Abstract
Purpose
Bisphosphonates are the mainstay of the treatment of Paget’s disease of bone (PDB). Clinical practice guidelines recommend treatment with intravenous zoledronic acid or high-dose oral nitrogen bisphosphonates (N-BPs). We present our long-term experience treating PDB patients with lower than recommended oral doses of N-BPs, equivalent to once-weekly doses used for treating osteoporosis.
Methods
PDB patients were seen, between 1990 and 2015 at the endocrine clinic of an academic medical center. Diagnosis was established according to accepted criteria. Patients were initially treated with alendronate 70 mg/week or risedronate 35 mg/week. Whenever the initial dose failed to produce remission, the dosage was increased to twice a week the respective dose.
Results
Patients were followed for a mean of 11.9 years (range: 1.7–24.8). Out of 96 treatment courses with N-BPs, 89% were with alendronate and 11% with risedronate. Remission was achieved in 84% of the courses with alendronate 70 mg/week. 90% of those who did not achieve remission subsequently responded to 140 mg/week. Out of the 8 treatment courses with risedronate 35 mg/week, 87% achieved remission, and the 2 patients who did not achieve remission subsequently responded to 70 mg/week. The median duration of remissions following 3-4 months courses of alendronate 70 mg/week or risedronate 35 mg/week was 8.8 months (IQR: 5.5, 14.8).
Conclusion
In a large proportion of “real world” PDB patients, remission can be achieved with once-weekly, “osteoporosis doses” of alendronate or risedronate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paget’s disease of bone (PDB) is a focal, disorder of bone remodeling consisting of increased bone resorption by abnormal osteoclasts, resulting in disorganized bone formation at affected skeletal sites. The disease is characterized by distinct radiographic and scintigraphic features and increased levels of bone turnover markers, particularly serum alkaline phosphatase (AP), which is the most readily available, and most commonly used, marker for determining PDB activity [1,2,3]. Clinical presentation varies from asymptomatic disease to localized bone pain, deformed long bones, which may lead to secondary osteoarthritis and nerve-root compression adjacent to affected bone. Hyperuricemia, hypercalcemia, high-output heart failure, and sarcomatous transformation may also occur [1,2,3].
Current guidelines favor treatment with intravenous amino-bisphosphonates (N-BPs), particularly zoledronic acid, for its prolonged effective control of PDB activity, or high-dose oral N-BPs (4–6 times the recommended dose for osteoporosis) [1, 4, 5]. Nevertheless, many clinicians, including bone experts, settle for considerably lower than the recommended doses, as low as 5 mg/day of alendronate, based on their clinical judgment, experience, or constrains that preclude the use of the recommended regimens [6,7,8,9].
N-BPs were gradually introduced in Israel since 1995 and were initially exclusively approved for the treatment of osteoporosis. Oral N-BPs became widely available in 2000 and we have used them since to treat our PDB patients, some of whom were switched from the intermittent, cyclic, etidronate regimen. The current study summarizes our long-term experience treating real-world PDB patients with low-doses of oral N-BPs.
Patients and methods
Patients
Patients were seen (by Y.L.) between 1990 and 2015 at the Soroka University Medical Center Endocrine Clinic, which provides secondary and tertiary endocrine care for a population of ~700,000 in Southern Israel. All PDB patients treated with N-BPs were included in the study and no exclusion criteria were applied. None of our patients received high-dose oral, or intravenous, bisphosphonate treatment prior to receiving the low-dose regimen. Clinical data and laboratory results were extracted retrospectively from paper charts and electronic medical records and transferred to an electronic worksheet for statistical analysis.
PDB was often discovered serendipitously due to elevated AP, suggestive X-ray, or bone scintigraphy findings. The patients suffered from mild to moderate skeletal pain; none had severe pain or overt complications of PDB. The diagnosis of PDB was definitively established based on accepted clinical, radiographic and scintigraphic criteria [3]. Disease activity was determined based on symptoms and total serum AP, following exclusion of vitamin D deficiency or other metabolic bone disease. When in doubt regarding possible confounding hepatobiliary origin of AP, AP isoenzymes were determined by electrophoresis, and gamma-glutamyl-transferase (GGT) was measured. Patients with active disease were initially prescribed once-weekly, brand-name bisphosphonate preparations (alendronate 70 mg or risedronate 35 mg). Brand-name preparations were occasionally switched to generic preparations, as they became available. We aimed at decreasing and maintaining serum AP at mid-normal range. Based on results of available published studies with high-dose N-BPs [1, 4, 5], we allowed 3–4 month to achieve normalization of AP during N-BPs treatment to assess response. Dose was modified, according to the initial response, either increased to twice “weekly” tablets (140 mg/week or 70 mg/week for alendronate and risedronate, respectively), and occasionally decreased to a one “weekly” tablet every 2 weeks. None of our patients was switched between oral bisphosphonates, except those initially treated with intermittent, cyclic, courses of etidronate who were switched to N-BPs [10]. All our patients received regular calcium and vitamin D supplementations.
