Abstract
This study evaluated the clinical efficacy of treatment with oral risedronate (17.5 mg once daily) for 8 weeks in 11 Japanese patients with Paget’s disease of bone (PDB). Risedronate suppressed the excessive bone turnover associated with PDB and improved several biochemical markers, including serum alkaline phosphatase (ALP), serum bone-specific ALP (BALP), urinary deoxypyridinoline (DPD), and urinary cross-linked N-telopeptide of type 1 collagen (NTX). These markers began to decrease within about 2 weeks after the initiation of treatment in most patients, and the response persisted for up to 40 weeks after the cessation of treatment. Risedronate reduced pain by week 24 in most patients. According to quantitative bone scintigraphy, the lesion with the highest radioisotope (RI) uptake showed a decrease of uptake from 12.7 ± 6.8 to 6.0 ± 2.3 (mean ± SD) in week 24, although each lesion of patients with polyostotic disease had a different scintigraphic response. Overall, risedronate at a dose of 17.5 mg once daily was well tolerated by patients with PDB, even though the dosage was seven times higher than that approved for the treatment of osteoporosis in Japan (2.5 mg once daily). In conclusion, treatment with high-dose risedronate for 8 weeks resulted in clinically significant and sustained improvement of biochemical markers of bone turnover for 48 weeks in patients with PDB, and this improvement was associated with a decrease of RI uptake by Paget’s bone lesions and with reduced pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paget’s disease of bone (PDB) is a chronic disorder characterized by focal areas of excessive bone turnover [1–3]. PDB is the second most common metabolic bone disease after osteoporosis in both Europe and North America [1, 2], where it has been estimated to affect approximately 1–5% of individuals aged over 55 years [1–6]. Marked geographic variations in the prevalence of PDB have been reported. This disease has a high prevalence in Western Europe, New Zealand, Australia and the United States, whereas a relatively low prevalence has been reported in Northern Europe, and PDB is extremely rare in Asia and Africa [1–7]. Indeed, the overall prevalence of PDB in Japan was reported to be only 2.8 per million, which means that the total number of patients would range between 200 and 300 [7].
There are essentially no differences of the underlying pathophysiology, clinical signs and symptoms, and diagnostic criteria between PDB in Japan and this disease in the high-prevalence countries [2, 3]. However, management of PDB in Japan differs from that in the high-prevalence countries, partly because of the marked difference in prevalence. Recent clinical studies performed in Europe and the United States have shown that the second- and third-generation bisphosphonates are preferable to first-generation products because these are more effective at suppressing bone turnover, so these potent bisphosphonates are commonly used as first-line therapy in these countries [8–10]. In Japan, however, calcitonin and etidronate were the only pharmaceutical treatments approved for PDB until very recently, and there were no data about the efficacy of second- and third-generation bisphosphonates for Japanese patients.
Accordingly, the aim of this phase III clinical study was to evaluate the efficacy, tolerability, and safety of risedronate in Japanese patients with PDB by examining several biochemical markers of bone turnover and by bone scintigraphy.
Materials and methods
Patients
Eight male and 4 female patients aged 20–85 years with PDB diagnosed according to the standard clinical criteria of the Japanese Osteoporosis Society [11] were enrolled in this study. Enrolment criteria included a serum alkaline phosphatase (ALP) level more than twice the upper limit of the normal range and a period of at least 2 years since menopause in the female patients. Patients had not been treated or had failed to respond to bisphosphonate or to calcitonin.
Exclusion criteria were as follows: treatment with bisphosphonates within 8 weeks before the beginning of the study; treatment with other drugs that could affect bone metabolism (calcitonin and vitamin D preparations) within 4 weeks or for 4 weeks or more within 24 weeks before the beginning of the study; esophagitis and/or peptic ulcer (esophageal, gastric, or duodenal ulcer); disorders that could delay esophageal transit (e.g., dysphagia, esophageal stenosis, and achalasia); inability to maintain a standing or upright sitting posture for 30 min or more; hyperparathyroidism, hyperthyroidism, and/or osteomalacia within 1 year before the start of the study; serious renal, hepatic, or cardiac disease; and malignancy being treated with chemotherapy.
