Abstract
Over the past two decades, rheumatologists from around the world have not only championed the musculoskeletal system examination but also modified the undergraduate teaching curriculum. This has led to the development and adoption of the gait, arms, legs and spine (GALS) screening along with regional examination techniques. The purpose of this study is to review current practice, determining the frequency of patient exposure to appropriate examination and confidence of junior doctors when dealing with MSK conditions. Two district-general hospitals (non-teaching) and one teaching hospital in North-East London were chosen. At each site, 50 patient notes were reviewed from the acute admission wards for medicine and surgery and the medical assessment unit. Factors considered included whether GALS screenings had taken place, documentation of MSK examinations and assessment of confidence of junior doctors in assessing MSK conditions. GALS screenings were performed for 4% of patients on the medical assessment unit, 7% of acute medical and 0% of acute surgical patients on admission. Examination of the MSK system yielded better results with 16%, 22% and 10% on each of the respective wards. Interviews with junior doctors found 10% routinely screening for MSK conditions, despite 87% feeling confident in taking MSK histories. This prospective audit of clinical practice highlights that patients failed to have a minimal assessment of the MSK system through GALS screenings. When examining the MSK system, results were somewhat better, although still fewer than expected. It is curious that the majority of junior doctors in training felt confident in dealing with MSK disease but few did it in practice. This begs the question of whether current teaching curricula and strategies are adequate. At a time where there is ever-increasing national momentum to address issues on obesity and cardiovascular health, our patients are still deprived of a standard MSK examination by the medical faculty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Examination of the musculoskeletal (MSK) system should be an integral part to the holistic clinical assessment. It is particularly important as complaints arising from MSK conditions remain a significant cause of pain, disability, unemployment and dependence on state support while also impacting upon other non-MSK related medical conditions. A 2003 census by the Office for National Statistics in the United Kingdom (UK) found Arthritis to be responsible for over five hundred thousand Disability Living Allowance (DLA) claims. This is far greater than the three hundred and thirty thousand claims for mental health illnesses [1].
A number of publications from various corners of the globe have raised concerns about inadequacies in MSK examination for hospital patients over the past two decades [2–12]. Various proposals have been made [13–16], but in 1990, a specific structured tool (gait, arms, legs and spine (GALS)) was developed in the UK, for instructing MSK assessment and examination at the undergraduate level in local universities [17, 18]. Further investigation by other academic institutions and within primary care reiterated the lack of MSK examination for hospitalised patients [19–23].
Despite developments in MSK education at the undergraduate level, few junior doctors continue to apply their skills in routine clinical practice [23]. This inevitably leads to delays in referral for specialist care with a resultant increase in in-patient stay, greater associated disability and a negative impact upon the work force. Most published studies have been conducted in teaching hospitals and none attempted a comparison with non-teaching institutions. We have performed this audit, for the first time, from a non-teaching hospital in direct comparison with a neighbouring teaching hospital.
An initial pilot study was performed in 1997 at the Barking, Havering and Redbridge National Health Service (NHS) Trust (a non-teaching institution). All inpatient referrals to Rheumatology over a three month period (May–July) were screened with the aim to assess if the patients had undergone a standard MSK examination. Emphasis was placed on aspects of training received by students at the undergraduate level. Individual case notes were reviewed followed by interviews with the junior doctors. The outcome was very poor reporting of MSK examination and this had a direct positive effect on the discharge policy of the hospital. This early investigation prompted us to undertake a larger, prospective, multicentre audit after educating the students and junior doctors in the hospital about key elements of GALS and the MSK examination. It was conducted during the same time period to enable a fair comparison.
The aims of the current cross-sectional audit were to assess:
-
1.
If the patients were being screened for symptoms/signs using the GALS technique followed by a regional MSK examination at the point of entry or having been admitted to the hospital.
-
2.
If any difference existed between the performances of doctors based at teaching vs non-teaching hospitals with regard to MSK practice.
Patients and methods
One hundred and fifty patients were included in the current audit over the period of 3 months (2007). Due to time limitations of the student researchers, numbers were capped at this level and three centres were chosen. Two were non-teaching district general hospitals (DGH) and the other was a neighbouring teaching hospital, all within North East London.
In addition to assessing medical notes, face-to-face interviews with junior doctors caring for patients on the respective wards were conducted. They reviewed the attitude and practice of professionals towards MSK screening and examination at each site. A questionnaire similar to previous published studies was implemented [18].
Information gathered assessed:
-
1.
Whether junior doctors were routinely screening for MSK disease using the GALS screening technique and if they felt that GALS should be done routinely for all admissions.
-
2.
Junior doctors' confidence in taking an MSK history rated on a five-point scale with 1 being the least and 5 being the most confident. They were asked if they had received instruction into MSK examination as an undergraduate, whether they felt it was useful or beneficial to assess the MSK system and the time since qualification.
