbidity and mortality associated with Paget’s disease of bone: a population-based study. J Bone Miner Res 23(6):819–825. doi:10.1359/jbmr.080215
Mackenzie I, Young C, Fraser WD (2006) Tinnitus and Paget’s disease of bone. J Laryngol Otol 120(11):899–902. doi:10.1017/S0022215106002519
Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R, Kincaid W, Porter D (2004) Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet 364(9430):263–269. doi:10.1016/S0140-6736(04)16676-2
Hosking D, Lyles K, Brown JP, Fraser WD, Miller P, Curiel MD, Devogelaer JP, Hooper M, Su G, Zelenakas K, Pak J, Fashola T, Saidi Y, Eriksen EF, Reid IR (2007) Long-term control of bone turnover in Paget’s disease with zoledronic acid and risedronate. J Bone Miner Res 22(1):142–148. doi:10.1359/jbmr.061001
Acknowledgments
This work was supported in part by the Suzuken Memorial Foundation and by the Ministry of Education, Culture, Sports, Science and Technology of Japan [Grant-in-Aid 20591751 for Scientific Research (C)].
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishida, Y., Yamada, Y., Tsukushi, S. et al. Midterm outcome of risedronate therapy for patients with Paget’s disease of bone in the central part of Japan. Clin Rheumatol 32, 241–245 (2013). https://doi.org/10.1007/s10067-012-2109-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2109-y