Study design
This was a phase III, multicenter, noncomparative, open-label study of oral risedronate (17.5 mg once daily for 8 weeks), with a 40-week posttreatment follow-up period, which was conducted between April 2006 and October 2007. The study protocol was approved by the Institutional Review Board of each participating institution, and all patients provided written informed consent. This study was conducted in compliance with Good Clinical Practice guidelines, and conformed to the ethical principles set out in the Declaration of Helsinki. The investigators who participated in this study are listed in the Appendix.
After a washout period for previous PDB treatments (8 weeks for bisphosphonates or 4 weeks for other agents such as calcitonin), each patient was given 17.5 mg risedronate orally once daily for 8 weeks. The dosage was based on the results of a phase III study from North America [12] and previous studies of risedronate performed in Japanese osteoporosis patients [13–16]. Risedronate was supplied by Ajinomoto and by Takeda Pharmaceutical Company. Throughout the 48-week study period, concomitant use of drugs known to influence PDB, such as other bisphosphonates or calcitonin, was prohibited.
Assessment of efficacy
Serum and urinary biochemical markers of bone metabolism were investigated to determine the percent changes of serum ALP, serum bone-specific ALP (BALP), urinary deoxypyridinoline (DPD), and urinary cross-linked N-telopeptide of type 1 collagen (NTX) from baseline to week 48. All urinary parameters were corrected for creatinine (CRN) excretion. Other outcome measures included the evaluation of pain and scintigraphic assessment of bone lesions.
Serum and urine samples were collected at baseline and in weeks 2, 4, 8, 12, 16, 24, 32, 40, and 48 for the measurement of bone metabolism markers. All markers were measured at a central laboratory (SRL, Tokyo, Japan) by standard methods. Serum ALP was determined by the Japan Society of Clinical Chemistry (JSCC) method using Cica Liquid ALP (Kanto Chemical, Tokyo, Japan), and serum BALP was determined by an enzyme immunoassay (Osteolinks “BAP”; Quidel, San Diego, CA, USA). Urinary NTX was measured by an enzyme-linked immunosorbent assay (Osteomark; Inverness Medical Japan, Tokyo, Japan), and urinary DPD was determined by high-performance liquid chromatography (SRL, Tokyo, Japan).
Pain at rest was assessed by each patient with a visual analogue scale (VAS) on which 0 mm corresponded to no pain and 100 mm represented maximum pain. Pain was assessed at baseline, in week 8, and in week 24.
Paget’s bone lesions were assessed and staging of the disease was done by plain radiography and bone scintigraphy at baseline and in week 24. Scintigraphy was done by performing a bone scan at 3 h after the injection of 99mTc-labeled methyl diphosphonate (MDP). Images were input into digital analyzers, and the area and intensity of lesions were quantified through digital image processing. For scintigraphic assessment, the region of interest (ROI) was drawn around each bone lesion, and the radioisotope (RI) uptake ratio was calculated as the uptake in the ROI relative to that at a non-Paget’s reference site, which was either the contralateral bone (if normal) or an unaffected humerus. The mean radioactivity per pixel of each lesional ROI was divided by that of the reference ROI to calculate the RI uptake ratio as described previously [17–20]. To perform staging of PDB, a Central Assessment Committee with four members was organized. To minimize variation in the assessment of imaging data, one committee member confirmed the eligibility of each patient and the ROIs on bone scintigraphy images at baseline. During the study, the four committee members independently viewed bone images to assess disease progression and then reached a consensus regarding the disease status by discussion.
Assessment of safety
Adverse events were recorded throughout the study. Vital signs and results of laboratory tests (i.e., hematology tests, biochemistry tests, and urinalysis) were also monitored. Each adverse event was assessed with regard to its frequency, severity (mild, moderate, or severe), timing of onset, and relationship to risedronate therapy.
