Abstract
Background
Basic competency in musculoskeletal medicine is essential for many specialties being particularly relevant to primary care.
Aim
The purpose of this study was to objectively assess the adequacy of musculoskeletal education at multiple levels of medical training from undergraduate level to primary care.
Methods
A previously validated musculoskeletal examination was administered to 303 volunteers consisting of medical students, orthopaedic specialist registrars, general practice trainees and general practitioners.
Results
Forty (71%) general practitioners and 74 (71.8%) general practice trainees failed to obtain the passing score of 70. Sixty-three (87.5%) medical students who had completed an intensive 1-week long course in musculoskeletal medicine failed the examination. The pass rate improved significantly for general practitioners who had completed a postgraduate rotation in musculoskeletal medicine (47.8 vs 18.1%, P < 0.01).
Conclusions
These findings suggest that training in musculoskeletal medicine is inadequate at multiple levels of medical education with reform urgently required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders are common and consume significant healthcare and social resources. They account for more than half of all chronic conditions in people older than 50 years of age in developed countries and are the most common cause of severe long-term pain and disability [1, 2]. The prevalence of musculoskeletal disorders is predicted to increase dramatically due to an ageing population and a trend towards sedentary lifestyles with associated obesity. The Centres for Disease Control (USA) predict that by 2020 the number of new patients with arthritis will have increased more than the number of patients with any other disease [3]. A number of specialties will be involved in meeting this increasing demand for musculoskeletal care. Currently, the bulk of care is provided by orthopaedic surgeons, general practitioners, general physicians and physiotherapists. In general practice, musculoskeletal disorders are the second most common reason for visits where they account for 10–28% of all visits across Europe and the USA [2, 4–8].
Basic competency in musculoskeletal medicine is thus essential for many specialists, being particularly relevant in the specialty of general practice. However, medical students, hospital doctors and general practitioners perceive their training in musculoskeletal medicine to be inadequate and have little confidence in performing a basic musculoskeletal examination [9–12]. Investigators who have used specially designed examinations report deficiencies in musculoskeletal knowledge amongst medical students, hospital residents and physicians [9, 13, 14]. A more important group than hospital doctors to assess is general practitioners whose second most common patient complaint is a musculoskeletal symptom. Sneiderman et al. [11] in a survey of 302 general practitioners found that 51% were not satisfied with their training in musculoskeletal medicine. The purpose of this study was to objectively assess the adequacy of musculoskeletal education at multiple levels of medical training in Ireland from undergraduate level to primary care using a validated examination developed by Freedman and Bernstein [13].
Materials and methods
Study participants
A validated cognitive musculoskeletal examination was administered to medical students, general practice trainees and general practitioners. This examination has been validated by orthopaedic surgeons and internal medicine programme directors in the USA, who set a passing score of 70% [13, 14]. The examination consisted of 25 short-answer open-ended questions (see Appendix 1). Based on the validation process, a weighted marking system was used with partial credit given for partially correct answers. A demographic questionnaire was also administered with the examination (see Appendix 2). Topics included those frequently seen in general practice such as low-back pain, arthritis and minor injuries. Orthopaedic emergencies necessitating immediate referral to an orthopaedic surgeon were also included.
The recruitment process involved recruiting participants at a respective education session. For example, medical students were asked to complete the examination after a lecture and general practice trainees after a scheme training day. General practitioners were recruited at respective Irish College of General Practitioners (ICGP) continuing medical education (CME) sessions. CME sessions dealing with musculoskeletal medicine were excluded. The response/participation rate was 100%. No student, general practice trainee or general practitioner declined to take the examination. The first medical student group consisted of 60 students who were in their 5th year and had not yet taken a formal course in musculoskeletal medicine. The second medical student group consisted of 72 students in their 5th year who had just completed an intensive 1-week long course in musculoskeletal medicine. 103 general practice trainees were recruited from six regional general practice training schemes. 53 general practitioners were recruited from three continuing medical education groups (CME) study groups. As an additional test of validity the examination was administered to 15 specialist registrars on the Irish Orthopaedic Higher Surgical Training scheme. Respective programme directors were contacted in advance of the project to introduce the study and obtain their support to recruit participants.