The three areas selected in each of the hospitals were the Medical Assessment Unit (MAU), acute Medical and acute Surgical admission wards. These were the primary admission wards for each hospital. On each ward an allocation of beds were randomly selected and the records of prospectively admitted patients were reviewed retrospectively. This was done to avoid biasing the normal admission, decision-making and record keeping processes.
To enable fair comparison with previous studies, the same criteria were used when assessing patient case notes [18].
-
1.
Patient demographics
-
2.
Documentation of the GALS screening questions
-
3.
Documentation of signs and symptoms of any MSK disease
-
4.
Documentation of an MSK and other clinical system examination
-
5.
Previous acute admissions through accident and emergency (A&E), documentation of an MSK examination on initial assessment and final diagnosis upon discharge
-
6.
History of falls and fractures in the past year
Approval was obtained from the audit departments at each centre and to retain a fair comparison, the same number of patient notes was reviewed in each centre.
Results
The current prospective audit reviewed fifty randomly selected medical notes from each hospital site. In total, case notes for 83 (83/150; 55%) male and 67 (67/150; 45%) female patients, with a mean age of 67 years (range 18–98 years), were reviewed. Most patients were based on the MAU (25) followed by the acute medical admission (15) and acute surgical admission (10) wards.
Analysis of primary medical complaints collated by physical system revealed 32 (32/150; 21%) cardiovascular, 21 (21/150; 14%) respiratory, 46 (46/150; 30%) gastro-intestinal, 23 (23/150; 15%) neurological and only 18 (18/150; 12%) had predominantly MSK conditions. Only 10 out of the 150 patients (10/150; 6%) had non-specific symptoms with no provisional diagnosis at the time of the review.
Of all the admissions, only six (6/150; 4%) patients had a documented full GALS assessment while five (5/150: 3%) had a partial assessment (total 11/150; 7%). For the majority (139/150; 93%) there was no documentation of them receiving a GALS screening.
While a documented clinical examination was performed for most specialties including cardiovascular (136/150; 90%), respiratory (139/150; 93%), gastrointestinal (137/150; 91%) and neurological (41/150; 27%), paucity existed for the MSK system (25/150; 16%). This was despite 61 (61/150; 41%) patients mentioning symptoms specific to MSK disease on admission; 19 (19/150; 12%) had severe joint pain while 17 (17/150; 11%) had muscle pain and a similar number noted decreased mobility. Eight (8/150; 5%) patients had complex multi-system MSK disease on admission. It was evident that 71 patients (71/150; 47%) also had previous MSK illnesses of differing varieties (Table 1).
Eighty-nine (89/150; 59%) patients had previously been admitted through casualty (A&E) but only 14 (14/150; 15%) had an MSK examination documented. From those with previous A&E admissions, 52 (52/150; 35%) were diagnosed to have a MSK ailment upon discharge. Seventy-one patients (71/150; 48%) incurred previous falls and 22 (22/150; 15%) had a history of fractures.
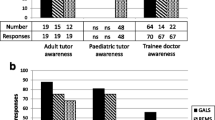
Overall the results indicated significant paucity of documented GALS screening and MSK clinical examination in all wards at all sites (Table 2). A total of 30 junior doctors, including 16 Pre-Registration House Officers (PRHO) and 14 Senior House Officers (SHO), all qualified within the last 2 years, were interviewed. Only three (3/30; 10%) were using GALS screening questions but 12 (12/30; 40%) claimed their documentation included a MSK examination. Twenty-six doctors (26/30; 87%) claimed confidence with the entire MSK assessment process. All doctors admitted to being taught how to examine the MSK system as undergraduates with the majority feeling their training was useful. Little difference could be found between the teaching centre and DGH(s) in terms of doctors' attitude or behaviour.
Discussion
Our preliminary audit in 1997 showed that no patient had received a formal MSK examination upon admission or prior to being referred to the rheumatologists. This investigation, a decade later, demonstrates that although high volumes of patients present with current symptoms (41%) or a previous history of MSK disease (47%), there is no documented assessment for the majority (96%). Additionally, despite receiving appropriate training, only one in ten doctors actually routinely screened for MSK disease with GALS and yet a significant number felt confident they could assess this system. This was largely based on their training as undergraduates.
The lack of a documented GALS screening and MSK examination in clinical practice, despite good levels of confidence amongst trainees, is somewhat surprising and suggests further in-depth analysis of our teaching and training programmes may be necessary [24–27]. One must question whether our utilisation of educational resources for training has delivered the desired improvement in patient care [28–34]. It is also necessary to address the attitude and behaviour of clinical practitioners, be it in the hospital or the community setting.