Statistical analysis
A previous survey estimated that the total number of PDB patients in Japan was only a few hundred [7], so the sample size was set at ten, considering the feasibility of patient recruitment. The statistical power was calculated to be 100% with a group of ten patients when a one-sample t test was applied with significance accepted at P < 0.05 based on the percent changes of biomarkers during a phase III study performed in North America [12].
For efficacy variables, the changes from baseline to each time point were assessed with a one-sample t test, and P < 0.05 was considered as statistically significant. Results are presented as the mean ± standard deviation (SD).
Results
Twelve patients (8 men and 4 women, aged 68.6 ± 7.7 years) were enrolled in the study, and they were all treated with 17.5 mg risedronate orally once a day for 8 weeks. The demographic characteristics of the patients are described in Table 1.
One patient suffered from recurrence of bile duct cancer during this study. Because the recurrent cancer led to the elevation of serum ALP and BALP, we concluded that it was not appropriate to assess efficacy in this patient. Accordingly, the efficacy assessment was done in the remaining 11 patients who completed the 40-week follow-up period. With respect to the baseline bone metabolism markers of these 11 patients, the mean serum ALP and BALP levels were 1090.3 ± 616.6 and 189.7 ± 153.0 U/l, respectively; mean urinary DPD and NTX were 28.9 ± 14.3 pmol/μmol·CRN and 390.9 ± 164.1 nmol bone collagen equivalents (BCE)/mmol·CRN, respectively. These values were similar to the mean baseline values for the original 12 patients.
Biochemical markers of bone metabolism
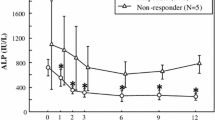
The mean percent changes of bone formation markers (serum ALP and BALP) from baseline to week 48 are shown in Fig. 1. Both markers decreased significantly from week 8 to week 48 compared with baseline (P < 0.001). After 8 weeks of treatment, mean serum ALP and BALP levels were decreased by 45.8% and 49.1%, respectively, and the markers continued to decline during the subsequent 16-week period. The maximum mean reduction from baseline was seen in week 24, with a reductions of 63.2% for serum ALP and 71.6% for serum BALP. Similar levels were then sustained until week 48.
With respect to the serum ALP excess*, which is a parameter used in previous overseas studies to combine data from different laboratories where the normal range varied [21, 22], there was a reduction of 85.3% in week 24 and 82.1% in week 48.
The mean percent changes of the bone resorption markers (urinary DPD and NTX) from baseline to week 48 are shown in Fig. 2. Both markers decreased significantly from week 2 to week 48 compared with baseline (P < 0.001). After 8 weeks of treatment, the mean urinary DPD and NTX levels were decreased by 56.4% and 78.3%, respectively, with similar levels being maintained until week 48.
Percent changes (mean ± SD) of urinary deoxypyridinoline (DPD)/creatinine and urinary cross-linked N-telopeptide of type 1 collagen (NTX)/creatinine in 11 Japanese patients with Paget’s disease of bone treated for 8 weeks with risedronate (17.5 mg orally once daily) and observed for the following 40 weeks (to week 48)
Individual serum ALP levels were decreased by 47.7–82.7%, with the mean maximum reduction being 66.4%. During the period from week 8 after the initiation of treatment to week 40, 9 of 11 patients showed reduction to within the normal range, and the level was within the normal range until the final observation in week 48 for 7 patients. The 2 patients who did not show reduction to the reference level both had polyostotic disease. For these patients, the baseline value and the lowest value after starting treatment were 2770 and 717 U/l versus 1429 (48.4% reduction) and 375 U/l (47.7% reduction), respectively.
Assessment of pain (VAS)
Table 2 shows the profile of VAS pain scores over time. The mean baseline VAS score was 12.0 ± 15.0 mm; it decreased to 10.0 ± 13.4 mm in week 8 and to 6.2 ± 11.8 mm in week 24. With respect to individual patient responses, there were 9 symptomatic patients with pain at baseline. The VAS score was decreased by week 8 in 7 patients and 5 patients had no pain (0 mm) in week 24; 1 patient was unchanged and 1 showed minimal deterioration.