Statistical analysis
The means scores of each group were compared with the use of a two-tailed Student’s t test. Comparisons of multiple means were performed with a one-way analysis of variance. Specific groups were then compared with the use of the Bonferroni multiple-comparisons adjustment. All proportions were compared with the use of the chi-square test or the Fisher’s exact test (when indicated). The level of significance was set at 0.05. Statistical analysis was performed with the use of Analyse-It software (Analyse-It, Leeds, UK)
Results
Participant characteristics
Of the 103 general practice trainees 38 were in their first year, 24 in their second year, 32 in their third year and 9 in their fourth year of a general practice training programme. 27 (26%) general practice trainees had completed a rotation in musculoskeletal medicine at postgraduate level. Regarding workload, 102 (65%) general practice trainees and general practitioners claimed that musculoskeletal complaints made up 10–20% of their daily practice. The remaining 35% of general practitioners claimed that musculoskeletal conditions made up less than 10% of their daily workload.
Scores
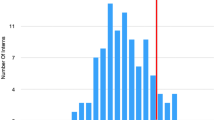
Figure 1 illustrates the average score per group. The average scores for medical students who were pre and post an undergraduate course in musculoskeletal education were 41.9 and 54.3%, respectively. Regarding general practice, the average score for general practice trainees was 61.9 and 60.4% for general practitioners. The mean score for general practice trainees was significantly better than that of the post-course medical students (61.9 vs 54.3%, P < 0.0001). The average score for orthopaedic trainees who were used as an additional test of validity was 95.2%.
Average scores by group. Ortho Reg = Orthopaedic specialist training registrars, Med pre course = medical students before an undergraduate course in musculoskeletal medicine, Med post-course = medical students after an undergraduate course (1 week) in musculoskeletal medicine, GP trainees = general practice trainees, GP = general practitioners
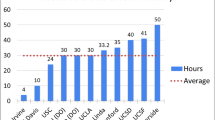
Pass rates
Figure 2 illustrates the pass rates per group. 13 (24%) general practitioners and 29 (28%) general practice trainees achieved the set passing mark of 70. The pass rates for medical students pre and post a week-long course in musculoskeletal medicine were 0 and 12.5%, respectively (P = 0.0128). The pass rate of 27% for general practitioners and trainees was significantly better than that of medical students 12.5% who had undergone a one week-long undergraduate course in musculoskeletal education (P = 0.0223).
Pass rates by group. Ortho Reg = Orthopaedic specialist training registrars, Med pre course = medical students before an undergraduate course in musculoskeletal medicine, Med post-course = medical students after an undergraduate course (1 week) in musculoskeletal medicine, GP trainees = general practice trainees, GP = general practitioners
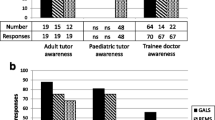
Scores according to whether postgraduate training had included a rotation in musculoskeletal medicine
In the demographic questionnaire, general practitioners and general practice trainees were asked about postgraduate experience in musculoskeletal medicine. A rotation in musculoskeletal medicine was defined as a minimum 3-month rotation in either orthopaedic surgery or rheumatology including internship. 46 (29%) general practitioners and trainees undertook such a rotation. 90% of such rotations occurred outside their general practice training scheme. The average score for general practice trainees and general practitioners who had completed a rotation in musculoskeletal medicine was 67.9%. This was significantly better than those who had not completed a rotation whose average score was 58.7% (P < 0.001). The pass rates correlated with the improved scores and were similarly significantly better for both trainees and general practitioners who had completed a rotation in musculoskeletal medicine (see Fig. 3).