Perhaps the MSK examination should have greater emphasis, featuring as a general system in all clerking processes and thereby avoiding being ‘over-looked’ by choice or otherwise. Data from documentation of other clinical systems implies a relative and perceived importance of MSK clinical examination by junior doctors. It is not unusual to note that a patient may have delayed rehabilitation and discharge due to difficulties with mobility and independence despite the primary diagnosis on admission being unrelated to the MSK system. It is common practice to document examination of the cardiovascular system even though a patient may have been admitted for a surgical cause such as appendicitis. One would anticipate the same should be true for the MSK system.
We acknowledge that the study was limited by a number of factors but primarily time restraints placed on student researchers. To maintain uniformity, time the period investigated was identical to that a decade earlier and meant that the number of patients and centres included was limited.
To take these concerns further and draw stronger conclusions about what is the underlying problem, we would be interested in conducting a longer-term prospective study, with greater patient numbers in multiple centres. We would also be interested in evaluating the impact of an intervention, perhaps as part of a randomised controlled trial. The true impact on clinical practice by GALS training in the final years of undergraduate, and postgraduate years, remains largely unknown.
Conclusion
Two decades have passed since health professionals in MSK medicine initially identified the ‘cry for help from the joints’ [2]. Even in the twenty-first century, this trend persists despite investments in educational techniques, teaching and training [35, 36]. We also know that musculoskeletal disease is a major cause of disability in the UK [1].
Numerous publications emphasising these deficiencies exist, together with novel ways to educate undergraduates, but it appears that the impact on actual clinical practice remains unaltered. Screening the loco motor system can be made using three simple questions included in GALS incorporating gait, arms, legs and spine. However, while this is often ignored in routine clinical practice and while it is not a substitute to a detailed MSK examination, GALS can potentially dispel the idea that MSK assessment is difficult.
It is disappointing to see that at a time when the nation is struggling to improve the cardiovascular health of its people though exercise, the importance of the MSK system remains largely ignored. Urgent attention is needed at all levels, beginning with universities and continuing to postgraduate training. Two decades have passed and we are still debating on how to detect and treat MSK diseases at the earliest opportunity. Without our intervention, these deficiencies will continue to affect long term illnesses leaving a considerable impact on society, resources and patient themselves.
References
Office of National Statistics UK (2003) Recipients of disability living allowance (DLA): by main disabling condition, 2003: Social Trends 34. (www.statistics.gov.uk/StatBase/ssdataset.asp?vlnk=7403&More=Y)
Doherty M, Abawi J, Pattrick M (1990) Audit of medical inpatient examination: A cry from the joint. J R Coll Physicians Lond 24(2):115–118
Abou-Raya A, Abou-Raya S (2010) The inadequacies of musculoskeletal education, Clin Rheumatol. In press
Menon J, Patro DK (2009) Undergraduate orthopedic education: Is it adequate? Indian J Orthop 43(1):82–86
Freedman KB, Bernstein J (2002) Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am 84-A(4):604–608
Dequeker J, Rasker JJ, Woolf AD (2000) Educational issues in rheumatology. Baillières Best Pract Res Clin Rheumatol 14(4):715–729
Oswald AE, Bell MJ, Snell L, Wiseman J (2008) The current state of musculoskeletal clinical skills teaching for preclerkship medical students. J Rheumatol 35(12):2419–2426
McCarthy EM, Sheane BJ, Cunnane G (2009) Greater focus on clinical rheumatology is required for training in internal medicine. Clin Rheumatol 28(2):139–143
Queally JM, Kiely PD, Shelly MJ, O'Daly BJ, O'Byrne JM, Masterson EL (2008) Deficiencies in the education of musculoskeletal medicine in Ireland. Ir J Med Sci 177(2):99–105
Day CS, Yeh AC (2008) Evidence of educational inadequacies in region-specific musculoskeletal medicine. Clin Orthop Relat Res 466(10):2542–2547
Day CS, Yeh AC, Franko O, Ramirez M, Krupat E (2007) Musculoskeletal medicine: An assessment of the attitudes and knowledge of medical students at Harvard Medical School. Acad Med 82(5):452–457
Ahern MJ, Soden M, Schultz D, Clark M (1991) The musculo-skeletal examination, a neglected clinical skill. Aust NZ J Med 21:303–306