Definitions
“Treatment course”—the period between initiation and cessation of bisphosphonate treatment or change in dose; “Remission”—normalization of serum AP activity (<130 IU); “Duration of remission”—the time period following discontinuation of a treatment course after achieving normal AP, until the first occurrence of AP ≥ 130 IU, or until re-initiation of a new treatment course (whenever treatment was resumed before AP ≥ 130 IU).
Statistical analysis
Results are presented as mean (±SD) for continuous variables and as percentages for categorical variables. Categorical variables were compared using the chi-square test. Continuous variables were examined with the Student's t-test. Continuous variables that were not normally distributed were reported as median and interquartile range (IQR) and compared by the Kruskal Wallis or Mann–Whitney U-test. Statistical analyses were performed using IBM SPSS version 24 (Chicago, USA). P-values < 0.05 were considered statistically significant.
Results
Patients’ baseline characteristics
The baseline characteristics of the patients are presented in Table 1. There were 21 patients, 7 women and 14 men, with a mean age at presentation of 64 ± 3 years (range 43–87), who were followed-up for a mean of 11.9 years (range: 1.7–24.8 years).
Active-treatment courses with oral N-BPs
We observed a total of 95 with oral N-BPs: 85 with alendronate (32 of which with generic alendronate), and 11 with risedronate (6 of which with generic risedronate).
Table 2 presents the treatment outcomes for the various drugs and dose regimens. Of 85 treatment courses with alendronate, 71 (83%) were with 70 mg/week, 10 (12%) with an augmented dose of 70 mg twice a week (140 mg/week), and 4 (5%) with a reduced alendronate dose of 70 mg every 2 weeks (70 mg/2 weeks).
Out of 11 treatment courses with risedronate, 8 were with 35 mg/week, 2 with an augmented dose of 35 mg twice a week (140 mg/week), and 1 with a reduced dose of 35 mg every 2 weeks (35 mg/2 weeks).
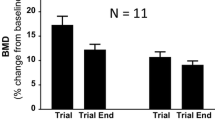
Remissions were achieved in 84% of the courses with alendronate 70 mg/week, and in 90% of courses with 140 mg/week, 7 of which following failure to achieve remission with the 70 mg/w dose, and remission was achieved in all but one patient (Fig. 1). Similarly, 87% of those treated with risedronate 35 mg/week achieved remission, and the 2 patients who did not achieve remission with the 35 mg/week, achieved remission with 35 mg/twice a week (70 mg/week). In patients treated with N-BPs who achieved remission, the median time to reach normal AP was 3–4 months, irrespective of drug.
Individual responses of serum alkaline phosphatase to alendronate, 70 mg/week, and an augmented, 140 mg/week dose. The horizontal dashed line indicates the upper limit of the normal for serum alkaline phosphatase. The one patient (asterisk) who failed to respond to the augmented oral dose subsequently achieved long-term remission with iv zoledronic acid
Figure 2 provides an illustration of long-term management in a patient treated with intermittent oral alendronate, 70 mg/week.
Remissions
We observed a total of 60 documented remission periods in patients following oral N-BPs (Table 2). The remissions’ duration was highly variable with a median of 7–9.5 months (note: since re-institution of treatment was often initiated while AP still within normal range, the results reflect minimal estimates of remission duration).
Following alendronate courses the median increase rate of AP during no-treatment periods was 6.1 IU/month (IQR 3.9, 10.7). The AP increase rate following risedronate was 9.7 U/month (IQR 5.7, 14.8); the difference between the drugs did not reach significance.
We observed a slight, non-significant, positive correlation (r = 0.24) between the length of the preceding treatment courses and the duration of subsequent remissions.