Satisfaction with training in musculoskeletal medicine
Regarding undergraduate musculoskeletal education, 84 (54%) general practitioners (including trainees) had 1 week of formal teaching in musculoskeletal education at undergraduate level. 36 (23%) participants had 2 weeks of formal teaching, while 40 (26%) had no formal teaching. 11 (15%) medical students who had completed a 1-week course were satisfied with their undergraduate training in musculoskeletal medicine. 31 (20%) general practitioners and trainees were satisfied with their undergraduate training in musculoskeletal medicine.
Regarding postgraduate training, 17 (17 %) general practice trainees and 6 (11%) general practitioners were satisfied with their postgraduate training in musculoskeletal medicine. 4 (8%) undertook a continuing medical education (CME) course that dealt primarily with musculoskeletal medicine. 46 (45%) general practice trainees and 34 (60%) general practitioners were satisfied with their ability to perform a basic musculoskeletal examination. The most common reasons participants were not comfortable performing the examination were “inadequate undergraduate training” (60%), “inadequate postgraduate training” (50%) and “other” (10%).
Discussion
Basic competency in musculoskeletal medicine is essential for many specialties being particularly relevant to primary care where musculoskeletal conditions are the second most common reason for visiting a general practitioner accounting for up to 28% of visits [4–8]. Despite this high prevalence, there is a consensus in the literature that general practitioners are not well trained in musculoskeletal medicine [11, 12, 15, 16]. Fowler et al. [16] reported that 95% of patients with symptomatic chronic tears of the anterior cruciate ligament were misdiagnosed by their general practitioner. Sneiderman [11] in a survey of 302 general practitioners found that over half perceived their training in orthopaedics to be inadequate. Lynch et al. [15] in the USA objectively confirmed this in their study where 59 (64%) of 92 general practitioners failed the same validated examination used in this study. Our study agrees with this consensus with 76.7% of general practitioners and 71.8% of general practice trainees failed in the examination. This deficiency in musculoskeletal knowledge may be due to inadequate exposure to musculoskeletal medicine at a number of levels of medical training from medical school through to general practice.
The foundation of musculoskeletal knowledge must begin at undergraduate level. In our study only 11 (15%) of 72 fifth-year medical students surveyed were satisfied with their undergraduate training in musculoskeletal medicine which was reflected by only nine (12.5%) students passing the examination. This poor passing rate after a 1-week course in musculoskeletal medicine highlights the inadequacy of musculoskeletal education at undergraduate level. Current undergraduate medical school curricula are under considerable pressure to accommodate the continuous advance of medical knowledge. In our study the majority (54%) of medical students, general practice trainees and general practitioners received just 1 week of formal undergraduate education in musculoskeletal medicine. Many did not receive any formal training.
This finding of minimal exposure to musculoskeletal medicine in medical school concurs with other studies in the USA, Canada and the UK [17–19]. In a survey in the USA, only 20.5% (25) of 122 medical schools surveyed required a formal period of musculoskeletal education, with that period being an average 2.4 weeks in length [19]. This lack of formal training at undergraduate level needs to be redressed, given the high prevalence of musculoskeletal disorders seen by a wide range of specialists. Whilst musculoskeletal medicine should not necessarily be the dominant topic of medical school curricula, it should be a part of the core curriculum and merit more than 1 week of formal teaching.
The lack of exposure at undergraduate level is not compensated for at postgraduate level. 133 (85%) general practitioners and trainees in our study were not satisfied with their postgraduate training in musculoskeletal medicine and were not comfortable performing a basic musculoskeletal examination. Only 29% of general practitioners undertook a postgraduate rotation in musculoskeletal medicine with the majority of such rotations occurring outside of official general practice training schemes. A similar lack of postgraduate rotations in general practice training schemes has been highlighted in other studies in the UK [17, 20] where in one survey only 10% of general practice training schemes included a rotation in orthopaedics. Our study shows that the score and pass rate improved significantly for general practitioners and trainees who did undertake a rotation in orthopaedic surgery or rheumatology (see Fig. 3). It must be noted however, that even with a postgraduate rotation in musculoskeletal medicine the pass rate for general practitioners was still poor at 36.8%. This demonstrates that although the postgraduate rotations improve the scores, they do not do so to an acceptable level. In light of these findings, general practice trainees would benefit from rotating through musculoskeletal medicine (i.e. orthopaedic surgery or rheumatology) during their training schemes. These rotations however need to be further improved to reflect the needs of general practitioners.