Radiologic assessment
Plain radiography and bone scintigraphy revealed that Paget’s disease was of the mixed type (lytic-sclerotic) in all lesions of all patients, with polyostotic disease in 6 patients and monostotic disease in the others. Abnormal RI uptake was detected at a total of 36 sites in 11 patients at baseline. The most common sites were the pelvis (n = 8), lumbar vertebrae (n = 5), femur (n = 4), and thoracic vertebrae (n = 4). The mean value of the highest RI uptake ratio for the bone lesions identified at baseline in each patient decreased from 12.7 ± 6.8 to 6.0 ± 2.3 by week 24. The mean change from baseline was –6.7 ± 6.1, and the reduction was significant (P = 0.004). Ten of the 11 patients (90.9%) showed a decrease of the RI uptake ratio, although 1 patient had an increased uptake ratio for six of seven lesions.
Adverse events
The incidence of adverse events is summarized in Table 3. Except for one case of bile duct cancer recurrence, the adverse events were mild to moderate. Five events that were potentially related to risedronate occurred in 3 of the 12 patients (25.0%), and these events included three episodes of diarrhea and one each of stomach discomfort and peripheral edema. All these events were mild, and all resolved. With regard to upper gastrointestinal disorders, which are a well-known concern with bisphosphonate therapy, stomach discomfort occurred in 3 of the 12 patients (25.0%), but only one event was potentially related to risedronate therapy, as already noted. All these events were mild and all resolved.
With regard to the biochemical parameters, serum calcium decreased slightly during risedronate treatment because of the inhibitory effect on bone resorption, and serum intact parathyroid hormone (PTH) increased as a compensatory mechanism to restore the serum calcium level. Serum calcium and intact PTH levels returned to baseline after the completion of treatment. None of the patients developed symptomatic hypocalcemia.
Discussion
This Japanese phase III study demonstrated that oral risedronate at a dose of 17.5 mg once daily for 8 weeks could significantly decrease the abnormal levels of biochemical markers that had been increased by activation of bone metabolism associated with PDB, and the improvement was maintained for up to 40 weeks after the cessation of drug treatment. Risedronate normalized the serum ALP level in 9 of 11 patients (81.8%) during the 48-week study period and reduced the pain scores of most patients in week 24.
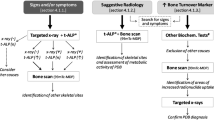
Bone lesions were assessed by quantitative bone scintigraphy in the present study. Risedronate reduced the RI uptake ratio of bone lesions in the majority of patients over 24 weeks, with a reduction to approximately half of baseline for the mean RI uptake ratio. Figure 3 shows the time course of the RI uptake ratio for the individual lesions of 6 patients with polyostotic disease (Fig. 3A) and 5 patients with monostotic disease (Fig. 3B). The RI uptake ratios of polyostotic lesions showed the following three distinct patterns (Fig. 3A): 2 patients had a similar reduction of the ratio in all bone lesions (a-1), 1 patient exhibited no response (a-2), and 3 patients had differing responses of different lesions (a-3). In the patients with a different response of each lesion (Fig. 3A, a-3), the greatest reduction was seen for the lesion with highest uptake at baseline. Possible factors explaining this finding include the preferential uptake of bisphosphonate (risedronate) by the most severely affected lesion [20, 23, 24], as is seen with diagnostic 99mTc-labeled MDP for bone scintigraphy, and/or a difference in the lytic, blastic, and mixed components of each bone lesion. Despite the suppression of biochemical markers, 1 patient exhibited no response to treatment based upon bone scintigraphic assessment (Fig. 3A, a-2). Avramidis et al. [20] reported one similar case in a study of zoledronic acid treatment. The overall findings of bone scintigraphy suggested that 99mTc-labeled MDP uptake is not necessarily decreased selectively in Paget’s bone compared with healthy bone and that the reduction of bone uptake after bisphosphonate treatment could depend on the severity and/or the stage of each lesion. Therefore, biochemical markers of bone metabolism may be more sensitive and useful for monitoring the response to treatment.