Maintenance of remission with continuous oral N-BPs treatment
Twenty one treatment courses with alendronate 70 mg/week and 1 with risedronate 35 mg/week treatment started while patients were still in remission (AP < 130). AP remained normal in 18 (86%) and increased above normal range in 3 (14%) of the alendronate courses and remained normal in the one continuous risedronate treatment course.
Effect of further reduced dose of alendronate
There were 4 treatment courses with alendronate 70 mg/2 weeks. Three courses which were started during remission, resulted in relapse. One which started with AP > 130 resulted in remission.
Adverse events
Low-dose oral N-BPs were well tolerated. None of our patients discontinued oral bisphosphonate treatment or reported bisphosphonate-related adverse effects.
Discussion
Our results indicate that in a population of PDB patients with mild to moderately active disease, disease activity could be controlled for very-long periods of time with once-weekly preparations of either alendronate (70 mg/week) or risedronate (35 mg/week), originally intended for osteoporosis treatment. These dose regimens are considerably lower than the 40 mg/day and 30 mg/day recommended in clinical practice guidelines for alendronate and risedronate, respectively [4, 5]. Most of our patients who did not achieve remission with the “once-weekly osteoporosis dose” subsequently responded to an increase to twice a week the “weekly” dose (Fig. 1), yet still considerably lower than the currently recommended doses. While higher doses of oral alendronate were associated with adverse effects and withdrawal from treatment [11,12,13], our results with low-dose N-BPs revealed comparable success rates with no appreciable adverse effects and no withdrawal from treatment.
Few others have referred to the efficacy of lower than the recommended doses of N-BPs, as low as 5 mg/day (35 mg/week) of alendronate, in “real-world” patients [6,7,8,9, 14]. Some disparities between doses deemed effective in seminal controlled studies and reports from “real-world” settings, could be due to more extensive disease in patients participating in controlled studies conducted in referral centers vs. patients treated in “real-world” settings [15, 16].
The median duration of active N-BPs treatment courses for patients treated with either oral alendronate or risedronate who started treatment courses with AP > 130 was between 8 months and a year. The time required to achieve remission was variable, with a median of 3–4 months, comparable to the observed response with a much higher dose of alendronate, 40 mg/day [12]. Remissions’ lengths were also of variable duration and lasted for a median of 7–17 months. It should be noted that since laboratory testing was not performed regularly, the recorded times to achieve remission reflect maximal estimates, while the recorded remissions duration, occasionally interrupted by re-initiation of treatment, reflect minimal estimates. It has previously been suggested that the duration of remission was related to the duration of treatment and to the nadir levels of AP [13, 17, 18]. Our data revealed a slight, non-significant, correlation between treatment length and remission duration. The variable response of individual patients could be attributed to the extent of bone involvement, the degree of disease activity, the particular bisphosphonate used, the compliance rate, and the bioavailability of the oral bisphosphonates in individual patients. The maintenance of long-term efficacy of low-dose oral N-BPs in our PDB patients is remarkable, given the relatively high rate of treatment failure observed by us in long-term oral N-BPs treated osteoporotic women [19]. We observed no difference in the rate of remissions achieved with either alendronate or risedronate, and we observed no appreciable difference in response to brand-name and generic N-BPs preparations (data not shown).
Our study has limitation: it is observational, retrospective, and reflects a single institute experience. Patients suffered from mild to moderately active disease. Treatment of mildly symptomatic patients is still a controversial issue [2, 9, 16, 20], despite investigative attempts to settle it [21, 22]. Our choice was to treat all PBD patients with active disease. Our results cannot be necessarily generalized to patients with extensive disease.
The number of risedronate treatment courses was small. We used only AP as marker for determining disease activity, because of its availability and proven utility, and unavailability of modern bone turnover markers (e.g., P1NP, CTx, NTx) during the study period. However, the new markers have been suggested as ancillary to AP assessment mainly in patients with concurrent hepatobiliary disease [4], but otherwise, their use in routine practice is not recommended or controversial [2, 23]. Due to the well-established correlation between AP and bone scan [23], we did not repeat bone scans in asymptomatic patients. Finally, we did not use formal assessment tools to evaluate pain in our routine clinic, but we were attentive to patients’ complaints.