The limitations of this study include the validation process and the selection process for general practitioners. The validation process may have been more appropriately performed by general practitioners rather than internal medicine physicians. It is possible that an internal physicians’ opinion of what is important may not reflect the reality in primary care. Regarding the selection process for general practitioners, only practitioners who participated in CME were included. They are more likely to do better than those who did not participate in CME. However, this does not nullify the results, instead it makes our findings a best-case scenario. Despite these shortcomings, overall we believe it is a useful examination in assessing musculoskeletal knowledge.
This study assessed musculoskeletal knowledge at multiple levels of medical education from undergraduate level to primary care. Deficiencies were found at all levels. The vast majority of participants perceived their education in musculoskeletal education to be inadequate. These findings suggest reform of musculoskeletal education is needed at multiple levels of medical education from undergraduate level to primary care, given the high prevalence of musculoskeletal disease. Curricula should focus on educating students and medical practitioners on common musculoskeletal conditions, emergencies and practical procedures such as joint injection. As the prevalence of bone and joint disease increases, these steps are necessary to ensure that patients receive the optimum level of care when they present to their general practitioner with a musculoskeletal disorder.
References
Weinstein SL (2000) 2000–2010: the bone and joint decade. J Bone Joint Surg Am 82(1):1–3
Woolf AD, Akesson K (2001) Understanding the burden of musculoskeletal conditions. The burden is huge and not reflected in national health priorities. BMJ 322(7294):1079–1080
Simon LS (1999) Osteoarthritis: a review. Clin Cornerstone 2(2):26–37
Geyman JP, Gordon MJ (1979) Orthopedic problems in family practice: incidence, distribution, and curricular implications. J Fam Pract 8(4):759–765
Kahl LE (1987) Musculoskeletal problems in the family practice setting: guidelines for curriculum design. J Rheumatol 14(4):811–814
Marsland DW, Wood M, Mayo F (1976) Content of family practice. Part I. Rank order of diagnoses by frequency. Part II. Diagnoses by disease category and age/sex distribution. J Fam Pract 3(1):37–68
Mulhall KJ, Masterson E (2005) Relating undergraduate musculoskeletal medicine curricula to the needs of modern practice. Ir J Med Sci 174(2):46–51
Lynch JR, Gardner GC, Parsons RR (2005) Musculoskeletal workload versus musculoskeletal clinical confidence among primary care physicians in rural practice. Am J Orthop 34(10):487–491 (discussion)
Matzkin E, Smith EL, Freccero D, Richardson AB (2005) Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am 87(2):310–314
Matheny JM, Brinker MR, Elliott MN, Blake R, Rowane MP (2000) Confidence of graduating family practice residents in their management of musculoskeletal conditions. Am J Orthop 29(12):945–952
Sneiderman C (1977) Orthopedic practice and training of family physicians: a survey of 302 North Carolina practitioners. J Fam Pract 4(2):267–50
Clawson DK, Jackson DW, Ostergaard DJ (2001) It’s past time to reform the musculoskeletal curriculum. Acad Med 76(7):709–710
Freedman KB, Bernstein J (1998) The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am 80(10):1421–1427
Freedman KB, Bernstein J (2002) Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am 84-A(4):604–608
Lynch JR, Schmale GA, Schaad DC, Leopold SS (2006) Important demographic variables impact the musculoskeletal knowledge and confidence of academic primary care physicians. J Bone Joint Surg Am 88(7):1589–1595
Fowler PJ, Regan WD (1987) The patient with symptomatic chronic anterior cruciate ligament insufficiency. Results of minimal arthroscopic surgery and rehabilitation. Am J Sports Med 15(4):321–325
Booth A, Wise DI (1990) General practice training in musculoskeletal disorders. Br J Gen Pract 40(338):390
Pinney SJ, Regan WD (2001) Educating medical students about musculoskeletal problems. Are community needs reflected in the curricula of Canadian medical schools? J Bone Joint Surg Am 83-A(9):1317–1320
DiCaprio MR, Covey A, Bernstein J (2003) Curricular requirements for musculoskeletal medicine in American medical schools. J Bone Joint Surg Am 85-A(3):565–567
Williams JR (2000) The teaching of trauma and orthopaedic surgery to the undergraduate in the United Kingdom. J Bone Joint Surg Br 82(5):627–628
Conflict of interest
No financial support was sought for this study.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
-
1.