Bone scintigraphy radioisotope (RI) uptake ratios for the individual lesions of 6 Japanese patients with polyostotic Paget’s disease (A) and 5 Japanese patients with monostotic Paget’s disease (B) treated for 8 weeks with risedronate (17.5 mg orally once daily) and observed for the following 16 weeks (to week 24): a-1, patients with a similar reduction; a-2, a patient with no response; a-3, patients with a different response
Serum ALP, serum BALP, urinary DPD, and urinary NTX were simultaneously measured in this phase III study to evaluate the impact of drug therapy on biochemical markers of bone turnover. It was demonstrated that urinary NTX, a bone resorption marker, showed a significant decrease of 53.0% in week 2 (P < 0.001). Its response to risedronate was faster and more prominent than that of the other markers (see Figs. 1, 2), reflecting the antiresorptive mechanism of action of bisphosphonates. This finding suggests that urinary NTX might be a useful marker for monitoring the response of PDB to treatment.
Our results for the biochemical markers showed that the effects of risedronate at 17.5 mg daily in Japanese PDB patients were almost equivalent to those obtained with 30 mg daily in Europe and the United States [12, 25, 26], at which dosage the drug exhibited a stronger and more prolonged effect than etidronate [12]. Our results for biochemical markers were similar to the findings obtained with other second- and third-generation bisphosphonates, including alendronate [27], ibandronate [28], pamidronate [25, 27, 29], and zoledronic acid [20, 30]. Moreover, risedronate at 17.5 mg daily had a scintigraphic effect in Japanese PDB patients that was similar to other second- and third-generation bisphosphonates [18–20], and greater improvement was observed than had been seen in a previous Japanese study of etidronate [31]. With regard to the optimal dose of risedronate, previous pharmacokinetic studies demonstrated that the maximum plasma concentration (Cmax) and the area under the plasma concentration–time curve (AUC) of risedronate were two to three times higher in Japanese subjects compared with Caucasians because of bioavailability differences [32, 33]. This finding has been confirmed clinically: dosages of 2.5 mg once daily and 17.5 mg once weekly produce results in Japanese osteoporosis patients equivalent to 5 mg once daily and 35 mg once weekly in Caucasian patients [13–16]. Because risedronate acts on PDB via the same mechanism as for osteoporosis, mainly by suppressing excessive bone turnover through the inhibition of bone resorption, approximately half the clinical dose of risedronate used in Europe and the Unites States for PDB should exhibit sufficient efficacy in Japanese PDB patients.
In this Japanese phase III study, risedronate was well tolerated despite the fact that the dosage of 17.5 mg once daily is seven times higher than the approved dosage for osteoporosis in Japan. No clinically significant adverse drug reactions were observed. These results are consistent with overseas clinical trials, in which the tolerability of risedronate was the same as that of etidronate [12].
This study demonstrated the efficacy and safety of risedronate for Japanese PDB patients by assessing biochemical markers, quantitative scintigraphy of bone lesions, and symptoms over 48 weeks, although the sample size was relatively small because of the low prevalence of PDB in Japan. Our findings will contribute to improved understanding of the risk/benefit ratio for risedronate in PDB patients and will also help to identify the long-term clinical outcome.