The study’s strength is that it reflects a less-conventional, but effective, “real-world” approach to treatment PBD patients. It included all PDB patients treated in our clinic during the respective period following the introduction of N-BPs and thus faithfully reflects outcomes of treatment during short and very-long follow-ups in “real-world” PBD patients. Despite limitations, our results are both clinically and statistically highly significant.
Our results indicate that whenever the use of the recommended standard of care for controlling active PDB, i.e., single intravenous infusion of zoledronic acid, is precluded, oral N-BPs, at doses equal or twice those recommended for osteoporosis treatment, can be extremely efficacious in controlling disease activity in a large proportion of “real-world” patients. Other parenteral alternatives, such as s.c. or intranasal Salmon calcitonin or intravenous pamidronate were not used in our clinic during the present study time-frame, due to previous somewhat-disappointing clinical outcomes. Other intravenous treatment options besides zoledronate, such as ibandronate or neridronate were never available in Israel. We show that 4–6 months on an oral N-BP treatment can provide prolonged subsequent remissions in a very large proportion of “real-world” patients. Given the linear rate of AP increase following treatment courses [13], the approximate timing for re-initiation of treatment, to maintain continuous control of the disease activity, can be predicted. In our study the median AP increase rates were 6.3 and 9.7 IU/months for alendronate and risedronate, respectively. The difference between the two drugs could possibly reflect the higher affinity of alendronate to bone and its longer residual effect, as previously demonstrated in osteoporotic patients [24,25,26].
Despite reports that alendronate at doses as low as 5 mg/day could provide long-term control of PDB activity, [7, 14], our results suggest that its efficacy is limited.
Conclusions
We provide a strong proof of concept that low-dose oral amino-bisphosphonates are highly effective in controlling Paget’s disease of bone in a large proportion of “real-world” patients, and could be considered as reasonable therapeutic alternative, particularly in the present era of decreasing prevalence and decreasing severity of the disease [27].
References
S. Takata, J. Hashimoto, K. Nakatsuka, N. Yoshimura, K. Yoh, I. Ohno et al. Guidelines for diagnosis and management of Paget’s disease of bone in Japan. J. Bone Miner. Metab. 24, 359–367 (2006)
J.P. Devogelaer, P. Bergmann, J.J. Body, Y. Boutsen, S. Goemaere, J.M. Kaufman et al. Management of patients with Paget’s disease: a consensus document of the Belgian Bone Club. Osteoporos. Int. 19, 1109–1117 (2008)
E.S Siris, G.D Roodman. Paget’s disease of bone. In Primer on the metabolic bone diseases and disorders of mineral metabolism, ed by Rosen C.J, Bouillon R., Compston J.E., Rosen V. 8 edn. (Wiley-Blackwell, Danvers, MA, 2013) pp. 659-668.
F.R. Singer, H.G. Bone, D.J. Hosking, K.W. Lyles, M.H. Murad, I.R. Reid et al. Paget’s disease of bone: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99, 4408–4422 (2014)
C. Muschitz, X. Feichtinger, J. Haschka, R. Kocijan, Diagnosis and treatment of Paget’s disease of bone: a clinical practice guideline. Wien. Med. Wochenschr. 167, 18–24 (2017)
M. Hoshiro, T. Harada, H. Iwai, T. Miyatake, A. Nishimura, Y. Ohno et al. Two cases of monostotic Paget’s disease: effects of bisphosphonate. Endocr. J. 50, 385–392 (2003)
J. Takada, K. Iba, T. Yamashita, Low dose of oral alendronate decreases bone turnover in Japanese patients with Paget’s disease of bone. J. Bone Miner. Metab. 23, 333–336 (2005)
Anjali, N. Thomas, S. Rajaratnam, N. Shanthly, R. Oommen, M.S. Seshadri, Paget’s disease of bone: experience from a centre in southern India. J. Assoc. Physicians India 54, 525–529 (2006)