What common problem must all newborns be examined for?
-
2.
What is a compartment syndrome?
-
3.
Acute septic arthritis of the knee may be differentiated from inflammatory arthritis by which laboratory test?
-
4.
A patient dislocates his knee in a car accident. What structure(s) is/are at risk for injury and therefore must be evaluated?
-
5.
A patient punches his companion in the face and sustains a fracture of the 5th metacarpal and a 3 mm break in the skin over the fracture. What is the correct treatment and why?
-
6.
A patient comes to the office complaining of low-back pain that wakes him from sleep. What two diagnoses are you concerned about?
-
7.
How is compartment syndrome treated?
-
8.
A patient lands on his hand and is tender to palpation in the “snuff box” (the space between the thumb extensor and abductor tendons). Initial radiographs do not show a fracture. What diagnosis must be considered?
-
9.
A 25-year old male is involved in a motor-vehicle accident. His left lower limb is in a position of flexion at the knee and hip, with internal rotation and adduction of the hip. What is the most likely diagnosis?
-
10.
What nerve is compressed in carpal tunnel syndrome?
-
11.
A patient has a disc herniation pressing on the 5th lumbar nerve root. How is motor function of the 5th lumbar nerve root tested?
-
12.
How is motor function of the median nerve tested in the hand?
-
13.
A 12-year-old-boy severely twists his ankle. Radiographs show only soft-tissue swelling. He is tender at the distal aspect of the fibula. What are the two possible diagnoses?
-
14.
A patient presents with new-onset low back pain. Under what conditions are plain radiographs indicated? Please name five (example history of trauma).
-
15.
A patient has a displaced fracture near the fibular neck. What structure is at risk for injury?
-
16.
A 20-year-old injured his knee while playing football. You see him on the same day, and he has a knee effusion. An aspiration shows frank blood. What are the three most common diagnoses?
-
17.
What are the five most common sources of cancer metastatses to bone?
-
18.
Name two differences between rheumatoid arthritis and osteoarthritis.
-
19.
What malignancy may be present in bone yet typically is not detected with a bone scan?
-
20.
What is the function of the normal anterior cruciate ligament at the knee?
-
21.
What is the difference between osteoporosis and osteomalacia?
-
22.
In elderly patients, displaced fractures of the femoral neck are typically treated with joint replacement, whereas fractures near the trochanter are treated with plates and screws. Why?
-
23.
What muscle(s) is/are involved in lateral epicondylitis (tennis elbow)?
-
24.
Rupture of the biceps at the elbow results in weakness of both elbow flexion and ___________?
-
25.
What muscle(s) control(s) external rotation of the humerus with the arm at the side?
Appendix 2

Rights and permissions
About this article
Cite this article
Queally, J.M., Kiely, P.D., Shelly, M.J. et al. Deficiencies in the education of musculoskeletal medicine in Ireland. Ir J Med Sci 177, 99–105 (2008). https://doi.org/10.1007/s11845-008-0153-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-008-0153-z