Lawry GV, Schuldt SS, Kreiter CD, Densen P, Albanese MA (1999) Teaching a screening musculoskeletal examination: A randomized, controlled trial of different instructional methods. Acad Med 74(2):199–201
Woolf AD, Walsh NE, Akesson K (2004) Global core recommendations for a musculoskeletal undergraduate curriculum. Ann Rheum Dis 63(5):517–524
Coady DA, Walker DJ, Kay LJ (2004) Teaching medical students musculoskeletal examination skills: Identifying barriers to learning and ways of overcoming them. Scand J Rheumatol 33(1):47–51
Woolf AD (2003) How to assess musculoskeletal conditions. History and physical examination. Best Pract Res Clin Rheumatol 17(3):381–402
Jones A, Ledingham J, Regan M, Doherty M (1991) A proposed minimal rheumatological screening history and examination. The joint answers back. J R Coll Physicians Lond 25(2):111–115
Doherty M, Dacre J, Dieppe P, Snaith M (1992) The ‘GALS’ loco motor screen. Ann Rheum Dis 51(10):1165–1169
Lillicrap MS, Byrne E, Speed CA (2003) Musculoskeletal assessment of general medical in-patients - Joints still crying out for attention. Rheumatology 42:951–954
Beattie KA, Bobba R, Bayoumi I, Chan D, Schabort I, Boulos P, Kean W, Obeid J, McCallum R, Ioannidis G, Papaioannou A, Cividino A (2008) Validation of the GALS musculoskeletal screening exam for use in primary care: A pilot study. BMC Musculoskelet Disord 27(9):115
Fox RA, Dacre JE, Clark CL, Scotland AD (2000) Impact on medical students of incorporating GALS screen teaching into the medical school curriculum. Ann Rheum Dis 59(9):668–671
Haywood BL, Porter SL, Grana WA (2006) Assessment of musculoskeletal knowledge in primary care residents. Am J Orthop (Belle Mead NJ) 35(6):273–275
Al-Nammari SS, James BK, Ramachandran M (2009) The inadequacy of musculoskeletal knowledge after foundation training in the United Kingdom. J Bone Joint Surg Br 91(11):1413–1418
Freedman KB, Bernstein J (1998) The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am 80(10):1421–1427
Mulhall KJ, Masterson E (2005) Relating undergraduate musculoskeletal medicine curricula to the needs of modern practice. Ir J Med Sci 174(2):46–51
Knobe M, Münker R, Sellei RM, Holschen M, Mooij SC, Schmidt-Rohlfing B, Niethard FU, Pape HC (2009) Peer teaching: A randomised controlled trial using student-teachers to teach musculoskeletal ultrasound. Med Educ 44(2):148–155
Saleh K, Messner R, Axtell S, Harris I, Mahowald ML (2004) Development and evaluation of an integrated musculoskeletal disease course for medical students. J Bone Joint Surg Am 86-A(8):1653–1658
Perry ME, Burke JM, Friel L, Field M (2010) Can training in musculoskeletal examination skills be effectively delivered by undergraduate students as part of the standard curriculum? Rheumatology (Oxford). Jun 4. In press
Schrieber L, Hendry GD, Hunter D (2000) Musculoskeletal examination teaching in rheumatoid arthritis education: Trained patient educators compared to nonspecialist doctors. J Rheumatol 27(6):1531–1532
Bideau M, Guerne PA, Bianchi MP, Huber P (2006) Benefits of a programme taking advantage of patient-instructors to teach and assess musculoskeletal skills in medical students. Ann Rheum Dis 65(12):1626–1630
Modica RF, Thundiyil JG, Chou C, Diab M, Von Scheven E (2009) Teaching musculoskeletal physical diagnosis using a web-based tutorial and pathophysiology-focused cases. Med Educ Online 14:13
Bilderback K, Eggerstedt J, Sadasivan KK, Seelig L, Wolf R, Barton S, McCall R, Chesson AL Jr, Marino AA (2008) Design and implementation of a system-based course in musculoskeletal medicine for medical students. J Bone Joint Surg Am 90(10):2292–2300
Wright SA, Bell AL (2008) Enhancement of undergraduate rheumatology teaching through the use of musculoskeletal ultrasound. Rheumatology (Oxford) 47(10):1564–1566
Vivekananda-Schmidt P, Lewis M, Coady D, Morley C, Kay L, Walker D, Hassell AB (2007) Exploring the use of videotaped objective structured clinical examination in the assessment of joint examination skills of medical students. Arthritis Rheum 57(5):869–876, 15
Smith CC, Newman L, Davis RB, Yang J, Ramanan R (2005) A comprehensive new curriculum to teach and assess resident knowledge and diagnostic evaluation of musculoskeletal complaints. Med Teach 27(6):553–558
Williams SC, Gulihar A, Dias JJ, Harper WM (2010) A new musculoskeletal curriculum: Has it made a difference? J Bone Joint Surg Br 92(1):7–11
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sirisena, D., Begum, H., Selvarajah, M. et al. Musculoskeletal examination—an ignored aspect. Why are we still failing the patients?. Clin Rheumatol 30, 403–407 (2011). https://doi.org/10.1007/s10067-010-1632-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-010-1632-y