References
Siris ES, Roodman GD (2006) Paget’s disease of bone. In: Favus MJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism, 6th edn. The American Society of Bone and Mineral Research, Washington, DC, pp 320–330
Takata S, Hashimoto J, Nakatsuka K, Yoshimura N, Yoh K, Ohno I, Yabe H, Abe S, Fukunaga M, Terada M, Zamma M, Ralston SH, Morii H, Yoshikawa H (2006) Guidelines for diagnosis and management of Paget’s disease of bone in Japan. J Bone Miner Metab 24:359–367
Selby PL, Davie MWJ, Ralston SH, Stone MD, Bone and Tooth Society of Great Britain, the National Association for the Relief of Paget’s Disease (2002) Guidelines on the management of Paget’s disease of bone. Bone (NY) 31:366–373
Guyer PB, Chamberlain AT (1980) Paget’s disease of bone in two American cities. Br Med J 280:985
Cooper C, Schafheutle K, Dennison E, Kellingray S, Guyer P, Barker D (1999) The epidemiology of Paget’s disease in Britain: is the prevalence decreasing? J Bone Miner Res 14:192–197
Cooper C, Harvey NC, Dennison EM, van Staa TP (2006) Update on the epidemiology of Paget’s disease of bone. J Bone Miner Res 21(suppl 2):3–8
Hashimoto J, Ohno I, Nakatsuka K, Yoshimura N, Takata S, Zamma M, Yabe H, Abe S, Terada M, Yoh K, Fukunaga M, Cooper C, Morii H, Yoshikawa H (2006) Prevalence and clinical features of Paget’s disease of bone in Japan. J Bone Miner Metab 24:186–190
Selby PL (2006) Guidelines for the diagnosis and management of Paget’s disease: a UK perspective. J Bone Miner Res 21(suppl 2):92–93
Siris ES, Lyles KW, Singer FR, Meunier PJ (2006) Medical management of Paget’s disease of bone: indications for treatment and review of current therapies. J Bone Miner Res 21(suppl 2):94–98
Ralston SH, Langston AL, Reid IR (2008) Pathogenesis and management of Paget’s disease of bone. Lancet 372:155–163
Japanese Committee on Clinical Guideline of Diagnosis and Treatment of Paget’s Disease of Bone in Japan Osteoporosis Society (2005) Atlas of Paget’s disease of bone (in Japanese). Osteoporosis Jpn 13(suppl)
Miller PD, Brown JP, Siris ES, Hoseyni MS, Axelrod DW, Bekker PJ (1999) A randomized, double-blind comparison of risedronate and etidronate in the treatment of Paget’s disease of bone. Am J Med 106:513–520
Fukunaga M, Kushida K, Kishimoto H, Shiraki M, Taketani Y, Minaguchi H, Inoue T, Morita R, Morii H, Yamamoto K, Ohashi Y, Orimo H (2002) A comparison of the effect of risedronate and etidronate on lumbar bone mineral density in Japanese patients with osteoporosis: a randomized controlled trial. Osteoporos Int 13:971–979
Shiraki M, Fukunaga M, Kushida K, Kishimoto H, Taketani Y, Minaguchi H, Inoue T, Morita R, Morii H, Yamamoto K, Ohashi Y, Orimo H (2003) A double-blind dose-ranging study of risedronate in Japanese patients with osteoporosis (a study by the Risedronate Late Phase II Research Group). Osteoporos Int 14:225–234
Kushida K, Fukunaga M, Kishimoto H, Shiraki M, Itabashi A, Inoue T, Kaneda K, Morii H, Nawata H, Yamamoto K, Ohashi Y, Orimo H (2004) A comparison of incidences of vertebral fracture in Japanese patients with involutional osteoporosis treated with risedronate and etidronate: a randomized, double-masked trial. J Bone Miner Metab 22:469–478
Kishimoto H, Fukunaga M, Kushida K, Shiraki M, Itabashi A, Nawata H, Nakamura T, Ohta H, Takaoka K, Ohashi Y (2006) Efficacy and tolerability of once-weekly administration of 17.5 mg risedronate in Japanese patients with involutional osteoporosis: a comparison with 2.5-mg once-daily dosage regimen. J Bone Miner Metab 24:405–413
Lavender JP, Evans IM, Arnot R, Bowring S, Doyle FH, Joplin GF, MacIntyre I (1977) A comparison of radiography and radioisotope scanning in the detection of Paget’s disease and in the assessment of response to human calcitonin. Br J Radiol 50:243–250
Vellenga CJLR, Pauwels EKJ, Bijvoet OLM, Harinck HIJ, Frijlink WB (1985) Quantitative bone scintigraphy in Paget’s disease treated with APD. Br J Radiol 58:1165–1172