J.P. Walsh, R. Attewell, B.G. Stuckey, M.J. Hooper, J.D. Wark, S. Fletcher et al. Treatment of Paget’s disease of bone: a survey of clinical practice in Australia. Bone 42, 1219–1225 (2008)
R.D. Altman, Long-term follow-up of therapy with intermittent etidronate disodium in Paget’s disease of bone. Am. J. Med. 79, 583–590 (1985)
S. Adami, M. Mian, P. Gatti, M. Rossini, N. Zamberlan, F. Bertoldo et al. Effects of two oral doses of alendronate in the treatment of Paget’s disease of bone. Bone 15, 415–417 (1994)
S.A. Khan, S. Vasikaran, E.V. McCloskey, M.N. Beneton, S. Rogers, L. Coulton et al. Alendronate in the treatment of Paget’s disease of bone. Bone 20, 263–271 (1997)
J.P. Brown, D.J. Hosking, L. Ste-Marie, C.C.J. Johnston, J. Reginster, W.G. Ryan et al. Risedronate, a highly effective, short-term oral treatment for Paget’s disease: a dose-response study. Calcif. Tissue Int. 64, 93–99 (1999)
K. Iba, J. Takada, T. Wada, T. Yamashita, Five-year follow-up of Japanese patients with Paget’s disease of the bone after treatment with low-dose oral alendronate: a case series. J. Med. Case Rep. 4, 166 (2010)
J.R. Hampton, Evidence-based medicine, opinion-based medicine, and real-world medicine. Perspect. Biol. Med. 45, 549–568 (2002)
I.R. Reid, D.J. Hosking, Bisphosphonates in Paget’s disease. Bone 49, 89–94 (2011)
R.E. Gray, A.J. Yates, C.J. Preston, R. Smith, R.G. Russell, J.A. Kanis, Duration of effect of oral diphosphonate therapy in Paget’s disease of bone. Q. J. Med. 64, 755–767 (1987)
S.A. Khan, E.V. McCloskey, K. Nakatsuka, J. Orgee, G.M. Coombes, J.A. Kanis, Duration of response with oral clodronate in Paget’s disease of bone. Bone 18, 185–190 (1996)
Y. Liel, Y. Plakht, M. Abu Tailakh, Bone turnover in osteoporotic women during long-term oral bisphosphonates treatment. Implications for treatment failure and "drug holiday" in the real world. Endocr. Pract 23, 787–793 (2017).
S.H. Ralston, L. Corral-Gudino, W.D. Fraser, L. Gennari, N. Guañabens, P.L. Selby, Letter to the Editor: the endocrine society clinical practice guidelines on Paget’s disease: many recommendations are not evidence based. J. Clin. Endocrinol. Metab. 100, L45–L46 (2015)
A.L. Langston, M.K. Campbell, W.D. Fraser, G.S. MacLennan, P.L. Selby, S.H. Ralston et al. Randomized trial of intensive bisphosphonate treatment versus symptomatic management in Paget’s disease of bone. J. Bone Miner. Res. 25, 20–31 (2010)
A. Tan, K. Goodman, A. Walker, J. Hudson, G.S. MacLennan, P.L. Selby et al. Long-term randomized trial of intensive versus symptomatic management in Paget’s disease of bone: The PRISM-EZ Study. J. Bone Miner. Res. 32, 1165–1173 (2017)
A.A. Al Nofal, O. Altayar, K. BenKhadra, O.Q. Qasim Agha, N. Asi, M. Nabhan et al. Bone turnover markers in Paget’s disease of the bone: A Systematic review and meta-analysis. Osteoporos. Int. 26, 1875–1891 (2015)
F.H. Ebetino, A.M. Hogan, S. Sun, M.K. Tsoumpra, X. Duan, J.T. Triffitt et al. The relationship between the chemistry and biological activity of the bisphosphonates. Bone 49, 20–33 (2011)
P. Peris, M. Torra, V. Olivares, R. Reyes, A. Monegal, A. Martínez-Ferrer et al. Prolonged bisphosphonate release after treatment in women with osteoporosis. Relatsh. Bone Turnover Bone 49, 706–709 (2011)
R. Eastell, R.A. Hannon, D. Wenderoth, J. Rodriguez-Moreno, A. Sawicki, Effect of stopping risedronate after long-term treatment on bone turnover. J. Clin. Endocrinol. Metab. 96, 3367–3373 (2011)
T. Cundy, Treating Paget’s disease-why and how much? J. Bone Miner. Res. 32, 1163–1164 (2017)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The study protocol was approved by the Soroka Medical Center Human Research Review Board in accordance with the Declaration of Helsinki. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Liel, Y., Abu Tailakh, M. Long-term control of Paget’s disease of bone with low-dose, once-weekly, oral bisphosphonate preparations, in a “real world” setting. Endocrine 63, 651–656 (2019). https://doi.org/10.1007/s12020-018-1806-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1806-y