Patel S, Pearson D, Hosking DJ (1995) Quantitative bone scintigraphy in the management of monostotic Paget’s disease of bone. Arthritis Rheum 38:1506–1512
Avramidis A, Polyzos SA, Moralidis E, Arsos G, Efstathiadou Z, Karakatsanis K, Grollios G, Kita M (2008) Scintigraphic, biochemical, and clinical response to zoledronic acid treatment in patients with Paget’s disease of bone. J Bone Miner Metab 26:635–641
Brown JP, Hosking DJ, Ste-Marie L, Johnston CC Jr, Reginster J, Ryan WG, Johnson TD, Bekker PJ (1999) Risedronate, a highly effective, short-term oral treatment for Paget’s disease: a dose-response study. Calcif Tissue Int 64:93–99
Hosking DJ, Eusebio RA, Chines AA (1998) Paget’s disease of bone: reduction of disease activity with oral risedronate. Bone (NY) 22:51–55
Fleisch H (1998) Bisphosphonates: mechanisms of action. Endocr Rev 19:80–100
Russell RG, Watts NB, Ebetino FH, Rogers MJ (2008) Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int 19:733–759
Rendina D, Mossetti G, Viceconti R, Sorrentino M, Nunziata V (2004) Risedronate and pamidronate treatment in the clinical management of patients with severe Paget’s disease of bone and acquired resistance to bisphosphonates. Calcif Tissue Int 75:189–196
Peris P, Alvarez L, Vidal S, Martinez MA, Monegal A, Guaňabens N (2007) Treatment with tiludronate has a similar effect to risedronate on Paget’s disease activity assessed by bone markers and bone scintigraphy. Clin Exp Rheumatol 25:206–210
Walsh JP, Ward LC, Stewart GO, Will RK, Criddle RA, Prince RL, Stuckey BG, Dhaliwal SS, Bhagat CI, Retallack RW, Kent GN, Drury PJ, Vasikaran S, Gutteridge DH (2004) A randomized clinical trial comparing oral alendronate and intravenous pamidronate for the treatment of Paget’s disease of bone. Bone (NY) 34:747–754
Reid IR, Davidson JS, Wattie D, Wu F, Lucas J, Gamble GD, Rutland MD, Cundy T (2004) Comparative responses of bone turnover markers to bisphosphonate therapy in Paget’s disease of bone. Bone (NY) 35:224–230
Randall AG, Kent GN, Garcia-Webb P, Bhagat CI, Pearce DJ, Gutteridge DH, Prince RL, Stewart G, Stuckey B, Will RK, Retallack RW, Price RI, Ward L (1996) Comparison of biochemical markers of bone turnover in Paget disease treated with pamidronate and a proposed model for the relationships between measurements of the different forms of pyridinoline cross-links. J Bone Miner Res 11:1176–1184
Garnero P, Gineyts E, Schaffer AV, Seaman J, Delmas PD (1998) Measurement of urinary excretion of nonisomerized and β-isomerized forms of type I collagen breakdown products to monitor the effects of the bisphosphonate zoledronate in Paget’s disease. Arthritis Rheum 41:354–360
Torizuka K, Furukawa Y, Yoshikawa Y, Komatsubara Y, Morita R et al (1989) Clinical evaluation of Paget’s disease of bone with EHDP (etidronate disodium) (in Japanese). Clin Rep 23:1375–1385
Ogura Y, Gonsho A, Cyong J-C, Orimo H (2004) Clinical trial of risedronate in Japanese volunteers: single and multiple oral dose studies. J Bone Miner Metab 22:111–119
Mitchell DY, Eusebio RA, Sacco-Gibson NA, Pallone KA, Kelly SC, Nesbitt JD, Brezovic CP, Thompson GA, Powell JH (2000) Dose-proportional pharmacokinetics of risedronate on single-dose oral administration to healthy volunteers. J Clin Pharmacol 40:258–265
Acknowledgments
This study was supported by the Joint Development Program of Ajinomoto and Takeda Pharmaceutical Company.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Please refer to the following Table 4.
About this article
Cite this article
Yoh, K., Takata, S., Yoshimura, N. et al. Efficacy, tolerability, and safety of risedronate in Japanese patients with Paget’s disease of bone. J Bone Miner Metab 28, 468–476 (2010). https://doi.org/10.1007/s00774-009-0152-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-009-0152-9